Examining an Altruism-Eliciting Video Intervention to Increase COVID-19 Vaccine Intentions in Younger Adults: A Qualitative Assessment Using the Realistic Evaluation Framework
Abstract
1. Introduction
2. Methods
2.1. Study Design and Ethics Statement
2.2. Participants and Setting
2.3. Study Context
2.4. Recruitment
2.5. Procedure
2.6. Interview Guide Development
2.7. Analysis
3. Results
3.1. Focus Group Participants
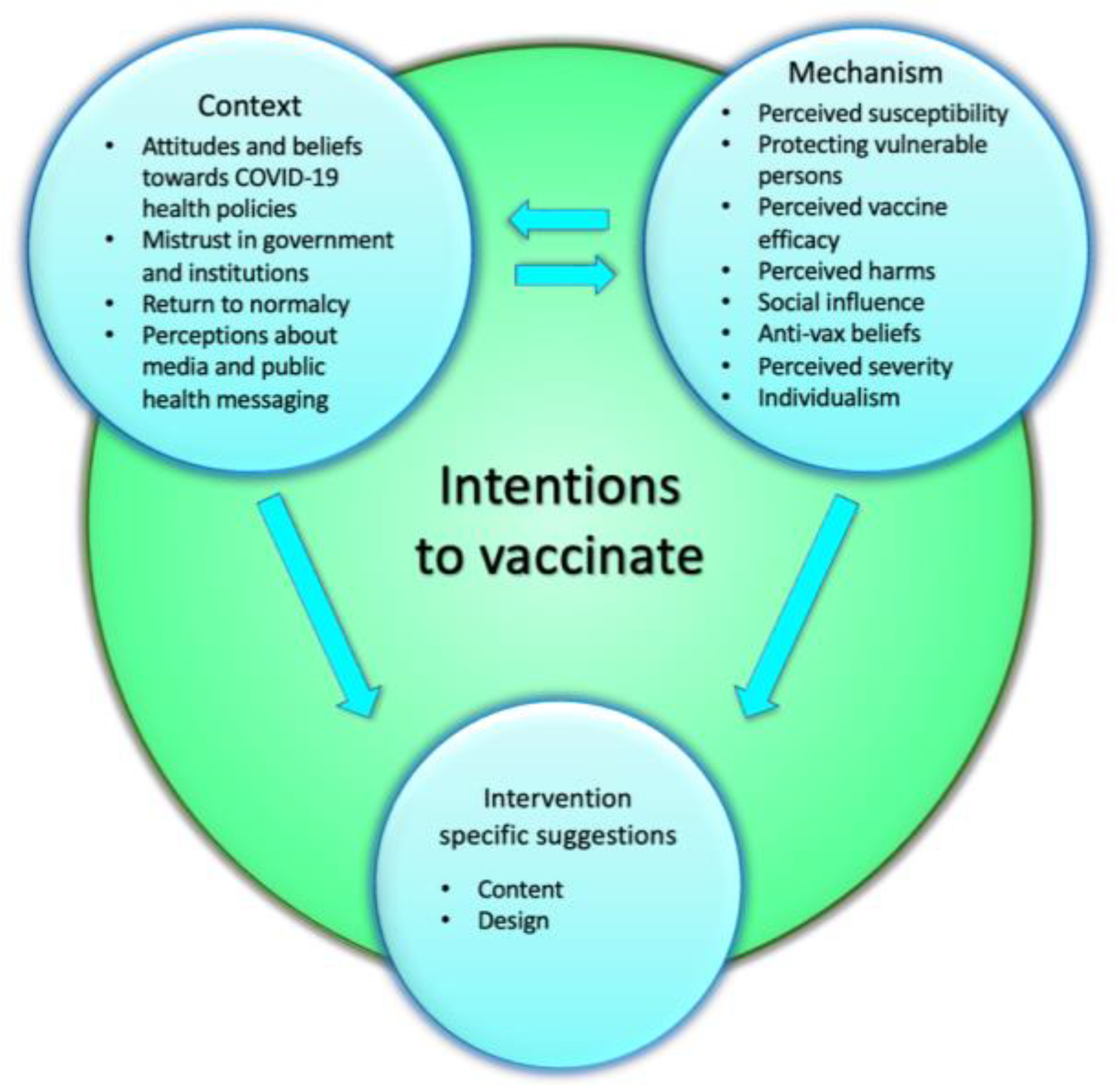
3.2. Thematic Structure
3.3. Context
3.3.1. Attitudes and Beliefs towards COVID-19 Health Policies
“The resolution seems to be, ‘Let’s get vaccinated every six months.’ But what about the next variant or the next pandemic?… I don’t think the solution is just vaccinate yourself out of fear every six months.” (Unvaccinated, P1)
“So if we live in a society where I’m allowed to decide if I want to get the flu vaccine, I’m allowed to make a decision if I want to be on birth control. I’m allowed to make a decision to get an abortion. To me, this is no different. Where does it begin and where does it end?” (Unvaccinated, P3)
3.3.2. Mistrust in Government and Institutions
“If you look at vaccine-induced myocarditis in younger people, I think the Canadian government says it’s—I think they were saying there’s Ontario did a study, I think it was one in 5000. But you look across the world, and it’s a lot more frequent in certain places. So I’d just like to see more transparency, and see these issues looked into more.” (Unvaccinated, P4)
“But the issue is six months from now, when that doesn’t happen, it just hurts trust. At this point, I’m not even sure who to trust. Right? Can you trust Trudeau [Canadian Prime Minister]? Can you trust Legault [Quebec Premier]? I can’t.” (Unvaccinated, P3)
3.3.3. Return to Normalcy
“So they felt that it was good to lift the restrictions to live a more free life, but it was sort of neglecting that other people have different lives, different backgrounds, different family situations and whatnot, and so on. And yeah, I think people became a little self-centered in what they wanted and their desires of society, and they stopped realizing that everybody has a different situation.” (Boosted, P6)
3.3.4. Perceptions about Media and Public Health Messaging
“What I would have liked to see during the pandemic that I wasn’t able to find myself, whether or not it was there, was a certain availability of… the science that was in between the direct academia and what I saw was potentially overly simplified messaging on the official government websites and maybe the newsclips in media that it wasn’t really getting… there was something kind of a middle ground, it was kind of missing, that I think I would have really enjoyed to get a better understanding of what actually was happening in the pandemic, and then I would be able to feel like I was making a more informed decision.” (Boosted, P4)
“with the first messaging that you created, that was also at a time where we didn’t have as much information as we do now, and at that time as well there was—I don’t want to use the word ‘hysteria’, but there was a lot of panic and stress being felt along a lot of people who were, honestly, very scared of what was coming out.” (Fully vaccinated, P7)
“The general ads that roll on TV, I think that’s an antiquated way of relaying information or trying to convince people of doing things.” (Fully vaccinated, P3)
3.4. Mechanism
3.4.1. Perceived Susceptibility
“Given the fact that a significant amount of the population is already vaccinated, they don’t feel perhaps a need to get vaccinated now, because they feel as though they’re sort of immune to the challenges that are happening, yeah, I guess, as it relates to COVID-19.” (Boosted, P2)
“… but when I was forced to go back to school in September in person, that was when I was like “Okay. Now I am going into rooms with hundreds of people who I don’t know”, so that’s what pushed me more to get my vaccines.” (Fully vaccinated, P3)
3.4.2. Protecting Vulnerable Persons, Significant Others, the Community
“and I’m actually an example, because my father was diagnosed with leukemia a week ago. So if I saw that video, it would be a push for me to go get the third and the fourth” (Fully vaccinated, P1)
3.4.3. Perceived Vaccine Efficacy
“And also, if they were 95% effective, (the pandemic) would have been gone away. I’m determined that we’re all going to catch COVID, and we’re just giving each other false hope by vaccinating.” (Unvaccinated, P3)
3.4.4. Perceived Harms
“I think a lot of people are not okay with the not knowing… it can make one feel “Am I a lab rat?” (Fully vaccinated, P7)
“There’s so much learning that needs to be done around COVID, and long COVID, and the effects of COVID, and where the heck did COVID come from. Sorry, I don’t want to be your human guinea pig.” (Unvaccinated, P1)
“But in terms of the vaccine, how do I know what’s going to happen to me 10 years from now? If you guys don’t know what’s happening five days from now or a month from now, you can’t even tell me what’s going to happen 10 years from now.” (Unvaccinated, P2)
“I could see why people would not want to get the vaccine after having caught COVID, because why risk side effects for potentially no benefit and vaccine benefits post COVID” (Fully vaccinated, P3)
“…when I had gone to get a vaccine, and my decision not to do it was that I asked the person at the counter, I said, ‘If anything ends up happening and I get side effects, is there any recourse?’ And the answer was no. And that didn’t sit well” (Unvaccinated, P2)
3.4.5. Social Influence
“Maybe personally, just around my circle, there’s people who have boosters, people who have double dose, some unvaccinated friends, and a lot of people around them got sick, and there didn’t really seemed to be a difference in terms of the severity of COVID when they caught it. And so, I guess, for me, personally, I didn’t think it was really necessary for me.” (Fully vaccinated, P4)
“I remember when people first started taking the shot, and there was TikTok videos of magnets. My cousin, it happened to her. She put a video on Facebook how after she took the shot, her arm was magnetized. So I believe my cousin, because it was working, there were magnets on her arm.” (Unvaccinated, P1)
“… when I did discuss with somebody in my entourage who was really against vaccinations, he didn’t believe in COVID, he—I think one of the things that he did mention is that every time he spoke to anybody, they really—antagonizing his views and made him even more, I think, want to go to an alternative media, where he felt there was a community with people like himself who had similar beliefs and where he felt more listened to.” (Boosted, P5)
3.4.6. Anti-vaccination Beliefs
“I think people who are conspiracy theorists might feel like they’re really attacked all the time. They just don’t want to participate in that, and I think it makes them even more want to go against the grain and to not get the vaccinations, not wear masks” (Boosted, P5).
3.4.7. Perceived Severity
“Well, okay, a lot of my friends are getting it, and then after a couple days or maybe a week or two they’ve recovered.” (Boosted, P4).
“I haven’t seen anyone in a situation like this, this intense, but my sister, she caught it, and she still has effects, she hasn’t regained her sense of smell, taste. So it is quite intense. I would be very sad and depressed if I were in her situation.” (Boosted, P7)
3.4.8. Individualism
“Well, I don’t have a relative with a major disease or I’m not having any particular health condition, so why would I get the vaccine?” (Boosted, P5).
“…if you aren’t able to maintain your health and this does occur, there will be significant and long-lasting effects on freedom, if that’s your ultimate sort of value that you hold near and dear” (Boosted, P2)
3.5. Intervention-Specific Suggestions
3.5.1. Content
“The messaging shouldn’t be like a one shoe fits all type of things, I feel like different people, different personalities, different levels of empathy, they have different reasons for why they get the vaccine, some people might be immunocompromised, some people want to protect their families, and so kind of a more personalized one-to-one messaging I think would be more effective in this kind of mass marketing type of messaging” (Fully vaccinated, P4)
“Just getting whole numbers. I’m not one for anecdotes, I don’t like these stories, I don’t like being lectured by an advertisement. I just want the numbers. I don’t know, it feels like there’s trickery going on when it’s these stories.” (Fully vaccinated, P3)
“I think making it more personal and making people be able to understand the facts, but then also be able to voice their concerns in a way that they don’t feel, maybe, getting any pushback from society and to make it more of a private, personal choice” (Fully vaccinated, P7)
“…or maybe figuring out a way to communicate how at an individual level and as a collective group people can create meaningful actions, so as to ensure that there is tangible change moving forward, I think would be a really powerful thing to do…” (Boosted, P2)
3.5.2. Design
“… for example, is to show, perhaps, the significant and devastating effects of COVID, like to show graphic images of people lying in hospital beds, struggling to maintain their basic functions.” (Boosted, P2)
“‘Only 1% of people who have had the vaccine have suffered any serious side effects.’ Statistics. Numbers. Don’t come to me with feelings.” (Unvaccinated, P1)
“It’s kind of hard to say to somebody’s face like, “I’m sorry, your ad didn’t actually help at all.” I’m not saying that that’s a fact. I’m just saying just the social element, I could see why somebody would say, ‘Yeah, you know, actually I do want to get vaccinated,’ but then, as soon as they leave the study, they’re like, ‘It didn’t change my mind at all.’” (Fully vaccinated, P3)
4. Discussion
Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Watson, O.J.; Barnsley, G.; Toor, J.; Hogan, A.B.; Winskill, P.; Ghani, A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022, 22, 1293–1302. [Google Scholar] [CrossRef]
- Nordström, P.; Ballin, M.; Nordström, A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: A retrospective, total population cohort study in Sweden. Lancet 2022, 399, 814–823. [Google Scholar] [CrossRef]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, E.S.; Dorabawila, V.; Easton, D.; Bauer, U.E.; Kumar, J.; Hoen, R.; Hoefer, D.; Wu, M.; Lutterloh, E.; Conroy, M.B.; et al. COVID-19 Vaccine Effectiveness in New York State. N. Engl. J. Med. 2021, 386, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. COVID-19 Vaccine: Canadian Immunization Guide. Available online: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-26-covid-19-vaccine.html (accessed on 8 November 2022).
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. Available online: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf (accessed on 27 February 2023).
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Cheshmehzangi, A.; McDonnell, D.; da Veiga, C.P.; Xiang, Y.-T. Mind the “Vaccine Fatigue”. Front. Immunol. 2022, 13. [Google Scholar] [CrossRef]
- Government of Canada. COVID-19 Vaccination in Canada. Available online: https://health-infobase.canada.ca/covid-19/vaccination-coverage/ (accessed on 27 February 2023).
- Chapman, G.B.; Li, M.; Vietri, J.; Ibuka, Y.; Thomas, D.; Yoon, H.; Galvani, A.P. Using game theory to examine incentives in influenza vaccination behavior. Psychol. Sci. 2012, 23, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing Vaccination: Putting Psychological Science Into Action. Psychol. Sci. Public Interest 2017, 18, 149–207. [Google Scholar] [CrossRef]
- Betsch, C.; Böhm, R.; Korn, L.; Holtmann, C. On the benefits of explaining herd immunity in vaccine advocacy. Nat. Hum. Behav. 2017, 1, 1–6. [Google Scholar] [CrossRef]
- Zhu, P.; Perez, S.; Griffin-Mathieu, G.; Tatar, O.; Rosberger, Z. What influences parents to vaccinate (or not) their sons with the Human Papillomavirus (HPV) vaccine: An examination of HPV vaccine decision-making changes over time. J. Psychosoc. Oncol. Res. Pract. 2022, 4, e068. [Google Scholar] [CrossRef]
- Pfattheicher, S.; Nielsen, Y.A.; Thielmann, I. Prosocial behavior and altruism: A review of concepts and definitions. Curr. Opin. Psychol. 2022, 44, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.; Tatar, O.; Griffin-Mathieu, G.; Perez, S.; Haward, B.; Zimet, G.; Tunis, M.; Dubé, È.; Rosberger, Z. The Efficacy of a Brief, Altruism-Eliciting Video Intervention in Enhancing COVID-19 Vaccination Intentions Among a Population-Based Sample of Younger Adults: Randomized Controlled Trial. JMIR Public Health Surveill. 2022, 8, e37328. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef]
- Zoom Video Communications Inc. Zoom Security Guide. Available online: https://explore.zoom.us/docs/doc/Zoom-Security-White-Paper.pdf (accessed on 27 February 2023).
- Tatar, O.; Shapiro, G.K.; Perez, S.; Wade, K.; Rosberger, Z. Using the precaution adoption process model to clarify human papillomavirus vaccine hesitancy in Canadian parents of girls and parents of boys. Hum. Vaccin. Immunother 2019, 15, 1803–1814. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Vaccination Video (EN). Available online: https://www.youtube.com/watch?v=hNhNiingRjw&ab_channel=PSOLab (accessed on 27 February 2023).
- Vaccination Video (FR). Available online: https://www.youtube.com/watch?v=Zoa7VBgIzQA (accessed on 27 February 2023).
- Hinyard, L.J.; Kreuter, M.W. Using Narrative Communication as a Tool for Health Behavior Change: A Conceptual, Theoretical, and Empirical Overview. Health Educ. Behav. 2007, 34, 777–792. [Google Scholar] [CrossRef]
- Pawson, R.; Tilley, N. Realistic Evaluation; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 1997. [Google Scholar]
- Westhorp, G. Realist Impact Evaluation: An Introduction; Overseas Development Institute: London, UK, 2014; Available online: https://odi.org/en/publications/realist-impact-evaluation-an-introduction/ (accessed on 27 February 2023).
- QSR International Ply Ltd. NVivo (Released March 2020); QSR International Ply Ltd.: Burlington, MA, USA, 2022. [Google Scholar]
- Champion, V.L.; Skinner, C.S. The Health Belief Model. In Health Behavior and Health Education: Theory, Research, and Practice; Jossey-Bass: San Francisco, CA, USA, 2008; Volume 4, pp. 45–65. [Google Scholar]
- World Health Organization (WHO). Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19. In Policy Framework for Supporting Pandemic Prevention and Management; 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/335820/WHO-EURO-2020-1160-40906-55390-eng.pdf (accessed on 27 February 2023).
- Bodas, M.; Kaim, A.; Velan, B.; Ziv, A.; Jaffe, E.; Adini, B. Overcoming the effect of pandemic fatigue on vaccine hesitancy—Will belief in science triumph? J. Nurs. Sch. 2022, 55, 262–271. [Google Scholar] [CrossRef]
- Cleofas, J.V.; Oducado, R.M.F. Demographic, Health and Pandemic-Related Determinants of COVID-19 Vaccination Intention Among Filipino Emerging Adults. Emerg. Adulthood 2022, 10, 815–820. [Google Scholar] [CrossRef]
- Haktanir, A.; Can, N.; Seki, T.; Kurnaz, M.F.; Dilmaç, B. Do we experience pandemic fatigue? Current state, predictors, and prevention. Curr. Psychol. 2022, 41, 7314–7325. [Google Scholar] [CrossRef]
- Benham, J.L.; Lang, R.; Kovacs Burns, K.; MacKean, G.; Léveillé, T.; McCormack, B.; Sheikh, H.; Fullerton, M.M.; Tang, T.; Boucher, J.-C.; et al. Attitudes, current behaviours and barriers to public health measures that reduce COVID-19 transmission: A qualitative study to inform public health messaging. PLoS ONE 2021, 16, e0246941. [Google Scholar] [CrossRef]
- Gong, Z.; Tang, Z.; Li, J. What Strategy Is Better for Promoting COVID-19 Vaccination? A Comparison between Gain-Framed, Loss-Framed, and Altruistic Messages. Ann. Behav. Med. 2021, 56, 325–331. [Google Scholar] [CrossRef]
- Hong, Y.; Hashimoto, M. I Will Get Myself Vaccinated for Others: The Interplay of Message Frame, Reference Point, and Perceived Risk on Intention for COVID-19 Vaccine. Health Commun. 2021, 38, 1–11. [Google Scholar] [CrossRef]
- Peng, L.; Guo, Y.; Hu, D. Information Framing Effect on Public’s Intention to Receive the COVID-19 Vaccination in China. Vaccines 2021, 9, 995. [Google Scholar] [CrossRef]
- Reinhardt, A.; Rossmann, C. Age-related framing effects: Why vaccination against COVID-19 should be promoted differently in younger and older adults. J. Exp. Psychol. Appl. 2021, 27, 669–678. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Belati, A.; Tulone, O.; Diella, L.; Fiore Bavaro, D.; Bonica, R.; Genna, V.; Smith, L.; Trott, M.; Bruyere, O.; et al. Incidence of long COVID-19 in people with previous SARS-Cov2 infection: A systematic review and meta-analysis of 120,970 patients. Intern. Emerg. Med. 2022. [Google Scholar] [CrossRef]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef]
- Wake, A.D. The Willingness to Receive COVID-19 Vaccine and Its Associated Factors: “Vaccination Refusal Could Prolong the War of This Pandemic”—A Systematic Review. Risk Manag. Healthc. Policy 2021, 14, 2609–2623. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2021, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Aw, J.; Seng, J.J.; Seah, S.S.; Low, L.L. COVID-19 Vaccine Hesitancy—A Scoping Review of Literature in High-Income Countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef]
- Betsch, C.; Brewer, N.T.; Brocard, P.; Davies, P.; Gaissmaier, W.; Haase, N.; Leask, J.; Renkewitz, F.; Renner, B.; Reyna, V.F.; et al. Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine 2012, 30, 3727–3733. [Google Scholar] [CrossRef] [PubMed]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccin. Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Lockyer, B.; Islam, S.; Rahman, A.; Dickerson, J.; Pickett, K.; Sheldon, T.; Wright, J.; McEachan, R.; Sheard, L.; The Bradford Institute for Health Research COVID-19 Scientific Advisory Group. Understanding COVID-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021, 24, 1158–1167. [Google Scholar] [CrossRef]
- Wang, R.; Zhang, H. Who spread COVID-19 (mis)information online? Differential informedness, psychological mechanisms, and intervention strategies. Comput. Hum. Behav. 2023, 138, 107486. [Google Scholar] [CrossRef]
- Pennycook, G.; Epstein, Z.; Mosleh, M.; Arechar, A.A.; Eckles, D.; Rand, D.G. Shifting attention to accuracy can reduce misinformation online. Nature 2021, 592, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Pennycook, G.; McPhetres, J.; Zhang, Y.; Lu, J.G.; Rand, D.G. Fighting COVID-19 Misinformation on Social Media: Experimental Evidence for a Scalable Accuracy-Nudge Intervention. Psychol. Sci. 2020, 31, 770–780. [Google Scholar] [CrossRef]
- Burke, P.F.; Masters, D.; Massey, G. Enablers and barriers to COVID-19 vaccine uptake: An international study of perceptions and intentions. Vaccine 2021, 39, 5116–5128. [Google Scholar] [CrossRef]
- Walsh, J.C.; Comar, M.; Folan, J.; Williams, S.; Kola-Palmer, S. The psychological and behavioural correlates of COVID-19 vaccine hesitancy and resistance in Ireland and the UK. Acta Psychol. 2022, 225, 103550. [Google Scholar] [CrossRef]
- Hajek, A.; König, H.-H. Level and correlates of empathy and altruism during the COVID-19 pandemic. Evidence from a representative survey in Germany. PLoS ONE 2022, 17, e0265544. [Google Scholar] [CrossRef] [PubMed]
- Wismans, A.; Thurik, R.; Baptista, R.; Dejardin, M.; Janssen, F.; Franken, I. Psychological characteristics and the mediating role of the 5C Model in explaining students’ COVID-19 vaccination intention. PLoS ONE 2021, 16, e0255382. [Google Scholar] [CrossRef]
- Rieger, M.O. Triggering altruism increases the willingness to get vaccinated against COVID-19. Soc. Health Behav. 2020, 3, 78. [Google Scholar] [CrossRef]
- Tatar, O.; Haward, B.; Zhu, P.; Griffin-Mathieu, G.; Perez, S.; Zimet, G.; Rosberger, Z. Using Best-Worst Scaling to investigate younger adult Canadians’ preferences for COVID-19 vaccination and public health measures: An observational study. Prev. Med. Rep. 2022, 26, 101755. [Google Scholar] [CrossRef]
- Tanaka, T.; Nihonsugi, T.; Ohtake, F.; Haruno, M. A message of the majority with scientific evidence encourages young people to show their prosocial nature in COVID-19 vaccination. Sci. Rep. 2021, 11, 23261. [Google Scholar] [CrossRef]
- Shawar, B.A.; Atwell, E. Chatbots: Are they really useful? J. Lang. Technol. Comput. Linguist. 2007, 22, 29–49. [Google Scholar] [CrossRef]
- Luk, T.T.; Lui, J.H.T.; Wang, M.P. Efficacy, Usability, and Acceptability of a Chatbot for Promoting COVID-19 Vaccination in Unvaccinated or Booster-Hesitant Young Adults: Pre-Post Pilot Study. J. Med. Internet Res. 2022, 24, e39063. [Google Scholar] [CrossRef]
- Altay, S.; Hacquin, A.-S.; Chevallier, C.; Mercier, H. Information delivered by a chatbot has a positive impact on COVID-19 vaccines attitudes and intentions. J. Exp. Psychol. Appl. 2021, 29, 52–62. [Google Scholar] [CrossRef] [PubMed]
- El Hefny, W.; Elshimy, M.; El Bolock, A.; Abdennadher, S. Vaxera: An Empathetic Chatbot for COVID-19 Vaccination. In Proceedings of the Highlights in Practical Applications of Agents, Multi-Agent Systems, and Complex Systems Simulation, L’Aquila, Italy, 13–15 July 2022; The PAAMS Collection: Cham, Switzerland, 2022; pp. 157–168. [Google Scholar]
- Kobayashi, T.; Nishina, Y.; Tomoi, H.; Harada, K.; Tanaka, K.; Matsumoto, E.; Horimukai, K.; Ishihara, J.; Sasaki, S.; Inaba, K.; et al. Corowa-kun: A messenger app chatbot delivers COVID-19 vaccine information, Japan 2021. Vaccine 2022, 40, 4654–4662. [Google Scholar] [CrossRef]
- John, P.; McAndrews, J.; Loewen, P.; Banerjee, S.; Savani, M.; Koenig, R.; Nyhan, B.; Lee-Whiting, B. Overcoming Barriers to Vaccination by Empowering Citizens to Make Deliberate Choices; The British Academy: London, UK, 2022. [Google Scholar]
- Thaler, R.H.; Sunstein, C.R. Nudge: Improving Decisions about Health, Wealth, and Happiness; Yale University Press: New Haven, CT, USA, 2008; Volume 1, p. 89. [Google Scholar]
- Reñosa, M.D.C.; Landicho, J.; Wachinger, J.; Dalglish, S.L.; Bärnighausen, K.; Bärnighausen, T.; McMahon, S.A. Nudging toward vaccination: A systematic review. BMJ Glob. Health 2021, 6, e006237. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Yu, L.-M.; Freeman, J.; Chadwick, A.; Vaccari, C.; Shanyinde, M.; Harris, V.; Waite, F.; Rosebrock, L.; et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomised controlled trial. Lancet Public Health 2021, 6, e416–e427. [Google Scholar] [CrossRef]
- Bardosh, K.; de Figueiredo, A.; Gur-Arie, R.; Jamrozik, E.; Doidge, J.; Lemmens, T.; Keshavjee, S.; Graham, J.E.; Baral, S. The unintended consequences of COVID-19 vaccine policy: Why mandates, passports and restrictions may cause more harm than good. BMJ Global Health 2022, 7, e008684. [Google Scholar] [CrossRef]
- Vujovich-Dunn, C.; Kaufman, J.; King, C.; Skinner, S.R.; Wand, H.; Guy, R.; Leask, J. A systematic review and meta-analysis of effectiveness of decision aids for vaccination decision-making. Vaccine 2021, 39, 3655–3665. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.A.; Dayton, L.; Miller, J.R.; Yi, G.; Jaleel, A.; Nwosu, C.C.; Yang, C.; Falade-Nwulia, O. Behavioral and Attitudinal Correlates of Trusted Sources of COVID-19 Vaccine Information in the US. Behav. Sci. 2021, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Van Oost, P.; Yzerbyt, V.; Schmitz, M.; Vansteenkiste, M.; Luminet, O.; Morbée, S.; Van den Bergh, O.; Waterschoot, J.; Klein, O. The relation between conspiracism, government trust, and COVID-19 vaccination intentions: The key role of motivation. Soc. Sci. Med. 2022, 301, 114926. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Chen, X.; Lee, W.; Lin, F. Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. Int. J. Environ. Res. Public Health 2022, 19, 8033. [Google Scholar] [CrossRef]
- Elgar, F.J.; Stefaniak, A.; Wohl, M.J.A. The trouble with trust: Time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc. Sci. Med. 2020, 263, 113365. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Parsons Leigh, J.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef]
- Hyland-Wood, B.; Gardner, J.; Leask, J.; Ecker, U.K.H. Toward effective government communication strategies in the era of COVID-19. Humanit. Soc. Sci. Commun. 2021, 8, 30. [Google Scholar] [CrossRef]
- World Health Organization. Vaccination and Trust: How Concerns Arise and the Role of Communication in Mitigating Crises. Available online: https://www.euro.who.int/__data/assets/pdf_file/0004/329647/Vaccines-and-trust.PDF (accessed on 27 February 2023).
- Flick, U. Triangulation revisited: Strategy of validation or alternative? J. Theory Soc. Behav. 1992, 22, 175–197. [Google Scholar] [CrossRef]
- Bor, A.; Jørgensen, F.; Petersen, M.B. Discriminatory Attitudes against the Unvaccinated during a Global Pandemic. Nature 2022, 613, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Olsen, R. Encyclopedia of Survey Research Methods; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2008; Available online: https://methods.sagepub.com/reference/encyclopedia-of-survey-research-methods (accessed on 27 February 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, P.; Tatar, O.; Haward, B.; Steck, V.; Griffin-Mathieu, G.; Perez, S.; Dubé, È.; Zimet, G.; Rosberger, Z. Examining an Altruism-Eliciting Video Intervention to Increase COVID-19 Vaccine Intentions in Younger Adults: A Qualitative Assessment Using the Realistic Evaluation Framework. Vaccines 2023, 11, 628. https://doi.org/10.3390/vaccines11030628
Zhu P, Tatar O, Haward B, Steck V, Griffin-Mathieu G, Perez S, Dubé È, Zimet G, Rosberger Z. Examining an Altruism-Eliciting Video Intervention to Increase COVID-19 Vaccine Intentions in Younger Adults: A Qualitative Assessment Using the Realistic Evaluation Framework. Vaccines. 2023; 11(3):628. https://doi.org/10.3390/vaccines11030628
Chicago/Turabian StyleZhu, Patricia, Ovidiu Tatar, Ben Haward, Veronica Steck, Gabrielle Griffin-Mathieu, Samara Perez, Ève Dubé, Gregory Zimet, and Zeev Rosberger. 2023. "Examining an Altruism-Eliciting Video Intervention to Increase COVID-19 Vaccine Intentions in Younger Adults: A Qualitative Assessment Using the Realistic Evaluation Framework" Vaccines 11, no. 3: 628. https://doi.org/10.3390/vaccines11030628
APA StyleZhu, P., Tatar, O., Haward, B., Steck, V., Griffin-Mathieu, G., Perez, S., Dubé, È., Zimet, G., & Rosberger, Z. (2023). Examining an Altruism-Eliciting Video Intervention to Increase COVID-19 Vaccine Intentions in Younger Adults: A Qualitative Assessment Using the Realistic Evaluation Framework. Vaccines, 11(3), 628. https://doi.org/10.3390/vaccines11030628






