Qualitative Insights into Vaccine Uptake of Nursing Staff in Long-Term Care Facilities in Finland
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Recruitment
2.2. Data Collection
2.3. Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Information Sources of COVID-19 Vaccines
“They just told us that the vaccine was now available, and we could take it during working hours at the city vaccination sites.”(Assistant nurse, private sector)
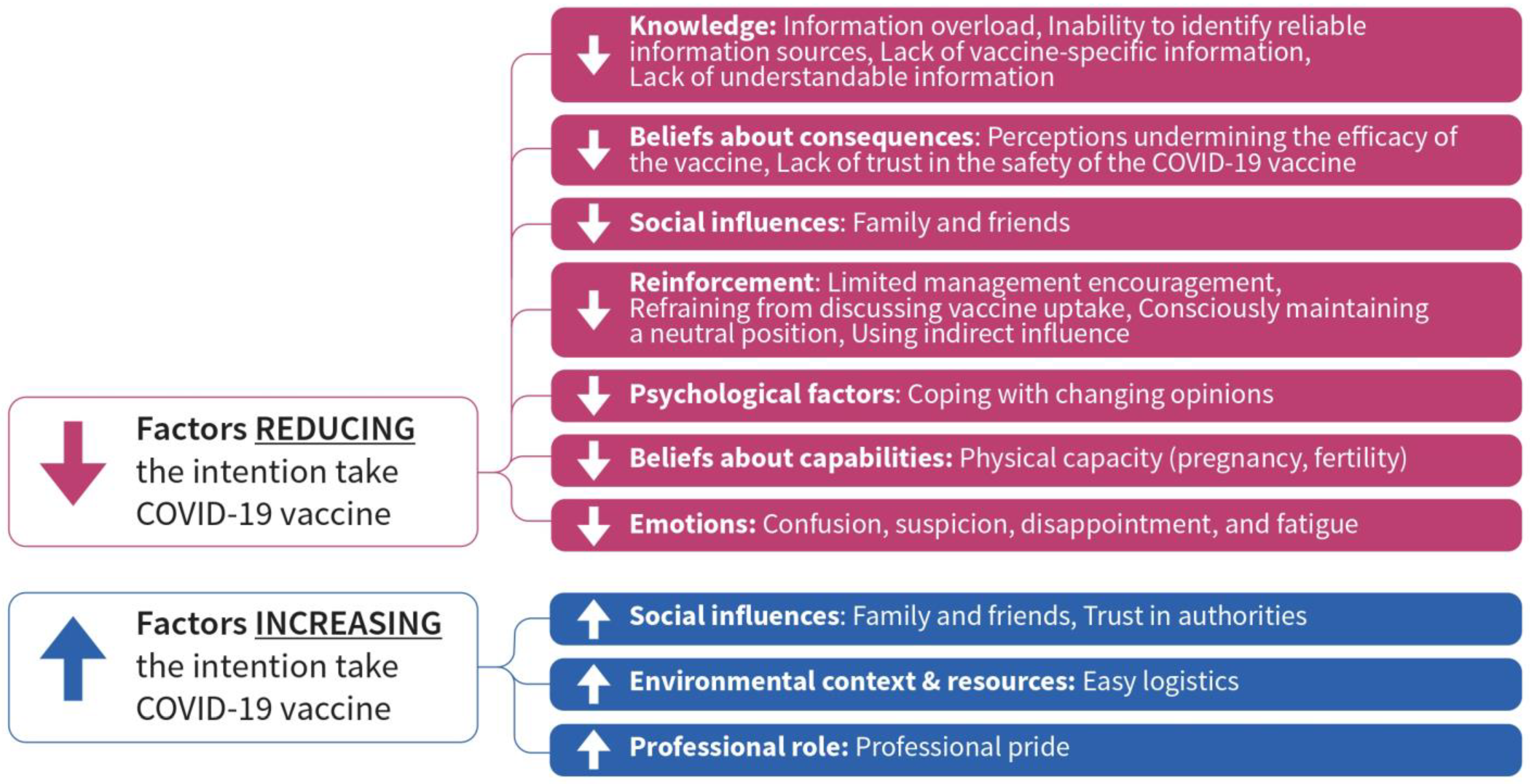
3.3. Factors Discouraging Uptake of COVID-19 Vaccine
3.3.1. Domain: Knowledge
Information Overload
“I am getting tired. Too much information, too confusing. I don’t feel I am getting a clear understanding of the vaccine.”(Assistant nurse, public sector)
Inability to Identify Reliable Information Sources
“Different doctors said different things about corona vaccines. In the end, you can’t trust anyone. You decide to follow your instincts. I felt the corona vaccine could be a risk and I am not willing to take that risk.”(Assistant nurse, private sector)
Lack of Vaccine-Specific Information
“I went to the vaccination point in the city and asked them to show me the package so that I know what the vaccine contains and what the potential side effects are. Any medicine has this description. They told me that this information was not available. This is when I decided not to take the vaccine.”(Assistant nurse, private sector)
Lack of Understandable Information
“We sometimes have to read the information a number of times. I am not surprised that the nursing staff does not always grasp what is being communicated. When the Astra Zeneca vaccine was halted, I found many staff members not understanding the situation. They wondered why and how that vaccine differed from the other available vaccines. There was general worry around the vaccine and no available information to reassure.”(Manager, private sector)
“I think there is so much information, so we do not need to take the role of disseminating vaccine-related information.”(Manager, public sector)
3.3.2. Domain: Beliefs about Consequences
Perceptions Undermining the Efficacy of the Vaccine
“We have learned that even if you are vaccinated you can transmit the virus. What kind of vaccine is this? How does it make sense to take the vaccine?”(Assistant nurse, private sector)
“We thought that the vaccine can prevent virus transmission. But it does not. Many of our residents were vaccinated and they still got the virus. I see no reason to take the vaccine.”(Assistant nurse, private sector)
“Many of my nursing staff believe strongly that the vaccine was a failure and with or without the vaccine the situation remains the same. I only had some staff members who didn’t take the vaccine but this is where the discussions were focused.”(Manager, private sector)
“Speaking with my colleagues, nothing has happened although all residents and many nursing staff members have received the vaccine. It is a big disappointment that we have to carry on using the masks.”(Assistant nurse, public sector)
“First, they told me to wait 6 months because I had corona. After that, I did not feel like taking it. What would I benefit of the vaccine? I have immunity.”(Assistant nurse, private sector)
Lack of Trust in the Safety of the COVID-19 Vaccine
“Honestly, I have very bad experiences from my childhood. I got so sick when I got my vaccination. This is what my mom used to say. I am thinking that I will have some strong side effects should I take the [COVID-19] vaccine.”(Assistant nurse, private sector)
“I only need to think about the swine flu pandemic and I get worried. I don’t want to get severe side effects and be unable to continue my everyday life. I am thinking of all these people who got narcolepsy from that vaccine.”(Assistant nurse, public sector)
“I had some staff members that believe in these circulating rumors about infertility. They are not based on any real information, but they are real and powerful.”(Manager, private sector)
3.3.3. Domain: Social Influences
Influence of Family and Friends
“None of my friends have taken the vaccine. It was clear to me that I would not take it either.”(Assistant nurse, public sector)
3.3.4. Domain: Reinforcement
Limited Management Encouragement
“Nobody has asked me about the vaccine. We don’t speak about it.”(Assistant nurse, public sector)
“My boss told us that the vaccine was available. He did not say anything more. I felt perhaps he wanted us to take the vaccine, but it was for me to decide that.”(Assistant nurse, public sector)
Refraining from Discussing Vaccine Uptake
“We haven’t spoken about it. I don’t know who took the vaccine. It is a personal matter.”(Manager, private sector)
Consciously Maintaining a Neutral Position
“I made clear to my staff that I am neutral, and I am not planning to give them advice.”(Manager, public sector)
Using Indirect Influence
“I made sure that all my staff knew that I took the vaccine. It is important to be an example.”(Manager, public sector)
“I am not convinced about the vaccine myself.”(Manager, private sector)
3.3.5. Domain: Psychological Factors
Coping with Changing Opinions
“I had some inaccurate ideas about the pandemic. I did not understand that it would reach such a massive scope. But because I had already made up my mind not to take the vaccine, I was not ready to change my position.”(Assistant nurse, public sector)
3.3.6. Domain: Beliefs about Capabilities
Physical Capability
“I don’t want to take the risk of not having children. I am still young.”(Assistant nurse, public sector)
“Those who were pregnant refused the vaccine even after it was recommended. They wanted to play it safe.”(Manager, private sector)
3.3.7. Domain: Emotions
Confusion, Suspicion, Disappointment, and Fatigue
“This has been an emotional rollercoaster with different feelings but always strong ones.”(Assistant nurse, private sector)
3.4. Factors That Encourage the Uptake of the COVID-19 Vaccine
3.4.1. Domain: Social Influences
Influence of Family and Friends
“My husband thinks I should take the vaccine. I am considering it.”(Assistant nurse, private sector)
Trust in Authorities
“I know that any vaccine that is offered to us is well researched and planned. I know nobody wants to harm us.”(Assistant nurse, private sector)
3.4.2. Domain: Environmental Context and Resources
Easy Logistics
“Vaccines were made available and instructions on how to take them were given. There was nothing unclear about it or difficult.”(Assistant nurse, private sector)
3.4.3. Domain: Professional Role
Professional Pride
“I know that as frontline workers, we must take the vaccine, but I am afraid. It makes me feel so guilty.”(Assistant nurse, public sector)
“I make sure to practice hand hygiene procedures and I am always wearing a mask. This is the way I protect the residents. The vaccine does not play a major role.”(Assistant nurse, private sector)
“The great majority of my staff believes that nursing staff has a special need to take the vaccine.”(Manager, public sector)
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Christie, A.; Henley, S.J.; Mattocks, L.; Fernando, R.; Lansky, A.; Ahmad, F.B.; Adjemian, J.; Anderson, R.N.; Binder, A.M.; Carey, K.; et al. Decreases in COVID-19 Cases, Emergency Department Visits, Hospital Admissions, and Deaths Among Older Adults Following the Introduction of COVID-19 Vaccine—United States, September 6, 2020–May 1, 2021. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 858–864. [Google Scholar] [CrossRef]
- Chemaitelly, H.; Ayoub, H.H.; AlMukdad, S.; Coyle, P.; Tang, P.; Yassine, H.M.; Al-Khatib, H.A.; Smatti, M.K.; Hasan, M.R.; Al-Kanaani, Z.; et al. Duration of mRNA vaccine protection against SARS-CoV-2 Omicron BA.1 and BA.2 subvariants in Qatar. Nat. Commun. 2022, 13, 3082. [Google Scholar] [CrossRef] [PubMed]
- Crèvecoeur, J.; Hens, N.; Neyens, T.; Larivière, Y.; Verhasselt, B.; Masson, H.; Theeten, H. Change in COVID19 outbreak pattern following vaccination in long-term care facilities in Flanders, Belgium. Vaccine 2022, 40, 6218–6224. [Google Scholar] [CrossRef] [PubMed]
- Fallon, A.; Dukelow, T.; Kennelly, S.P.; O’Neill, D. COVID-19 in nursing homes. Qjm Int. J. Med. 2020, 113, 391–392. [Google Scholar] [CrossRef] [PubMed]
- Telford, C.T.; Onwubiko, U.; Holland, D.P.; Turner, K.; Prieto, J.; Smith, S.; Yoon, J.; Brown, W.; Chamberlain, A.; Gandhi, N.; et al. Preventing COVID-19 Outbreaks in Long-Term Care Facilities Through Preemptive Testing of Residents and Staff Members—Fulton County, Georgia, March–May 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1296–1299. [Google Scholar] [CrossRef]
- Pitkälä, K.H. COVID-19 has hit nursing homes hard. Eur. Geriatr. Med. 2020, 11, 889–891. [Google Scholar] [CrossRef]
- Forma, L.; Aaltonen, M.; Pulkki, J. COVID-19 and Clients of Long-Term Care in Finland—Impact and Measures to Control the Virus. 2020. Available online: https://ltccovid.org/country-reports-on-covid-19-and-long-term-care/ (accessed on 2 November 2022).
- ECDC Public Health Emergency Team; Danis, K.; Fonteneau, L.; Georges, S.; Daniau, C.; Bernard-Stoecklin, S.; Domegan, L.; O’Donnell, J.; Hauge, S.H.; Dequeker, S.; et al. High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA, May 2020. Eurosurveillance 2020, 25, 2000956. [Google Scholar] [CrossRef]
- Cella, P.; Voglino, G.; Barberis, I.; Alagna, E.; Alessandroni, C.; Cuda, A.; D’aloisio, F.; Dallagiacoma, G.; De Nitto, S.; Di Gaspare, F.; et al. Resources for assessing parents’ vaccine hes-itancy: A systematic review of the literature. J. Prev. Med. Hyg. 2020, 61, E340–E373. [Google Scholar] [CrossRef]
- Heyerdahl, L.W.; Dielen, S.; Nguyen, T.; Van Riet, C.; Kattumana, T.; Simas, C.; Vandaele, N.; Vandamme, A.-M.; Vandermeulen, C.; Giles-Vernick, T.; et al. Doubt at the core: Unspoken vaccine hesitancy among healthcare workers. Lancet Reg. Health Eur. 2022, 12, 100289. [Google Scholar] [CrossRef]
- Sonawane, K.; Troisi, C.L.; Deshmukh, A.A. COVID-19 vaccination in the UK: Addressing vaccine hesitancy. Lancet Reg. Health Eur. 2021, 1, 100016. [Google Scholar] [CrossRef]
- Kerr, J.; Freeman, A.; Marteau, T.; van der Linden, S. Effect of Information about COVID-19 Vaccine Effectiveness and Side Effects on Behavioural Intentions: Two Online Experiments. Vaccines 2021, 9, 379. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.J.; Lee, B.; Nugent, K. COVID-19 Vaccination Hesitancy among Healthcare Workers—A Review. Vaccines 2022, 10, 948. [Google Scholar] [CrossRef] [PubMed]
- Mejri, N.; Berrazega, Y.; Ouertani, E.; Rachdi, H.; Bohli, M.; Kochbati, L.; Boussen, H. Understanding COVID-19 vaccine hesitancy and resistance: Another challenge in cancer patients. Support. Care Cancer 2022, 30, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Kontio, M.; Skogberg, N.; Sivelä, J.; Nohynek, H.; Salo, H.; Mäntymaa, P.; Helve, O. Koronarokotuskattavuuteen vaikuttavat tekijät. 2021. Available online: https://www.julkari.fi/handle/10024/143238 (accessed on 2 November 2022). (In Finnish).
- Li, M.; Luo, Y.; Watson, R.; Zheng, Y.; Ren, J.; Tang, J.; Chen, Y. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: A rapid systematic review. Postgrad. Med. J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef]
- Harrison, J.; Berry, S.; Mor, V.; Gifford, D. “Somebody Like Me”: Understanding COVID-19 Vaccine Hesitancy among Staff in Skilled Nursing Facilities. J. Am. Med. Dir. Assoc. 2021, 22, 1133–1137. [Google Scholar] [CrossRef]
- Unroe, K.T.; Evans, R.; Weaver, L.; Rusyniak, D.; Blackburn, J. Willingness of Long-Term Care Staff to Receive a COVID-19 Vaccine: A Single State Survey. J. Am. Geriatr. Soc. 2021, 69, 593–599. [Google Scholar] [CrossRef]
- Gogoi, M.; Wobi, F.; Qureshi, I.; Al-Oraibi, A.; Hassan, O.; Chaloner, J.; Nellums, L.B.; Pareek, M. UK-REACH Collaborative Group “The vaccination is positive; I don’t think it’s the panacea”: A qualitative study on COVID-19 vaccine attitudes among ethnically diverse healthcare workers in the United Kingdom. PLoS ONE 2022, 17, e0273687. [Google Scholar] [CrossRef]
- Yilmaz, S.; Çolak, F.; Yilmaz, E.; Ak, R.; Hökenek, N.M.; Altıntaş, M.M. Vaccine Hesitancy of Health-Care Workers: Another Challenge in the Fight Against COVID-19 in Istanbul. Disaster Med. Public Health Prep. 2021, 16, 1134–1140. [Google Scholar] [CrossRef]
- de Bruin, M.; E Suk, J.; Baggio, M.; Blomquist, S.E.; Falcon, M.; Forjaz, M.J.; Godoy-Ramirez, K.; Leurs, M.; Rodriguez-Blazquez, C.; Romay-Barja, M.; et al. Behavioural insights and the evolving COVID-19 pandemic. Eurosurveillance 2022, 27, 2100615. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.E.; Prentice, J.A.; Saad-Roy, C.M.; Yang, L.; Grenfell, B.T.; Levin, S.A.; Laxminarayan, R. Economic and Behavioral Influencers of Vaccination and Antimicrobial Use. Front. Public Health 2020, 8, 614113. [Google Scholar] [CrossRef] [PubMed]
- Tentori, K.; Pighin, S.; Giovanazzi, G.; Grignolio, A.; Timberlake, B.; Ferro, A. Nudging COVID-19 Vaccine Uptake by Changing the Default: A Randomized Controlled Trial. Med. Decis. Mak. 2022, 42, 837–841. [Google Scholar] [CrossRef]
- Obach, D.; Solastie, A.; Liedes, O.; Vara, S.; Krzyżewska-Dudek, E.; Brinkmann, L.; Haveri, A.; Hammer, C.C.; Dub, T.; Meri, S.; et al. Impaired immunity and high attack rates caused by SARS-CoV-2 variants among vaccinated long-term care facility residents. Immunity, Inflamm. Dis. 2022, 10, e679. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Williams, L.; Gallant, A.J.; Rasmussen, S.; Nicholls, L.A.B.; Cogan, N.; Deakin, K.; Young, D.; Flowers, P. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: Outlining evidence-based and theoretically informed future intervention content. Br. J. Health Psychol. 2020, 25, 1039–1054. [Google Scholar] [CrossRef]
- Lohiniva, A.-L.; Toura, S.; Arifulla, D.; Ollgren, J.; Lyytikäinen, O. Exploring behavioural factors influencing COVID-19-specific infection prevention and control measures in Finland: A mixed-methods study, December 2020 to March 2021. Eurosurveillance 2022, 27, 2100915. [Google Scholar] [CrossRef]
- Benoot, C.; Hannes, K.; Bilsen, J. The use of purposeful sampling in a qualitative evidence synthesis: A worked example on sexual adjustment to a cancer trajectory. BMC Med. Res. Methodol. 2016, 16, 21. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Thomas, D.R. A general inductive approach for analyzing qualitative evaluation data. Am. J. Eval. 2006, 27, 237–246. [Google Scholar] [CrossRef]
- Brown, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2008, 3, 77–101. [Google Scholar]
- Tangcharoensathien, V.; Calleja, N.; Nguyen, T.; Purnat, T.; D’Agostino, M.; Garcia-Saiso, S.; Landry, M.; Rashidian, A.; Hamilton, C.; Abdallah, A.; et al. Framework for Managing the COVID-19 Infodemic: Methods and Results of an Online, Crowdsourced WHO Technical Consultation. J. Med. Internet Res. 2020, 22, e19659. [Google Scholar] [CrossRef] [PubMed]
- Klerings, I.; Weinhandl, A.S.; Thaler, K.J. Information overload in healthcare: Too much of a good thing? Z. Evidenz Fortbild. Qual. Gesundh. 2015, 109, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Khan, A.N. Investigating the Impacts of Information Overload on Psychological Well-being of Healthcare Professionals: Role of COVID-19 Stressor. Inq. J. Health Care Organ. Provis. Financ. 2022, 59, 469580221109677. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.; Walton, G. Information overload within the health care system: A literature review. Health Inf. Libr. J. 2004, 21, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Smith, A. Information Overload, Wellbeing and COVID-19: A Survey in China. Behav. Sci. 2021, 11, 62. [Google Scholar] [CrossRef]
- Pacutova, V.; Geckova, A.M.; Kizek, P.; de Winter, A.F.; Reijneveld, S.A. The Impact of Pandemic Management on the Quality of Life of Slovak Dentists. Int. J. Environ. Res. Public Health 2021, 18, 5484. [Google Scholar] [CrossRef]
- Zhang, N.; Xu, D.; Li, J.; Xu, Z. Effects of role overload, work engagement and perceived organisational support on nurses’ job performance during the COVID-19 pandemic. J. Nurs. Manag. 2022, 30, 901–912. [Google Scholar] [CrossRef]
- Poonia, S.K.; Rajasekaran, K. Information Overload: A Method to Share Updates among Frontline Staff during the COVID-19 Pandemic. Otolaryngol. Neck Surg. 2020, 163, 60–62. [Google Scholar] [CrossRef]
- Fernandez, R.; Green, H.; Hobbs, C.; Loveday, C.; Almasi, E.; Middleton, R.; Halcomb, E.J.; Moxham, L. Adaption of the Cancer Information Overload Scale for pandemics and assessment of infodemic levels among nurses and midwives. Int. J. Nurs. Pract. 2022, 29, e13055. [Google Scholar] [CrossRef]
- Fuller, A.; Hancox, J.; Vedhara, K.; Card, T.; Mallen, C.; Van-Tam, J.S.N.; Abhishek, A. Barriers and facilitators to vaccination uptake against COVID-19, influenza, and pneumococcal pneumonia in immunosuppressed adults with immune-mediated inflammatory diseases: A qualitative interview study during the COVID-19 pandemic. PLoS ONE 2022, 17, e0267769. [Google Scholar] [CrossRef]
- Ackah, M.; Ameyaw, L.; Salifu, M.G.; Asubonteng, D.P.A.; Yeboah, C.O.; Annor, E.N.; Ankapong, E.A.K.; Boakye, H. COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0268711. [Google Scholar] [CrossRef]
- Desye, B. Prevalence and Determinants of COVID-19 Vaccine Acceptance Among Healthcare Workers: A Systematic Review. Front. Public Health 2022, 10, 941206. [Google Scholar] [CrossRef]
- Crawshaw, J.; Konnyu, K.; Castillo, G.; van Allen, Z.; Grimshaw, J.; Presseau, J. Behavioural determinants of COVID-19 vaccination acceptance among healthcare workers: A rapid review. Public Health 2022, 210, 123–133. [Google Scholar] [CrossRef]
- Davis, C.J.; Golding, M.; McKay, R. Efficacy information influences intention to take COVID-19 vaccine. Br. J. Health Psychol. 2021, 27, 300–319. [Google Scholar] [CrossRef]
- Chong, D.; Drucman, J.N. Framing theory. Annu. Rev. Polit. Sci. 2007, 10, 103–126. [Google Scholar] [CrossRef]
- Palm, R.; Bolsen, T.; Kingsland, J.T. The Effect of Frames on COVID-19 Vaccine Resistance. Front. Political Sci. 2021, 3, 661257. [Google Scholar] [CrossRef]
- Purvis, R.S.; Moore, R.; Willis, D.E.; Hallgren, E.; McElfish, P.A. Factors influencing COVID-19 vaccine decision-making among hesitant adopters in the United States. Hum. Vaccines Immunother. 2022, 18, 2114701. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Zhang, Y.; Chen, L.; Yu, L.; Li, L.; Wang, Q. The influence of social network on COVID-19 vaccine hesitancy among healthcare workers: A cross-sectional survey in Chongqing, China. Hum. Vaccines Immunother. 2021, 17, 5048–5062. [Google Scholar] [CrossRef] [PubMed]
- Daugherty, J.D.; Blake, S.C.; Grosholz, J.; Omer, S.B.; Polivka-West, L.; Howard, D.H. Influenza vaccination rates and beliefs about vaccination among nursing home employees. Am. J. Infect. Control. 2015, 43, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Konstantinou, P.; Georgiou, K.; Kumar, N.; Kyprianidou, M.; Nicolaides, C.; Karekla, M.; Kassianos, A. Transmission of Vaccination Attitudes and Uptake Based on Social Contagion Theory: A Scoping Review. Vaccines 2021, 9, 607. [Google Scholar] [CrossRef] [PubMed]
- Al-Metwali, B.Z.; Al-Jumaili, A.A.; Al-Alag, Z.A.; Sorofman, B. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J. Eval. Clin. Pract. 2021, 27, 1112–1122. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, D.; Malli, F.; Raptis, D.; Papathanasiou, I.; Fradelos, E.; Daniil, Z.; Rachiotis, G.; Gourgoulianis, K. Assessment of Knowledge, Attitudes, and Practices towards New Coronavirus (SARS-CoV-2) of Health Care Professionals in Greece before the Outbreak Period. Int. J. Environ. Res. Public Health 2020, 17, 4925. [Google Scholar] [CrossRef]
- Woolf, K.; McManus, I.C.; A Martin, C.; Nellums, L.B.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; Gogoi, M.; Wobi, F.; Al-Oraibi, A.; et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. Lancet Reg. Health Eur. 2021, 9, 100180. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 vaccine acceptance of healthcare providers in a tertiary Pediatric hospital. Hum. Vaccines Immunother. 2021, 17, 2946–2950. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. [Google Scholar] [CrossRef]
- Anderson, L.; Bell, H.G.; Gilbert, M.; E Davidson, J.; Winter, C.; Barratt, M.J.; Win, B.; Painter, J.L.; Menone, C.; Sayegh, J.; et al. Using Social Listening Data to Monitor Misuse and Nonmedical Use of Bupropion: A Content Analysis. JMIR Public Health Surveill. 2017, 3, e6. [Google Scholar] [CrossRef]
- Berry, S.D.; Johnson, K.S.; Myles, L.; Herndon, L.; Montoya, A.; Fashaw, S.; Gifford, D. Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J. Am. Geriatr. Soc. 2021, 69, 1140–1146. [Google Scholar] [CrossRef]
- Dzieciolowska, S.; Hamel, D.; Gadio, S.; Dionne, M.; Gagnon, D.; Robitaille, L.; Cook, E.; Caron, I.; Talib, A.; Parkes, L.; et al. COVID-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am. J. Infect. Control. 2021, 49, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Fares, S.; Elmnyer, M.M.; Mohamed, S.S.; Elsayed, R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J. Prim. Care Community Health 2021, 12, 21501327211013303. [Google Scholar] [CrossRef]
- Tabong, P.T.; Mensah, K.O.; Asampong, E. Preparation for COVID-19 vaccines rollout: Interventions to increase trust, acceptability, and uptake in West African countries. Int. J. Health Plan. Manag. 2022, 37, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Andreas, M.; Iannizzi, C.; Bohndorf, E.; Monsef, I.; Piechotta, V.; Meerpohl, J.J.; Skoetz, N. Interventions to increase COVID-19 vaccine uptake: A scoping review. Cochrane Database Syst. Rev. 2022, 8, CD015270. [Google Scholar] [CrossRef] [PubMed]
- Bokemper, S.E.; Huber, G.A.; Gerber, A.S.; James, E.K.; Omer, S.B. Timing of COVID-19 vaccine approval and endorsement by public figures. Vaccine 2021, 39, 825–829. [Google Scholar] [CrossRef] [PubMed]
- Ojikutu, B.O.; Stephenson, K.E.; Mayer, K.H.; Emmons, K.M. Building Trust in COVID-19 Vaccines and Beyond Through Authentic Community Investment. Am. J. Public Health 2021, 111, 366–368. [Google Scholar] [CrossRef]
- Rutten, L.J.F.; Zhu, X.; Leppin, A.L.; Ridgeway, J.L.; Swift, M.D.; Griffin, J.M.; Sauver, J.L.S.; Virk, A.; Jacobson, R.M. Evidence-Based Strategies for Clinical Organizations to Address COVID-19 Vaccine Hesitancy. Mayo Clin. Proc. 2021, 96, 699–707. [Google Scholar] [CrossRef]
- Hawryluck, L.; Lapinsky, S.E.; Stewart, T.E. Clinical review: SARS—Lessons in disaster management. Crit. Care. 2005, 9, 384–389. [Google Scholar] [CrossRef]
- Opel, D.J.; Salmon, D.A.; Marcuse, E.K. Building Trust to Achieve Confidence in COVID-19 Vaccines. JAMA Netw. Open 2020, 3, e2025672. [Google Scholar] [CrossRef]
- Latkin, C.A.; Edwards, C.; Davey-Rothwell, M.A.; Tobin, K.E. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict. Behav. 2017, 73, 133–136. [Google Scholar] [CrossRef]
- Anand, P.; Stahel, V.P. The safety of COVID-19 mRNA vaccines: A review. Patient Saf. Surg. 2021, 15, 20. [Google Scholar] [CrossRef] [PubMed]
- Bechini, A.; Lorini, C.; Zanobini, P.; Tacconi, F.M.; Boccalini, S.; Grazzini, M.; Bonanni, P.; Bonaccorsi, G. Utility of Healthcare System-Based Interventions in Improving the Uptake of Influenza Vaccination in Healthcare Workers at Long-Term Care Facilities: A Systematic Review. Vaccines 2020, 8, 165. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Social Affairs and Health Finland. Communicable Diseases Act (1227/2016); Finnish Government: Helsinki, Finnish, 2016. Available online: https://www.finlex.fi/en/laki/kaannokset/2016/en20161227.pdf (accessed on 2 November 2022).
- Hammer, C.C.; Lyytikäinen, O.; Arifulla, D.; Toura, S.; Nohynek, H. High influenza vaccination coverage among healthcare workers in acute care hospitals in Finland, seasons 2017/18, 2018/19 and 2019/20. Eurosurveillance 2022, 27, 2100411. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lohiniva, A.-L.; Hussein, I.; Lehtinen, J.-M.; Sivelä, J.; Hyökki, S.; Nohynek, H.; Nuorti, P.; Lyytikäinen, O. Qualitative Insights into Vaccine Uptake of Nursing Staff in Long-Term Care Facilities in Finland. Vaccines 2023, 11, 530. https://doi.org/10.3390/vaccines11030530
Lohiniva A-L, Hussein I, Lehtinen J-M, Sivelä J, Hyökki S, Nohynek H, Nuorti P, Lyytikäinen O. Qualitative Insights into Vaccine Uptake of Nursing Staff in Long-Term Care Facilities in Finland. Vaccines. 2023; 11(3):530. https://doi.org/10.3390/vaccines11030530
Chicago/Turabian StyleLohiniva, Anna-Leena, Idil Hussein, Jaana-Marija Lehtinen, Jonas Sivelä, Suvi Hyökki, Hanna Nohynek, Pekka Nuorti, and Outi Lyytikäinen. 2023. "Qualitative Insights into Vaccine Uptake of Nursing Staff in Long-Term Care Facilities in Finland" Vaccines 11, no. 3: 530. https://doi.org/10.3390/vaccines11030530
APA StyleLohiniva, A.-L., Hussein, I., Lehtinen, J.-M., Sivelä, J., Hyökki, S., Nohynek, H., Nuorti, P., & Lyytikäinen, O. (2023). Qualitative Insights into Vaccine Uptake of Nursing Staff in Long-Term Care Facilities in Finland. Vaccines, 11(3), 530. https://doi.org/10.3390/vaccines11030530




