Cognitive and Behavioral Factors Predicting the Decision to Vaccinate against COVID-19 in Clinical Psychiatric Population—A Cross-Sectional Survey
Abstract
1. Introduction
1.1. Psychiatric Population as a Highly Vulnerable Category for COVID-19 Infection
1.2. Heterogeneity of Vaccination Determinants
1.2.1. Cognitive Factors: Risk Perception and Uncertainty in Health Decisions
1.2.2. Behavioral Factors: Vaccination History, Social Media Use, and Preventive Behaviors
1.3. Current Study
Diagnosis Severity, Comorbidities, and Vaccination Decision
2. Materials and Methods
2.1. Participants
2.2. Design and Procedure
2.3. Instruments and Measurements
2.4. Data Analysis
3. Results
3.1. Demographic Data
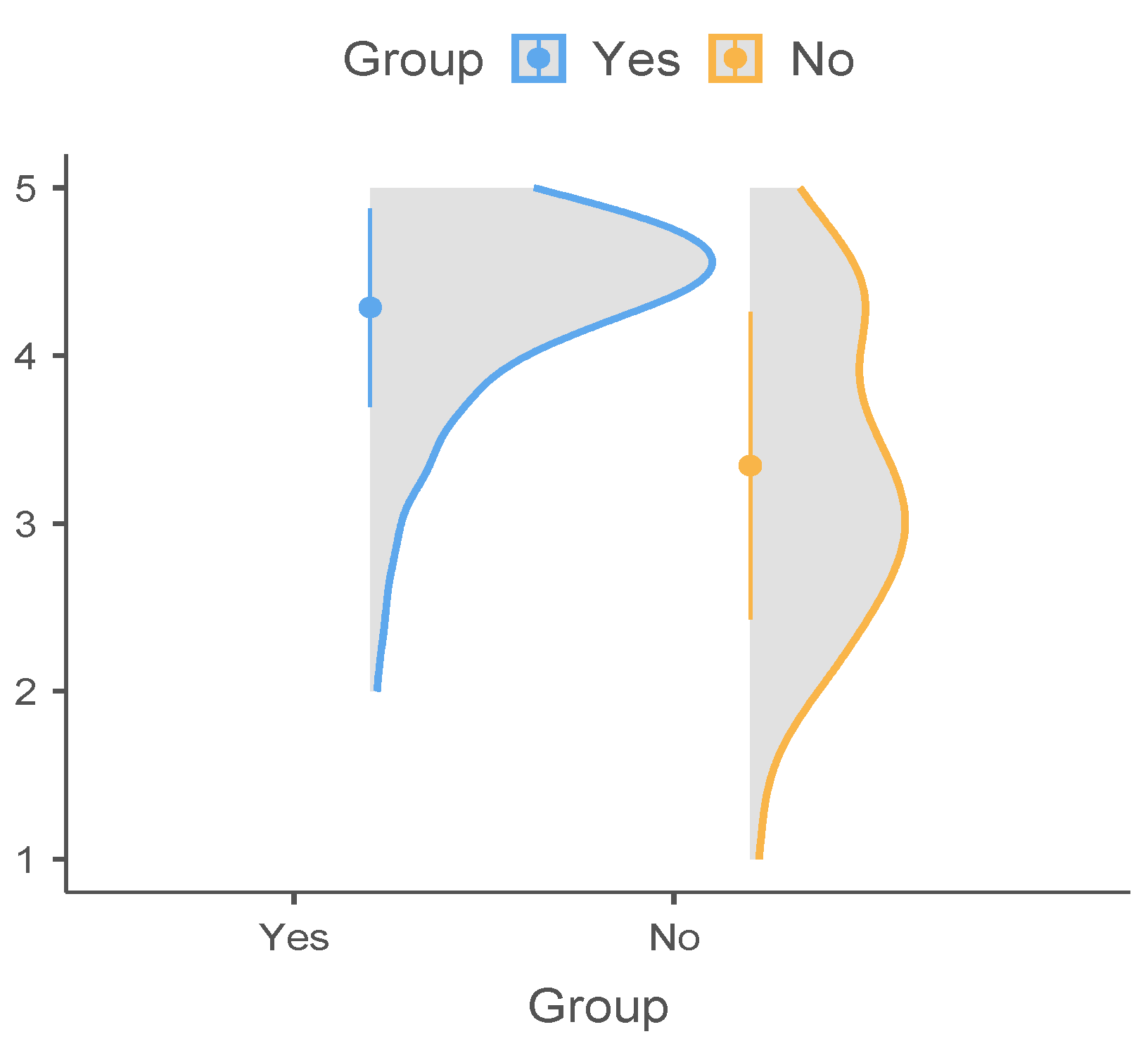
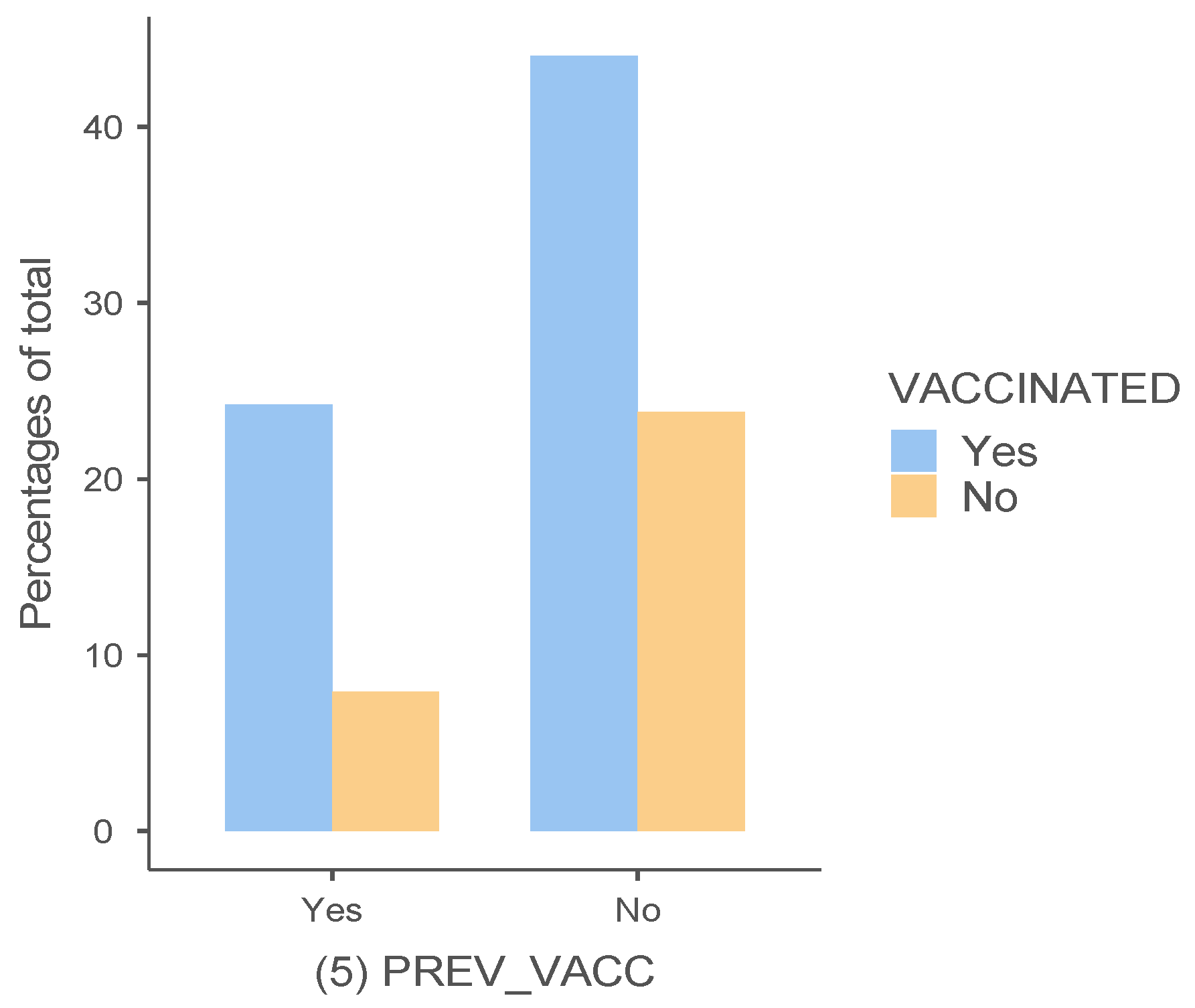
3.2. Factors Associated with the Vaccination Decision
3.3. Regression Model for Prediction of Decision to Vaccinate
4. Discussion
4.1. Psychiatric Patients vs. Normal Population in the Decision to Vaccinate against COVID-19
4.2. Cognitive Predictors: Risk Perception
4.3. Cognitive Predictors: Perceived Personal Vulnerability, Perceived Uncertainty, and Trust in One’s Own Decision to Vaccinate
4.4. Behavioral Predictors: Former Voluntary Vaccination
4.5. Behavioral Predictors: Social Media Engagement
4.6. Behavioral Predictors: Preventive Behaviors
4.7. Vaccine Coverage—Country-Specific Differences
4.8. Psychiatric Population Peculiarities
4.9. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Behav. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Romania: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data|WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Available online: https://covid19.who.int/region/euro/country/ro/ (accessed on 6 January 2023).
- Blix, I.; Birkeland, M.S.; Thoresen, S. Worry and mental health in the COVID-19 pandemic: Vulnerability factors in the general Norwegian population. BMC Public Health 2021, 21, 928. [Google Scholar] [CrossRef] [PubMed]
- Valdés-Florido, M.J.; López-Díaz, Á.; Palermo-Zeballos, F.J.; Martínez-Molina, I.; Martín-Gil, V.E.; Crespo-Facorro, B.; Ruiz-Veguilla, M. Reactive psychoses in the context of the COVID-19 pandemic: Clinical perspectives from a case series. Rev. Psiquiatr. Salud Ment. 2020, 13, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Mazereel, V.; Van Assche, K.; Detraux, J.; De Hert, M. COVID-19 vaccination for people with severe mental illness: Why, what, and how? Lancet Psychiatry 2021, 8, 444–450. [Google Scholar] [CrossRef]
- Lee, S.W.; Yang, J.M.; Moon, S.Y.; Yoo, I.K.; Ha, E.K.; Kim, S.Y.; Park, U.M.; Choi, S.; Lee, S.-H.; Ahn, Y.M.; et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: A nationwide cohort study. Lancet Psychiatry 2020, 7, 1025–1031. [Google Scholar] [CrossRef]
- Maripuu, M.; Bendix, M.; Öhlund, L.; Widerström, M.; Werneke, U. Death Associated With Coronavirus (COVID-19) Infection in Individuals With Severe Mental Disorders in Sweden During the Early Months of the Outbreak-An Exploratory Cross-Sectional Analysis of a Population-Based Register Study. Front. Psychiatry 2020, 11, 609579. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Xu, R.; Volkow, N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States. World Psychiatry 2021, 20, 124–130. [Google Scholar] [CrossRef]
- Yang, H.; Chen, W.; Hu, Y.; Chen, Y.; Zeng, Y.; Sun, Y.; Ying, Z.; He, J.; Qu, Y.; Lu, D.; et al. Pre-pandemic psychiatric disorders and risk of COVID-19: A UK Biobank cohort analysis. Lancet Healthy Longev. 2020, 1, e69–e79. [Google Scholar] [CrossRef]
- Nemani, K.; Li, C.; Olfson, M.; Blessing, E.M.; Razavian, N.; Chen, J.; Petkova, E.; Goff, D.C. Association of Psychiatric Disorders With Mortality Among Patients With COVID-19. JAMA Psychiatry 2021, 78, 380–386. [Google Scholar] [CrossRef]
- Vinogradova, Y.; Coupland, C.; Hippisley-Cox, J.; Whyte, S.; Penny, C. Effects of severe mental illness on survival of people with diabetes. Br. J. Psychiatry 2010, 197, 272–277. [Google Scholar] [CrossRef]
- Walker, E.R.; McGee, R.E.; Druss, B.G. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 2015, 72, 334–341. [Google Scholar] [CrossRef]
- De Hert, M.; Mazereel, V.; Detraux, J.; Van Assche, K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry 2021, 20, 54–55. [Google Scholar] [CrossRef] [PubMed]
- Bechara, A.; Martin, E.M. Impaired decision making related to working memory deficits in individuals with substance addictions. Neuropsychology 2004, 18, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Cáceda, R.; Nemeroff, C.B.; Harvey, P.D. Toward an understanding of decision making in severe mental illness. J. Neuropsychiatry Clin. Neurosci. 2014, 26, 196–213. [Google Scholar] [CrossRef] [PubMed]
- Lesh, T.A.; Niendam, T.A.; Minzenberg, M.J.; Carter, C.S. Cognitive control deficits in schizophrenia: Mechanisms and meaning. Neuropsychopharmacology 2011, 36, 316–338. [Google Scholar] [CrossRef] [PubMed]
- Simon, H.A. A Behavioral Model of Rational Choice. Q. J. Econ. 1955, 69, 99. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Belief in the law of small numbers. Psychol. Bull. 1971, 76, 105–110. [Google Scholar] [CrossRef]
- Borges, J.; Byrne, M. Investigating COVID-19 risk perception and preventive behaviours in third-level students in Ireland. Acta Psychol. (Amst.) 2022, 224, 103535. [Google Scholar] [CrossRef] [PubMed]
- Lu, P.; Kong, D.; Shelley, M. Risk Perception, Preventive Behavior, and Medical Care Avoidance among American Older Adults During the COVID-19 Pandemic. J. Aging Health 2021, 33, 577–584. [Google Scholar] [CrossRef]
- Trifiletti, E.; Shamloo, S.E.; Faccini, M.; Zaka, A. Psychological predictors of protective behaviours during the Covid-19 pandemic: Theory of planned behaviour and risk perception. J. Community Appl. Soc. Psychol. 2022, 32, 382–397. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, R.; Klein, W.M. Risk perceptions and health behavior. Curr. Opin. Psychol. 2015, 5, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Loewenstein, G.F.; Weber, E.U.; Hsee, C.K.; Welch, N. Risk as feelings. Psychol. Bull. 2001, 127, 267–286. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef]
- Savadori, L.; Lauriola, M. Risk Perception and Protective Behaviors During the Rise of the COVID-19 Outbreak in Italy. Front. Psychol. 2020, 11, 577331. [Google Scholar] [CrossRef]
- Sheeran, P.; Harris, P.R.; Epton, T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol. Bull. 2014, 140, 511–543. [Google Scholar] [CrossRef] [PubMed]
- Taber, J.M.; Klein, W.M.P. The role of conviction in personal disease risk perceptions: What can we learn from research on attitude strength? Soc. Personal. Psychol. Compass 2016, 10, 202–218. [Google Scholar] [CrossRef] [PubMed]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef] [PubMed]
- Attema, A.E.; L’Haridon, O.; Raude, J.; Seror, V. COCONEL Group Beliefs and Risk Perceptions About COVID-19: Evidence from Two Successive French Representative Surveys during Lockdown. Front. Psychol. 2021, 12, 619145. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Shahrabani, S.; Benzion, U.; Yom Din, G. Factors affecting nurses’ decision to get the flu vaccine. Eur. J. Health Econ. 2009, 10, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Brewer, N.T.; Brocard, P.; Davies, P.; Gaissmaier, W.; Haase, N.; Leask, J.; Renkewitz, F.; Renner, B.; Reyna, V.F.; et al. Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine 2012, 30, 3727–3733. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccin. Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Schuchard, R.J.; Crooks, A.T. Examining emergent communities and social bots within the polarized online vaccination debate in twitter. Soc. Media Soc. 2019, 5, 205630511986546. [Google Scholar] [CrossRef]
- Wang, Y.; McKee, M.; Torbica, A.; Stuckler, D. Systematic Literature Review on the Spread of Health-related Misinformation on Social Media. Soc. Sci. Med. 2019, 240, 112552. [Google Scholar] [CrossRef] [PubMed]
- Zeballos Rivas, D.R.; Lopez Jaldin, M.L.; Nina Canaviri, B.; Portugal Escalante, L.F.; Alanes Fernández, A.M.C.; Aguilar Ticona, J.P. Social media exposure, risk perception, preventive behaviors and attitudes during the COVID-19 epidemic in La Paz, Bolivia: A cross sectional study. PLoS ONE 2021, 16, e0245859. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Behavioral Intention to Receive a COVID-19 Vaccination Among Chinese Factory Workers: Cross-sectional Online Survey. J. Med. Internet Res. 2021, 23, e24673. [Google Scholar] [CrossRef]
- Latkin, C.; Dayton, L.A.; Yi, G.; Konstantopoulos, A.; Park, J.; Maulsby, C.; Kong, X. COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine 2021, 39, 2288–2294. [Google Scholar] [CrossRef]
- Hofmann, F.; Ferracin, C.; Marsh, G.; Dumas, R. Influenza vaccination of healthcare workers: A literature review of attitudes and beliefs. Infection 2006, 34, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Nexøe, J.; Kragstrup, J.; Søgaard, J. Decision on influenza vaccination among the elderly. A questionnaire study based on the Health Belief Model and the Multidimensional Locus of Control Theory. Scand. J. Prim. Health Care 1999, 17, 105–110. [Google Scholar] [CrossRef]
- Seale, H.; Heywood, A.E.; Leask, J.; Sheel, M.; Durrheim, D.N.; Bolsewicz, K.; Kaur, R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect. Dis. 2021, 21, 120. [Google Scholar] [CrossRef]
- Graffigna, G.; Palamenghi, L.; Boccia, S.; Barello, S. Relationship between Citizens’ Health Engagement and Intention to Take the COVID-19 Vaccine in Italy: A Mediation Analysis. Vaccines 2020, 8, 576. [Google Scholar] [CrossRef] [PubMed]
- Cohen, B.; Ferng, Y.; Wong-McLoughlin, J.; Jia, H.; Morse, S.S.; Larson, E.L. Predictors of flu vaccination among urban Hispanic children and adults. J. Epidemiol. Community Health 2012, 66, 204–209. [Google Scholar] [CrossRef]
- Kee, S.Y.; Lee, J.S.; Cheong, H.J.; Chun, B.C.; Song, J.Y.; Choi, W.S.; Jo, Y.M.; Seo, Y.B.; Kim, W.J. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J. Infect. 2007, 55, 273–281. [Google Scholar] [CrossRef]
- Cevallos, M.; Egger, M. STROBE (STrengthening the Reporting of Observational studies in Epidemiology). In Guidelines for Reporting Health Research: A User’s Manual; Moher, D., Altman, D.G., Schulz, K.F., Simera, I., Wager, E., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2014; pp. 169–179. [Google Scholar] [CrossRef]
- Lakens, D. Equivalence Tests: A Practical Primer for t Tests, Correlations, and Meta-Analyses. Soc. Psychol. Personal. Sci. 2017, 8, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Lakens, D.; Scheel, A.M.; Isager, P.M. Equivalence testing for psychological research: A tutorial. Adv. Methods Pract. Psychol. Sci. 2018, 1, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Bhuiya, T.; Klares Iii, R.; Conte, M.A.; Cervia, J.S. Predictors of misperceptions, risk perceptions, and personal risk perceptions about COVID-19 by country, education and income. J. Investig. Med. 2021, 69, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Reyna, V.F.; Nelson, W.L.; Han, P.K.; Dieckmann, N.F. How numeracy influences risk comprehension and medical decision making. Psychol. Bull. 2009, 135, 943–973. [Google Scholar] [CrossRef] [PubMed]
- Strauss, G.P.; Waltz, J.A.; Gold, J.M. A review of reward processing and motivational impairment in schizophrenia. Schizophr. Bull. 2014, 40 (Suppl. 2), S107–S116. [Google Scholar] [CrossRef] [PubMed]
- Benke, T.; Marksteiner, J.; Ruepp, B.; Weiss, E.M.; Zamarian, L. Decision Making under Risk in Patients Suffering from Schizophrenia or Depression. Brain Sci. 2021, 11, 1178. [Google Scholar] [CrossRef]
- Hay, J.L.; McCaul, K.D.; Magnan, R.E. Does worry about breast cancer predict screening behaviors? A meta-analysis of the prospective evidence. Prev. Med. 2006, 42, 401–408. [Google Scholar] [CrossRef]
- Maddux, J.E.; Rogers, R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. J. Exp. Soc. Psychol. 1983, 19, 469–479. [Google Scholar] [CrossRef]
- Rogers, R.W. A protection motivation theory of fear appeals and attitude change1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef] [PubMed]
- Gillman, A.S.; Scharnetzki, L.; Boyd, P.; Ferrer, R.A.; Klein, W.M.P.; Han, P.K.J. Perceptions and tolerance of uncertainty: Relationship to trust in COVID-19 health information and vaccine hesitancy. J. Behav. Med. 2022, 1–14. [Google Scholar] [CrossRef]
- Brun, C.; Akinyemi, A.; Houtin, L.; Zerhouni, O.; Monvoisin, R.; Pinsault, N. Intolerance of Uncertainty and Attitudes towards Vaccination Impact Vaccinal Decision While Perceived Uncertainty Does Not. Vaccines 2022, 10, 1742. [Google Scholar] [CrossRef]
- Allington, D.; Duffy, B.; Wessely, S.; Dhavan, N.; Rubin, J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol. Med. 2021, 51, 1763–1769. [Google Scholar] [CrossRef]
- Basch, C.H.; Zybert, P.; Reeves, R.; Basch, C.E. What do popular YouTubeTM videos say about vaccines? Child Care Health Dev. 2017, 43, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Global Daily Social Media Usage 2022|Statista. Available online: https://www.statista.com/statistics/433871/daily-social-media-usage-worldwide/ (accessed on 5 February 2023).
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Parsons Leigh, J.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef]
- Mazereel, V.; Vanbrabant, T.; Desplenter, F.; De Hert, M. COVID-19 vaccine uptake in patients with psychiatric disorders admitted to or residing in a university psychiatric hospital. Lancet Psychiatry 2021, 8, 860–861. [Google Scholar] [CrossRef]
- Jefsen, O.H.; Kølbæk, P.; Gil, Y.; Speed, M.; Dinesen, P.T.; Sønderskov, K.M.; Østergaard, S.D. COVID-19 vaccine willingness amongst patients with mental illness compared with the general population. Acta Neuropsychiatr. 2021, 33, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Zhao, Z.; Teng, Z.; Xu, B.; Wang, X.; Guo, J.; Huang, J.; Wu, H. COVID-19 vaccination coverage among patients with psychiatric disorders in China during the pandemic: A cross-sectional study. BMC Psychiatry 2022, 22, 659. [Google Scholar] [CrossRef]
- Michie, S. Encouraging vaccine uptake: Lessons from behavioural science. Nat. Rev. Immunol. 2022, 22, 527–528. [Google Scholar] [CrossRef] [PubMed]

| Cross Table for Dependent: Vaccinated | ||||
|---|---|---|---|---|
| N | Yes (N = 172) | No (N = 80) | Statistical Test | |
| SMOKER: No | 250 | 0.6 107/170 (62.94%) | 0.7 57/80 (71.25%) | X12 = 1.66, p = 0.202 |
| AGE | 252 | X22 = 5.85, p = 0.052 | ||
| 18–39 years | 0.1 14/172 (8.14%) | 0.2 14/80 (17.5%) | ||
| 40–64 years | 0.6 107/172 (62.21%) | 0.5 40/80 (50%) | ||
| 65 and above 65 years | 0.3 51/172 (29.65%) | 0.3 26/80 (32.5%) | ||
| SEX: Female | 252 | 0.6 107/172 (62.21%) | 0.7 53/80 (66.25%) | X12 = 0.38, p = 0.542 |
| DIAGNOSTIC | 238 | X42 = 3.12, p = 0.542 | ||
| Affective disorder | 0.7 111/160 (69.38%) | 0.6 47/78 (60.28%) | ||
| Psychosis | 0.1 19/160 (11.88%) | 0.2 14/78 (17.95%) | ||
| Dementia | 0.0 7/160 (4.38%) | 0.1 6/78 (7.69%) | ||
| Addiction | 0.1 10/160 (6.25%) | 0.1 6/78 (7.69%) | ||
| Personality disorder | 0.1 10/160 (6.25%) | 0.1 5/78 (6.41%) | ||
| MARITAL STATUS: No | 152 | 0.4 68/172 (39.53%) | 0.4 34/80 (42.5%) | X12 = 0.20, p = 0.662 |
| STUDIES | 252 | |||
| Primary | 0.2 35/172 (20.35%) | 0.5 38/80 (47.5%) | ||
| Secondary | 0.6 102/172 (59.3%) | 0.3 28/80 (35%) | ||
| Higher | 0.2 35/172 (20.35%) | 0.2 14/80 (17.5%) | ||
| SOCIAL MEDIA | 252 | X42 = 0.94, p = 0.922 | ||
| 0 h | 0.4 74/172 (43.02%) | 0.4 30/80 (37.5%) | ||
| Under 1 h | 0.4 64/172 (37.21%) | 0.4 32/80 (40%) | ||
| 1–3 h | 0.2 31/172 (18.02%) | 0.2 16/80 (20%) | ||
| 3–5 h | 0.0 2/172 (1.16%) | 0.0 1/80 (1.25%) | ||
| Above 5 h | 0.0 1/172 (0.58%) | 0.0 1/80 (1.25%) | ||
| TRUST IN SOCIAL MEDIA | 165 | X22 = 0.18, p = 0.912 | ||
| Low | 0.6 67/108 (62.04%) | 0.6 35/57 (61.4%) | ||
| Medium | 0.3 30/108 (27.78%) | 0.3 15/57 (26.32%) | ||
| High | 0.1 11/108 (10.19%) | 0.1 7/57 (12.28%) | ||
| N | Mean | Median | SD | Variance | Minimum | Maximum | W | p | |
|---|---|---|---|---|---|---|---|---|---|
| Perceived risk of vaccination | 252 | 3.987 | 4.286 | 0.832 | 0.693 | 1.00 | 5.00 | 0.900 | <0.001 * |
| Perceived risk of illness | 252 | 5.412 | 5.500 | 1.473 | 2.171 | 1.00 | 9.13 | 0.990 | 0.076 * |
| Perceived vulnerability | 252 | 5.209 | 5.250 | 1.732 | 3.000 | 1.00 | 9.25 | 0.984 | 0.007 * |
| Perceived uncertainty | 252 | 6.304 | 6.500 | 0.806 | 0.649 | 2.00 | 7.00 | 0.813 | <0.001 * |
| Trust in own decision | 252 | 8.190 | 10.000 | 2.566 | 6.585 | 1 | 10 | 0.732 | <0.001 * |
| Social media engagement | 252 | 0.992 | 0.500 | 1.404 | 1.970 | 0.00 | 10.50 | 0.691 | <0.001 * |
| Preventive behavior | 252 | 3.783 | 3.917 | 0.674 | 0.455 | 1.50 | 5.00 | 0.971 | <0.001 * |
| Cognitive and Behavioral Factors | χ2 | df | p | ε2 |
|---|---|---|---|---|
| Perceived risk of illness | 6.8297 | 1 | 0.009 | 0.02721 |
| Perceived risk of vaccination | 58.5887 | 1 | <0.001 | 0.23342 |
| Perceived vulnerability | 0.0584 | 1 | 0.809 | 2.33 × 10−4 |
| Perceived uncertainty | 1.6584 | 1 | 0.198 | 0.00661 |
| Social media engagement | 0.5210 | 1 | 0.470 | 0.00208 |
| Preventive behavior | 1.4279 | 1 | 0.232 | 0.00569 |
| 90% Confidence Interval | ||||
|---|---|---|---|---|
| Estimate | Lower | Upper | ||
| (1) PERC_RISK_VACC | Cohen’s d(av) | 1.22 | 0.982 | 1.49 |
| Raw | 0.941 | 0.756 | 1.13 | |
| Trust in One’s Decision to Vaccinate | VACCINATED | Total | |
|---|---|---|---|
| Yes | No | ||
| low | 5 | 16 | 21 |
| Medium | 26 | 23 | 49 |
| High | 141 | 41 | 182 |
| Total | 172 | 80 | 252 |
| Value | Df | p | |
| χ2 | 31.5 | 2 | <0.001 |
| VACCINATED | Total | |||
|---|---|---|---|---|
| Previously Vaccinated | Yes | No | ||
| Yes | Observed | 61 | 20 | 81 |
| % Within row | 75.3% | 24.7% | 100.0% | |
| No | Observed | 111 | 60 | 171 |
| % Within row | 64.9% | 35.1% | 100.0% | |
| Total | Observed | 172 | 80 | 252 |
| % Within row | 68.3 % | 31.7% | 100.0% | |
| Value | df | p | ||
| χ2 | 2.74 | 1 | 0.098 | |
| Perceived Risk of Illness | Perceived Risk of Vaccination | Perceived Vulnerability | Perceived Uncertainty | Social Media Engagement | Preventive Behavior | ||
|---|---|---|---|---|---|---|---|
| Perceived risk of illness | Spearman’s rho | — | |||||
| p-value | — | ||||||
| Perceived risk of vaccination | Spearman’s rho | −0.062 | — | ||||
| p-value | 0.330 | — | |||||
| Perceived vulnerability | Spearman’s rho | 0.488 *** | 0.211 *** | — | |||
| p-value | <0.001 | <0.001 | — | ||||
| Perceived uncertainty | Spearman’s rho | 0.083 | 0.041 | 0.063 | — | ||
| p-value | 0.190 | 0.519 | 0.318 | — | |||
| Social media engagement | Spearman’s rho | −0.127 * | −0.196 ** | −0.177 ** | 0.076 | — | |
| p-value | 0.044 | 0.002 | 0.005 | 0.230 | — | ||
| Preventive behavior | Spearman’s rho | −0.039 | 0.259 *** | 0.049 | 0.080 | −0.014 | — |
| p-value | 0.539 | <0.001 | 0.439 | 0.203 | 0.823 | — |
| Perceived Risk of Vaccination | Mask | Hand Gel | Washing 20s | Avoid Crowds | Disinfectants | Search Info | ||
|---|---|---|---|---|---|---|---|---|
| Perceived risk of vaccination | Spearman’s rho | — | ||||||
| p-value | — | |||||||
| Mask | Spearman’s rho | 0.002 | — | |||||
| p-value | 0.975 | — | ||||||
| Hand Gel | Spearman’s rho | 0.214 *** | 0.414 *** | — | ||||
| p-value | <0.001 | <0.001 | — | |||||
| Washing 20s | Spearman’s rho | 0.163 * | 0.447 *** | 0.590 *** | — | |||
| p-value | 0.010 | <0.001 | <0.001 | — | ||||
| Avoid crowds | Spearman’s rho | 0.152 * | 0.339 *** | 0.375 *** | 0.526 *** | — | ||
| p-value | 0.016 | <0.001 | <0.001 | <0.001 | — | |||
| Disinfectants | Spearman’s rho | 0.218 *** | 0.138 * | 0.459 *** | 0.431 *** | 0.432 *** | — | |
| p-value | <0.001 | 0.032 | <0.001 | <0.001 | <0.001 | — | ||
| Search info | Spearman’s rho | 0.153 * | 0.100 | 0.125 | 0.227 *** | 0.308 *** | 0.479 *** | — |
| p-value | 0.021 | 0.131 | 0.063 | <0.001 | <0.001 | <0.001 | — |
| Model Fit Measures | ||||||||
|---|---|---|---|---|---|---|---|---|
| Overall Model Test | ||||||||
| Model | Deviance | AIC | R²McF | R²CS | R²N | χ2 | df | p |
| 1 | 218 | 238 | 0.309 | 0.320 | 0.449 | 97.2 | 9 | <0.001 |
| Model Coefficients—VACCINATED | ||||||||
| 95% Confidence Interval | ||||||||
| Predictor | Estimate | SE | Z | p | Odds Ratio | Lower | Upper | |
| Intercept | 0.6092 | 1.980 | 0.308 | 0.758 | 1.839 | 0.0379 | 89.105 | |
| (5) PREV_VACC: | ||||||||
| No—Yes | 0.3707 | 0.392 | 0.946 | 0.344 | 1.449 | 0.6722 | 3.123 | |
| (4) TRUST_VACC_DEC: | ||||||||
| Low-high | 2.1901 | 0.619 | 3.540 | <0.001 | 8.936 | 2.6579 | 30.045 | |
| Medium-high | 1.0555 | 0.419 | 2.520 | 0.012 | 2.873 | 1.2645 | 6.529 | |
| (1) PERC_RISK_ILL | 0.2333 | 0.146 | 1.600 | 0.110 | 1.263 | 0.9489 | 1.680 | |
| (1) PERC_RISK_VACC | −1.5639 | 0.239 | −6.530 | <0.001 | 0.209 | 0.1309 | 0.335 | |
| (2) PERC_VULN | −0.0309 | 0.120 | −0.257 | 0.797 | 0.970 | 0.7660 | 1.227 | |
| (3) PERC_UNCERTAIN | 0.1504 | 0.209 | 0.720 | 0.471 | 1.162 | 0.7719 | 1.750 | |
| (6) SOCIAL_MEDIA | −0.0399 | 0.128 | −0.312 | 0.755 | 0.961 | 0.7476 | 1.235 | |
| (7) PREV_BEHAV | 0.5170 | 0.273 | 1.895 | 0.058 | 1.677 | 0.9824 | 2.863 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcu, G.M.; Radu, A.M.; Bucuță, M.D.; Fleacă, R.S.; Tanasescu, C.; Roman, M.D.; Boicean, A.; Bacilă, C.I. Cognitive and Behavioral Factors Predicting the Decision to Vaccinate against COVID-19 in Clinical Psychiatric Population—A Cross-Sectional Survey. Vaccines 2023, 11, 441. https://doi.org/10.3390/vaccines11020441
Marcu GM, Radu AM, Bucuță MD, Fleacă RS, Tanasescu C, Roman MD, Boicean A, Bacilă CI. Cognitive and Behavioral Factors Predicting the Decision to Vaccinate against COVID-19 in Clinical Psychiatric Population—A Cross-Sectional Survey. Vaccines. 2023; 11(2):441. https://doi.org/10.3390/vaccines11020441
Chicago/Turabian StyleMarcu, Gabriela Mariana, Ana Maria Radu, Mihaela Dana Bucuță, Radu Sorin Fleacă, Ciprian Tanasescu, Mihai Dan Roman, Adrian Boicean, and Ciprian Ionuț Bacilă. 2023. "Cognitive and Behavioral Factors Predicting the Decision to Vaccinate against COVID-19 in Clinical Psychiatric Population—A Cross-Sectional Survey" Vaccines 11, no. 2: 441. https://doi.org/10.3390/vaccines11020441
APA StyleMarcu, G. M., Radu, A. M., Bucuță, M. D., Fleacă, R. S., Tanasescu, C., Roman, M. D., Boicean, A., & Bacilă, C. I. (2023). Cognitive and Behavioral Factors Predicting the Decision to Vaccinate against COVID-19 in Clinical Psychiatric Population—A Cross-Sectional Survey. Vaccines, 11(2), 441. https://doi.org/10.3390/vaccines11020441







