COVID-19 Vaccine Status, Intent, Hesitancy, and Disease-Related Beliefs in People with Multiple Sclerosis
Abstract
1. Introduction
2. Materials and Methods
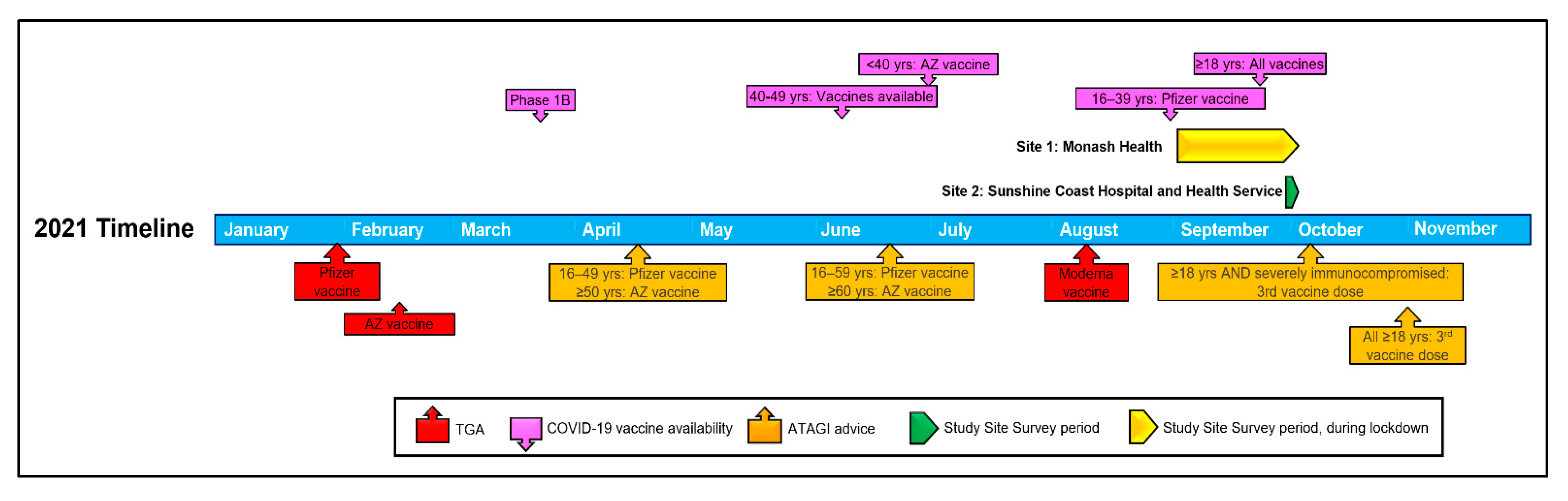
2.1. Study Design
2.2. Study Participants
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Vaccination Status and Intent
3.3. Vaccine Hesitancy, Confidence and Complacency
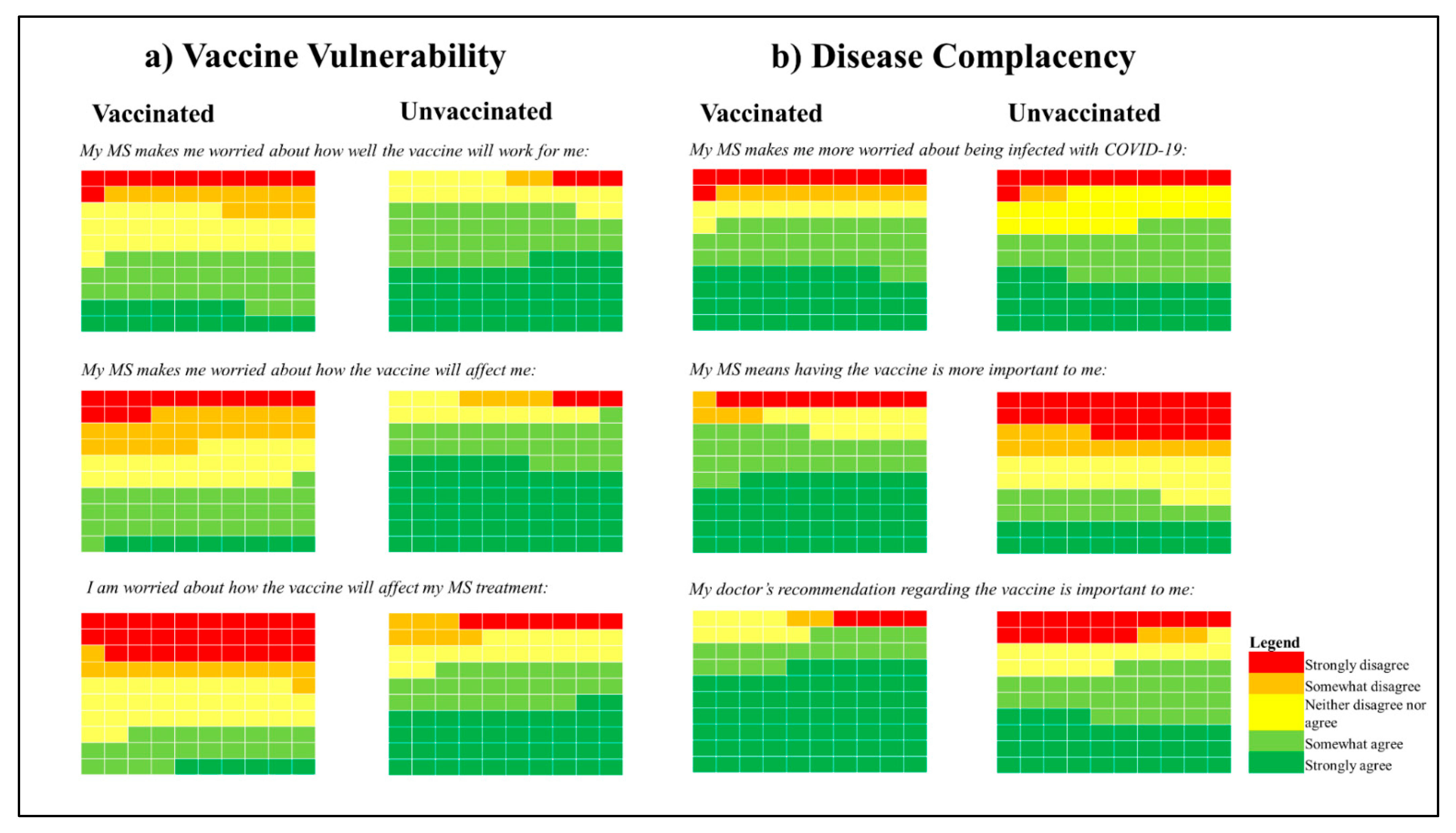
3.4. Disease-Related Vaccine Concerns (DIVAS-6)
3.5. Predicting Vaccine Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Multiple Sclerosis International Federation. Atlas of MS 2020. September 2020. Available online: https://www.msif.org/wp-content/uploads/2020/10/Atlas-3rd-Edition-Epidemiology-report-EN-updated-30-9-20.pdf (accessed on 12 November 2022).
- Chaudhry, F.; Jageka, C.; Levy, P.D.; Cerghet, M.; Lisak, R.P. Review of the COVID-19 Risk in Multiple Sclerosis. J. Cell. Immunol. 2021, 3, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Garjani, A.; Middleton, R.M.; Nicholas, R.; Evangelou, N. Recovery From COVID-19 in Multiple Sclerosis: A Prospective and Longitudinal Cohort Study of the United Kingdom Multiple Sclerosis Register. Neurol. Neuroimmunol. Neuroinflamm. 2022, 9, e1118. [Google Scholar] [CrossRef]
- Magyari, M.; Sorensen, P.S. Comorbidity in Multiple Sclerosis. Review. Front. Neurol. 2020, 11, 851. [Google Scholar] [CrossRef] [PubMed]
- Australian Government. Australia’s COVID-19 Vaccine National Roll-Out Strategy. Available online: https://www.health.gov.au/sites/default/files/documents/2021/01/covid-19-vaccination-australia-s-covid-19-vaccine-national-roll-out-strategy.pdf (accessed on 12 November 2022).
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef]
- CDC. COVID-19 Vaccine: Interim COVID-19 Immunization Schedule for Ages 5 Years and Older; CDC (Centers for Disease Control and Prevention): Atlanta, GA, USA, 2022. Available online: https://www.cdc.gov/vaccines/covid-19/downloads/COVID-19-immunization-schedule-ages-5yrs-older.pdf (accessed on 12 November 2022).
- Di Fusco, M.; Lin, J.; Vaghela, S.; Lingohr-Smith, M.; Nguyen, J.L.; Sforzolini, T.S.; Judy, J.; Cane, A.; Moran, M.M. COVID-19 vaccine effectiveness among immunocompromised populations: A targeted literature review of real-world studies. Expert Rev. Vaccines 2022, 21, 435–451. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Humbert, A.T.; Herring, T.E.; Alschuler, K.N. COVID-19 vaccine hesitancy in adults with multiple sclerosis in the United States: A follow up survey during the initial vaccine rollout in 2021. Mult. Scler. Relat. Disord. 2021, 54, 103163. [Google Scholar] [CrossRef] [PubMed]
- Uhr, L.; Mateen, F.J. COVID-19 vaccine hesitancy in multiple sclerosis: A cross-sectional survey. Mult. Scler. 2021, 28, 1072–1080. [Google Scholar] [CrossRef]
- Yap, S.M.; Al Hinai, M.; Gaughan, M.; Callanan, I.; Kearney, H.; Tubridy, N.; McGuigan, C. Vaccine hesitancy among people with multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 56, 103236. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Sage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- World Health Organisation. Top Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 12 November 2022).
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.; Failla, G.; Ricciardi, W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine 2021, 40, 101113. [Google Scholar] [CrossRef] [PubMed]
- Toussirot, É.; Bereau, M. Vaccination and induction of autoimmune diseases. Inflamm. Allergy Drug Targets 2015, 14, 94–98. [Google Scholar] [CrossRef]
- Nistri, R.; Barbuti, E.; Rinaldi, V.; Tufano, L.; Pozzilli, V.; Ianniello, A.; Marinelli, F.; De Luca, G.; Prosperini, L.; Tomassini, V.; et al. Case report: Multiple sclerosis relapses after vaccination against SARS-CoV2: A series of clinical cases. Case Report. Front. Neurol. 2021, 12, 765954. [Google Scholar] [CrossRef] [PubMed]
- Grech, L.; Loe, B.S.; Day, D.; Freeman, D.; Kwok, A.; Nguyen, M.; Bain, N.; Segelov, E. The Disease Influenced Vaccine Acceptance Scale-Six (DIVAS-6): Validation of a Measure to Assess Disease-Related COVID-19 Vaccine Attitudes and Concerns. Behav. Med. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 52, 3127–3141. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Australian Government Department of Health. COVID-19 Vaccine Roll-Out Update 06 October 2021. Available online: https://www.health.gov.au/sites/default/files/documents/2021/10/covid-19-vaccine-rollout-update-6-october-2021.pdf (accessed on 11 November 2022).
- Kalron, A.; Dolev, M.; Menascu, S.; Aloni, R.; Frid, L.; Givon, U.; Magalashvilli, D.; Achiron, A. Overcoming COVID-19 vaccine hesitancy in people with multiple sclerosis. Mult. Scler. 2021, 27 (Suppl. 2), 218. [Google Scholar]
- Wu, H.; Ward, M.; Brown, A.; Blackwell, E.; Umer, A. COVID-19 Vaccine intent in appalachian patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 57, 103450. [Google Scholar] [CrossRef]
- Epstein, S.; Xia, Z.; Lee, A.J.; Dahl, M.; Edwards, K.; Levit, E.; Longbrake, E.E.; Perrone, C.; Kavak, K.; Weinstock-Guttman, B.; et al. Vaccination Against SARS-CoV-2 in Neuroinflammatory Disease: Early Safety/Tolerability Data. Mult. Scler. Relat. Disord. 2022, 57, 103433. [Google Scholar] [CrossRef]
- Nabavi, S.M.; Mehrabani, M.; Ghalichi, L.; Nahayati, M.A.; Ghaffari, M.; Ashtari, F.; Mohammadianinejad, S.E.; Karimi, S.; Faghani, L.; Yazdanbakhsh, S.; et al. COVID-19 Vaccination Willingness and Acceptability in Multiple Sclerosis Patients: A Cross Sectional Study in Iran. Vaccines 2022, 10, 135. [Google Scholar] [CrossRef]
- Panisset, M.G.; Kilpatrick, T.; Cofré Lizama, L.E.; Galea, M.P. Implementing education: Personal communication with a healthcare professional is a critical step to address vaccine hesitancy for people with multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 63, 103933. [Google Scholar] [CrossRef]
- Marrie, R.A.; Dolovich, C.; Cutter, G.R.; Fox, R.J.; Salter, A. Attitudes toward coronavirus disease 2019 vaccination in people with multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2022, 8, 20552173221102067. [Google Scholar] [CrossRef] [PubMed]
- Mailand, M.T.; Frederiksen, J.L. Vaccines and multiple sclerosis: A systematic review. J. Neurol. 2017, 264, 1035–1050. [Google Scholar] [CrossRef] [PubMed]
- Xiang, X.M.; Hollen, C.; Yang, Q.; Brumbach, B.H.; Spain, R.I.; Wooliscroft, L. COVID-19 vaccination willingness among people with multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2021, 7, 20552173211017159. [Google Scholar] [CrossRef]
- Thistlethwaite, J.; Evans, R.; Tie, R.N.; Heal, C. Shared decision making and decision aids—A literature review. Aust. Fam. Physician 2006, 35, 537–540. [Google Scholar] [PubMed]
- Yamout, B.I.; Zakaria, M.; Inshasi, J.; Al-Jumah, M.; Zeineddine, M.; Dahdaleh, M.; Bohlega, S.; Gouider, R.; Alroughani, R. MENACTRIMS practice guideline for COVID-19 vaccination in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 56, 103225. [Google Scholar] [CrossRef]
- Kaufman, J.; Bagot, K.L.; Tuckerman, J.; Biezen, R.; Oliver, J.; Jos, C.; Ong, D.S.; Manski-Nankervis, J.; Seale, H.; Sanci, L.; et al. Qualitative exploration of intentions, concerns and information needs of vaccine-hesitant adults initially prioritised to receive COVID-19 vaccines in Australia. Aust. N. Z. J. Public Health 2022, 46, 16–24. [Google Scholar] [CrossRef]
- Kaufman, J.; Tuckerman, J.; Danchin, M. Overcoming COVID-19 vaccine hesitancy: Can Australia reach the last 20 percent? Expert Rev. Vaccines 2022, 21, 159–161. [Google Scholar] [CrossRef]
- Abbasi, N.; Ghadiri, F.; Moghadasi, A.N.; Azimi, A.; Navardi, S.; Heidari, H.; Karaminia, M.; Sahraian, M.A. COVID-19 vaccine hesitancy in Iranian patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 60, 103723. [Google Scholar] [CrossRef]
- Beauchamp, A.; Buchbinder, R.; Dodson, S.; Batterham, R.W.; Elsworth, G.R.; McPhee, C.; Sparkes, L.; Hawkins, M.; Osborne, R.H. Distribution of health literacy strengths and weaknesses across socio-demographic groups: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health 2015, 15, 678. [Google Scholar] [CrossRef]
- Khurana, V.; Sharma, H.; Medin, J. Estimated prevalence of secondary progressive multiple sclerosis in the USA and Europe: Results from a systematic literature search (P2.380). Neurology 2018, 90 (Suppl. 15), P2.380. [Google Scholar]
| Characteristic | Total n = 281 (%) | Vaccinated n = 239 (82.9%) | Unvaccinated n = 48 (17.1%) |
|---|---|---|---|
| Male | 65 (23.1) | 57 (87.7) | 8 (12.3) |
| Female * | 213 (75.8) | 174 (81.7) | 39 (18.3) |
| Age: mean (SD) | 47.7 (12.8) | 49.1 (12.6) | 40.6 (11.7) |
| Age (years) | |||
| 18–39 | 83 (29.5) | 56 (67.5) | 27 (32.5) |
| 40–59 | 138 (49.1) | 120 (87.0) | 18 (13.0) |
| ≥60 | 60 (21.4) | 57 (95.0) | 3 (5.0) |
| Highest level of education ** | |||
| No formal/primary school | 4 (1.4) | 3 (75.0) | 1 (25.0) |
| Secondary school | 86 (30.6) | 73 (84.9) | 13 (15.1) |
| Vocational/Trade | 75 (26.7) | 57 (76.0) | 18 (24.0) |
| University | 115 (40.9) | 100 (87.0) | 15 (13.0) |
| Annual household income (AUD) | |||
| <50 K | 72 (25.6) | 62 (86.1) | 10 (13.9) |
| 50 K–100 K | 76 (27.0) | 59 (77.6) | 17 (22.4) |
| 100 K–150 K | 41 (14.6) | 33 (80.5) | 8 (19.5) |
| >150 K | 40 (14.2) | 35 (87.5) | 5 (12.5) |
| Prefer not to say | 52 (18.5) | 44 (84.6) | 8 (15.4) |
| English as first language | |||
| Yes | 257 (91.5) | 215 (83.7) | 42 (16.3) |
| Location | |||
| Metropolitan | 239 (85.1) | 202 (84.5) | 37 (15.5) |
| Regional/Rural | 42 (14.9) | 31 (73.8) | 11 (26.2) |
| Multiple sclerosis type | |||
| Relapsing-remitting MS (RRMS) | 203 (72.2) | 170 (83.7) | 33 (16.3) |
| Primary progressive MS (PPMS) | 26 (9.3) | 19 (73.1) | 7 (26.9) |
| Secondary progressive MS (SPMS) | 30 (10.7) | 26 (86.7) | 4 (13.3) |
| Other/Don’t know | 22 (7.8) | 18 (81.8) | 4 (18.2) |
| Time since diagnosis | |||
| <1 year | 10 (3.6) | 9 (90.0) | 1 (10.0) |
| 1–5 years | 78 (27.8) | 56 (71.8) | 22 (28.2) |
| 5.1–10 years | 58 (20.6) | 47 (81.0) | 11 (19.0) |
| >10 years | 135 (48.0) | 121 (89.6) | 14 (10.4) |
| Current MS treatment | |||
| Tablets | 106 (37.7) | 94 (88.7) | 12 (11.3) |
| Injectables | 26 (9.3) | 22 (84.6) | 4 (15.4) |
| Intravenous | 92 (32.7) | 71 (77.2) | 21 (22.8) |
| No specific treatment/Other | 57 (20.3) | 46 (80.7) | 11 (19.3) |
| MS control over the past 6 months | |||
| Yes | 226 (80.4) | 191 (84.5) | 35 (15.5) |
| No | 27 (9.6) | 19 (70.4) | 8 (29.6) |
| Don’t know | 28 (10.0) | 23 (82.1) | 5 (17.9) |
| No. of times missed disease modifying therapies in the past month | |||
| All of the time | 7 (2.5) | 4 (57.1) | 3 (42.9) |
| Most of the time | 3 (1.1) | 3 (100.0) | 0 (0.0) |
| Some of the time | 9 (3.3) | 6 (66.7) | 3 (33.3) |
| Occasionally | 36 (13.1) | 32 (88.9) | 4 (11.1) |
| Never | 220 (80.0) | 184 (83.6) | 36 (16.4) |
| MS affect daily activities in last 4 weeks | |||
| All of the time | 44 (15.7) | 33 (75.0) | 11 (25.0) |
| Most of the time | 35 (12.5) | 31 (88.6) | 4 (11.4) |
| Some of the time | 85 (30.2) | 69 (81.2) | 16 (18.8) |
| Not very often | 53 (18.9) | 45 (84.9) | 8 (15.1) |
| Not at all | 64 (22.8) | 55 (85.9) | 9 (14.1) |
| Category (Reference, n) | OR (95% CI) | p-Value |
|---|---|---|
| Age (n = 281) | 1.06 (1.03–1.08) | <0.001 |
| Time since diagnosis (>10 years, n = 281) | ||
| <1 year | 1.18 (0.14–10.22) | 0.88 |
| 1–5 years | 0.31 (0.15–0.66) | 0.002 |
| 5.1–10 years | 0.52 (0.22–1.24) | 0.14 |
| Step 1 | Step 2 | ||||
|---|---|---|---|---|---|
| Category (Reference, n) | Adj. R2 | Adj. R2 | Δ Adj. R2 | B (SE) | p-Value |
| Gender (Male, n = 261) | 0.043 | 0.068 | 0.025 | ||
| Female | 2.21 (0.77) | 0.005 | |||
| Age (n = 264) | 0.043 | 0.063 | 0.020 | −0.07 (0.03) | 0.01 |
| Location (Metropolitan, n = 264) | 0.043 | 0.043 | 0.000 | ||
| Regional/rural | 3.82 (3.87) | 0.32 | |||
| Time since diagnosis (>10 years, n = 264) | 0.043 | 0.050 | 0.007 | ||
| <1 year | −0.21 (1.84) | 0.91 | |||
| 1–5 years | 1.69 (0.79) | 0.03 | |||
| 5.1–10 years | 0.83 (0.86) | 0.34 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grech, L.; Kwok, A.; Nguyen, M.; Winkel, A.; Butler, E.; Allan, M.; Bain, N.; Segelov, E.; on behalf of the MSVACCS Investigators. COVID-19 Vaccine Status, Intent, Hesitancy, and Disease-Related Beliefs in People with Multiple Sclerosis. Vaccines 2023, 11, 410. https://doi.org/10.3390/vaccines11020410
Grech L, Kwok A, Nguyen M, Winkel A, Butler E, Allan M, Bain N, Segelov E, on behalf of the MSVACCS Investigators. COVID-19 Vaccine Status, Intent, Hesitancy, and Disease-Related Beliefs in People with Multiple Sclerosis. Vaccines. 2023; 11(2):410. https://doi.org/10.3390/vaccines11020410
Chicago/Turabian StyleGrech, Lisa, Alastair Kwok, Mike Nguyen, Antony Winkel, Ernest Butler, Michelle Allan, Nathan Bain, Eva Segelov, and on behalf of the MSVACCS Investigators. 2023. "COVID-19 Vaccine Status, Intent, Hesitancy, and Disease-Related Beliefs in People with Multiple Sclerosis" Vaccines 11, no. 2: 410. https://doi.org/10.3390/vaccines11020410
APA StyleGrech, L., Kwok, A., Nguyen, M., Winkel, A., Butler, E., Allan, M., Bain, N., Segelov, E., & on behalf of the MSVACCS Investigators. (2023). COVID-19 Vaccine Status, Intent, Hesitancy, and Disease-Related Beliefs in People with Multiple Sclerosis. Vaccines, 11(2), 410. https://doi.org/10.3390/vaccines11020410







