Abstract
Scheduled or routine childhood vaccinations are known for their effectiveness in eradicating fear for many life-threatening and disabling diseases and saving lives globally. This paper is aimed at assessing determinants of parents taking their children for scheduled vaccinations during the COVID-19 pandemic in South Africa. Data used for this paper were obtained from the Human Sciences Research Council’s (HSRC) COVID-19 Online Survey titled “One Year Later Survey”, which was conducted between 25 June and 11 October 2021 in South Africa. Multivariate logistic regression analysis was performed to achieve this study goal. Findings showed that just over half of parents (56.7%) reported taking their children for scheduled vaccinations across the country. Males were significantly less likely (aOR = 0.53 95% CI [0.45–0.61], p < 0.001) to have taken their children for scheduled vaccinations than females. Parents’ experiences and views were among key determinants of parents having taken their children for scheduled vaccinations in South Africa. Parents who had never taken influenza (flu) vaccines were significantly less likely (aOR = 0.33 [0.28–039], p < 0.001) to have taken their children for scheduled vaccinations than those who had taken flu vaccines. Parents who did not know anyone who had personally experienced serious side effects to any vaccine were significantly less likely (aOR = 0.77 [0.66–0.90], p = 0.001) to have taken their children for scheduled vaccinations than those who knew anyone who had experienced them. Parents who did not think vaccines were a good way to protect communities from disease were significantly less likely (aOR = 0.50 [0.33–0.77], p = 0.001) to have taken their children for scheduled vaccinations than those who thought vaccines were a good way to protect communities from disease. These findings are of significance especially during the time when the country is still struggling to reach a substantial proportion of its population vaccinated for COVID-19. Thus, these findings may be relevant in determining parents’ intentions to have their children receive the South African Department of Health recommended vaccines for their respective age group.
1. Introduction
Scheduled or routine childhood vaccines are known for their effectiveness in eradicating fear of many life-threatening and disabling diseases and saving lives globally, and several governments have institutionalised childhood immunization programmes. However, during disasters such as COVID-19 pandemic, immunisation uptake can be disrupted. The World Health Organization (WHO) reported that 25 million children missed out on vaccination in 2021 due to COVID-19 disruptions to health care systems. COVID-19 lockdowns disrupted routine childhood vaccine coverage for under-five-year-olds globally [1], leading to significant declines in vaccination rates. Disruptions are creating a risk for infectious disease outbreaks, but the extent to which these possible outbreaks are a source of concern to parents may be unclear. Average periodic records of routine vaccines and proportions of children with up-to-date vaccination for age decreased in the early stages of the pandemic [2].
Parents’ decision making about initiating or continuing their children’s scheduled immunisation is compounded by contextual changes and psychological factors that emerge during crises. Delayed immunisation and nonvaccination compromise protection of children from outbreaks of vaccine-preventable diseases and death [3]. South Africa has a relatively long history with its routine childhood vaccination programme, which started in 1974 [4], though not comparable to some developed countries such as the United Kingdom’s availability of viral smallpox vaccination, which began in the 18th century [5] and was later followed by development and bacterial vaccination for tuberculosis. South Africa has since introduced a suite of routine childhood vaccines that form part of the national expanded immunisation programme (EIP-SA) funded by the government. The childhood immunisation schedule entails vaccines administered at birth and subsequent doses until 12 years provided as follows: Bacillus Calmette-Guérin (BCG) and Oral polio vaccine (OPV)(0) at birth; OPV(1), Rotavirus (RV)(1), Diphtheria/Tetanus/Pertussis, inactive polio vaccine, Haemophilus influenzae and Hepatitis B antigens (DTP-IPV-Hib-HepB)(1) and Pneumococcal conjugate vaccine (PCV)(1) at six weeks; DTP-IPV-HiB-HepB(2) at 10 weeks; RV(2), DTP-IPV-Hib-HepB(3) and PCV(2) at 14 weeks; Measles(1) at six months; PCV(3) at nine months; Measles(2) at 12 months; DTP-IPV-Hib-HepB(4) at 18 months; and Tetanus-Diphtheria (Td)(1) at six years, followed by two doses of Human papilloma virus vaccine (HPV) at nine years and Td(2) at 12 years [6]. Although they are a crucial element of the universal health coverage, unlike in countries such as Saudi Arabia where completeness of preschool age immunization is mandatory [7], in South Africa childhood vaccines are not mandatory.
Scheduled or routine childhood vaccines in South Africa are available for free in public primary health care facilities and are primarily offered for young children under the age of five years. The majority of them are to be taken in the first year of life. However, the global challenge of incomplete or no vaccination [8], also common in South Africa, means that the national government and provincial health authorities can prevent diseases that cause childhood suffering, disability, and death by improving the readiness of the health system to maintain optimal childhood vaccination rates even during disasters such as pandemics. During disasters in low- and middle-income countries, health care systems are severely disrupted thus exposing children to missing scheduled immunizations. A study conducted in India before COVID-19 reported about 18% decline in age-appropriate full immunization of children in disaster-affected areas [9].
Despite the proven benefits of childhood vaccines in eradicating life-threatening and disabling diseases, South Africa’s vaccine coverage in the pre-COVID-19 period was already suboptimal. Results from district health administrative data showed that national immunization coverage was 77% in 2017/2018 [10] (District Health Information System estimates do not accurately capture vaccinations administered in the private sector (Makamba-Mutevedzi et al., 2020). In 2019, Makamba-Mutevedzi and colleagues [11] reported a similar national average, 76.8% (75.4–78.2), from the nationally representative EPI survey of full vaccination coverage, that is, children who received all age-appropriate vaccinations from birth to 18 months. Disparities have been noted with some provinces and districts performing above national average coverage of routine immunisation and a handful of districts registering far below the national average [3,11]. Vaccine uptake determines full immunisation coverage, and vaccine timeliness is necessary for optimal prevention of debilitating childhood diseases and child death.
Research has identified various factors contributing to childhood immunisation incompleteness, and some studies and evidence reviews identify parent-related reasons. The determinants of parental decision making about vaccination are categorised as religious reasons, personal beliefs, safety concerns, and desire to have information from the health care professional [12,13,14]. Evidence reviews identify parents’ low trust in a health system due to social exclusion [12] and lack of confidence in the safety and effectiveness of vaccines as some of the factors that lead to suboptimal immunisation rates [15]. A study conducted in South Africa on EPI managers’ perspectives on the challenges affecting immunisation coverage before the onset of COVID-19 reported that apart from systemic barriers that constrain the health system in supporting families in ensuring optimal immunisation, parents’ reluctance to take their children for immunisation also lowered national coverage [16]. A national EPI survey found that in South Africa parents refused some of the scheduled vaccines (BCG and OPV0), and some reported forgetfulness, but religious reasons were insignificant [11].
Understanding determinants of parental reasons for their children receiving, delaying, or not receiving routine vaccination in countries with high infection rates during COVID-19 outbreaks is crucial. A few reviews and studies have examined parental views and experiences about routine childhood vaccines and the challenges of routine immunization during disasters and pandemics such as COVID-19. A systematic review of how delivery of maternal and child health services is affected during public health emergencies and pandemics in low- and middle-income countries identified common challenges that studies report to include disruptions in public health care systems, immunization becoming irregular, many children missing routine vaccinations as scheduled, and postponing until the situation was normal to complete their routine immunization schedule [17]. It is crucial to understand the social and behavioural drivers of parental attitudes towards vaccines and routine childhood vaccine behaviour in a low- and middle-income country given the limited evidence on strategies that can improve parents’ attitudes towards routine immunization during COVID-19 outbreaks.
Parental views and experiences are crucial because parents are an important group in society since they are not only responsible for their own health but also proxy for the health of their children [18,19]. They do not only participate in decision making about their children’s vaccination through consenting, but they also weigh the benefits of vaccinating or not vaccinating children during raging pandemics. Understanding parents’ views and experiences with vaccines can inform strategies needed to encourage parents to comply with the EPI programme and retain their children on scheduled vaccination programmes during pandemics such as COVID-19. This paper is aimed at assessing determinants of parents taking their children for scheduled vaccinations during the COVID-19 pandemic in South Africa.
2. Materials and Methods
2.1. Study Design and Sampling
Data used for this paper were obtained from the Human Sciences Research Council’s (HSRC) COVID-19 Online Survey titled “One Year Later Survey”, which was conducted between 25 June and 11 October 2021 in South Africa. The One Year Later Survey was conducted to assess the social and behavioural factors related to the pandemic, including vaccine-related attitudes, intentions, and behaviours. An online survey method, which was supplemented by telephonic interviews, was employed since face-to-face interviews were a challenge due to lockdown restrictions. Online surveys are more of convenience sampling as those with access to smart phones and internet are more likely to participate. To reduce this bias, telephonic interviews were included for disadvantaged areas such as townships and informal settlements.
2.2. Target Population and Sampling Frame
The study population was all adults aged 18 years and older who resided in South Africa regardless of their population group, sex, religion, and nationality. In terms of exclusion criteria, respondents who reported that they did not have children were excluded from the study sample as the focus was on parents. There were no exclusion criteria set for age of children in this study.
2.3. Sample Size
There was no sample size calculation; thus, a targeted minimum sample size was not predetermined for this online survey. The realised sample size of 12,708 parents is regarded large enough for the purpose of this study. It has been shown that reweighted online samples can produce response patterns that are statistically similar to general population characteristics [20]. Therefore, the data from the survey were weighted to distribution of South Africa’s estimated parent population using the general population demographics by age, sex, population group, and province.
2.4. Study Procedures
Invitations to participate in the study were widely distributed on social media platforms, the HSRC website, radio, and television stations. These media platforms included WhatsApp, Facebook, Twitter, and Instagram. The survey was administered online using a data-free platform, and data collection was supplemented by telephonic interviews. In addition to being a data-free platform, Moya Messaging platform has a large user base of four million members and one million daily engaged users. Telephonic interviews were to ensure that population from disadvantaged areas such as townships and informal settlements who did not have access to smart phones and computers were not excluded. Both online and telephonic surveys were conducted in six of the 11 official languages of South Africa, namely English, Afrikaans, IsiZulu, IsiXhosa, Xitsonga, and Tshivenda.
2.5. Study Instrument
The questionnaire was developed based on the initial questionnaires of HSRC COVID-19 Online Surveys [21,22,23], which were primarily based on previous work on public reactions to the pandemic [24,25] and in consultation with socio-behavioural scientists, public health experts, and epidemiologists both locally and globally.
2.6. Measures
The primary outcome variable was respondents having taken their children for scheduled vaccinations. The following question was asked, “Have you taken your children for scheduled vaccinations?” with response being 1 = yes, 2 = no, and 3 = I don’t have children. These responses were further recoded into 1 = yes and 0 = no. Those who reported that they did not have children were excluded from the study sample as the focus was on parents. The explanatory variables included sociodemographic variables and variables that indicated parents’ experiences and views about vaccines in general (Table 1).

Table 1.
Explanatory variables.
2.7. Data Analysis
Data analysis was conducted using Stata version 15 [26]. Data from the survey were benchmarked using the general population demographics by age, sex, population group, and province, based on Statistics South Africa’s 2021 population mid-year estimates [27]. The Stata “svy” command was used to incorporate benchmarking weights into the analysis. Descriptive analysis (frequencies and percentages) was used to summarize the sample characteristics of the study across demographic variables. Differences in the percentage of respondents who took their children for scheduled vaccinations versus those that did not were compared across the explanatory variables using 95% Confidence Intervals (CIs) and the Chi-square test. ArcGIS10.8 was used for map production [28].
Logistic regression models were considered as they are most appropriate statistical method for binary (yes or no) outcome variable [29,30]. One of the assumptions underlying the logistic regression models is that the explanatory variables should not be too highly correlated with each other, thus there should be little or no multicollinearity among the explanatory variables. Therefore, a correlation matrix was conducted to assess multicollinearity between explanatory variables. Estimates from logistic regression models, including multiple or multivariate logistic regression, which frequently used the multivariate technique, calculates odds ratios (ORs) and not Risk Ratios [30,31]. Some of the advantages of ORs are that they provide an estimate for the relationship between two binary variables, and they enable examining the effects of other variables on that relationship [32]. This means that the relationship between each variable and the binary outcome can be studied while holding constant the values of the other explanatory variables [28]. This is also useful to adjust the estimates for the effects of confounding variables in observational data [29]. Bivariate logistic regression models were conducted, and all significant variables were fitted into a multivariate logistic regression. Multivariate logistic regression analysis was performed to determine factors associated with parents taking their children for scheduled vaccinations during the COVID-19 pandemic in South Africa. Adjusted Odds Ratios (aOR) with 95% Confidence Intervals (CIs) were reported, and p value equal to or less than 0.05 was considered statistically significant.
3. Results
3.1. Characteristics of Study Sample
The study sample was 12,708 parents who responded to the question of having taken their children for scheduled vaccinations (Table 2). Female respondents or mothers accounted for 60.7% of the study sample. The majority of parents were Black Africans (80.6%), 42.6% had matric as their highest education qualification, 67.7% were unemployed, and 44.5% were residing in townships.

Table 2.
Characteristics of the study sample.
Regarding vaccine experiences, less than one third (30.5%) of the parents reported that they had taken the flu vaccine themselves. More than one in seven (15.2%) of the parents had personally refused to take any vaccine while over one quarter (26.3%) indicated that they have objected to allow someone else to take a vaccine. Parents who did not know anyone who had personally experienced serious side effects to any vaccine constituted 31.1%.
Respondents were asked questions about their views and opinions regarding vaccines in general. Less than two thirds (62.0%) believed that vaccines were a good way to protect communities from disease while more than half of (52%) the parents thought vaccines strengthen the immune system. The majority (72.4%) of the parents indicated that they would take the COVID-19 vaccines once they were made available while 10.3% reported that they would not take them.
3.2. Parents who Took Their Children for Scheduled Vaccinations by Sociodemographics, Experiences, and Views
Of the 12,708 parents, 56.7% reported that they had taken their children for scheduled vaccinations (Table 3). The proportion of parents who took their children for scheduled vaccinations differed significantly by sex, population group, age group, education level, employment status, and locality (p < 0.001). For instance, a significantly higher proportion of females (49.6%, 95% CI [47.6–51.6]) reported that they took their children for scheduled vaccinations compared to males (35.9%, [33.6–38.3]). Parents from rural or traditional tribal areas reported the lowest proportion of (34.8%, [31.5–38.2]) taking their children for scheduled vaccinations.

Table 3.
Parents’ taking children for scheduled vaccination by sociodemographics, experiences, and views.
When considering parents’ experiences with vaccines, parents who had taken the flu vaccine had significantly higher percentage of (62.1%, [59.0–65.0]) having taken their children for scheduled vaccinations than those who had never taken flu vaccine. Those who had personally refused to take any vaccine had significantly higher percentage of (52.3%, [48.3–56.3]) having taken their children for scheduled vaccinations than those who had never done so. Parents who knew anyone who had personally experienced serious side effects to any vaccine had significantly higher proportion of (47.9%, [45.1–50.6]) having taken their children for scheduled vaccinations than those who did not know anyone.
In terms of parents’ views on vaccines, parents who thought vaccines are a good way to protect communities from disease had significantly higher proportion of (47.2%, [45.1–49.2]) having taken their children for scheduled vaccinations than those who did not think so and those who were not sure. Those who thought vaccines strengthen the immune system had significantly higher percentage of (48.4%, [46.2–50.5]) having taken their children for scheduled vaccinations than those who did not think so and those who were not sure.
There was a significant difference (p < 0.001) in the proportions of parents who took their children for scheduled vaccinations by province. Western Cape had the highest proportion with 50.6% of parents who indicated that they had taken their children for scheduled vaccinations, followed by Gauteng and KwaZulu-Natal with 45.4% and 45.1%, respectively (Figure 1). Free State and North West provinces accounted for the lowest proportions with 33.1% and 29.7%, respectively.
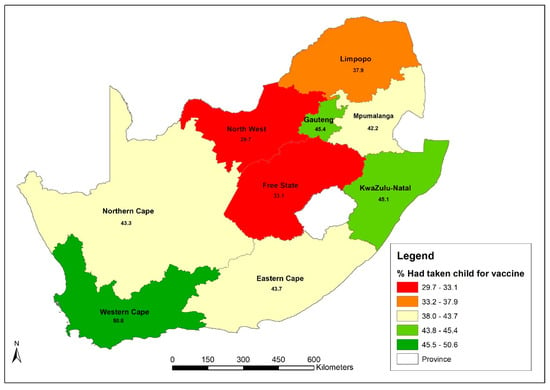
Figure 1.
Map showing proportions of parents who took their children for scheduled vaccinations.
3.3. Multivariate Logistic Regression Analysis of Factors Influencing Parents’ Taking Children for Scheduled Vaccinations
Males were significantly less likely (aOR = 0.53 95% CI [0.45–0.61], p < 0.001) to have taken their children for scheduled vaccinations than females (Table 4). Parents from the all other population groups were significantly more likely (Whites: aOR = 4.08 [2.79–5.96], p < 0.001; Coloureds: aOR = 1.72 [1.42–2.08], p < 0.001; Indian/Asians: aOR = 3.50 [2.23–5.49], p < 0.001) to have ever taken their children for scheduled vaccinations than Black Africans. The parents’ likelihood of taking their children for scheduled vaccinations gradually increased with increasing parental age as older parents were significantly more likely (30 to 39 years: aOR = 1.19 [1.05–1.35], p = 0.007; 40 to 49 years: aOR = 1.27 [1.08–1.49], p = 0.004; 50 to 59 years: aOR = 1.29 [1.02–1.64], p = 0.035; 60 years and older: aOR = 1.90 [1.24–2.90], p = 0.003) to have taken their children for scheduled vaccinations than younger people (those aged 18 to 29 years). Parents residing in suburbs, townships, and informal settlements were significantly more likely (aOR = 1.78 [1.33–2.38], p < 0.001; aOR = 1.41 [1.09–1.82], p = 0.009; aOR = 1.45 [1.04–2.03], p = 0.029 respectively) to have taken their children for scheduled vaccinations than those residing in the city.

Table 4.
Multivariate logistic regression of factors that influence parents’ having taken their children for scheduled vaccinations.
In terms of parents’ experiences with vaccines as determinant factors, those who had never taken flu vaccines were significantly less likely (aOR = 0.33 [0.28–039], p < 0.001) to have taken their children for scheduled vaccinations than those who had taken flu vaccines. Parents who did not know anyone who had personally experienced serious side effects to any vaccine were significantly less likely (aOR = 0.77 [0.66–0.90], p = 0.001) to have taken their children for scheduled vaccinations than those who knew anyone who had experienced them. Parents who did not think vaccines were a good way to protect communities from disease were significantly less likely (aOR = 0.50 [0.33–0.77], p = 0.001) to have taken their children for scheduled vaccinations than those who thought vaccines were a good way to protect communities from disease.
4. Discussion
This study sought to explore and understand the determinants of parents taking their children for scheduled childhood vaccination during the COVID-19 pandemic in South Africa. Vaccination of the paediatric population is a significant public health intervention even during disasters such as COVID-19. As He and colleagues [33] stated, it is critical for policy makers and health care professionals to have adequate knowledge about factors that influence routine childhood vaccine uptake including hesitancy to maintain paediatric vaccination rates and promote vaccine confidence during and after the COVID-19 pandemic.
In this study, the proportion of parents who reported taking their children for scheduled vaccinations was far smaller than the proportions reported by previous research including the nationally representative South African EPI survey conducted in the period prior to the COVID-19 pandemic [11]. It is always crucial that children scheduled or routine vaccination rates do not decrease during public health disasters and pandemics because missed or delayed immunisation can expose children to serious illness, disability, or death. Unfortunately, childhood immunisation programmes were reported to have been negatively affected by the pandemic globally, and the numbers of children who missed immunisation increased raising concerns about outbreaks of vaccine-preventable diseases due to the impact of COVID-19 on global health systems [33,34,35,36].
Our study findings showed that 52% of the parents thought vaccines strengthen the immune system while more than 39% were uncertain. Parents could have been concerned about exposing themselves or their young children to coronavirus infection by visiting public health facilities during the lockdowns. Bell and colleagues [37] found that even in a study with more than 85% of parents and guardians who believed that it was vital to adhere to paediatric vaccination schedules, “…this was balanced against their concerns over vaccinating their children during the pandemic…participants discussed the weighing up of perceived risks and benefits of taking their children for vaccination” [37] (p. 12). The context in which vaccination takes place is as important as parents’ characteristics in influencing routine childhood vaccination.
Our findings also showed that there were clear differences in parents’ gender and age regarding them reporting vaccinating their children during COVID-19. Fathers or male caregivers were less likely to have taken their children for scheduled vaccinations than mothers or female caregivers. This does not necessarily mean that fathers were against their children receiving scheduled vaccinations but is because mothers are the ones who mostly take responsibility for children’s caregiving and health; hence, they have a better chance of taking them for vaccinations. Notably, a review synthesis shows that especially in low- and middle-income countries, including in Africa, child vaccination facilities as social settings are highly feminised and can make men feel alienated from this social role [12]. If the women were fearful about risks associated with COVID-19, their behaviour would change despite the delivery of routine vaccination remaining unchanged, as indicated by Sahoo and colleagues: “…however, women often did not prefer to visit the immunization site, due to fear or suspicion of infection. Some studies reported perceptions about contracting the infection among children through injections in healthcare facilities” [12] (p. 9). Notably, in another study, they found that mothers were more fearful than fathers about risks associated with COVID-19 vaccination in Saudi Arabia [38].
Furthermore, in our analysis, younger parents (18 to 29 years old) were more hesitant to vaccinate their children than older parents. The parents’ likelihood of ever taking their children for scheduled vaccinations gradually increased with increasing parental age. With the onset of COVID-19, parents’ practices with maintaining scheduled vaccines and their appraisal of the benefits of vaccination during the pandemic would change because these decisions are hardly ever static [12]. They were influenced by how well informed the parents were with the national childhood vaccination programme. Young parents would not have as much experience with vaccines as older parents. One of the well-documented reasons for parents’ hesitancy to vaccinate their children is lack of information and their need to be provided with adequate information about the benefits and risks of vaccines under any circumstance, so they can make informed decisions [14]. Considering that health communication resources during the pandemic were mostly devoted to the developments in the response of government to the pandemic, reports of dwindling childhood vaccination rates could have been easily drowned by daily reports about South Africa’s pandemic. Young parents would have been disadvantaged by lack of information about whether to vaccinate children considering that their experience with vaccines would only be at embryonic stage compared with older parents who probably had longer history with these interventions. This means that they would tremendously benefit from clinic visits where health professionals consistently provided them with vaccination information.
It is not plausible that the young parents in our sample would be similar to parents in high-income countries who actively seek information on childhood vaccines to decide based on their particular and individual child if they indeed will benefit from any specific vaccine [12]; young parents would rely on government decision makers and health professionals for vaccination information during time of uncertainty. Since parental lack of knowledge about childhood vaccines was found to be associated with younger age of parents, it is important for the Department of Health to intensify health literacy of young parents and consistently provide them with information on childhood immunization, vaccines, and technology used, as well as the benefits of immunization, to address possible uncertainty during periods of reduced social interaction at health facilities. This finding is paradoxical but crucial as South Africa may also be different from other middle-income countries where studies report that younger parents tend to have better knowledge about childhood immunization than the older age cohorts of parents [7].
Concerns about catching coronavirus while accessing health services are real and require effective communication by health authorities and professionals emphasising availability of these services during outbreaks and health education about the benefits of up-to-date scheduled childhood vaccines. Evidence-based health policy guidelines and communication can facilitate parental decision making about children’s immunization schedule during uncertainty. When parents discontinue or suspend contact with the vaccination facilities, the number of unvaccinated children increases. This situation is associated with outbreaks of vaccine-preventable diseases such as measles. Already in 2022, some of the provinces with lower than national immunization coverage have reported measles outbreaks threatening the health and survival of young children.
Our findings also showed some racial differences whereby Black Africans reported the lowest levels of taking children for scheduled vaccinations when compared to other racial groups. This could be due to several factors such as access to health facilities, poverty, and unemployment as well as other racial disparities that are found in South African society. The findings of this study further showed that parents residing in suburbs, townships, and informal settlements were significantly more likely to have ever taken their children for scheduled vaccinations than those residing in the inner cities. It is important to note that although the term city is inclusive of informal settlements, townships, and suburbs, the sociodemographic characteristics of these areas are distinctly different given the history of extensive state interference in urban development in South Africa [39,40]. Parents who reside in most inner cities in South Africa are mostly young people who at the later stage move to surrounding suburbs and townships. Additionally, COVID-19 disproportionately occurred in urban areas, and government lockdowns accentuated the “second-order impacts” of the pandemic related to health service disruptions on the vulnerable urban populations [41]. This notion supports the finding that inner city residents were less likely to have ever taken their children for scheduled vaccinations as parents’ likelihood of ever taking their children for scheduled vaccinations has been found to be positively associated with increasing parental age in this study.
Among the parents/caregivers who participated in our online survey and had opted to vaccinate their children in the past, about two fifths indicated they had objected to allowing someone else to take a vaccine, which is lower than the proportion who objected to taking the COVID-19 vaccination in other countries. For instance, 52%, (n = 1094) of parents were unsure or not intending to vaccinate their children in Australia [42] whilst 73% (n = 274) of parents expressed negative or indecisive views on vaccinating their children in Turkey [43].
Parents’ views or beliefs about the efficacy of childhood vaccines influence whether they had taken their children for scheduled vaccinations. Parents who believed vaccines offered no protection from disease were significantly less likely to have taken their children for scheduled vaccinations than those who thought vaccines were a good way to protect communities from disease suggesting that knowledge about vaccine efficacy might be a driver in decision making. When considering parents’ views on vaccines as determinants of having taken their children for scheduled vaccinations, only one out of three variables was found to be significant. That is, those who did not think vaccines were a good way to protect communities from disease were significantly less likely to have taken their children for scheduled vaccinations than those who thought vaccines were a good way to protect communities from disease. Certain health behaviours of parents in relation to own health were associated with their behaviour when it came to protecting their children’s health from vaccine-preventable diseases. Parents who had never taken flu vaccines were significantly less likely to have ever taken their children for scheduled vaccinations than those who had taken flu vaccines. Surprisingly, parents who did not know anyone who had personally experienced serious side effects to any vaccine were significantly less likely to have ever taken their children for scheduled vaccinations than those who knew someone who had experienced such. This finding suggests that knowledge about the risk of experiencing side effects of vaccines was not influential in the parents’ decision making. The finding could be pointing to the importance of parents’ knowledge about childhood vaccination and diseases that are targeted with these interventions, as Alshammari and team [7] found that good knowledge about childhood vaccines increased the likelihood of parental adherence to scheduled vaccines. The challenge, however, would be a seeming low participation of parents in the sample in other disease prevention interventions such as flu vaccination taken periodically.
The study has some limitations. Firstly, the outcome variable is subject to self-report because a parent’s reporting of whether they took their child for their scheduled vaccinations does not fully measure vaccination status among their child/ren, and this also does not fully encompass parental experience of taking their children for scheduled vaccinations. Secondly, the survey was conducted as a general population survey administered online and telephonically, and thus the sample methodology was not aimed at specifically sampling parents of young children. Nevertheless, the study uses data from parents to assess patterns of associations between their experiences and views with vaccines and whether they reported taking their children for their scheduled vaccinations. In light of the COVID-19 vaccine hesitancy observed during the pandemic, the findings from this study may be relevant in determining parents’ intentions to have their children receive the South African Department of Health recommended vaccines for their age group.
5. Conclusions
Just over half of parents (56.7%) reported taking their children for scheduled vaccinations across the country. This might indicate that there is a substantial number of children who have not been taken for their scheduled vaccinations. Sex, age, population group, education, and locality were found to be key sociodemographic determinants of parents having taken their children for scheduled vaccinations. Parents’ experiences and views were also key determinants of parents having taken their children for scheduled vaccinations in South Africa. Initiatives that increase parents’ participation in other disease prevention interventions such as flu vaccination can increase chances of parents taking their children for scheduled vaccinations, specifically in the provinces with low proportions of parents taking children for vaccines (Free State, North West, and Limpopo). These findings are of significance especially during the time when the country is still struggling to reach a substantial proportion of its population vaccinated for COVID-19. Thus, these findings may be relevant in determining parents’ intentions to have their children receive the South African Department of Health recommended vaccines for their respective age group.
Author Contributions
Conceptualization and methodology, M.M. and T.M.; formal analysis, T.M.; validation, M.M., T.M., I.N., R.S. and S.S.; writing—original draft preparation, M.M., T.M. and I.N.; writing—review and editing, M.M., T.M., I.N., R.S. and S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by Research Ethics Committee (REC) of the HUMAN SCIENCES RESEARCH COUNCIL (HSRC) (REC 5/03/20 and in March 2020).
Informed Consent Statement
Consent for participation was obtained from all participants. Participants were informed of the right to withdraw from the survey at any time during the survey if they felt like doing so.
Data Availability Statement
Available on request from corresponding author upon reasonable time.
Acknowledgments
Thanks to participants who took part in the survey and to the HSRC COVID-19 Research Team.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alsuhaibani, M.; Alaqeel, A. Impact of the COVID-19 pandemic on routine childhood immunization in Saudi Arabia. Vaccines 2020, 8, 581. [Google Scholar] [CrossRef]
- DeSilva, M.B.; Haapala, J.; Vazquez-Benitez, G.; Daley, M.F.; Nordin, J.D.; Klein, N.P.; Henninger, M.L.; Williams, J.T.B.; Hambidge, S.J.; Jackson, M.L.; et al. Association of the COVID-19 pandemic with routine childhood vaccination rates and proportion up to date with vaccinations across 8 US health systems in the vaccine safety datalink. JAMA Pediatr. 2022, 176, 68–77. [Google Scholar] [CrossRef]
- Blose, N.; Amponsah-Dacosta, E.; Kagina, B.M.; Muloiwa, R. Descriptive analysis of routine childhood immunisation timeliness in the Western Cape, South Africa. Vaccine X 2022, 10, 100130. [Google Scholar] [CrossRef]
- Dlamini, N.R.; Maja, P. The Expanded Programme on Immunisation in South Africa: A story yet to be told. S. Afr. Med. J. 2016, 106, 675–677. [Google Scholar] [CrossRef]
- Calnan, M.; Douglas, T. (Eds.) Hopes, hesitancy and the risky business of vaccine development. Health Risk Soc. 2020, 22, 5–6. [Google Scholar]
- Ndwandwe, D.; Nnaji, C.A.; Mashunye, T.; Uthman, O.A.; Wiysonge, S.C. Incomplete vaccination and associated factors among children aged 12-23 months in South Africa: An analysis of the South African demographic and health survey 2016. Hum. Vaccines Immunother. 2020, 17. [Google Scholar] [CrossRef]
- Alshammari, S.Z.; AlFayyad, I.; Altannir, Y.; Al-Tannir, M. Parental awareness and attitude about childhood immunization in Riyadh, Saudi Arabia: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 8455. [Google Scholar] [CrossRef]
- Favin, M.; Steinglass, R.; Fields, R.; Banerjee, K.; Sawhney, M. Why children are not vaccinated: A review of the grey literature. Int. Health 2012, 4, 229–238. [Google Scholar]
- Datar, A.; Liu, J.; Linnemayr, S.; Stecher, C. The impact of natural disasters on child health and investments in rural India. Soc. Sci. Med. 2013, 76, 83–91. [Google Scholar] [CrossRef]
- Massyn, N.; Pillay, Y.; Padarath, A. District Health Barometer 2017/2018; Health Systems Trust: Pretoria, South Africa, 2019. [Google Scholar]
- Makamba-Mutevedzi, P.C.; Madhi, S.; Burnett, R. Expanded Programme on Immunisation (EPI) National Coverage Survey Report 2020; Department of Health, National Expanded Program on Immunization: Pretoria, South Africa, 2020. [Google Scholar]
- Cooper, S.; Schmidt, B.M.; Sambala, E.Z.; Swartz, A.; Colvin, C.J.; Leon, N.; Wiysonge, C.S. Factors that influence parents’ and informal caregivers’ views and practices regarding routine childhood vaccination: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2021, 10, CD013265. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef]
- McKee, C.; Bohannon, K. Exploring the reasons behind parental refusal of vaccines. J. Pediatr. Pharmacol. Ther. 2016, 21, 104–109. [Google Scholar] [CrossRef]
- Jacobson Vann, J.C.; Jacobson, R.M.; Coyne-Beasley, T.; Asafu-Adjei, J.K.; Szilagyi, P.G. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst. Rev. 2018, 1, CD003941. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Ngcobo, N.J.; Jeena, P.M.; Madhi, S.A.; Schoub, B.D.; Hawkridge, A.; Shey, M.S.; Hussey, G.D. Advances in childhood immunisation in South Africa: Where to now? Programme managers’ views and evidence from systematic reviews. BMC Public Health 2012, 12, 578. [Google Scholar] [CrossRef]
- Sahoo, K.C.; Negi, S.; Patel, K.; Mishra, B.K.; Palo, S.K.; Pati, S. Challenges in maternal and child health services delivery and access during pandemics or public health disasters in low-and middle-income countries: A systematic review. Healthcare 2021, 9, 828. [Google Scholar] [CrossRef]
- De Buhr, E.; Tannen, A. Parental health literacy and health knowledge, behaviours and outcomes in children: A cross-sectional survey. BMC Public Health 2020, 20, 1096. [Google Scholar] [CrossRef]
- Sinuraya, R.K.; Kusuma, A.S.W.; Pardoel, Z.E.; Postma, M.J.; Suwantika, A.A. Parents’ knowledge, attitude, and practice on childhood vaccination during the covid-19 pandemic in Indonesia. Patient Prefer. Adherence 2022, 16, 105–112. [Google Scholar] [CrossRef]
- Manyaapelo, T.; Mokhele, T.; Sifunda, S.; Ndlovu, P.; Dukhi, N.; Sewpaul, R.; Naidoo, I.; Jooste, S.; Tlou, B.; Moshabela, M.; et al. Determinants of confidence in overall knowledge about COVID-19 among healthcare workers in South Africa: Results from an online survey. Public Health Front 2021, 9, 1–9. [Google Scholar] [CrossRef]
- Mokhele, T.; Sewpaul, R.; Sifunda, S.; Weir-Smith, G.; Dlamini, S.; Manyaapelo, T.; Naidoo, I.; Parker, W.; Dukhi, N.; Jooste, S.; et al. Spatial analysis of perceived health system capability and actual health system capacity for COVID-19 in South Africa. Open Public Health J. 2021, 14, 388–398. [Google Scholar]
- Sifunda, S.; Mokhele, T.; Manyaapelo, T.; Dukhi, N.; Sewpaul, R.; Parker, W.; Parker, S.; Naidoo, I.; Jooste, S.; Ramlagan, S.; et al. Preparedness for self-isolation or quarantine and lockdown in South Africa: Results from a rapid COVID-19 online survey. BMC Public Health 2021, 21, 580. [Google Scholar] [CrossRef]
- Sewpaul, R.; Mabaso, M.; Dukhi, N.; Naidoo, I.; Vondo, N.; Davids, A.; Mokhele, T.; Reddy, P. Determinants of social distancing among South Africans from twelve days into the COVID-19 lockdown. Front. Public Health 2021, 9, 1–15. [Google Scholar] [CrossRef]
- Nooh, H.Z.; Alshammary, R.H.; Alenezy, J.M.; Alrowaili, N.H.; Alsharari, M.J.; Alenzi, N.M.; Sabaa, H.E. Public awareness of coronavirus in Al-Jouf region, Saudi Arabia. J. Public Health 2020, 29, 1107–1114. [Google Scholar] [CrossRef]
- Ipsos. Coronavirus: Opinion and Reaction Results from a Multi-Country Poll. 12—14 March 2020. 2020. Available online: https://www.ipsos.com/sites/default/files/ct/news/documents/2020-03/tracking-the-coronaviruswave-4-ipsos.pdf (accessed on 25 March 2020).
- Stata Corp. Stata Statistical Software: Release 15; Stata Corp LLC: College Station, TX, USA, 2017. [Google Scholar]
- Stats, S.A. Mid-Year Population Estimates 2021; Statistics South Africa: Pretoria, South Africa, 2021. [Google Scholar]
- ESRI. What’s New in ArcGIS Enterprise 10.8? California: United States of America. 2020. Available online: https://www.esri.com/arcgis-blog/products/arcgis-enterprise/announcements/whats-new-in-arcgis-enterprise-10-8/ (accessed on 20 August 2021).
- Schober, P.; Vetter, T.R. Logistic regression in medical research. Anesth. Analg. 2021, 132, 365–366. [Google Scholar]
- Bartlett, J. Estimating Risk Ratios from Observational Data in Stata. 2015. Available online: https://thestatsgeek.com/2015/03/09/estimating-risk-ratios-from-observational-data-in-stata/ (accessed on 25 January 2023).
- Ranganathan, P.; Aggarwal, R.; Pramesh, C.S. Common pitfalls in statistical analysis: Odds versus risk. Perspect. Clin. Res. 2015, 6, 222–224. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. The odds ratio. BMJ 2000, 320, 1468. [Google Scholar] [CrossRef]
- He, K.; Mack, W.J.; Neely, M.; Lewis, L.; Anand, V. Parental perspectives on immunizations: Impact of the COVID-19 pandemic on childhood vaccine hesitancy. J. Community Health. 2022, 47, 39–52. [Google Scholar] [CrossRef]
- Nelson, R. COVID-19 disrupts vaccine delivery. Lancet Infect Dis 2020, 20, 546. [Google Scholar] [CrossRef]
- Shet, A.; Carr, K.; Danovaro-Holliday, M.C.; Sodha, S.V.; Prosperi, C.; Wunderlich, J.; Wonodi, C.; Reynolds, H.W.; Mirza, I.; Gacic-Dobo, M.; et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: Evidence of disruption and recovery from 170 countries and territories. Lancet Glob. Health 2022, 10, e186–e194. [Google Scholar] [CrossRef]
- WHO and UNICEF Warn of a Decline in Vaccinations during COVID-19. 2020. Available online: https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19 (accessed on 18 July 2022).
- Bell, S.; Clarke, R.; Paterson, P.; Mounier-Jack, S. Parents’ and guardians’ views and experiences of accessing routine childhood vaccinations during the coronavirus (COVID-19) pandemic: A mixed methods study in England. PLoS ONE 2020, 15, e0244049. [Google Scholar] [CrossRef]
- Shati, A.A.; Al-Qahtani, S.M.; Alsabaani, A.A.; Mahmood, S.E.; Alqahtani, Y.A.; AlQahtani, K.M.; Aldarami, M.S.; Fahad, D.; AlAmri, F.D.; Alqahtani, A.S.; et al. Perceptions of parents towards COVID-19 vaccination in children, Aseer Region, Southwestern Saudi Arabia. Vaccines 2022, 10, 1222. [Google Scholar] [CrossRef]
- Turok, I. Urbanization. In The Oxford Companion to Economics in South Africa; Bhorat, H., Hirsch, A., Kanbur, R., Ncube., M., Eds.; Oxford University Press: Oxford, UK, 2014; pp. 360–365. [Google Scholar]
- Weir-Smith, G.; Mokhele, T.; Dlamini, S. National Health Insurance in the face of COVID-19: Urban tendencies in South Africa. S. Afr. Geogr. J. 2022, 104, 276–290. [Google Scholar] [CrossRef]
- Laituri, M.; Richardson, R.B.; Kim, J.; Cline, L.V.; Viscuso, S.; Schwartz, L. Examining second-order impacts of COVID-19 in urban areas. Annals GIS 2022, 28, 479–490. [Google Scholar] [CrossRef]
- Evans, S.; Klas, A.; Mikocka-Walus, A.; German, B.; Rogers, G.D.; Ling, M.; Fernando, J.W.; Kothe, E.; Westrupp, E.M. “Poison” or “protection”? A mixed methods exploration of Australian parents’ COVID-19 vaccination intentions. J. Psychosom. Res. 2021, 150, 110626. [Google Scholar] [CrossRef]
- Celik, M.Y. The thoughts of parents to vaccinate their children against COVID-19: An assessment of situations that may affect them. J. Child Adolesc. Psychiatr. Nurs. 2022, 35, 189–195. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).