Abstract
The rapid development of the vaccine and the infodemia have challenged communication about COVID-19 vaccines. This study aims to characterize—through the experience of vaccinators—the challenges faced during COVID-19 vaccination consultations and the communication strategies adopted. A qualitative study was conducted on COVID-19 vaccinators in Tuscany, Italy. Face-to-face interviews were conducted and examined by thematic analysis. In total, 30 vaccinators were interviewed. Four main themes emerged. The first highlighted distinct profiles of users’ attitudes toward COVID-19 vaccination. Barriers and promoters of vaccine uptake emerged in the second theme: concerns over the vaccine, excessive exposure to information, and a lack of clear guidance from institutions were the main factors behind hesitancy. The third theme highlighted users’ information-seeking behaviors; vaccinators observed that users ideologically opposed to the vaccine (IOV) unconsciously seek information that confirms their theories. The last theme comprised communication strategies for dealing with hesitancy. Empathy, first-hand examples, transparency, and tailored communication style appear to be effective in building vaccine trust. Lastly, the impossibility of developing a decision-making partnership with IOVs was noticed. These findings may help to better characterize public attitudes toward COVID-19 vaccination and highlight key communication principles and strategies to foster vaccine confidence.
1. Introduction
Vaccination is the main tool for the primary prevention of infectious diseases and among the most cost-effective public health measures available [1]; the immunization of the population not only reduces the spreading of diseases and prevents people from severe consequences of the diseases but also considerably reduces public spending on health [2]. Although vaccines are one of the most significant achievements of public health, and their benefits outweigh their risks for the majority of the population, increasing hesitation and refusal of vaccination have been reported all over the world [3]. In 2019, the World Health Organization (WHO) declared vaccine hesitancy among the ten most influential global health threats [3]. During the COVID-19 pandemic, many healthcare workers found themselves unprepared to deal with user rejection and scepticism. Despite the high case fatality rate, the overwhelming overload of patients’ admissions to hospitals, and the efforts made by the public health authorities, vaccine hesitancy towards COVID-19 vaccines was frequently reported [4,5].
Numerous factors have influenced the level of trust and adherence of the population to the vaccine campaign and to other mitigation measures for COVID-19; in particular, the novelty of the disease, the unusually rapid vaccine development, the use of new vaccine technologies, and the rapid and uncontrolled spreading of information and misinformation (i.e., “infodemia”) were reported among the main factors [6]. Furthermore, the highly evolutive scenario and the rapid evolution of evidence obliged governments and institutions to recurrent changes of course and forced healthcare workers to daily adaptations, further alimenting confusion in the population [7].
During the COVID-19 vaccination campaign, healthcare workers, who represented the main point of contact for the population, faced a threefold challenge: adapting to government and institutional directives, justifying the uncertainty to users, and confronting a more vaccine-hesitant population. Evidence shows that frontline healthcare workers are among the most trusted sources of vaccination information and advice, and thus, one of the main factors in the success/failure of a vaccination program [8]. Multiple studies demonstrated that receiving pertinent information from healthcare workers helps hesitant users in developing vaccine awareness and increases vaccine acceptance [9,10,11].
Carefully planned and proactive communication is one of the principal tools at the disposal of healthcare workers to improve vaccine acceptance during vaccination consultation [12,13]; effective communication helps to hinder misinformation and anti-immunization messages [14]. The COVID-19 pandemic indicated that this tool is—more than ever—essential to creating demand for preventive services. Before the pandemic, research concerning health communication mainly focused on childhood vaccination or health communication in general [15,16,17,18]; only a few analyzed vaccination campaigns carried out on the adult population [19,20], and the case of health communication about COVID-19 vaccine is pretty unique in various perspectives, as mentioned above.
In order to deal with hesitancy and vaccination refusal, it is of pivotal importance—both for institutions and healthcare workers—to develop communication strategies based on the experiences of those who worked on the front line during the vaccination campaign. Indeed, vaccinators represent a privileged point of view that may allow us to capture the different nuances of vaccine attitudes of users throughout the vaccination campaign and identify the determinants associated with them. Furthermore, through their experience, it is possible to comprehend the communication needs of different categories of users and define which strategies were the most effective during the evolving epidemic context. Therefore, the present study aimed to characterize public attitudes toward COVID-19 vaccination faced by vaccinators and factors influencing vaccine confidence and identify communication strategies adopted during vaccination consultation by vaccinators.
2. Materials and Methods
The study was conducted according to the Helsinki principles, and informed consent was obtained from all subjects involved in the study.
2.1. Setting, Design and Population
Italy has been one of the first European countries to be severely hit by the COVID-19 pandemic [21]. To contain the spread of the virus, the Italian government established a national lockdown from 10 March to 4 May 2020 [22]. The subsequent months of 2020 were characterized by the gradual reopening of services, but physical distancing rules and face masks remained mandatory [23]. The vaccination campaign started on 27 December 2020 [24], and it was organized according to the National Strategic Vaccine Plan for the Prevention of SARS-CoV-2 Infections, which gave priority to the elderly and the frail [25]. Once more vaccine doses became available, the vaccination campaign gradually extended the age groups for which it was possible to get the vaccine; on 16 June 2021, the vaccination was opened to anyone over the age of 16.
This qualitative study was conducted on a sample of healthcare workers involved in the COVID-19 immunization campaign in the Tuscany Region (the Province of Florence, Province of Pisa, Province of Grosseto, and the Province of Pistoia); in particular, vaccinators from different services were recruited: mass-vaccination campaigns (HUB), general practices (in the first phase of the vaccination campaign, general practitioners (G.P.) vaccinated the frail and elderly, and subsequently, other users, too), hospital vaccination services (in charge of vaccinating healthcare workers and frail inpatients), and USCA services (Unità Speciali di Continuità Assistenziale—special continuity care units, a service in charge of the vaccination of frail people at home and in nursing homes, as well as of refugee and migrant populations).
Purposive sampling was used in order to select participants from the different services according to the following urbanization level areas: urban areas, suburban areas or rural areas. Participants were asked to check their records about COVID-19 vaccination; G.P. participants were also asked to check records about patients enrolled in their practice. Vaccinators who had performed at least 1000 vaccination consultations and general practitioners who had at least 750 patients registered in their practice were included. Furthermore, in order to cover distinct phases of the vaccination campaign and the COVID-19 epidemic, vaccinators who did not take part continuously (at least 12 months) in the vaccination campaign were excluded. The participant recruitment was stopped when thematic saturation was reached; this was discussed and agreed upon among the authors. Participants were contacted and interviewed between April and November 2022.
2.2. Data Collection, Processing and Analysis
All participants were informed about the purpose of the study, and informed consent was obtained from all of them prior to their participation in the study. Data were collected through in-depth face-to-face interviews jointly conducted by two researchers (G.A.; M.F.C.). No relationship was established prior to the study commencement between participants and interviewers. The research team developed a semi-structured interview to explore the following domains: users’ information-seeking behaviors, perception of COVID-19 vaccination, and communication strategies implemented during consultation. The interviews lasted for about one hour. In order to test the interview guide, a pilot test was conducted; interviewers were trained not to suggest value judgements.
All the interviews were audio recorded and transcribed verbatim; no notes were taken during the interviews by the interviewers. Participants were informed that data from interviews would be collected in an anonymous form. To examine the content of the corpus, an inductive thematic analysis was conducted. The first phase included repeated readings of the interviews to familiarize the interviewers with the data. Subsequently, a coding framework (codebook) was developed to organize the data-coding process. After the examination of the codes, the subsequent step involved the identification of the themes emerging from the data. Codes and themes were identified from the data by three authors (G.A.; M.F.C.; P.B.) independently and revised jointly. Disagreements on coding and themes were resolved involving a fourth author (V.L.) where necessary. The names of themes to be included in the final report have been reviewed by all the researchers. To facilitate data management and coding, the transcripts were uploaded and analysed with Iramuteq software (GNU General Public License version 2, GPLv2).
Furthermore, determinants of vaccine acceptance/hesitancy concerning COVID-19 vaccination that emerged from interviews were identified and traced back to the conceptual model developed by the WHO Strategic Advisory Group of Experts (SAGE) [16]. Specifically, this model identifies three macro groups of factors influencing the vaccine decision-making process: individual and group influences, contextual factors, and vaccine/vaccination-specific issues. The definition of determinants of vaccine hesitancy applied was “concepts relating to barriers and enablers for uptake, reasons for vaccination refusal, beliefs and attitudes towards vaccination and system mediated factors” [26].
3. Results
The interviews were submitted to a total of 30 vaccinators (46.7% female) aged between 25 and 71 years old. The characteristics of the vaccinators are summarized in Table 1. Table S1 reports the characteristics of the vaccinators at an individual level.

Table 1.
Study sample characteristics.
From the inductive thematic analysis of the interviews, four main themes emerged; below, the four identified themes are summarized.
3.1. Theme 1—Users’ Attitudes towards COVID-19 Vaccination
Interviews with vaccinators revealed six categories of users’ vaccine attitudes: eager to get vaccinated, compliant with the recommendations, information/reassurance seekers, wait-and-seers, unwillingly vaccinated to avoid work and social restrictions, and ideologically opposed to the vaccine.
The respondents reported that the preponderance of the population was eager to get vaccinated; this attitude was related to a generally high level of confidence in the health system, science and vaccine efficacy and was observed particularly in the elderly and young adults for different underlying reasons, i.e., perceived susceptibility to COVID-19 and regaining social life, respectively.
Users compliant with the recommendations were described as those who were vaccinated on time without any doubt or concern and who did not want any further information, mainly because they trusted science and were willing to pursue their duty as citizens.
Other users delayed vaccination for fear of the vaccine; two distinct categories of such hesitant users were described: reassurance seekers and wait-and-seers. The first group openly shared their fears during the consultation, while the wait-and-seers were those mainly observed in the early phases of the vaccination campaign who waited to see the effects of the vaccine on those who received it; a substantial distrust in science and institutions was at the basis of this attitude. Lastly, some users reported a high level of mistrust in the health system and institutions and believed in conspiracy theories. These users frequently did not trust the scientific community even before the pandemic; the rapidly evolving scientific evidence and contradictory directives for pandemic management exacerbated this attitude. Some of these users eventually became vaccinated to avoid work and social restrictions, while others firmly pursued their beliefs and never became vaccinated. Generally, users belonging to these two categories were middle-aged, had an average to good education level, and belonged to the middle socio-economic class. The most relevant quotations for this theme are summarized in Table 2.

Table 2.
Illustrative quotes for theme 1, “users’ attitudes towards COVID-19 vaccination”.
3.2. Theme 2—Factors Influencing Vaccine Confidence
3.2.1. Sub-Theme 2.1—Determinants of Vaccine Hesitancy: Individual and Group Influence; Contextual Influences; Vaccine/Vaccination Specific Issues
All the determinants of vaccine hesitancy and confidence that emerged from the interviews were categorized according to the SAGE Working Group model. Factors identified as either barriers or promoters of vaccine confidence are shown in Table 3.

Table 3.
Factors identified in the interviews as either barriers (B) to or promoters (P) of COVID-19 vaccination and mapped onto the SAGE Working Group model of determinants of vaccine hesitancy.
The main barriers which lowered vaccine confidence were related to the rapid development of a new vaccine and the general belief that there were not enough clinical trials to guarantee vaccine safety. In particular, a widespread tendency among users has been to implement a heuristic risk-benefit calculation rather than one based on scientific evidence. Moreover, excessive exposure to mass-media information and a lack of clear guidance from institutions fostered users’ concerns (see theme 3).
COVID-19 normative/institutional restrictions, perceived disease severity, mode of delivery and accessibility of COVID-19 preventive services were identified as major promoters.
Lastly, socio-economic, religious, and cultural factors, as well as sex, did not emerge as significant determinants. The most relevant quotations for this subtheme are summarized in Table 4.

Table 4.
Illustrative quotes for theme 2, “factors influencing vaccine confidence”.
3.2.2. Sub-Theme 2.2—Changes in User Vaccine Confidence over the Course of the Vaccination Campaign
Vaccinators reported an evolution of users’ vaccine confidence during the different pandemic phases. In the early stages of the pandemic, when the vaccine was not yet developed, the perception of the disease severity was very high, and people strongly desired the possibility of having an effective vaccine. This explains the positive attitude observed at the beginning of the vaccination campaign. Vaccine confidence increased even more during the first phases of the vaccination campaign as more users became vaccinated without relevant side effects reported. In the subsequent stages, vaccine confidence increase was hampered and probably reversed due to various reasons. The first was related to the report of some cases of severe vaccine side effects amplified by the mass media. The second was the presence of different types of vaccines, with some believed to be safer or more effective; this generated a widespread willingness to opt for the preferred one, even though it was not possible to choose among vaccines. The third is related to the reduced perception of COVID-19 disease severity when a high level of immunization coverage in the population was reached. The fourth is related to the misleading messages—both from mass media and institutions—regarding the fact that the vaccine could protect from contracting the infection led to an increase in vaccine hesitation when infections in vaccinated people were raised. Furthermore, pandemic fatigue led to a general demotivation toward recommended preventive measures, including vaccination. In the most recent stages of the vaccination campaign, with the almost complete removal of containment measures and the return to a pre-COVID-19 social life, vaccination was perceived as safe as other routine vaccinations. The most relevant quotations for this subtheme are summarized in Table 4.
3.3. Theme 3—Information and Health Communication
3.3.1. Sub-Theme 3.1—COVID-19 Vaccine Knowledge and Information-Seeking Behaviors
Interviews highlighted that users generally utilized horizontal communication channels (i.e., mass media, social media, friends and relatives) and very few used vertical and official communication channels (i.e., responsible institutions). In this context, the main source of information for the elderly were mass media, general practitioners, and relatives, while the Internet and social media were mainly used by the young and middle-aged population groups; the population group aged 45–60 years was perceived more vulnerable to the Internet and social media misinformation. Some vaccinators observed that a frequent information-seeking behavior unconsciously applied by users was picking the sources that confirmed their presumptions and avoiding the ones that could refute or belittle their beliefs (i.e., “cherry picking”); this caused a bias and led an individual to validate the desired thesis, even when false. Interestingly, interviewees noticed that, although this phenomenon was common to most users, it was stronger in those who showed contrary or distorted ideas about vaccination.
Lastly, vaccinators from the HUB service highlighted that adherence to the vaccination campaign could have benefited from a more proactive contribution in terms of vaccine advocacy from the general practitioners, especially in people aged below 60 years. Indeed, it was reported that they would have benefited—both in terms of user vaccine confidence and time spent in consultation—by also having these users previously informed by the most proximal and trusted health information source, i.e., the general practitioner. The most relevant quotations for this subtheme are summarized in Table 5.

Table 5.
Illustrative quotes for theme 3, “information and health communication”.
3.3.2. Sub-Theme 3.2—The Impact of Institutional and Media Communication on Users’ Vaccine Perception and the Related Consequences on Vaccinators
Vaccinators perceived that users had access to an enormous quantity of information about the COVID-19 vaccine and that the vaccine topic became of public wisdom as never before. A discrete proportion of users were reported to be highly impacted by this unfiltered amount of information, misinformation, and disinformation; this fuelled uncertainty, a general sense of helplessness, and, consequently, fertile ground for vaccine hesitancy and conspiracy theories.
Furthermore, vaccinators reported a lack of guidance from institutions in terms of crisis communication to the population; users were confused by the inconsistency and the rapidly evolving institutional directives on the pandemic and vaccine campaign. This, together with the infodemia, further increased mistrust and vaccine hesitation and undermined the credibility not only of the institutions but also of the vaccinators, who have felt abandoned in the task of informing users. Vaccinators noticed that more consistent, transparent, and coordinated communication from the involved public institutions would have been fundamental to strengthening population trust and reducing the opportunity for rumours to spread, ultimately facilitating their work. Lastly, vaccinators highlighted the limits of the COVID-19 vaccine communication campaign that addressed the entire population indiscriminately, leaving a sense of vagueness. The most relevant quotations for this subtheme are summarized in Table 5.
3.4. Theme 4—Principles and Strategies for Dealing with Vaccine Hesitancy and Refusal
All the vaccinators reported that their professional opinion matters, and they felt influential in the user decision-making process. Several communication strategies for dealing with hesitant users emerged from the interviews; key principles and effective communication strategies for dealing with hesitant users were mainly inherent in the following areas:
- Empathy: it emerged how crucial it was to have active and non-judgmental listening, to make the user feel understood, and to ask for users’ feedback about the information provided during the consultation. Furthermore, putting themselves on the same level as the user was regarded as a useful strategy by several vaccinators, with some of them saying that sharing their own experience and initial concerns about the vaccine reassured hesitant users. Lastly, another strategy reported to reassure hesitant users was to involve other users’ trusted medical health professionals so as to make them feel truly heard and understood.
- Transparency: transparency and honesty about scientific evidence was deemed essential to establishing a relationship of trust with users. Furthermore, it highlighted the importance of clearly admitting the uncertainty of evidence when they were not strong enough. This situation occurred, for example, in the case of the vaccination of pregnant women at the beginning of the vaccination campaign.
- Highlighting the balance between risks and benefits: vaccinators found it useful to stress the high level of vaccine efficacy and safety on the one hand while highlighting the risk of getting COVID-19 on the other hand. The use of everyday life examples, such as pointing out that the COVID-19 vaccine had similar or fewer risks than other commonly used drugs, was useful in overcoming fear and hesitation. Since one of the most common fears was the unknown long-term effects of the vaccine, pointing out that COVID-19 also may have long-term effects was proven useful. Furthermore, highlighting specific aspects in terms of personal or familiar clinical risks helped to make users understand that vaccination is particularly useful for their case.
- Adopting a personalized approach: a user-centered approach was frequently mentioned in dealing with vaccine hesitancy. This required exploring reasons behind hesitancy without being judgmental and understanding the user’s belief and attitude toward health and vaccines in order to adapt the communication style. If the user shows beliefs and values in line with vaccine recommendations, reporting scientific data and evidence was reported to be persuasive; in the case of contrasting convictions, emotional stories were reported to be more effective.
Lastly, many vaccinators pointed out that explaining the importance of vaccination in order to achieve community immunity (i.e., collective responsibility) did not influence the vaccination choices; moreover, all the vaccinators did not use or share communication-supportive materials during the consultation since they noticed that users preferred to hear information directly from them.
As for users ideologically opposed to the vaccine, two different cases of dealing with this category emerged: the case in which they were actively called by their physician to receive the vaccination and the case in which they spontaneously came up to the vaccination HUB (usually merely to protest). In both cases, they were not open to discussion, hardly or never deviated from their beliefs, and sometimes verbally harassed vaccinators. Apparently, there is no effective communication strategy for developing an informed decision-making partnership. Interestingly, in the case of the general practitioners, the divergent opinions on the vaccine with users ideologically opposed did not hamper the patient-physician relationship in other health areas as mainly they believed that the G.P. themself was a victim of a conspiracy from institutions/pharmaceutical companies. Given the high levels of tension involved in the conversations with this type of user, avoiding dismissing and debating and instead providing clear and concise recommendations was deemed essential as a first approach to building trust; this may help in creating further opportunities to discuss the vaccination more openly. The most relevant quotations for this theme are summarized in Table 6.

Table 6.
Illustrative quotes for theme 4, “principles and strategies for dealing with vaccine hesitancy and refusal”.
4. Discussion
Several studies demonstrated that receiving pertinent information from health operators may increase vaccine acceptance [8,9,10,11]. Through the experiences of vaccinators, this study aimed to characterize public attitudes toward COVID-19 vaccination and the communication strategies adopted during vaccination consultations. The study was based on face-to-face in-depth interviews with vaccinators who had continuously worked during the different stages of the COVID-19 vaccination campaign for at least 12 months so as to draw evidence from a privileged viewpoint on the attitudes and beliefs of the population and on effective strategies for vaccine communication with users. The content analysis of the interviews highlighted four themes; the first and second themes described users’ attitudes towards COVID-19 vaccination and barriers or promoters influencing their decision-making about the vaccine. The third theme highlighted the information-seeking behaviors of users and the impact that the “infodemia” had on user vaccine confidence; and lastly, in the fourth theme, communication principles and strategies for dealing with vaccine hesitancy and refusal emerged.
The interviews revealed several profiles of users’ attitudes toward COVID-19 vaccination. The profiles described reflect the vaccine hesitancy continuum model described for routine vaccinations [13], with some specificities related to the case of the COVID-19 vaccine. Indeed, the rapid development of the vaccine and the new vaccine technology are probably the main underlying reasons behind the wait-and-see attitude observed in some users, while the stringent work and social restrictions foreseen for the unvaccinated had forced some of the more reluctant users to put aside their beliefs and become vaccinated. Furthermore, the mass vaccination campaign and the high media coverage had probably pushed, on the one hand, more people to get vaccinated, while on the other hand, it increased hesitancy in some users due to the infodemia.
Interestingly, all the vaccinators described a similar trend of vaccine confidence over the course of the vaccination campaign (depicted in Figure 1); vaccine confidence was reported to be high at the start of the campaign and to increase during the first phases—in this context, it should be taken into account that Italy was one the first western countries to be severely hit by the spread of the pandemic [22,27,28]; then, this trend stopped and reversed for several reasons, some directly related to the advancement of the vaccine campaign (the appearance of the first vaccine adverse events and the reduced perception of the disease severity due to the high level of vaccine coverage) and other external factors (i.e., misinformation/disinformation and pandemic fatigue) [29]. With the return to a pre-COVID-19 situation, the COVID-19 vaccine begins to be internalized by the population as a routine vaccination in terms of safety. These trends are of particular interest and should be taken into account, as they will presumably replicate in the event of future pandemics.
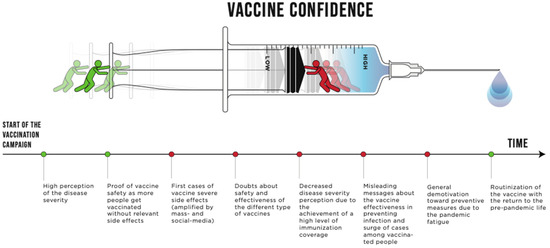
Figure 1.
Evolution of vaccine confidence over the course of the COVID-19 vaccination campaign.
Concerns over vaccine safety and fear of unknown long-term health consequences were among the main factors observed behind vaccine hesitancy for the COVID-19 vaccine. These factors were mainly related to the rapid development of the vaccine and to the novelty of the mRNA technology, as the main belief was that the vaccine had not been tested enough. These findings are in line with other studies carried out in different countries and settings [30,31,32,33,34]. Furthermore, socioeconomic, cultural factors and sex did not emerge as relevant determinants in our study; interestingly, studies from other high-income countries have observed a higher COVID-19 vaccine hesitancy in females, in people with lower levels of education, and in people not being of white ethnicity [30,35,36,37].
Findings also showed that these concerns and beliefs were highly exacerbated by the lack of clear guidance and communication from the government and competent health institutions and by the infodemia. Indeed, the experience of vaccinators highlighted that the COVID-19 pandemic had the characteristics—such as the novelty of the disease, the evolving situation, the need for rapid adaptations of policies and public health measures—to create fertile ground for the spread of rumour and that users were not able to navigate the huge amount of available information. Misinformation and disinformation created fears and discouraged people from their decision to get the vaccine [38,39,40]. Although the impact of fake news on vaccination campaigns has been widely observed in the context of other vaccines [41,42], during the pandemic, the viral spread of doubts travelled at unprecedented speed, especially on social media [43]. A more consistent and coordinated vaccine communication from the involved public institutions appeared to be fundamental to counter misinformation and to strengthen population trust. As seen in this pandemic and in other previous pandemics, feeling well-informed about the pandemic and establishing a relationship of trust between public institutions and the population seems to play a critical role in order to engage the population in vaccination campaigns [44,45,46,47].
During consultations with patients, vaccinators highlighted that their opinion matters and felt they were a trusted source of information for hesitant users. This finding confirms that first-line healthcare workers have a prominent role in guiding hesitant users and in increasing vaccine acceptance [8,9,10,11]. It has to be taken into account that healthcare workers in Italy had a positive public image during the pandemic, given their efforts during the health crisis and their great level of COVID-19 vaccination uptake—higher than in other high-income countries; this could have increased their credibility among the users [37,48,49,50]. Empathy, bringing first-hand and personal examples, exploring and legitimising patients’ fears (rather than dismissing them), and ensuring transparent communication appear to be effective in building trust and overcoming vaccine hesitancy. Moreover, a personalized approach and a tailored communication style according to the user attitudes and beliefs were other key principles that emerged in dealing with vaccine-hesitant users. These aspects are particularly important as risk perception—of both the disease and the vaccine—and vaccine hesitancy are multifaceted phenomena that are influenced by personal experiences and socio-cultural and economic backgrounds [51,52,53].
Interestingly, our findings clearly characterize a subgroup of users that were ideologically opposed to the vaccine; in line with other studies, our findings showed that these users had an a priori refusal of the vaccines, a high level of distrust in conventional medicine, health system and institutions, and a tendency to believe in conspiracy theories [54,55]. In this group of users, it seems that there was no room for discussing vaccination, sharing knowledge of the vaccine, and developing an informed decision-making partnership. Avoiding debating evidence, providing brief and clear recommendations, and being available for further consultations may be of help in establishing further occasions for discussing vaccination with this kind of user.
The present study had several strengths and limitations. As for the strengths, the maximum variation purposive sampling allowed to include the widest range of perspectives possible—i.e., vaccinators working with different types of users and in distinct services based in urban and rural contexts—so as to explore the topic from different angles and identify both common patterns and variations. Furthermore, the study included vaccinators that continuously vaccinated for at least one year; this allowed us to have a solid overall perspective on the evolution of vaccine confidence over time and on the challenges faced in the various vaccination campaign phases. As far as the limitations are concerned, the sample was selected from only one Italian region. Furthermore, as the study is based on data from face-to-face interviews, a social desirability tendency of participants cannot be dismissed; however, interview questions were specifically developed in order to be neutral, and interviewers were trained not to suggest value judgements or interpretations.
5. Conclusions
Our study explored the privileged viewpoint of vaccinators on the COVID-19 vaccine campaign. Our findings highlighted aspects and trends of user vaccine confidence that could recur in cases of future pandemics or rapid vaccine development, especially in the context of mass-vaccination campaigns and high public and media attention. At the population level, consistent, targeted and coordinated vaccine institutional communication is needed in order to build trust with the population and to empower the frontline healthcare workers involved in the vaccination campaign. At the individual level, our findings confirm that frontline operators are essential in dealing with vaccine hesitancy and in increasing vaccine acceptance. Several key communication principles and strategies were identified to foster vaccine confidence; while, although it may be proven difficult, avoiding debating and providing brief and clear recommendations may serve to start building trust with users ideologically opposed to the vaccine and to leave the door open for further occasions. Further studies that include user perspectives are needed in order to better identify leverages and strategies to engage with this population subgroup.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines11020223/s1, Table S1: Characteristics of the vaccinators at individual level.
Author Contributions
Conceptualization, G.A., M.F.C., P.B., M.J.C.P. and V.L.; methodology, G.A., M.F.C., P.B. and V.L.; formal analysis, G.A., M.F.C., P.B. and V.L.; investigation G.A., M.F.C., P.B., D.G., L.S. and V.L.; data curation, G.A., M.F.C. and V.L.; writing—original draft preparation, G.A., M.F.C. and V.L.; writing—review and editing P.B., L.S., D.G., C.L., G.B., M.J.C.P. and V.L.; supervision, M.J.C.P. and V.L.; project administration V.L.; funding acquisition, V.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research project is funded by the Tuscany region (Regione Toscana, Bando Ricerca COVID-19 Toscana, D.D. n. 17733 30 October 2020).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were not applicable as this is a qualitative study based on interviews collecting only professional experiences from healthcare workers.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. Data are not publicly available due to the current regulation on privacy.
Acknowledgments
This research project is funded by Tuscany Region (Regione Toscana, Bando Ricerca COVID-19 Toscana, D.D. n. 17733 30 October 2020). The authors want to thank Nuri Rashid for the help with data visualization for Figure 1.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Overview. Available online: https://health.ec.europa.eu/vaccination/overview_en (accessed on 28 November 2022).
- Cicchetti, A.; Ruggeri, M.; Gitto, L.; Mennini, F.S. Extending influenza vaccination to individuals aged 50–64: A budget impact analysis. Int. J. Technol. Assess. Health Care 2010, 26, 288–293. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 15 February 2022).
- Eriksson, C.O.; Stoner, R.C.; Eden, K.B.; Newgard, C.D.; Guise, J.-M. The Association Between Hospital Capacity Strain and Inpatient Outcomes in Highly Developed Countries: A Systematic Review. J. Gen. Intern. Med. 2016, 32, 686–696. [Google Scholar] [CrossRef]
- Trentini, F.; Marziano, V.; Guzzetta, G.; Tirani, M.; Cereda, D.; Poletti, P.; Piccarreta, R.; Barone, A.; Preziosi, G.; Arduini, F.; et al. Pressure on the Health-Care System and Intensive Care Utilization During the COVID-19 Outbreak in the Lombardy Region of Italy: A Retrospective Observational Study in 43,538 Hospitalized Patients. Am. J. Epidemiol. 2021, 191, 137–146. [Google Scholar] [CrossRef]
- Scherer, L.D.; Shaffer, V.A.; Patel, N.; Zikmund-Fisher, B.J. Can the vaccine adverse event reporting system be used to increase vaccine acceptance and trust? Vaccine 2016, 34, 2424–2429. [Google Scholar] [CrossRef]
- Chou, W.-Y.S.; Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, H.-J.; Booy, R.; Aston, R.; Van Damme, P.; Schumacher, R.F.; Campins, M.; Rodrigo, C.; Heikkinen, T.; Weil-Olivier, C.; Finn, A.; et al. How to optimise the coverage rate of infant and adult immunisations in Europe. BMC Med. 2007, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.; Schamel, J.; Fisher, A.; Frew, P.M. Influences on Immunization Decision-Making among US Parents of Young Children. Matern. Child Health J. 2017, 21, 2178–2187. [Google Scholar] [CrossRef] [PubMed]
- Gust, D.A.; Darling, N.; Kennedy, A.; Schwartz, B. Parents With Doubts About Vaccines: Which Vaccines and Reasons Why. Pediatrics 2008, 122, 718–725. [Google Scholar] [CrossRef]
- Goldstein, S.; MacDonald, N.E.; Guirguis, S. Health communication and vaccine hesitancy. Vaccine 2015, 33, 4212–4214. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Butler, R.; MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The Guide to Tailoring Immunization Programmes (TIP). Vaccine 2015, 33, 4176–4179. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control; Translating Health Communications Project Consortium. Systematic Literature Review of the Evidence for Effective National Immunisation Schedule Promotional Communications: Insights into Health Communication; Publications Office: Stockholm, Sweden, 2012. [Google Scholar]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Leask, J.; Kinnersley, P.; Jackson, C.; Cheater, F.; Bedford, H.; Rowles, G. Communicating with parents about vaccination: A framework for health professionals. BMC Pediatr. 2012, 12, 154. [Google Scholar] [CrossRef] [PubMed]
- WHO Strategic Communications Framework for Effective Communications. Geneva: World Health Organization. 2020. Available online: https://www.who.int/docs/default-source/documents/communicating-for-health/communication-framework.pdf (accessed on 28 November 2022).
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; et al. Strategies for Addressing Vaccine Hesitancy-A Systematic Review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Gagnon, D.; MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Cerqua, A.; Di Stefano, R. When did coronavirus arrive in Europe? Stat. Methods Appl. 2021, 31, 181–195. [Google Scholar] [CrossRef]
- Lastrucci, V.; Lorini, C.; Del Riccio, M.; Gori, E.; Chiesi, F.; Sartor, G.; Zanella, B.; Boccalini, S.; Bechini, A.; Puggelli, F.; et al. SARS-CoV-2 Seroprevalence Survey in People Involved in Different Essential Activities during the General Lock-Down Phase in the Province of Prato (Tuscany, Italy). Vaccines 2020, 8, 778. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Paoli, S.; Biamonte, M.A.; Moscadelli, A.; Baggiani, L.; Nerattini, M.; Lastrucci, V.; Zanobini, P.; Lorini, C. COVID-19 and schools: What is the risk of contagion? Results of a rapid-antigen-test-based screening campaign in Florence, Italy. Int. J. Infect. Dis. 2021, 112, 130–135. [Google Scholar] [CrossRef]
- Reno, C.; Sanmarchi, F.; Stoto, M.A.; Fantini, M.P.; Lenzi, J.; Golinelli, D. The impact of health policies and vaccine rollout on the COVID-19 pandemic waves in Italy. Health Policy Technol. 2022, 11, 100604. [Google Scholar] [CrossRef]
- Decreto Del Ministero Della Salute 12 Marzo 2021 (Approvazione Del Piano Strategico Nazionale Dei Vaccini per La Prevenzione Delle Infezioni Da SARS-CoV-2 Costituito Dal Documento Recante «Elementi Di Preparazione Della Strategia Vaccinale», Di Cui al Decreto 2 Gennaio 2021 Nonche’ Dal Documento Recante «Raccomandazioni Ad Interim Sui Gruppi Target Della Vaccinazione Anti SARS-CoV-2/COVID-19» Del 10 Marzo 2021); Istituto Poligrafico e Zecca dello Stato: Rome, Italy, 2021; Volume 21A01802.
- European Centre for Disease Prevention and Control. Let’s Talk about Hesitancy; ECDC: Stockholm, Sweden, 2016; Available online: https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/lets-talk-about-hesitancy-vaccination-guide.pdf (accessed on 28 November 2022).
- Lastrucci, V.; Collini, F.; Forni, S.; D’Arienzo, S.; Di Fabrizio, V.; Buscemi, P.; Lorini, C.; Gemmi, F.; Bonaccorsi, G. The indirect impact of COVID-19 pandemic on the utilization of the emergency medical services during the first pandemic wave: A system-wide study of Tuscany Region, Italy. PLoS ONE 2022, 17, e0264806. [Google Scholar] [CrossRef] [PubMed]
- Lastrucci, V.; Bonaccorsi, G.; Forni, S.; D’Arienzo, S.; Bachini, L.; Paoli, S.; Lorini, C.; Gemmi, F. The indirect impact of COVID-19 large-scale containment measures on the incidence of community-acquired pneumonia in older people: A region-wide population-based study in Tuscany, Italy. Int. J. Infect. Dis. 2021, 109, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, 210–221. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2021, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348, Correction in 2021, 5, 960. [Google Scholar] [CrossRef] [PubMed]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef]
- Lee, S.K.; Sun, J.; Jang, S.; Connelly, S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci. Rep. 2022, 12, 13681. [Google Scholar] [CrossRef]
- Rhodes, A.; Hoq, M.; Measey, M.-A.; Danchin, M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2020, 21, e110. [Google Scholar] [CrossRef]
- Momplaisir, F.; Haynes, N.; Nkwihoreze, H.; Nelson, M.; Werner, R.M.; Jemmott, J. Understanding Drivers of COVID-19 Vaccine Hesitancy Among Blacks. Clin. Infect. Dis. 2021, 73, 1784–1789. [Google Scholar] [CrossRef]
- Aw, J.; Seng, J.J.B.; Seah, S.S.Y.; Low, L.L. COVID-19 Vaccine Hesitancy—A Scoping Review of Literature in High-Income Countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef] [PubMed]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarðsson, V.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef] [PubMed]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.A.; Failla, G.; Puleo, V.; Melnyk, A.; Lontano, A.; Ricciardi, W. Social media and attitudes towards a COVID-19 vaccination: A systematic review of the literature. Eclinicalmedicine 2022, 48. [Google Scholar] [CrossRef] [PubMed]
- Aquino, F.; Donzelli, G.; De Franco, E.; Privitera, G.; Lopalco, P.L.; Carducci, A. The web and public confidence in MMR vaccination in Italy. Vaccine 2017, 35, 4494–4498. [Google Scholar] [CrossRef] [PubMed]
- Gahr, P.; DeVries, A.S.; Wallace, G.; Miller, C.; Kenyon, C.; Sweet, K.; Martin, K.; White, K.; Bagstad, E.; Hooker, C.; et al. An Outbreak of Measles in an Undervaccinated Community. Pediatrics 2014, 134, e220–e228. [Google Scholar] [CrossRef]
- Jama, A.; Ali, M.; Lindstrand, A.; Butler, R.; Kulane, A. Perspectives on the Measles, Mumps and Rubella Vaccination among Somali Mothers in Stockholm. Int. J. Environ. Res. Public Health 2018, 15, 2428. [Google Scholar] [CrossRef]
- Van Der Linden, S.; Roozenbeek, J.; Compton, J. Inoculating Against Fake News About COVID-19. Front. Psychol. 2020, 11, 566790. [Google Scholar] [CrossRef]
- Gilles, I.; Bangerter, A.; Clémence, A.; Green, E.G.T.; Krings, F.; Staerklé, C.; Wagner-Egger, P. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur. J. Epidemiol. 2011, 26, 203–210. [Google Scholar] [CrossRef]
- Gangarosa, E.; Galazka, A.; Wolfe, C.; Phillips, L.; Miller, E.; Chen, R. Impact of anti-vaccine movements on pertussis control: The untold story. Lancet 1998, 351, 356–361. [Google Scholar] [CrossRef]
- Ruiz, J.B.; Bell, R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef]
- Chanel, O.; Luchini, S.; Massoni, S.; Vergnaud, J.-C. Impact of information on intentions to vaccinate in a potential epidemic: Swine-origin Influenza A (H1N1). Soc. Sci. Med. 2011, 72, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.P.; Stefanizzi, P.; Brescia, N.; Lattanzio, S.; Martinelli, A.; Tafuri, S. COVID-19 vaccination hesitancy in Italian healthcare workers: A systematic review and meta-analysis. Expert Rev. Vaccines 2022, 21, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Aw, J.; Seah, S.S.Y.; Seng, B.J.J.; Low, L.L. COVID-19-Related Vaccine Hesitancy among Community Hospitals’ Healthcare Workers in Singapore. Vaccines 2022, 10, 537. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Behavioural Considerations for Acceptance and Uptake of COVID-19 Vaccines: WHO Technical Advisory Group on Behavioural Insights and Sciences for Health, Meeting Report, 15 October 2020; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/bitstream/handle/10665/337335/9789240016927-eng.pdf?sequence=1&isAllowed=y (accessed on 28 November 2022).
- Lastrucci, V.; Lorini, C.; Del Riccio, M.; Gori, E.; Chiesi, F.; Moscadelli, A.; Zanella, B.; Boccalini, S.; Bechini, A.; Puggelli, F.; et al. The Role of Health Literacy in COVID-19 Preventive Behaviors and Infection Risk Perception: Evidence from a Population-Based Sample of Essential Frontline Workers during the Lockdown in the Province of Prato (Tuscany, Italy). Int. J. Environ. Res. Public Health 2021, 18, 13386. [Google Scholar] [CrossRef]
- Lastrucci, V.; Lorini, C.; Stacchini, L.; Stancanelli, E.; Guida, A.; Radi, A.; Morittu, C.; Zimmitti, S.; Alderotti, G.; Del Riccio, M.; et al. Determinants of Actual COVID-19 Vaccine Uptake in a Cohort of Essential Workers: An Area-Based Longitudinal Study in the Province of Prato, Italy. Int. J. Environ. Res. Public Health 2022, 19, 13216. [Google Scholar] [CrossRef]
- Nicolo, M.; Kawaguchi, E.S.; Ghanem-Uzqueda, A.; Kim, A.E.; Soto, D.; Deva, S.; Shanker, K.; Rogers, C.; Lee, R.; Casagrande, Y.; et al. Characteristics associated with COVID-19 vaccination status among staff and faculty of a large, diverse University in Los Angeles: The Trojan Pandemic Response Initiative. Prev. Med. Rep. 2022, 27, 101802. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).