A Comparison of Strategies to Improve Uptake of COVID-19 Vaccine among High-Risk Adults in Nairobi, Kenya in 2022
Abstract
:1. Introduction
2. Materials and Methods
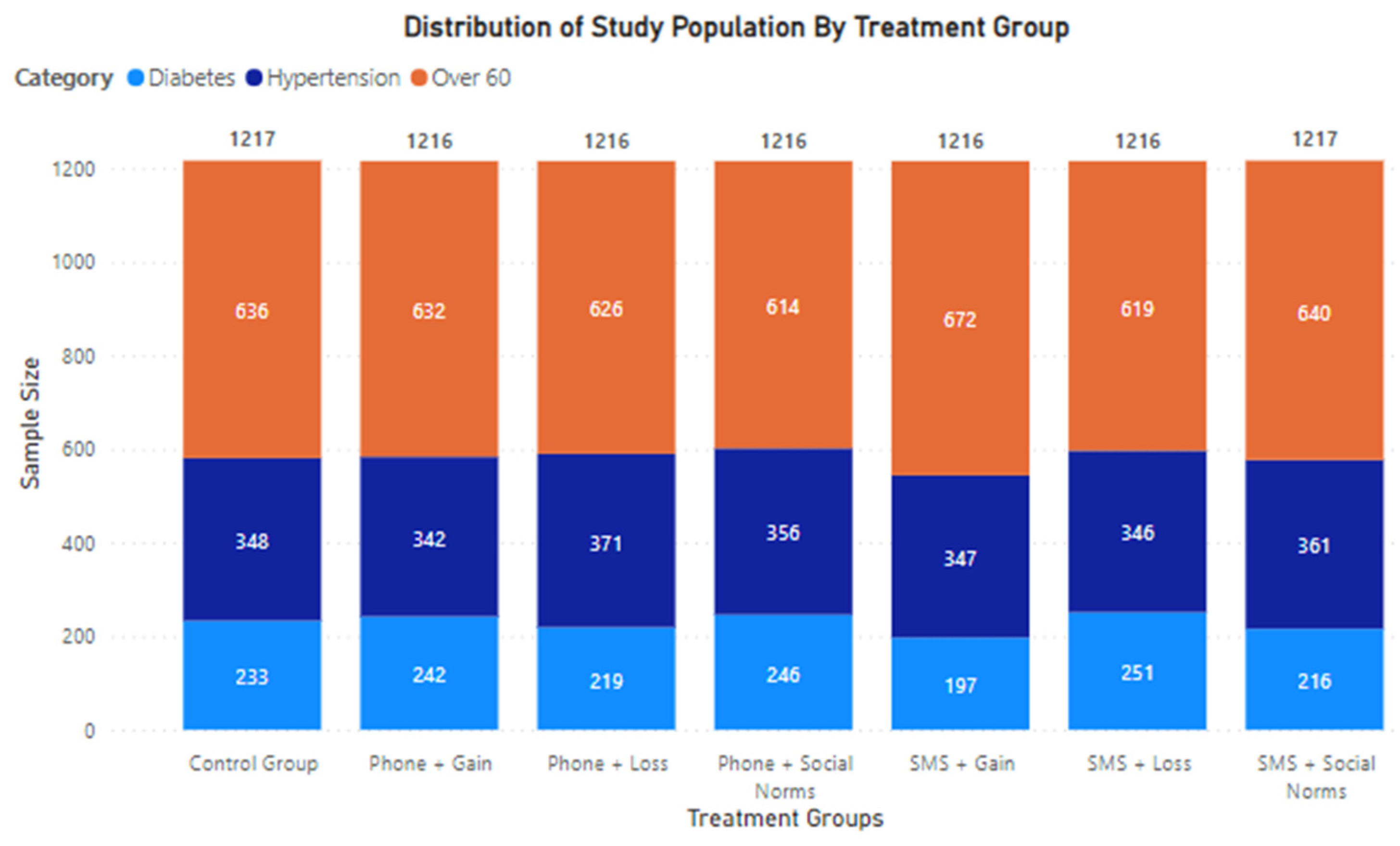
2.1. Patient Population and Sample Size
2.2. Intervention Channels
- (i)
- Outgoing Phone Calls: Patients in this treatment group received a phone call from a healthcare provider with the intended message. The phone calls were made by registered clinical officers fully employed at Penda’s Telemedicine Call Center. Calls were made using global call-center software (3CX, UK), and therefore appeared on patient phones as one consistent phone number that is known to be Penda’s contact number. If a patient could not be reached on the first attempt, health care providers would make at least one additional attempt later in the day. In the event of the patient calling back, the call would be routed to one of our healthcare providers to deliver the intended message.
- (ii)
- Bulk SMS Outreach: Patients in this treatment group received an SMS with the intervention message. SMSs were queued and loaded using a bulk messaging software (Africa’s Talking, Nairobi, Kenya) and were delivered on the same day.
2.3. Messaging Approaches
- (i)
- Gain Messaging: The focus of this approach was on highlighting a desirable or positive outcome of being vaccinated (e.g., spending time safely with family).
- (ii)
- Loss-Messaging: The focus of this approach was on emphasizing the undesirable or negative outcome of staying unvaccinated (e.g., the greater risk of negative health outcomes if you contract COVID-19 before having received the vaccine).
- (iii)
- Social proofing/norms: The focus in this approach was on relatability to actions by peers (e.g., many of your peers have already received the vaccine).
2.4. Treatment Groups
3. Results
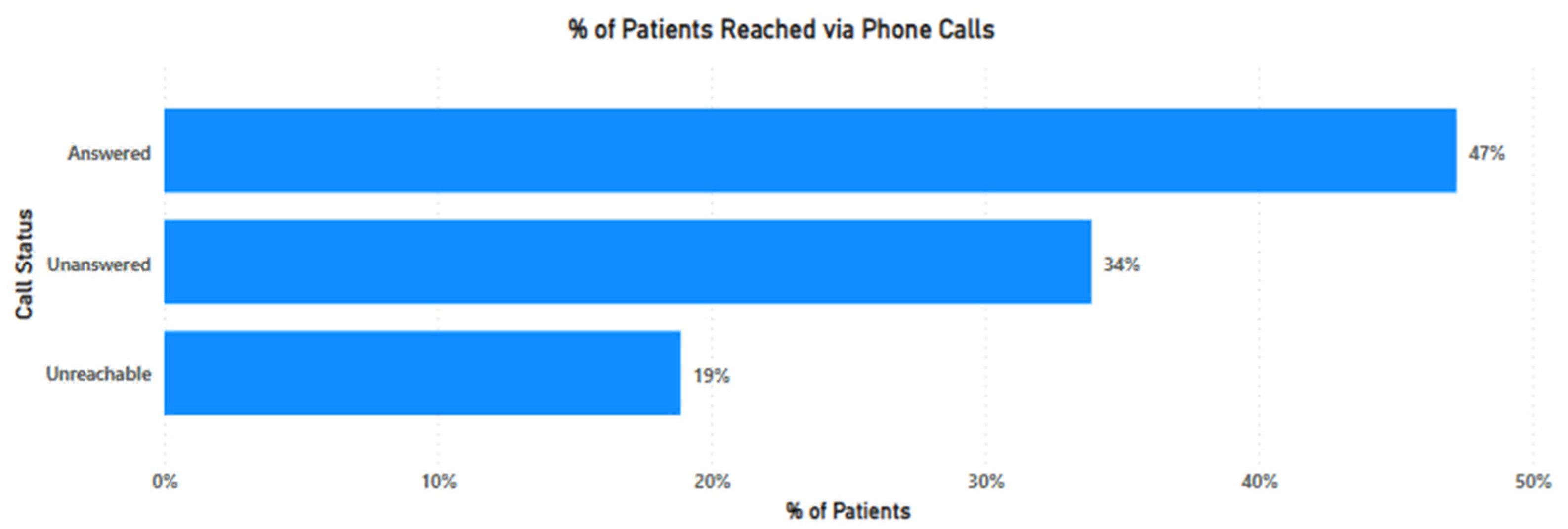
3.1. Reach via Phone Calls
3.2. Vaccination Status
3.3. SMS Intervention Channel
3.4. Overall Response to Call to Action
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. People with Certain Medical Conditions. 12 May 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 1 October 2022).
- Fekadu, G.; Bekele, F.; Tolossa, T.; Fetensa, G.; Turi, E.; Getachew, M.; Abdisa, E.; Assefa, L.; Afeta, M.; Demisew, W.; et al. Impact of COVID-19 pandemic on chronic diseases care follow-up and current perspectives in low resource settings: A narrative review. Int. J. Physiol. Pathophysiol. Pharmacol. 2021, 13, 86–93. [Google Scholar] [PubMed]
- Matta, S.; Chopra, K.K.; Arora, V.K. Morbidity and mortality trends of Covid 19 in top 10 countries. Indian J. Tuberc. 2020, 67, S167–S172. [Google Scholar] [CrossRef]
- Liu, B.; Spokes, P.; He, W.; Kaldor, J. High risk groups for severe COVID-19 in a whole of population cohort in Australia. BMC Infect. Dis. 2021, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E. Coronavirus Pandemic (COVID-19). 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 12 October 2022).
- Orenstein, W.A.; Bernier, R.H.; Dondero, T.J.; Hinman, A.R.; Marks, J.S.; Bart, K.J.; Sirotkin, B. Field evaluation of vaccine efficacy. Bull. World Health Organ. 1985, 63, 1055–1068. [Google Scholar] [PubMed]
- Sharif, N.; Alzahrani, K.J.; Ahmed, S.N.; Dey, S.K. Efficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. Front. Immunol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Vaccine Efficacy, Effectiveness and Protection. Available online: https://www.who.int/news-room/feature-stories/detail/vaccine-efficacy-effectiveness-and-protection (accessed on 8 October 2021).
- Holder, J. Tracking Coronavirus Vaccinations Around the World. 2022. Available online: https://www.nytimes.com/interactive/2021/world/covid-vaccinations-tracker.html (accessed on 23 October 2022).
- Patwary, M.M.; Alam, A.; Bardhan, M.; Disha, A.S.; Haque, Z.; Billah, S.M.; Kabir, P.; Browning, M.H.E.M.; Rahman, M.; Parsa, A.D.; et al. COVID-19 Vaccine Acceptance among Low- and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines 2022, 10, 427. [Google Scholar] [CrossRef] [PubMed]
- Reza, H.M.; Agarwal, V.; Sultana, F.; Bari, R.; Mobarak, A.M. Why are vaccination rates lower in low and middle income countries, and what can we do about it? BMJ 2022, 378, e069506. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.; Abeid, A.; Sharma, K.; Manji, S.; Nambafu, J.; Korom, R.; Patel, K.; Said, M.; Mohamed, M.A.; Sood, M.; et al. Perceptions and Knowledge towards COVID-19 Vaccine Hesitancy among a Subpopulation of Adults in Kenya: An English Survey at Six Healthcare Facilities. Vaccines 2022, 10, 705. [Google Scholar] [CrossRef] [PubMed]
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Available online: https://www.health.go.ke/ (accessed on 27 October 2022).
- Paltiel, A.D.; Schwartz, J.L.; Zheng, A.; Walensky, R.P.; Paltiel, A.D.; Schwartz, J.L.; Zheng, A.; Walensky, R.P. Clinical Outcomes of A COVID-19 Vaccine: Implementation Over Efficacy. Health Aff. 2021, 40, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Rutten, L.J.F.; Zhu, X.; Leppin, A.L.; Ridgeway, J.L.; Swift, M.D.; Griffin, J.M.; Sauver, J.L.S.; Virk, A.; Jacobson, R.M. Evidence-Based Strategies for Clinical Organizations to Address COVID-19 Vaccine Hesitancy. Mayo Clin. Proc. 2021, 96, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Limaye, R.J.; Balgobin, K.; Michel, A.; Schulz, G.; Erchick, D.J. What message appeal and messenger are most persuasive for COVID-19 vaccine uptake: Results from a 5-country survey in India, Indonesia, Kenya, Nigeria, and Ukraine. PLoS ONE 2022, 17, e0274966. [Google Scholar] [CrossRef] [PubMed]
- City Population. Available online: https://www.citypopulation.de/en/kenya/admin/nairobi/47__nairobi/ (accessed on 20 December 2022).
- Milkman, K.L.; Patel, M.S.; Gandhi, L.; Graci, H.N.; Gromet, D.M.; Ho, H.; Kay, J.S.; Lee, T.W.; Akinola, M.; Beshears, J.; et al. A megastudy of text-based nudges encouraging patients to get vaccinated at an upcoming doctor’s appointment. Proc. Natl. Acad. Sci. USA 2021, 118, e2101165118. [Google Scholar] [CrossRef] [PubMed]
- Kairu, A.; Were, V.; Isaaka, L.; Agweyu, A.; Aketch, S.; Barasa, E. Modelling the cost-effectiveness of essential and advanced critical care for COVID-19 patients in Kenya. BMJ Glob. Health 2021, 6, e007168. [Google Scholar] [CrossRef] [PubMed]

| Treatment Group | Intervention Channel | Messaging Approach | Script |
|---|---|---|---|
| Treatment Group 1 | Phone Call | Gain Messaging | The Coronavirus is still present and active. Vaccination not only reduces the risk of complications from the virus but also gives you the confidence to visit family, friends and loved ones without anxiety or fear. |
| Treatment Group 2 | Phone Call | Loss Messaging | The Coronavirus is still present and active. Studies show that those with underlying health conditions are more likely to suffer from severe infections, hospitalisations, and other serious health complications in the event that they contract COVID-19. |
| Treatment Group 3 | Phone Call | Social Norms | As of today, over 350 patients in our network of medical centers with chronic conditions such as hypertension, diabetes, kidney disease, etc. have been vaccinated against COVID-19. Have you received the vaccine? OR As of today, over 830 patients in our network of medical centers above the age of 60 have been vaccinated against COVID-19. Have you received the vaccine? |
| Treatment Group 3 | SMS | Gain Messaging | COVID-19 vaccination protects your health and gives you the confidence to visit family, friends and loved ones without anxiety or fear |
| Treatment Group 5 | SMS | Loss Messaging | Studies show that underlying health conditions are likely to trigger infections and health complications as a result of COVID-19 infections |
| Treatment Group 6 | SMS | Social Norms | Over 350 patients in our network of medical centers with chronic conditions such as hypertension, diabetes, kidney disease, etc. have been vaccinated against COVID-19 OR Message: Over 830 patients in our network of medical centers above the age of 60 have been vaccinated against COVID-19 |
| Messaging Approach | Total Unique Requests for Additional Information | As a % of Total SMS Sent |
|---|---|---|
| Gain Messaging | 14 | 1.15% |
| Loss-Messaging | 13 | 1.07% |
| Social Norms | 17 | 1.40% |
| Total | 44 | 1.21% |
| Intervention Channel | Messaging Approach | Total Sample Size | Sample Reached | Total Eligible Unvaccinated Patients | Converted Patients Within 1 Month | Conversion Rate |
|---|---|---|---|---|---|---|
| Phone Calls | Gain Messaging | 1216 | 583 | 84 | 0 | 0% |
| Loss-Messaging | 1216 | 555 | 110 | 3 | 2.37% | |
| Social Proofing | 1216 | 585 | 73 | 0 | 0% | |
| SMS | Gain Messaging | 1216 | n/a | n/a | 0 | 0% |
| Loss-Messaging | 1216 | n/a | n/a | 1 | 0.08% | |
| Social Proofing | 1217 | n/a | n/a | 0 | 0% | |
| Control Group | n/a | 1217 | n/a | n/a | 0 | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yego, J.; Korom, R.; Eriksson, E.; Njavika, S.; Sane, O.; Kanorio, P.; Rotich, O.; Wambui, S.; Mureithi, E. A Comparison of Strategies to Improve Uptake of COVID-19 Vaccine among High-Risk Adults in Nairobi, Kenya in 2022. Vaccines 2023, 11, 209. https://doi.org/10.3390/vaccines11020209
Yego J, Korom R, Eriksson E, Njavika S, Sane O, Kanorio P, Rotich O, Wambui S, Mureithi E. A Comparison of Strategies to Improve Uptake of COVID-19 Vaccine among High-Risk Adults in Nairobi, Kenya in 2022. Vaccines. 2023; 11(2):209. https://doi.org/10.3390/vaccines11020209
Chicago/Turabian StyleYego, Joan, Robert Korom, Emma Eriksson, Sharon Njavika, Oulimata Sane, Purity Kanorio, Oliver Rotich, Stellah Wambui, and Eunice Mureithi. 2023. "A Comparison of Strategies to Improve Uptake of COVID-19 Vaccine among High-Risk Adults in Nairobi, Kenya in 2022" Vaccines 11, no. 2: 209. https://doi.org/10.3390/vaccines11020209
APA StyleYego, J., Korom, R., Eriksson, E., Njavika, S., Sane, O., Kanorio, P., Rotich, O., Wambui, S., & Mureithi, E. (2023). A Comparison of Strategies to Improve Uptake of COVID-19 Vaccine among High-Risk Adults in Nairobi, Kenya in 2022. Vaccines, 11(2), 209. https://doi.org/10.3390/vaccines11020209






