Opinions, Attitudes and Factors Related to SARS-CoV-2 Vaccine Uptake in Eight South American Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Considerations and Informed Consent
2.2. Study Design and Participants
2.3. Statistical Analysis
3. Results
3.1. Participants’ Demographic Characteristics and COVID-19-Related Variables
3.2. Sources of COVID-19 Information
3.3. Perceptions about the Situation of the Country and the Discourse of the Authorities
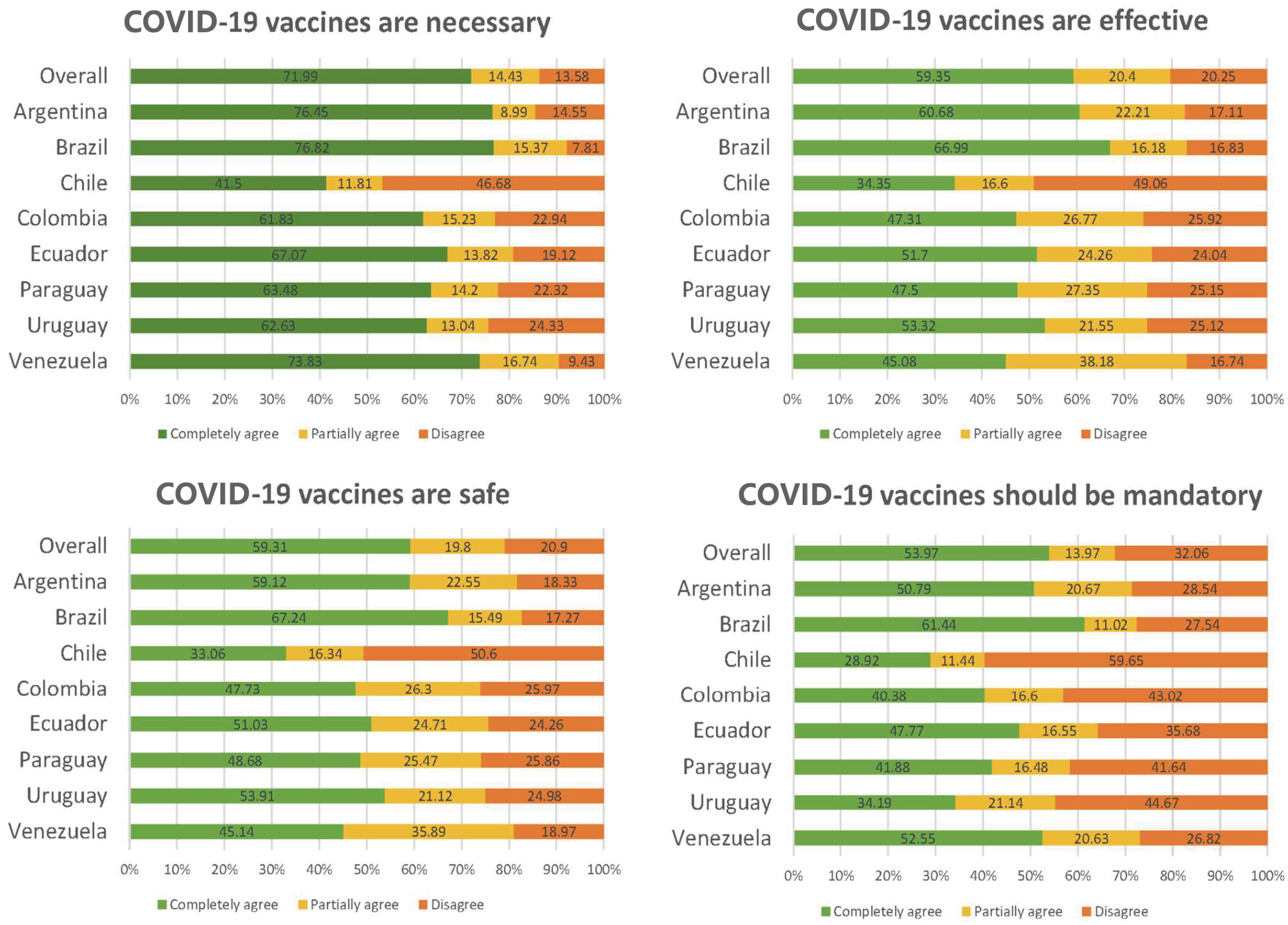
3.4. Opinions and Attitudes towards COVID-19 Vaccination
3.5. COVID-19 Vaccination
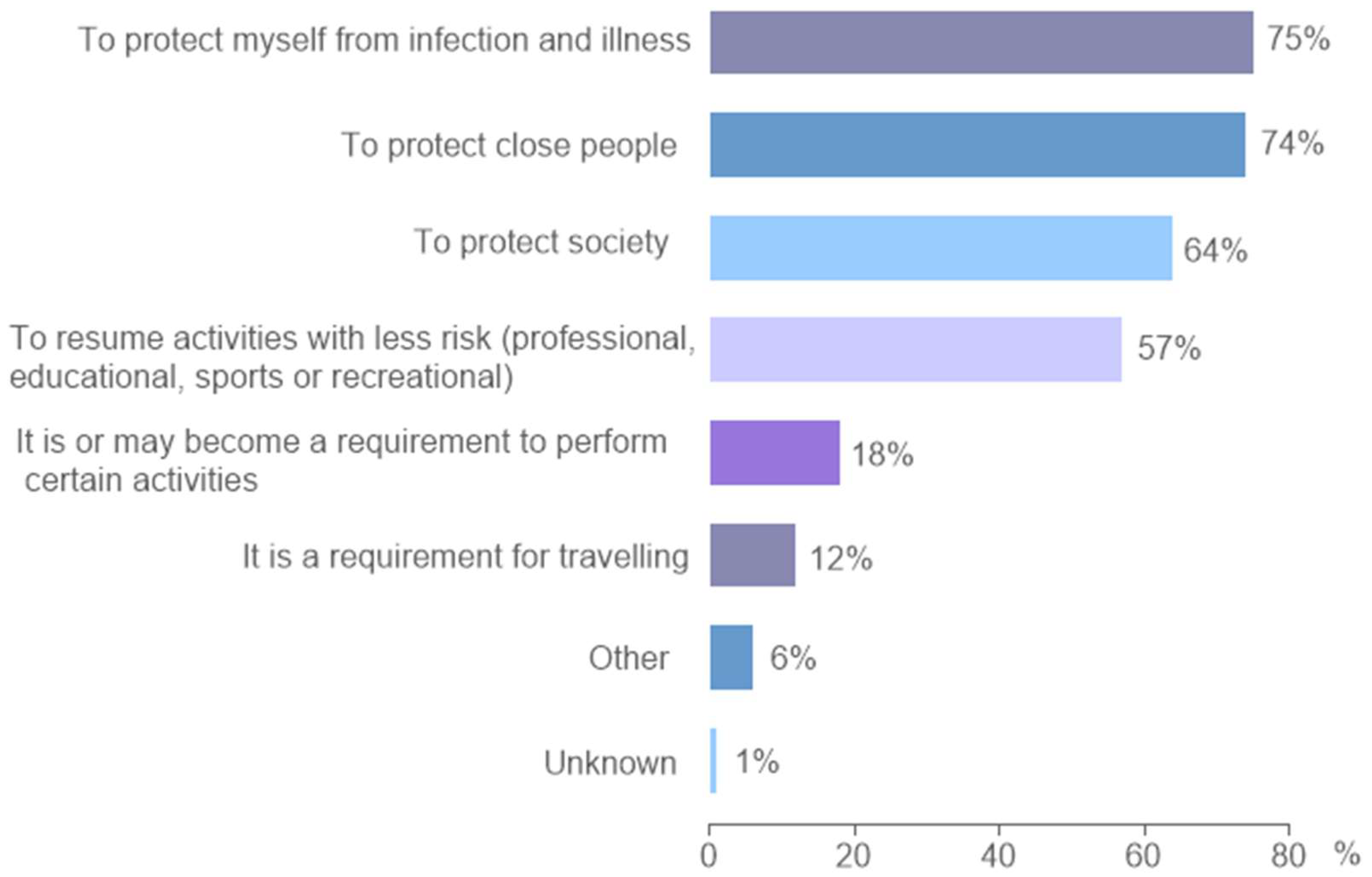
3.6. Reasons and Motivations for Vaccination
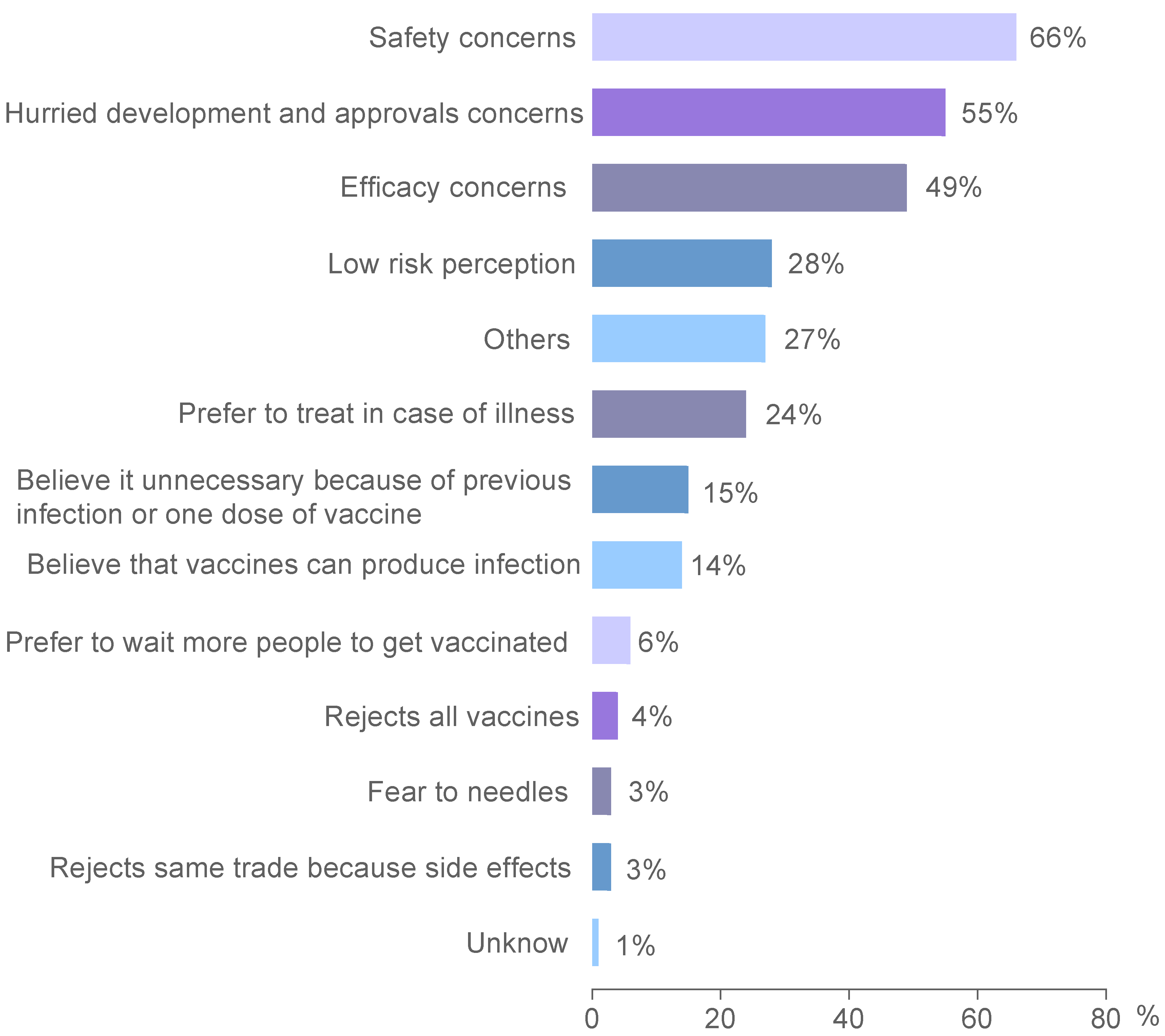
3.7. Reasons and Motivations for Not Getting Vaccinated
3.8. Vaccine Acceptance/Rejection according to Vaccine Type
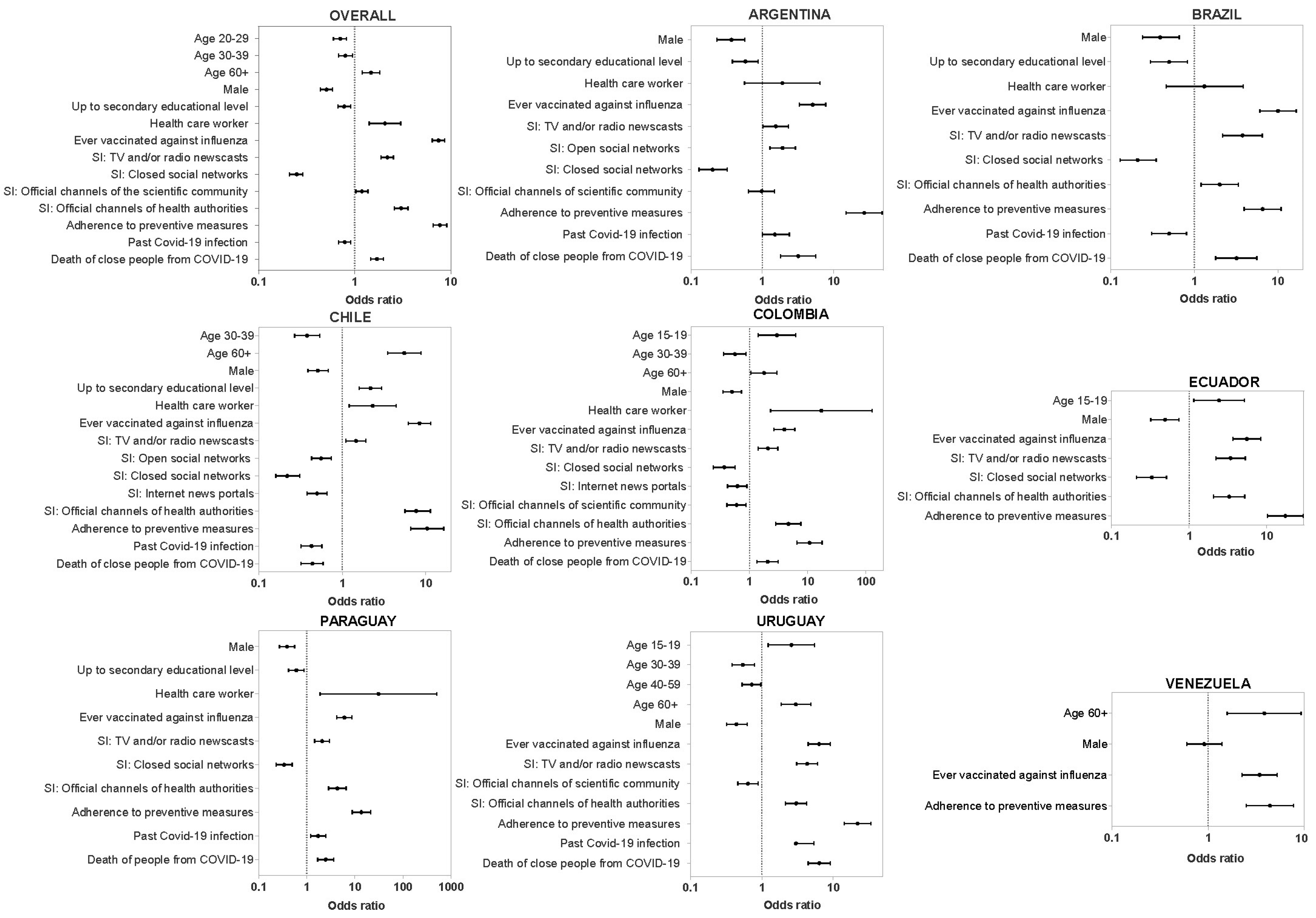
3.9. Factors Related to COVID-19 Vaccination Uptake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Piret, J.; Boivin, G. Pandemics Throughout History. Front. Microbiol. 2021, 11, 631736. [Google Scholar] [CrossRef] [PubMed]
- Clemens, S.A.C.; Clemens, R. The Need and Challenges for Development of Vaccines against Emerging Infectious Diseases. J. Pediatr. 2022, 99, S37–S45. [Google Scholar] [CrossRef] [PubMed]
- Riedel, S. Edward Jenner and the History of Smallpox and Vaccination. Baylor Univ. Med. Cent. Proc. 2005, 18, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Ehreth, J. The Global Value of Vaccination. Vaccine 2003, 21, 596–600. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.M.C.; Plotkin, S.A. Impact of Vaccines; Health, Economic and Social Perspectives. Front. Microbiol. 2020, 11, 1526. [Google Scholar] [CrossRef] [PubMed]
- WHO/Samuel Aranda WHO Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 23 February 2023).
- Nguyen, A.; Catalan-Matamoros, D. Digital Mis/Disinformation and Public Engagment with Health and Science Controversies: Fresh Perspectives from COVID-19. Media Commun. 2020, 8, 323–328. [Google Scholar] [CrossRef]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.A.; Failla, G.; Puleo, V.; Melnyk, A.; Lontano, A.; Ricciardi, W. Social Media and Attitudes towards a COVID-19 Vaccination: A Systematic Review of the Literature. EClinicalMedicine 2022, 48, 101454. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Ratzan, S.C.; Kamarulzaman, A.; El-Mohandes, A. A Survey of COVID-19 Vaccine Acceptance across 23 Countries in 2022. Nat. Med. 2023, 29, 366–375. [Google Scholar] [CrossRef]
- Dubé, E.; MacDonald, N.E. How Can a Global Pandemic Affect Vaccine Hesitancy? Expert Rev. Vaccines 2020, 19, 899–901. [Google Scholar] [CrossRef]
- COVAX Calls for Urgent Action to Close Vaccine Equity Gap. Available online: https://www.who.int/news/item/20-05-2022-covax-calls-for-urgent-action-to-close-vaccine-equity-gap (accessed on 29 June 2023).
- Lawal, L.; Aminu Bello, M.; Murwira, T.; Avoka, C.; Yusuf Ma’aruf, S.; Harrison Omonhinmin, I.; Maluleke, P.; Tsagkaris, C.; Onyeaka, H. Low Coverage of COVID-19 Vaccines in Africa: Current Evidence and the Way Forward. Hum. Vaccines Immunother. 2022, 18, 2034457. [Google Scholar] [CrossRef]
- Guzman-Holst, A.; DeAntonio, R.; Prado-Cohrs, D.; Juliao, P. Barriers to Vaccination in Latin America: A Systematic Literature Review. Vaccine 2020, 38, 470–481. [Google Scholar] [CrossRef]
- Bates, B.R.; Villegas-Botero, A.; Costales, J.A.; Moncayo, A.L.; Tami, A.; Carvajal, A.; Grijalva, M.J. COVID-19 Vaccine Hesitancy in Three Latin American Countries: Reasons Given for Not Becoming Vaccinated in Colombia, Ecuador, and Venezuela. Health Commun. 2022, 37, 1465–1475. [Google Scholar] [CrossRef]
- Tironi, P.A.; Barham, E.; Daly, S.Z.; Gerez, J.E.; Marshall, J.; Pocasangre, O. Messages That Increase COVID-19 Vaccine Acceptance: Evidence from Online Experiments in Six Latin American Countries. PLoS ONE 2021, 16, e0259059. [Google Scholar] [CrossRef]
- The Lancet. COVID-19 in Latin America: A Humanitarian Crisis. Lancet 2020, 396, 1463. [Google Scholar] [CrossRef]
- Otto, S.P.; Day, T.; Arino, J.; Colijn, C.; Dushoff, J.; Li, M.; Mechai, S.; Van Domselaar, G.; Wu, J.; Earn, D.J.D.; et al. The Origins and Potential Future of SARS-CoV-2 Variants of Concern in the Evolving COVID-19 Pandemic. Curr. Biol. 2021, 31, R918–R929. [Google Scholar] [CrossRef]
- World Population Prospects-Population Division-United Nations. Available online: https://population.un.org/wpp/Download/Standard/Population/ (accessed on 5 July 2023).
- Our World in Data. Share of People Vaccinated. 21 February 2022. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 8 October 2023).
- Urueña, A.; Ruiz, J.I.; Lew, D.A.; David, J.; Fidanza, E.; Bianculli, P.; Rearte, A.; Vizzotti, C. Opinions, Attitudes, and Barriers to Pediatric Vaccination in Argentina. Vaccine 2022, 40, 7042–7049. [Google Scholar] [CrossRef]
- Goodman, R.A.; Rothstein, M.A.; Hoffman, R.E.; Lopez, W.; Matthews, G.W. Vaccination Mandates: The Public Health Imperative and Individual Rights. In Law in Public Health Practice; Oxford University Press: Oxford, UK, 2003; pp. 262–284. [Google Scholar]
- Smith, M.J.; Emanuel, E.J. Learning from Five Bad Arguments against Mandatory Vaccination. Vaccine 2023, 41, 3301–3304. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 and Mandatory Vaccination: Ethical Considerations: Policy Brief, 30 May 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. COVID-19 Vaccines: Safety Surveillance Manual; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Vacunas Contra El SARS-CoV-2. Available online: https://www.argentina.gob.ar/anmat/covid-19-acciones/vacunas (accessed on 8 October 2023).
- Vacunas Contra El COVID-Ley 27.573. Available online: https://www.argentina.gob.ar/justicia/derechofacil/leysimple/covid-19-vacunas-contra-covid (accessed on 8 October 2023).
- Sojo, A. La Aprobación de CoronaVac En Brasil y Chile: Algunas Lecciones Sobre Los Retos Regulatorios de Vacunas. Rev. Panam. Salud Pública 2022, 46, 1–7. [Google Scholar] [CrossRef]
- Vacunas COVID En Chile. Available online: https://www.ispch.gob.cl/isp-covid-19/vacunas-covid-19/ (accessed on 8 October 2023).
- Lista Vacunas COVID-19 Colombia. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/COM/lista-vacunas-covid-19.pdf (accessed on 8 October 2023).
- Colombia Recibe Las Primeras Vacunas Que Llegan a Las Américas a Través Del Mecanismo COVAX. Available online: https://www.paho.org/es/noticias/1-3-2021-colombia-recibe-primeras-vacunas-que-llegan-americas-traves-mecanismo-covax (accessed on 8 October 2023).
- Arcsa Autoriza El Ingreso de La Vacuna CanSino a Ecuador. Available online: https://www.controlsanitario.gob.ec/arcsa-autoriza-el-ingreso-de-la-vacuna-cansino-a-ecuador/ (accessed on 8 October 2023).
- Vacunación Contra La COVID-19 En Ecuador. Available online: https://www.covid19ecuador.org/vacunas (accessed on 8 October 2023).
- Paraguay Recibe Las Primeras Vacunas COVID-19 a Través Del Mecanismo COVAX. Available online: https://www.paho.org/es/noticias/19-3-2021-paraguay-recibe-primeras-vacunas-covid-19-traves-mecanismo-covax (accessed on 8 October 2023).
- Montiel, D. Vacunas COVID-19, ¿Cuál de Ellas Llegará Al Paraguay? Rev. Científica Cienc. La Salud 2020, 2, 1–3. [Google Scholar] [CrossRef]
- Registro de Vacunas COVID-19 Administradas En Nuestro País. Available online: https://www.gub.uy/ministerio-salud-publica/comunicacion/noticias/registro-vacunas-covid-19-administradas-nuestro-pais (accessed on 8 October 2023).
- Venezuela Recibe Cuarto Lote de 3,1 Millones de Vacunas Contra La COVID-19. Available online: https://www.paho.org/es/noticias/4-1-2022-venezuela-recibe-cuarto-lote-31-millones-vacunas-contra-covid-19 (accessed on 8 October 2023).
- Cárdenas Quintero, R.; Madriz, C. Pandemia COVID-19 y Vacuna Sputnik V Al Personal de Salud Del Hospital Central de San Cristóbal, Venezuela. Rev. Venez. Cirugía Ortopédica y Traumatol. 2022, 54, 2–12. [Google Scholar] [CrossRef]
- Argote, P.; Barham, E.; Daly, S.Z.; Gerez, J.E.; Marshall, J.; Pocasangre, O. The Shot, the Message, and the Messenger: COVID-19 Vaccine Acceptance in Latin America. NPJ Vaccines 2021, 6, 118. [Google Scholar] [CrossRef] [PubMed]
- Hornsey, M.J.; Harris, E.A.; Fielding, K.S. The Psychological Roots of Anti-Vaccination Attitudes: A 24-Nation Investigation. Heal. Psychol. 2018, 37, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Alarcón-Braga, E.A.; Hernandez-Bustamante, E.A.; Salazar-Valdivia, F.E.; Valdez-Cornejo, V.A.; Mosquera-Rojas, M.D.; Ulloque-Badaracco, J.R.; Rondon-Saldaña, J.C.; Zafra-Tanaka, J.H. Acceptance towards COVID-19 Vaccination in Latin America and the Caribbean: A Systematic Review and Meta-Analysis. Travel Med. Infect. Dis. 2022, 49, 102369. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping Global Trends in Vaccine Confidence and Investigating Barriers to Vaccine Uptake: A Large-Scale Retrospective Temporal Modelling Study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef] [PubMed]
- Fundación Bunge y Born Índice de Confianza y Acceso a Las Vacunas. Resultados. 2022-Año 4. Available online: https://www.fundacionbyb.org/_files/ugd/2aae47_495e5460aa504c70b7400dc3028de3d5.pdf (accessed on 8 October 2023).
- Kirbiš, A. The Impact of Socioeconomic Status, Perceived Threat and Healthism on Vaccine Hesitancy. Sustainability 2023, 15, 6107. [Google Scholar] [CrossRef]
- Mendonça, J.; Hilário, A.P. Healthism Vis-à-Vis Vaccine Hesitancy: Insights from Parents Who Either Delay or Refuse Children’s Vaccination in Portugal. Societies 2023, 13, 184. [Google Scholar] [CrossRef]
- Zintel, S.; Flock, C.; Arbogast, A.L.; Forster, A.; von Wagner, C.; Sieverding, M. Gender Differences in the Intention to Get Vaccinated against COVID-19: A Systematic Review and Meta-Analysis. Z. Fur Gesundheitswissenschaften 2023, 31, 1. [Google Scholar] [CrossRef]
- Ortiz, A.C.; Akgün, K.M.; Bazan, I.S. Embracing the Diversity of Latinx Communities to Promote Vaccinations. YALE J. Biol. Med. 2022, 95, 257–263. [Google Scholar]
- Larson, H.J.; Schulz, W.S.; Tucker, J.D.; Smith, D.M.D. Measuring Vaccine Confidence: Introducing a Global Vaccine Confidence Index. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Teo, C.H.; Ng, C.J.; White, A. Factors Influencing Young Men’s Decision to Undergo Health Screening in Malaysia: A Qualitative Study. BMJ Open 2017, 7, e014364. [Google Scholar] [CrossRef]
- Ortiz-Sánchez, E.; Velando-Soriano, A.; Pradas-Hernández, L.; Vargas-Román, K.; Gómez-Urquiza, J.L.; Cañadas-de la Fuente, G.A.; Albendín-García, L. Analysis of the Anti-Vaccine Movement in Social Networks: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5394. [Google Scholar] [CrossRef] [PubMed]
- Broniatowski, D.A.; Jamison, A.M.; Qi, S.H.; AlKulaib, L.; Chen, T.; Benton, A.; Quinn, S.C.; Dredze, M. Weaponized Health Communication: Twitter Bots and Russian Trolls Amplify the Vaccine Debate. Am. J. Public Health 2018, 108, 1378–1384. [Google Scholar] [CrossRef]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the Impact of COVID-19 Vaccine Misinformation on Vaccination Intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Romero, D.; Kopka, C.J.; Karim, S.A.; Abu-Raddad, L.J.; Almeida, G.; Baptista-Leite, R.; Barocas, J.A.; Barreto, M.L.; Bar-Yam, Y.; et al. A Multinational Delphi Consensus to End the COVID-19 Public Health Threat. Nature 2022, 611, 332. [Google Scholar] [CrossRef] [PubMed]
- Nikoloski, Z.; Bain, R.; Elzalabany, M.K.; Hanna, P.; Aynsley, T.R.; Samhouri, D.; Menchini, L.; Kapil, N.; Gillespie, A. Modelling COVID-19 Vaccination Status and Adherence to Public Health and Social Measures, Eastern Mediterranean Region and Algeria. Bull. World Health Organ. 2023, 101, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Liu, M.; Liu, J. The Association between Influenza Vaccination and COVID-19 and Its Outcomes: A Systematic Review and Meta-Analysis of Observational Studies. Vaccines 2021, 9, 529. [Google Scholar] [CrossRef]

| Variable | Overall | Argentina | Brazil | Chile | Colombia | Ecuador | Paraguay | Uruguay | Venezuela |
|---|---|---|---|---|---|---|---|---|---|
| N (total) | 6655 | 900 | 900 | 853 | 699 | 761 | 851 | 893 | 668 |
| N (weighted) | 749 | 3694 | 338 | 868 | 281 | 111 | 61 | 453 | |
| Female gender (%) | 52.1 | 50.0 | 50.7 | 51.9 | 58.0 | 49.6 | 54.5 | 48.1 | 56.6 |
| Age group (%) | |||||||||
| 15–19 | 10.1 | 10.4 | 9.6 | 8.1 | 10.7 | 12.2 | 13.0 | 8.9 | 12.1 |
| 20–29 | 20.7 | 20.5 | 20.2 | 19.4 | 22.3 | 23.7 | 26.1 | 18.5 | 20.0 |
| 30–39 | 20.0 | 18.9 | 20.5 | 19.1 | 19.7 | 20.2 | 21.9 | 16.7 | 19.5 |
| 40–59 | 31.2 | 29.7 | 32.0 | 31.9 | 30.3 | 28.7 | 25.2 | 30.6 | 31.8 |
| 60+ | 18.0 | 20.6 | 17.7 | 21.5 | 16.9 | 15.2 | 13.9 | 25.4 | 16.7 |
| Educational level (%) | |||||||||
| Primary | 4.0 | 2.2 | 4.8 | 1.1 | 3.7 | 4.1 | 4.6 | 4.5 | 3.3 |
| Secondary | 30.6 | 33.7 | 28.2 | 30.4 | 35.9 | 33.2 | 28.4 | 48.6 | 30.8 |
| Higher education | 65.4 | 64.0 | 67.0 | 68.5 | 60.4 | 62.7 | 67.0 | 47.0 | 66.0 |
| Employment status (%) | |||||||||
| Student | 17.1 | 20.1 | 16.2 | 17.8 | 15.2 | 22.6 | 23.2 | 17.4 | 17.7 |
| Housewife/retired | 20.2 | 19.1 | 19.1 | 23.7 | 24.4 | 18.8 | 18.5 | 25.4 | 21.6 |
| Unemployed | 10.7 | 6.2 | 9.0 | 9.1 | 19.0 | 16.8 | 10.8 | 6.7 | 14.6 |
| Health care worker | 5.9 | 5.6 | 5.7 | 5.0 | 7.5 | 5.4 | 5.9 | 5.5 | 6.7 |
| Employed | 46.0 | 49.0 | 50.1 | 44.3 | 33.9 | 36.4 | 41.6 | 44.9 | 39.4 |
| COVID-19 sources of information (%) | |||||||||
| TV and/or radio newscasts | 51.7 | 52.7 | 51.4 | 52.7 | 52.6 | 52.9 | 51.5 | 56.5 | 49.1 |
| Open social networks (Facebook, Instagram, Twitter, etc.) | 52.8 | 62.8 | 48.2 | 54.8 | 52.9 | 60.3 | 57.8 | 52.3 | 66.7 |
| Closed social networks (WhatsApp, Telegram) | 16.1 | 14.7 | 13.7 | 28.5 | 17.7 | 16.8 | 18.1 | 17.8 | 25.3 |
| Internet news portals | 47.8 | 42.4 | 51.8 | 49.7 | 39.7 | 38.8 | 32.2 | 48.3 | 47.4 |
| Official channels of public health authorities | 43.3 | 50.2 | 43.8 | 36.9 | 40.1 | 44.5 | 45.7 | 48.3 | 37.2 |
| Official channels of the scientific community | 40.6 | 36.3 | 45.4 | 35.8 | 35.6 | 37.5 | 27.3 | 30.5 | 29.2 |
| Close people death from COVID-19 (%) | 43.5 | 31.5 | 48.1 | 30.5 | 38.9 | 43.0 | 41.8 | 15.8 | 48.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urueña, A.; Machado, R.; Cunha, J.; López Colmano, C.; Rancaño, C.; Kfouri, R.; Pírez, C.; Bonvehí, P.; Calvo, M.; Cuadros, R.; et al. Opinions, Attitudes and Factors Related to SARS-CoV-2 Vaccine Uptake in Eight South American Countries. Vaccines 2023, 11, 1660. https://doi.org/10.3390/vaccines11111660
Urueña A, Machado R, Cunha J, López Colmano C, Rancaño C, Kfouri R, Pírez C, Bonvehí P, Calvo M, Cuadros R, et al. Opinions, Attitudes and Factors Related to SARS-CoV-2 Vaccine Uptake in Eight South American Countries. Vaccines. 2023; 11(11):1660. https://doi.org/10.3390/vaccines11111660
Chicago/Turabian StyleUrueña, Analía, Ricardo Machado, Juarez Cunha, Clara López Colmano, Carolina Rancaño, Renato Kfouri, Catalina Pírez, Pablo Bonvehí, Mario Calvo, Robinson Cuadros, and et al. 2023. "Opinions, Attitudes and Factors Related to SARS-CoV-2 Vaccine Uptake in Eight South American Countries" Vaccines 11, no. 11: 1660. https://doi.org/10.3390/vaccines11111660
APA StyleUrueña, A., Machado, R., Cunha, J., López Colmano, C., Rancaño, C., Kfouri, R., Pírez, C., Bonvehí, P., Calvo, M., Cuadros, R., Muñoz, G., Rodríguez, M., Torres, J., Cahn, F., & Ballalai, I. (2023). Opinions, Attitudes and Factors Related to SARS-CoV-2 Vaccine Uptake in Eight South American Countries. Vaccines, 11(11), 1660. https://doi.org/10.3390/vaccines11111660








