Increasing Influenza Vaccination Uptake by Sending Reminders: A Representative Cross-Sectional Study on the Preferences of Italian Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Procedures
2.2. Study Outcomes
2.3. Study Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Participants
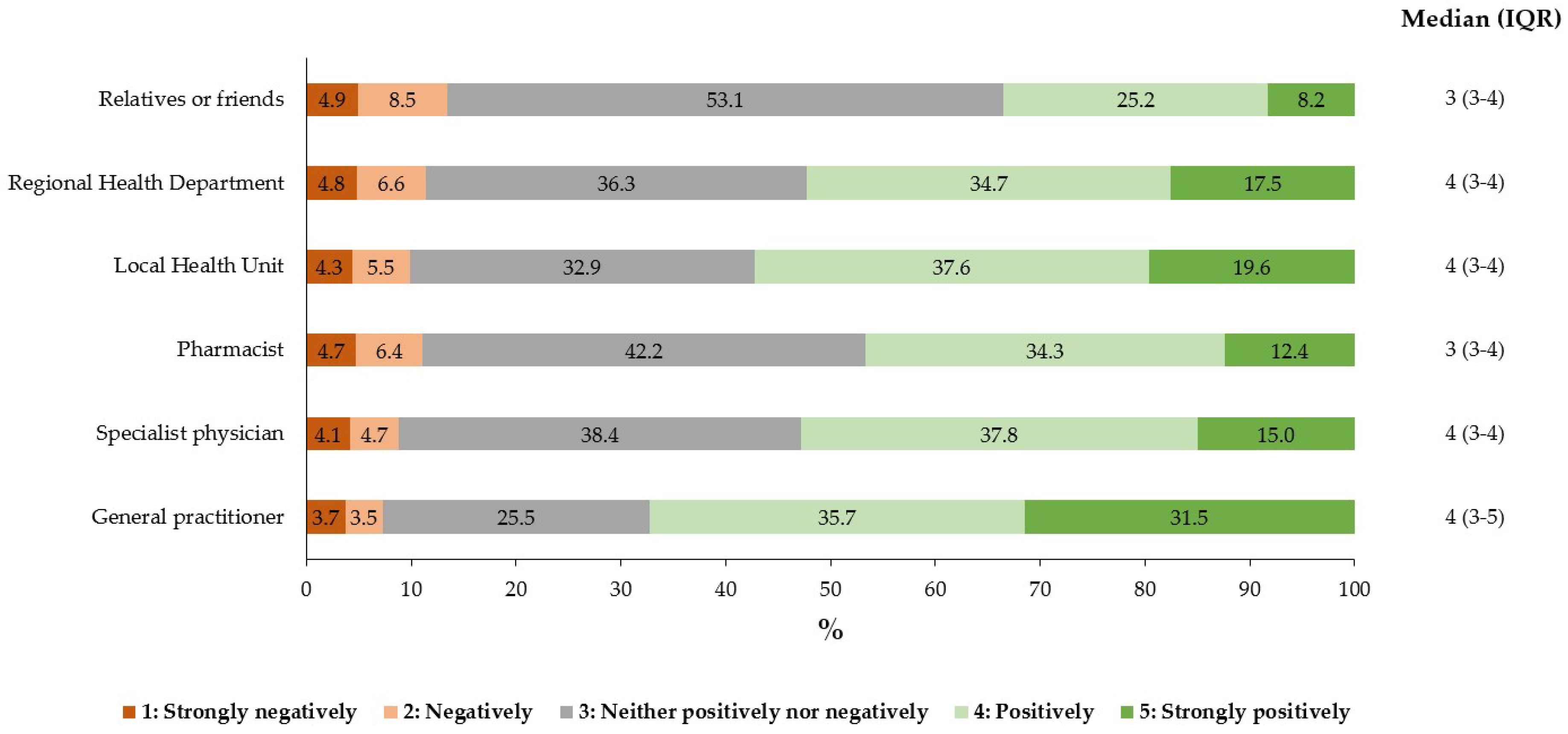
3.2. Association between Influenza Vaccination Uptake and Influenza Vaccination Reminder
3.3. Preferences on the Reminder Delivery Channel
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Vaccines against influenza: WHO position paper—May 2022. Wkly. Epidemiol. Rec. 2022, 97, 185–208. [Google Scholar]
- Palache, A.; Rockman, S.; Taylor, B.; Akcay, M.; Billington, J.K.; Barbosa, P.; IFPMA Influenza Vaccine Supply (IFPMA IVS) task force. Vaccine complacency and dose distribution inequities limit the benefits of seasonal influenza vaccination, despite a positive trend in use. Vaccine 2021, 39, 6081–6087. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; Lorenzetti, D.L. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst. Rev. 2018, 5, CD005188. [Google Scholar] [CrossRef]
- Bachtiger, P.; Adamson, A.; Chow, J.J.; Sisodia, R.; Quint, J.K.; Peters, N.S. The impact of the COVID-19 pandemic on the uptake of influenza vaccine: UK-wide observational study. JMIR Public Health Surveill. 2021, 7, e26734. [Google Scholar] [CrossRef]
- Domnich, A.; Cambiaggi, M.; Vasco, A.; Maraniello, L.; Ansaldi, F.; Baldo, V.; Bonanni, P.; Calabrò, G.E.; Costantino, C.; de Waure, C.; et al. Attitudes and beliefs on influenza vaccination during the COVID-19 pandemic: Results from a representative Italian survey. Vaccines 2020, 8, 711. [Google Scholar] [CrossRef]
- Leuchter, R.K.; Jackson, N.J.; Mafi, J.N.; Sarkisian, C.A. Association between COVID-19 vaccination and influenza vaccination rates. N. Engl. J. Med. 2022, 386, 2531–2532. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Influenza Vaccination Coverage. Available online: https://www.salute.gov.it/portale/influenza/dettaglioContenutiInfluenza.jsp?lingua=italiano&id=679&area=influenza&menu=vuoto#:~:text=Dalla%20stagione%202015%2F16%20l,)%20nella%20stagione%202022%2F2023 (accessed on 10 October 2023).
- European Centre for Disease Prevention and Control (ECDC). Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States—Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons; ECDC: Stockholm, Sweden, 2018; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/seasonal-influenza-antiviral-use-2018.pdf (accessed on 15 September 2023).
- Kassianos, G.; Blank, P.; Falup-Pecurariu, O.; Kuchar, E.; Kyncl, J.; De Lejarazu, R.O.; Nitsch-Osuch, A.; van Essen, G.A. Influenza vaccination: Key facts for general practitioners in Europe-a synthesis by European experts based on national guidelines and best practices in the United Kingdom and the Netherlands. Drugs Context 2016, 5, 212293. [Google Scholar] [CrossRef]
- Van Ourti, T.; Bouckaert, N. The Dutch influenza vaccination policy and medication use, outpatient visits, hospitalization and mortality at age 65. Eur. J. Public Health 2020, 30, 275–280. [Google Scholar] [CrossRef]
- Dexter, L.J.; Teare, M.D.; Dexter, M.; Siriwardena, A.N.; Read, R.C. Strategies to increase influenza vaccination rates: Outcomes of a nationwide cross-sectional survey of UK general practice. BMJ Open 2012, 2, e000851. [Google Scholar] [CrossRef]
- Anderson, L.J.; Shekelle, P.; Keeler, E.; Uscher-Pines, L.; Shanman, R.; Morton, S.; Aliyev, G.; Nuckols, T.K. The cost of interventions to increase influenza vaccination: A systematic review. Am. J. Prev. Med. 2018, 54, 299–315. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Prevention and Control of Influenza: Recommendations for the 2022–2023 Season. Available online: https://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2022&codLeg=87997&parte=1%20&serie=null (accessed on 15 September 2023).
- Barbieri, M.; Capri, S.; Waure, C.; Boccalini, S.; Panatto, D. Age- and risk-related appropriateness of the use of available influenza vaccines in the Italian elderly population is advantageous: Results from a budget impact analysis. J. Prev. Med. Hyg. 2017, 58, E279–E287. [Google Scholar] [PubMed]
- Fallani, E.; Orsi, A.; Signori, A.; Icardi, G.; Domnich, A. An exploratory study to assess patterns of influenza- and pneumonia-related mortality among the Italian elderly. Hum. Vaccin. Immunother. 2021, 17, 5514–5521. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, C.; Rezza, G.; Ricciardi, W. Strategies in recommending influenza vaccination in Europe and US. Hum. Vaccin. Immunother. 2018, 14, 693–698. [Google Scholar] [CrossRef]
- Tam, G.; Huang, Z.; Chan, E.Y.Y. Household preparedness and preferred communication channels in public health emergencies: A cross-sectional survey of residents in an Asian developed urban city. Int. J. Environ. Res. Public Health 2018, 15, 1598. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.P.; Taaffe, C.; Ahern, E.; McMahon, G.; Muldoon, O. A meta-analysis of influenza vaccination following correspondence: Considerations for COVID-19. Vaccine 2021, 39, 7606–7624. [Google Scholar] [CrossRef]
- Ilozumba, O.; Schmidt, P.; Ket, J.C.F.; Jaspers, M. Can mHealth interventions contribute to increased HPV vaccination uptake? A systematic review. Prev. Med. Rep. 2020, 21, 101289. [Google Scholar] [CrossRef]
- Domnich, A.; Grassi, R.; Fallani, E.; Spurio, A.; Bruzzone, B.; Panatto, D.; Marozzi, B.; Cambiaggi, M.; Vasco, A.; Orsi, A.; et al. Changes in attitudes and beliefs concerning vaccination and influenza vaccines between the first and second COVID-19 pandemic waves: A longitudinal study. Vaccines 2021, 9, 1016. [Google Scholar] [CrossRef]
- Domnich, A.; Grassi, R.; Fallani, E.; Ciccone, R.; Bruzzone, B.; Panatto, D.; Ferrari, A.; Salvatore, M.; Cambiaggi, M.; Vasco, A.; et al. Acceptance of COVID-19 and influenza vaccine co-administration: Insights from a representative Italian survey. J. Pers. Med. 2022, 12, 139. [Google Scholar] [CrossRef]
- Kohlhammer, Y.; Schnoor, M.; Schwartz, M.; Raspe, H.; Schäfer, T. Determinants of influenza and pneumococcal vaccination in elderly people: A systematic review. Public Health 2007, 121, 742–751. [Google Scholar] [CrossRef]
- Vezzosi, L.; Riccò, M.; Agozzino, E.; Odone, A.; Signorelli, C. Knowledge, attitudes, and practices of general practitioners from the Province of Parma (Northern Italy) towards vaccinations in adults ≥65 year-old. Acta Biomed. 2019, 90, 71–75. [Google Scholar]
- Levi, M.; Bonanni, P.; Biffino, M.; Conversano, M.; Corongiu, M.; Morato, P.; Maio, T. Influenza vaccination 2014–2015: Results of a survey conducted among general practitioners in Italy. Hum. Vaccin. Immunother. 2018, 14, 1342–1350. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.A.; Ostrowsky, J.T.; Kraigsley, A.M.; Mehr, A.J.; Bresee, J.S.; Friede, M.H.; Gellin, B.G.; Golding, J.P.; Hart, P.J.; Moen, A.; et al. A research and development (R&D) roadmap for influenza vaccines: Looking toward the future. Vaccine 2021, 39, 6573–6584. [Google Scholar] [PubMed]
- Agostino, D.; Arnaboldi, M.; Lema, M.D. New development: COVID-19 as an accelerator of digital transformation in public service delivery. Public Money Manag. 2021, 41, 69–72. [Google Scholar] [CrossRef]
- Frascella, B.; Oradini-Alacreu, A.; Balzarini, F.; Signorelli, C.; Lopalco, P.L.; Odone, A. Effectiveness of email-based reminders to increase vaccine uptake: A systematic review. Vaccine 2020, 38, 433–443. [Google Scholar] [CrossRef]
- Dumit, E.M.; Novillo-Ortiz, D.; Contreras, M.; Velandia, M.; Danovaro-Holliday, M.C. The use of eHealth with immunizations: An overview of systematic reviews. Vaccine 2018, 36, 7923–7928. [Google Scholar] [CrossRef]
- Regan, A.K.; Bloomfield, L.; Peters, I.; Effler, P.V. Randomized controlled trial of text message reminders for increasing influenza vaccination. Ann. Fam. Med. 2017, 15, 507–514. [Google Scholar] [CrossRef]
- Morris, J.; Wang, W.; Wang, L.; Peddecord, K.M.; Sawyer, M.H. Comparison of reminder methods in selected adolescents with records in an immunization registry. J. Adolesc. Health 2015, 56, S27–S32. [Google Scholar] [CrossRef]
- Mehta, S.J.; Mallozzi, C.; Shaw, P.A.; Reitz, C.; McDonald, C.; Vandertuyn, M.; Balachandran, M.; Kopinsky, M.; Sevinc, C.; Johnson, A.; et al. Effect of text messaging and behavioral interventions on COVID-19 vaccination uptake: A randomized clinical trial. JAMA Netw. Open 2022, 5, e2216649. [Google Scholar] [CrossRef]
- Welzel, F.D.; Stein, J.; Hajek, A.; König, H.H.; Riedel-Heller, S.G. Frequent attenders in late life in primary care: A systematic review of European studies. BMC Fam. Pract. 2017, 18, 104. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Flu Vaccination Coverage, United States, 2022–23 Influenza Season. Available online: https://www.cdc.gov/flu/fluvaxview/coverage-2223estimates.htm#:~:text=Flu%20vaccination%20coverage%20for%202022,22%20season%20(Figure%206) (accessed on 10 October 2023).
- Giacomelli, A.; Galli, M.; Maggi, S.; Noale, M.; Trevisan, C.; Pagani, G.; Antonelli-Incalzi, R.; Molinaro, S.; Bastiani, L.; Cori, L.; et al. Influenza vaccination uptake in the general Italian population during the 2020-2021 flu season: Data from the EPICOVID-19 online web-based survey. Vaccines 2022, 10, 293. [Google Scholar] [CrossRef]
- Nazareth, J.; Pan, D.; Martin, C.A.; Barr, I.; Sullivan, S.G.; Stephenson, I.; Sahota, A.; Clark, T.W.; Nellums, L.B.; Tang, J.W.; et al. Is the UK prepared for seasonal influenza in 2022-23 and beyond? Lancet Infect. Dis. 2022, 22, 1280–1281. [Google Scholar] [CrossRef] [PubMed]
- Pascucci, D.; Nurchis, M.C.; Lontano, A.; Marziali, E.; Vetrugno, G.; Cambieri, A.; Moscato, U.; Di Pilla, A.; Damiani, G.; Laurenti, P. Flu and COVID-19 vaccination: What happens to the flu shot when the campaigns overlap? Experience from a large Italian research hospital. Vaccines 2022, 10, 976. [Google Scholar] [CrossRef] [PubMed]
- King, J.P.; McLean, H.Q.; Belongia, E.A. Validation of self-reported influenza vaccination in the current and prior season. Influenza Other Respir. Viruses 2018, 12, 808–813. [Google Scholar] [CrossRef]
- Mac Donald, R.; Baken, L.; Nelson, A.; Nichol, K.L. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am. J. Prev. Med. 1999, 16, 173–177. [Google Scholar] [CrossRef]
- Khanijahani, A.; Calhoun, B.; Kiel, J. Internet use habits and influenza vaccine uptake among US adults: Results from seven years (2012–2018) of the National Health Interview Survey. Public Health 2021, 195, 76–82. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Level | % (n) | 95% CI |
|---|---|---|---|
| Sex | Female | 52.0 (1307) | 50.0–54.0 |
| Male | 48.0 (1206) | 46.0–50.0 | |
| Age, years | 18–24 | 8.2 (205) | 7.1–9.3 |
| 25–34 | 12.7 (318) | 11.4–14.0 | |
| 35–44 | 15.6 (392) | 14.2–17.1 | |
| 45–54 | 19.3 (485) | 17.8–20.9 | |
| 55–64 | 16.9 (424) | 15.4–18.4 | |
| 65–74 | 19.8 (497) | 18.2–21.4 | |
| ≥75 | 7.6 (192) | 6.6–8.8 | |
| Geographic area | North | 46.2 (1162) | 44.3–48.2 |
| Center | 20.1 (504) | 18.5–21.7 | |
| South | 33.7 (847) | 31.9–35.6 | |
| Education level | Low | 9.9 (249) | 8.8–11.1 |
| Medium | 48.8 (1226) | 46.8–50.8 | |
| High | 41.3 (1038) | 39.4–43.3 | |
| Occupation status | Employed | 56.4 (1417) | 54.4–58.3 |
| Student | 6.8 (172) | 5.9–7.9 | |
| Housekeeper | 7.8 (197) | 6.8–9.0 | |
| Retired | 23.1 (580) | 21.4–24.8 | |
| Unemployed | 4.4 (110) | 3.6–5.3 | |
| Other | 1.5 (37) | 1.0–2.0 | |
| Perceived income | Low | 2.9 (72) | 2.3–3.6 |
| Lower than average | 8.0 (202) | 7.0–9.2 | |
| Average | 33.2 (834) | 31.4–35.1 | |
| Higher than average | 38.5 (967) | 36.6–40.4 | |
| High | 1.7 (43) | 1.2–2.3 | |
| No personal income | 15.7 (395) | 14.3–17.2 | |
| 2021/22 influenza vaccination | No | 53.6 (1348) | 51.7–55.6 |
| Yes | 46.4 (1165) | 44.4–48.3 |
| Received Invitation to Get Vaccinated From | Level | Vaccinated, % (n) | Non-Vaccinated, % (n) | OR (95% CI) | aOR (95% CI) 1 |
|---|---|---|---|---|---|
| General practitioner | No | 36.9 (430) | 81.3 (1096) | Ref | Ref |
| Yes | 63.1 (735) | 18.7 (252) | 7.43 (6.20–8.91) | 4.43 (3.60–5.48) | |
| Specialist physician | No | 73.6 (858) | 92.5 (1247) | Ref | Ref |
| Yes | 26.4 (307) | 7.5 (101) | 4.42 (3.47–5.62) | 2.23 (1.64–3.05) | |
| Pharmacist | No | 82.0 (955) | 94.1 (1269) | Ref | Ref |
| Yes | 18.0 (210) | 5.9 (79) | 3.53 (2.69–4.37) | 1.16 (0.80–1.67) | |
| Local health unit | No | 80.3 (936) | 92.7 (1250) | Ref | Ref |
| Yes | 19.7 (229) | 7.3 (98) | 3.12 (2.43–4.01) | 1.54 (1.09–2.18) | |
| Regional health department | No | 81.2 (946) | 93.0 (1254) | Ref | Ref |
| Yes | 18.8 (219) | 7.0 (94) | 3.09 (2.39–3.99) | 1.11 (0.78–1.59) | |
| Relatives or friends | No | 68.2 (794) | 85.1 (1147) | Ref | Ref |
| Yes | 31.8 (371) | 14.9 (201) | 2.67 (2.20–3.24) | 1.26 (0.98–1.62) |
| Received Invitation to Get Vaccinated From (Reference Category = No) | Model 1 1 aOR (95% CI) 2 | Model 2 3 aOR (95% CI) 2 |
|---|---|---|
| General practitioner | 1.81 (1.44–2.28) | 1.68 (1.32–2.15) |
| Specialist physician | 1.00 (0.79–1.27) | 1.12 (0.87–1.45) |
| Pharmacist | 1.09 (0.86–1.38) | 1.30 (1.02–1.68) |
| Local health unit | 1.51 (1.17–1.95) | 1.42 (1.08–1.88) |
| Regional health department | 1.16 (0.92–1.47) | 0.98 (0.76–1.28) |
| Relatives or friends | 1.10 (0.89–1.36) | 1.03 (0.83–1.27) |
| Communication Channel | Total (N = 2513) | 18–59 Years (N = 1623) | ≥60 Years (N = 890) | |||
|---|---|---|---|---|---|---|
| % (n) | 95% CI | % (n) | 95% CI | % (n) | 95% CI | |
| Phone call | 8.6 (216) | 7.5–9.8 | 8.3 (135) | 7.0–9.8 | 9.1 (81) | 7.3–11.2 |
| Postal letter | 17.0 (427) | 15.5–18.5 | 18.0 (292) | 16.2–19.9 | 15.2 (135) | 12.9–17.7 |
| 27.2 (683) | 25.5–29.0 | 27.7 (449) | 25.5–29.9 | 26.3 (234) | 23.4–29.3 | |
| Text/instant message | 24.6 (618) | 22.9–26.3 | 21.6 (351) | 19.6–23.7 | 30.0 (267) | 27.0–33.1 |
| I do not want to receive any invitation | 22.6 (569) | 21.0–24.3 | 24.4 (396) | 22.3–26.6 | 19.4 (173) | 16.9–22.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domnich, A.; Grassi, R.; Fallani, E.; Costantini, G.; Panatto, D.; Ogliastro, M.; Salvatore, M.; Cambiaggi, M.; Vasco, A.; Orsi, A.; et al. Increasing Influenza Vaccination Uptake by Sending Reminders: A Representative Cross-Sectional Study on the Preferences of Italian Adults. Vaccines 2023, 11, 1601. https://doi.org/10.3390/vaccines11101601
Domnich A, Grassi R, Fallani E, Costantini G, Panatto D, Ogliastro M, Salvatore M, Cambiaggi M, Vasco A, Orsi A, et al. Increasing Influenza Vaccination Uptake by Sending Reminders: A Representative Cross-Sectional Study on the Preferences of Italian Adults. Vaccines. 2023; 11(10):1601. https://doi.org/10.3390/vaccines11101601
Chicago/Turabian StyleDomnich, Alexander, Riccardo Grassi, Elettra Fallani, Giulia Costantini, Donatella Panatto, Matilde Ogliastro, Marco Salvatore, Maura Cambiaggi, Alessandro Vasco, Andrea Orsi, and et al. 2023. "Increasing Influenza Vaccination Uptake by Sending Reminders: A Representative Cross-Sectional Study on the Preferences of Italian Adults" Vaccines 11, no. 10: 1601. https://doi.org/10.3390/vaccines11101601
APA StyleDomnich, A., Grassi, R., Fallani, E., Costantini, G., Panatto, D., Ogliastro, M., Salvatore, M., Cambiaggi, M., Vasco, A., Orsi, A., & Icardi, G. (2023). Increasing Influenza Vaccination Uptake by Sending Reminders: A Representative Cross-Sectional Study on the Preferences of Italian Adults. Vaccines, 11(10), 1601. https://doi.org/10.3390/vaccines11101601






