Differences in BNT126b2 and ChAdOx1 Homologous Vaccination Antibody Response among Teachers in Poznan, Poland
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants and Design
2.2. Laboratory Analysis
2.3. Statistical Analysis
2.4. Ethics Approval
3. Results
3.1. Characteristics of the Study Participants
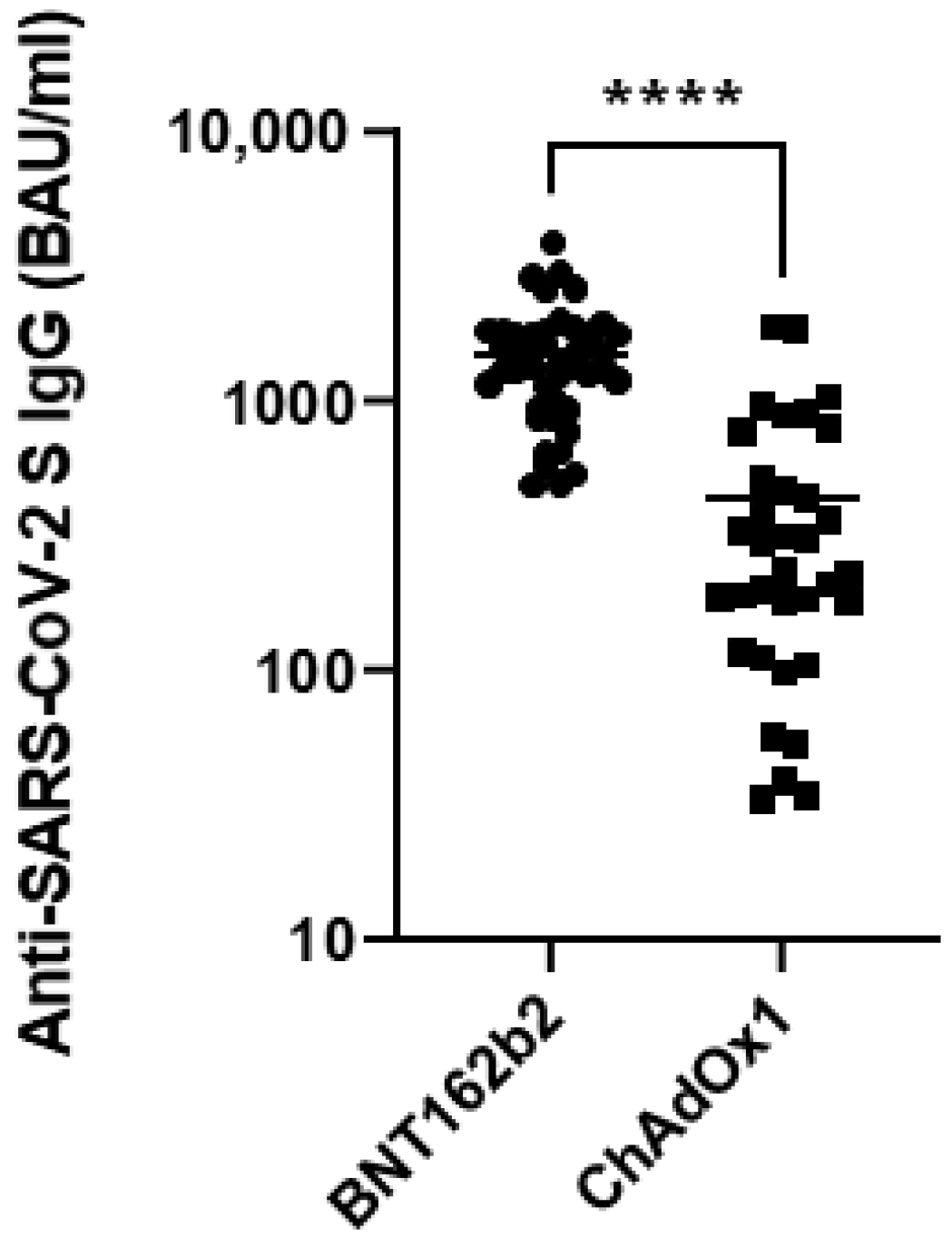
3.2. Anti-SARS-CoV-2 IgG S Antibody Levels at Two Weeks after the Second Dose of the COVID-19 Vaccine
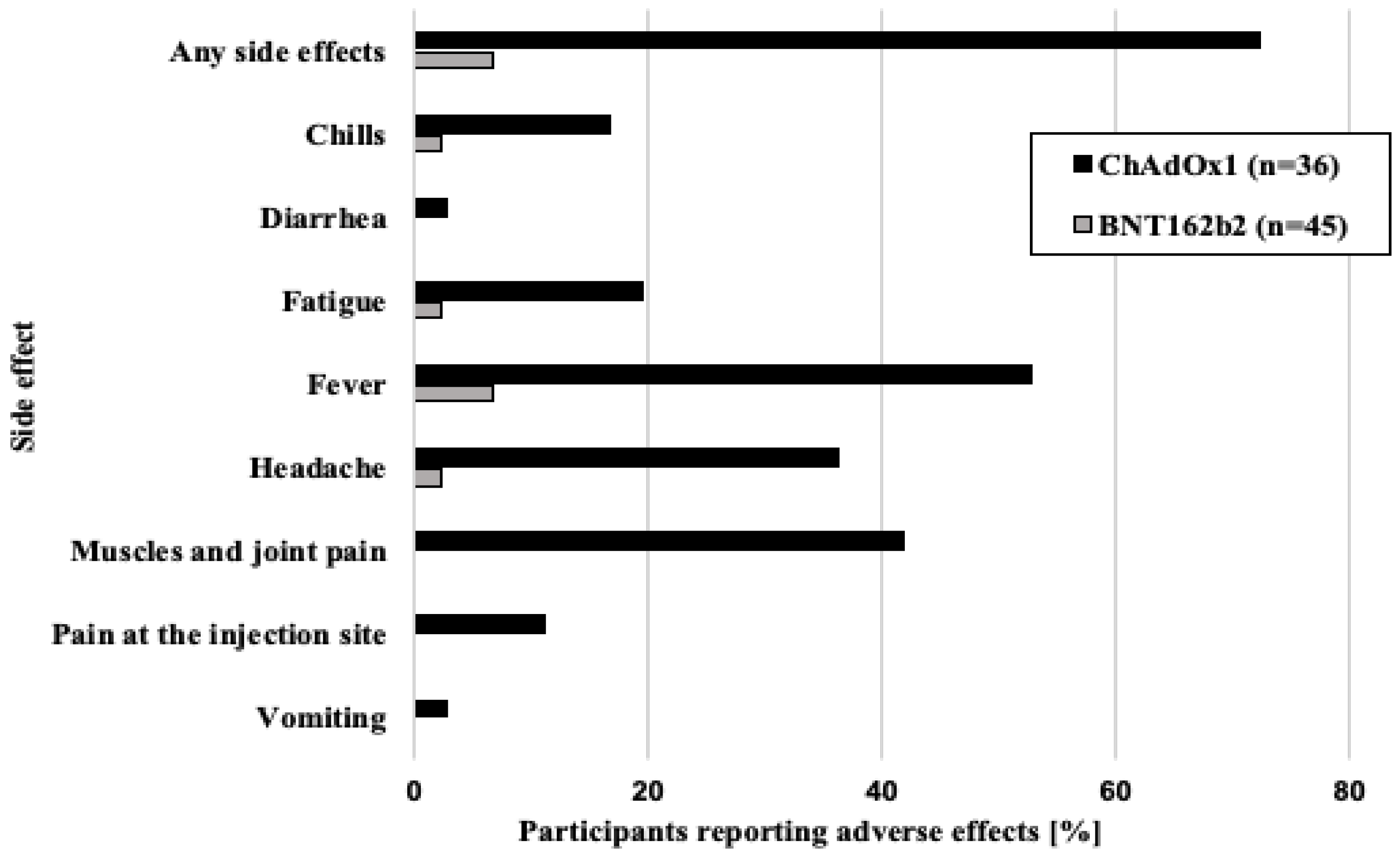
3.3. Side Effects after Two Doses of Either BNT162b2 or ChAdOx1
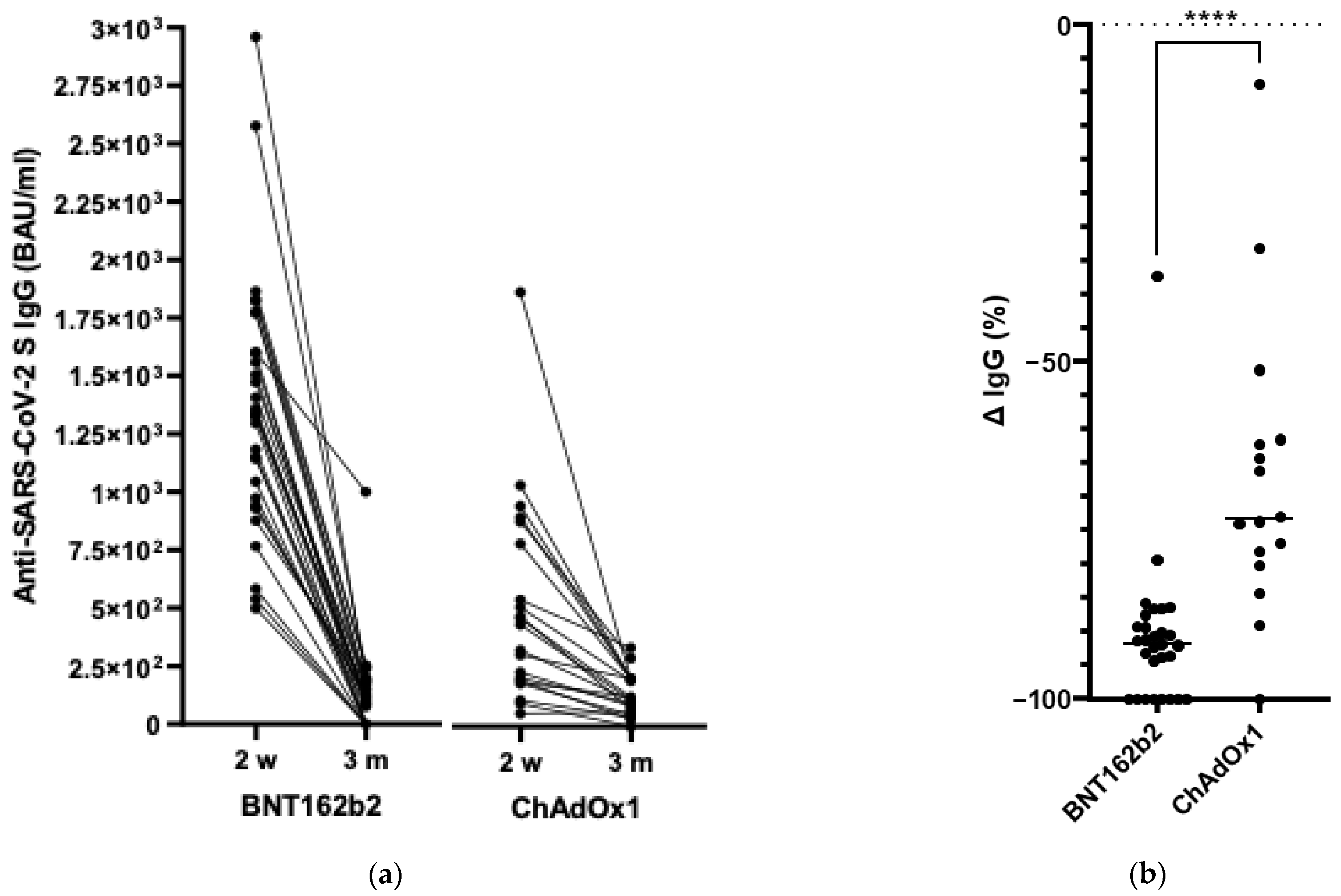
3.4. Anti-SARS-CoV-2 IgG S Antibody Levels Three Months after Vaccination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 14 November 2022).
- Barouch, D.H. Covid-19 vaccines—immunity, variants, boosters. N. Engl. J. Med. 2022, 387, 1011–1020. [Google Scholar] [CrossRef] [PubMed]
- Tregoning, J.S.; Flight, K.E.; Higham, S.L.; Wang, Z.; Pierce, B.F. Progress of the COVID-19 vaccine effort: Viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat. Rev. Immunol. 2021, 21, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Khandker, S.S.; Godman, B.; Jawad, M.I.; Meghla, B.A.; Tisha, T.A.; Khondoker, M.U.; Haq, M.A.; Charan, J.; Talukder, A.A.; Azmuda, N.; et al. A systematic review on COVID-19 vaccine strategies, their effectiveness, and issues. Vaccines 2021, 9, 1387. [Google Scholar] [CrossRef]
- COVID-19 Vaccine Tracker and Landscape. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 14 November 2022).
- EMA. Safety of COVID-19 Vaccines. Available online: https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/safety-covid-19-vaccines (accessed on 14 November 2022).
- Wang, B.; Ping, Y. A comparative analysis of COVID-19 vaccination certificates in 12 countries/regions around the world: Rationalising health policies for international travel and domestic social activities during the pandemic. Health Policy 2022, 126, 755–762. [Google Scholar] [CrossRef]
- Duan, Y.; Shi, J.; Wang, Z.; Zhou, S.; Jin, Y.; Zheng, Z.-J. Disparities in COVID-19 vaccination among low-, middle-, and high-income countries: The mediating role of vaccination policy. Vaccines 2021, 9, 905. [Google Scholar] [CrossRef]
- Narodowy Program Szczepień Przeciw COVID-19. Available online: https://www.gov.pl/web/szczepimysie/narodowy-program-szczepien-przeciw-covid-19 (accessed on 22 August 2022).
- Huang, Y.; Yang, C.; Xu, X.; Xu, W.; Liu, S. Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef]
- Watanabe, Y.; Mendonça, L.; Allen, E.R.; Howe, A.; Lee, M.; Allen, J.D.; Chawla, H.; Pulido, D.; Donnellan, F.; Davies, H.; et al. Native-like SARS-CoV-2 spike glycoprotein expressed by ChAdOx1 NCoV-19/AZD1222 vaccine. ACS Cent. Sci. 2021, 7, 594–602. [Google Scholar] [CrossRef]
- Xia, X. Detailed dissection and critical evaluation of the Pfizer/BioNTech and Moderna MRNA vaccines. Vaccines 2021, 9, 734. [Google Scholar] [CrossRef] [PubMed]
- Mapa Zarażeń—COVID-HUB. Available online: https://covidhub.psnc.pl/mapa/ (accessed on 25 July 2022).
- Vaxzevria, COVID 19 Vaccine (ChAdOx1 S [Recombinant]). Available online: https://www.ema.europa.eu/en/documents/product-information/vaxzevria-previously-covid-19-vaccine-astrazeneca-epar-product-information_pl.pdf (accessed on 22 November 2022).
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 NCoV-19 (AZD1222) vaccine: A pooled analysis of four randomised trials. Lancet 2021, 397, 881–891. [Google Scholar] [CrossRef]
- Covid, P.-B. Vaccines and Related Biological Products Advisory Committee Meeting December 10, 2020. Available online: https://www.fda.gov/media/144245/download (accessed on 22 November 2022).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 MRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Deeba, E.; Krashias, G.; Constantinou, A.; Koptides, D.; Lambrianides, A.; Christodoulou, C. Evaluation of S1RBD-Specific IgG antibody responses following COVID-19 vaccination in healthcare professionals in Cyprus: A comparative look between the vaccines of Pfizer-BioNTech and AstraZeneca. Microorganisms 2022, 10, 967. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Stoesser, N.; Matthews, P.C.; Ayoubkhani, D.; Studley, R.; Bell, I.; Bell, J.I.; Newton, J.N.; Farrar, J.; Diamond, I.; et al. Antibody responses to SARS-CoV-2 vaccines in 45,965 adults from the general population of the United Kingdom. Nat. Microbiol. 2021, 6, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Pouwels, K.B.; Stoesser, N.; Matthews, P.C.; Diamond, I.; Studley, R.; Rourke, E.; Cook, D.; Bell, J.I.; Newton, J.N.; et al. Antibody responses and correlates of protection in the general population after two doses of the ChAdOx1 or BNT162b2 vaccines. Nat. Med. 2022, 28, 1072–1082. [Google Scholar] [CrossRef] [PubMed]
- Barin, B.; Kasap, U.; Selçuk, F.; Volkan, E.; Uluçkan, Ö. Comparison of SARS-CoV-2 anti-spike receptor binding domain IgG antibody responses after CoronaVac, BNT162b2, ChAdOx1 COVID-19 vaccines, and a single booster dose: A prospective, longitudinal population-based study. Lancet Microbe 2022, 3, e274–e283. [Google Scholar] [CrossRef] [PubMed]
- Ward, H.; Whitaker, M.; Flower, B.; Tang, S.N.; Atchison, C.; Darzi, A.; Donnelly, C.A.; Cann, A.; Diggle, P.J.; Ashby, D.; et al. Population antibody responses following COVID-19 vaccination in 212,102 individuals. Nat. Commun. 2022, 13, 907. [Google Scholar] [CrossRef] [PubMed]
- Kaura, A.; Trickey, A.; Shah, A.S.V.; Benedetto, U.; Glampson, B.; Mulla, A.; Mercuri, L.; Gautama, S.; Costelloe, C.E.; Goodman, I.; et al. Comparing the longer-term effectiveness of a single dose of the Pfizer-BioNTech and Oxford-AstraZeneca COVID-19 vaccines across the age spectrum. eClinicalMedicine 2022, 46, 101344. [Google Scholar] [CrossRef]
- Hall, V.; Foulkes, S.; Insalata, F.; Kirwan, P.; Saei, A.; Atti, A.; Wellington, E.; Khawam, J.; Munro, K.; Cole, M.; et al. Protection against SARS-CoV-2 after Covid-19 vaccination and previous infection. N. Engl. J. Med. 2022, 386, 1207–1220. [Google Scholar] [CrossRef]
- Menni, C.; May, A.; Polidori, L.; Louca, P.; Wolf, J.; Capdevila, J.; Hu, C.; Ourselin, S.; Steves, C.J.; Valdes, A.M.; et al. COVID-19 Vaccine waning and effectiveness and side-effects of boosters: A prospective community study from the ZOE COVID study. Lancet Infect. Dis. 2022, 22, 1002–1010. [Google Scholar] [CrossRef]
- Andrews, N.; Tessier, E.; Stowe, J.; Gower, C.; Kirsebom, F.; Simmons, R.; Gallagher, E.; Thelwall, S.; Groves, N.; Dabrera, G.; et al. Duration of protection against mild and severe disease by COVID-19 vaccines. N. Engl. J. Med. 2022, 386, 340–350. [Google Scholar] [CrossRef]
- Nordström, P.; Ballin, M.; Nordström, A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: A retrospective, total population Cohort Study in Sweden. Lancet 2022, 399, 814–823. [Google Scholar] [CrossRef]
- Tartof, S.Y.; Slezak, J.M.; Fischer, H.; Hong, V.; Ackerson, B.K.; Ranasinghe, O.N.; Frankland, T.B.; Ogun, O.A.; Zamparo, J.M.; Gray, S.; et al. Effectiveness of MRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective Cohort Study. Lancet 2021, 398, 1407–1416. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Luciani, A.; Borgonovo, K.; Ghilardi, M.; Parati, M.C.; Petrò, D.; Lonati, V.; Pesenti, A.; Cabiddu, M. Third dose of SARS-CoV-2 vaccine: A systematic review of 30 published studies. J. Med. Virol. 2022, 94, 2837–2844. [Google Scholar] [CrossRef] [PubMed]
- Barda, N.; Dagan, N.; Cohen, C.; Hernán, M.A.; Lipsitch, M.; Kohane, I.S.; Reis, B.Y.; Balicer, R.D. Effectiveness of a third dose of the BNT162b2 MRNA COVID-19 vaccine for preventing severe outcomes in Israel: An observational study. Lancet Lond. Engl. 2021, 398, 2093–2100. [Google Scholar] [CrossRef] [PubMed]
- Moreira, E.D.; Kitchin, N.; Xu, X.; Dychter, S.S.; Lockhart, S.; Gurtman, A.; Perez, J.L.; Zerbini, C.; Dever, M.E.; Jennings, T.W.; et al. Safety and efficacy of a third dose of BNT162b2 COVID-19 vaccine. N. Engl. J. Med. 2022, 386, 1910–1921. [Google Scholar] [CrossRef]
- Saciuk, Y.; Kertes, J.; Shamir Stein, N.; Ekka Zohar, A. Effectiveness of a third dose of BNT162b2 MRNA vaccine. J. Infect. Dis. 2022, 225, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Yorsaeng, R.; Suntronwong, N.; Phowatthanasathian, H.; Assawakosri, S.; Kanokudom, S.; Thongmee, T.; Vichaiwattana, P.; Auphimai, C.; Wongsrisang, L.; Srimuan, D.; et al. Immunogenicity of a third dose viral-vectored COVID-19 vaccine after receiving two-dose inactivated vaccines in healthy adults. Vaccine 2022, 40, 524–530. [Google Scholar] [CrossRef]
- Hall, V.G.; Ferreira, V.H.; Ku, T.; Ierullo, M.; Majchrzak-Kita, B.; Chaparro, C.; Selzner, N.; Schiff, J.; McDonald, M.; Tomlinson, G.; et al. Randomized trial of a third dose of MRNA-1273 vaccine in transplant recipients. N. Engl. J. Med. 2021, 385, 1244–1246. [Google Scholar] [CrossRef]
- Bensouna, I.; Caudwell, V.; Kubab, S.; Acquaviva, S.; Pardon, A.; Vittoz, N.; Bozman, D.-F.; Hanafi, L.; Faucon, A.-L.; Housset, P. SARS-CoV-2 antibody response after a third dose of the BNT162b2 vaccine in patients receiving maintenance hemodialysis or peritoneal dialysis. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2022, 79, 185–192.e1. [Google Scholar] [CrossRef]
- Pappas, G.; Saloustros, E.; Boutis, A.; Tsoukalas, N.; Nikolaou, M.; Christopoulou, A.; Agelaki, S.; Boukovinas, I.; Ardavanis, A.; Saridaki, Z. Vaccine third dose and cancer patients: Necessity or luxury? ESMO Open 2021, 6, 100306. [Google Scholar] [CrossRef]
- EMA. ECDC and EMA Update Recommendations on Additional Booster Doses of MRNA COVID-19 Vaccines. Available online: https://www.ema.europa.eu/en/news/ecdc-ema-update-recommendations-additional-booster-doses-mrna-covid-19-vaccines (accessed on 21 November 2022).
- Caini, S.; Martinoli, C.; La Vecchia, C.; Raimondi, S.; Bellerba, F.; D’Ecclesiis, O.; Sasso, C.; Basso, A.; Cammarata, G.; Gandini, S. SARS-CoV-2 circulation in the school setting: A systematic review and meta-analysis. Int. J. Environ. Res. Public. Health 2022, 19, 5384. [Google Scholar] [CrossRef]
- Viner, R.M.; Mytton, O.T.; Bonell, C.; Melendez-Torres, G.J.; Ward, J.; Hudson, L.; Waddington, C.; Thomas, J.; Russell, S.; van der Klis, F.; et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: A systematic review and meta-analysis. JAMA Pediatr. 2021, 175, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Boey, L.; Roelants, M.; Merckx, J.; Hens, N.; Desombere, I.; Duysburgh, E.; Vandermeulen, C. Age-Dependent Seroprevalence of SARS-CoV-2 antibodies in school-aged children from areas with low and high community transmission. Eur. J. Pediatr. 2022, 181, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.A.; Saliba, V.; Lopez Bernal, J.; Ramsay, M.E.; Ladhani, S.N. SARS-CoV-2 infection and transmission in educational settings: A prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect. Dis. 2021, 21, 344–353. [Google Scholar] [CrossRef]
- Goldfarb, D.M.; Mâsse, L.C.; Watts, A.W.; Hutchison, S.M.; Muttucomaroe, L.; Bosman, E.S.; Barakauskas, V.E.; Choi, A.; Dhillon, N.; Irvine, M.A.; et al. SARS-CoV-2 seroprevalence among Vancouver public school staff in British Columbia, Canada: A cross-sectional study. BMJ Open 2022, 12, e057846. [Google Scholar] [CrossRef]
- Ladhani, S.N.; Ireland, G.; Baawuah, F.; Beckmann, J.; Okike, I.O.; Ahmad, S.; Garstang, J.; Brent, A.J.; Brent, B.; Walker, J.; et al. SARS-CoV-2 infection, antibody positivity and seroconversion rates in staff and students following full reopening of secondary schools in England: A prospective Cohort Study, September–December 2020. eClinicalMedicine 2021, 37, 100948. [Google Scholar] [CrossRef]
- Ladhani, S.N.; Ireland, G.; Baawuah, F.; Beckmann, J.; Okike, I.O.; Ahmad, S.; Garstang, J.; Brent, A.J.; Brent, B.; Aiano, F.; et al. Emergence of the delta variant and risk of SARS-CoV-2 infection in secondary school students and staff: Prospective surveillance in 18 schools, England. eClinicalMedicine 2022, 45, 101319. [Google Scholar] [CrossRef]
- Lorent, D.; Nowak, R.; Luwański, D.; Pisarska-Krawczyk, M.; Figlerowicz, M.; Zmora, P. The longitudinal analysis on the anti-SARS-CoV-2 antibodies among healthcare workers in Poland—Before and after BNT126b2 MRNA COVID-19 vaccination. Vaccines 2022, 10, 1576. [Google Scholar] [CrossRef] [PubMed]
- Ebinger, J.E.; Joung, S.; Liu, Y.; Wu, M.; Weber, B.; Claggett, B.; Botting, P.G.; Sun, N.; Driver, M.; Kao, Y.H.; et al. Demographic and clinical characteristics associated with variations in antibody response to BNT162b2 COVID-19 vaccination among healthcare workers at an academic medical centre: A longitudinal Cohort Analysis. BMJ Open 2022, 12, e059994. [Google Scholar] [CrossRef] [PubMed]
- Piccoli, L.; Ferrari, P.; Piumatti, G.; Jovic, S.; Rodriguez, B.F.; Mele, F.; Giacchetto-Sasselli, I.; Terrot, T.; Silacci-Fregni, C.; Cameroni, E.; et al. Risk assessment and seroprevalence of SARS-CoV-2 infection in healthcare workers of COVID-19 and non-COVID-19 hospitals in Southern Switzerland. Lancet Reg. Health–Eur. 2021, 1, 100013. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers: A systematic review and meta-analysis. J. Hosp. Infect. 2021, 108, 120–134. [Google Scholar] [CrossRef]
- Menni, C.; Klaser, K.; May, A.; Polidori, L.; Capdevila, J.; Louca, P.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Merino, J.; et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID symptom study app in the UK: A prospective observational study. Lancet Infect. Dis. 2021, 21, 939–949. [Google Scholar] [CrossRef] [PubMed]
- EMA. COVID-19 Vaccine AstraZeneca: Benefits Still Outweigh the Risks despite Possible Link to Rare Blood Clots with Low Platelets. Available online: https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-benefits-still-outweigh-risks-despite-possible-link-rare-blood-clots (accessed on 21 November 2022).
- Marking, U.; Havervall, S.; Greilert-Norin, N.; Ng, H.; Blom, K.; Nilsson, P.; Phillipson, M.; Hober, S.; Nilsson, C.; Mangsbo, S.; et al. Duration of SARS-CoV-2 immune responses up to six months following homologous or heterologous primary immunization with ChAdOx1 NCoV-19 and BNT162b2 MRNA vaccines. Vaccines 2022, 10, 359. [Google Scholar] [CrossRef] [PubMed]
- Nauczyciele Wg Wieku, Płci, Typu Podmiotu i Województw w Roku Szkolnym 2020/2021—Otwarte Dane. Available online: https://dane.gov.pl/pl/dataset/811,nauczyciele-w-osobach-i-etatach/resource/31197/table?page=1&per_page=20&q=&sort= (accessed on 21 November 2022).
| Study Participants | ||
|---|---|---|
| Primary School Teachers | Academic Teachers | |
| Number of participants | 36 (100%) | 45 (100%) |
| Sex | ||
| Female | 33 (91.67%) | 39 (86.67%) |
| Male | 3 (8.33%) | 6 (13.33%) |
| Age | ||
| <30 y.o. | 6 (16.67%) | 15 (33.33%) |
| 31–40 y.o. | 3 (8.83%) | 12 (26.67%) |
| 41–50 y.o | 12 (33.33%) | 12 (26.67%) |
| 51–60 y.o. | 13 (36.10%) a | 2 (4.44%) b |
| >60 y.o. | 2 (5.56%) | 4 (8.89%) |
| Comorbidities and CDs | ||
| None | 19 (52.78%) a | 36 (80.00%) b |
| Circulatory system CDs, i.e., hypertension | 12 (33.33%) | 4 (8.89%) |
| Respiratory system CDs, i.e., asthma | 2 (5.56%) | 1 (2.22%) |
| Infectious CDs, i.e., HIV/AIDS | - | - |
| Chronic kidney diseases | - | - |
| Digestive track CDs, i.e., Crohn diseases | - | - |
| Autoimmunological CDs, i.e., allergies | 4 (11.11%) | 4 (8.89%) |
| Neoplasmic diseases, i.e., cancer | - | - |
| Metabolic diseases, i.e., diabetes | - | - |
| Mental disorders, i.e., depression | 1 (2.78%) | 1 (2.22%) |
| COVID-19 | ||
| COVID-19 history | - | - |
| anti-SARS-CoV-2 N antibodies presence | 0 | 0 |
| COVID-19 vaccinated individuals | 36 (100%) | 45 (100%) |
| Type of vaccines | vector—ChAdOx1 (Astra Zeneca) | mRNA—BNT162b2 (Pfizer/BioNTech) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorent, D.; Nowak, R.; Jankowska, M.; Kuszel, Ł.; Zmora, P. Differences in BNT126b2 and ChAdOx1 Homologous Vaccination Antibody Response among Teachers in Poznan, Poland. Vaccines 2023, 11, 118. https://doi.org/10.3390/vaccines11010118
Lorent D, Nowak R, Jankowska M, Kuszel Ł, Zmora P. Differences in BNT126b2 and ChAdOx1 Homologous Vaccination Antibody Response among Teachers in Poznan, Poland. Vaccines. 2023; 11(1):118. https://doi.org/10.3390/vaccines11010118
Chicago/Turabian StyleLorent, Dagny, Rafał Nowak, Monika Jankowska, Łukasz Kuszel, and Paweł Zmora. 2023. "Differences in BNT126b2 and ChAdOx1 Homologous Vaccination Antibody Response among Teachers in Poznan, Poland" Vaccines 11, no. 1: 118. https://doi.org/10.3390/vaccines11010118
APA StyleLorent, D., Nowak, R., Jankowska, M., Kuszel, Ł., & Zmora, P. (2023). Differences in BNT126b2 and ChAdOx1 Homologous Vaccination Antibody Response among Teachers in Poznan, Poland. Vaccines, 11(1), 118. https://doi.org/10.3390/vaccines11010118










