Immunogenicity and Safety of COVID-19 Vaccines among People Living with HIV: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Risk of Bias Assessment
2.5. Data Synthesis and Statistical Analysis
3. Results
3.1. Characteristics of Included Studies
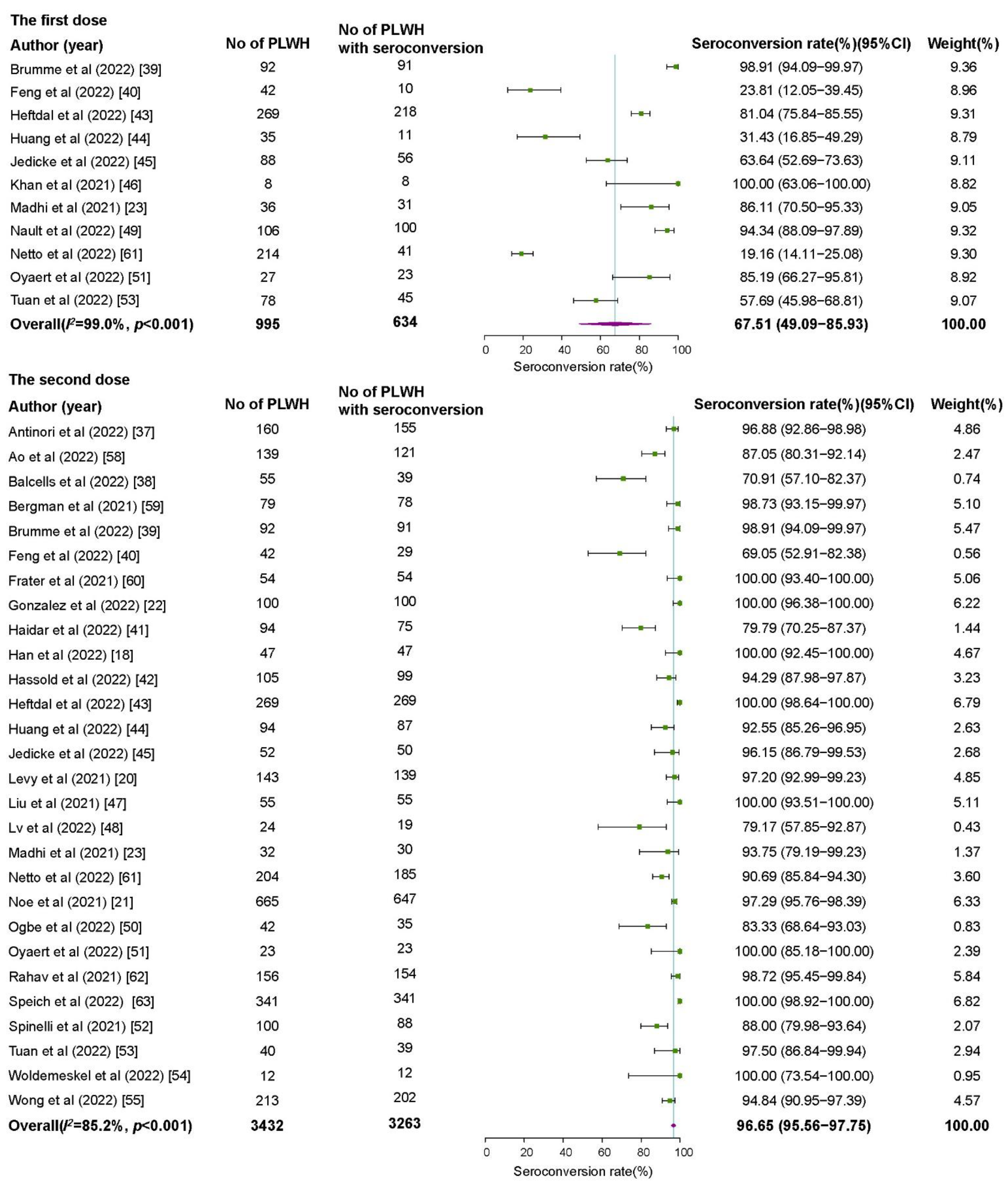
3.2. Seroconversion Rates among PLWH
3.3. Comparison of Seroconversion between PLWH and Healthy Controls
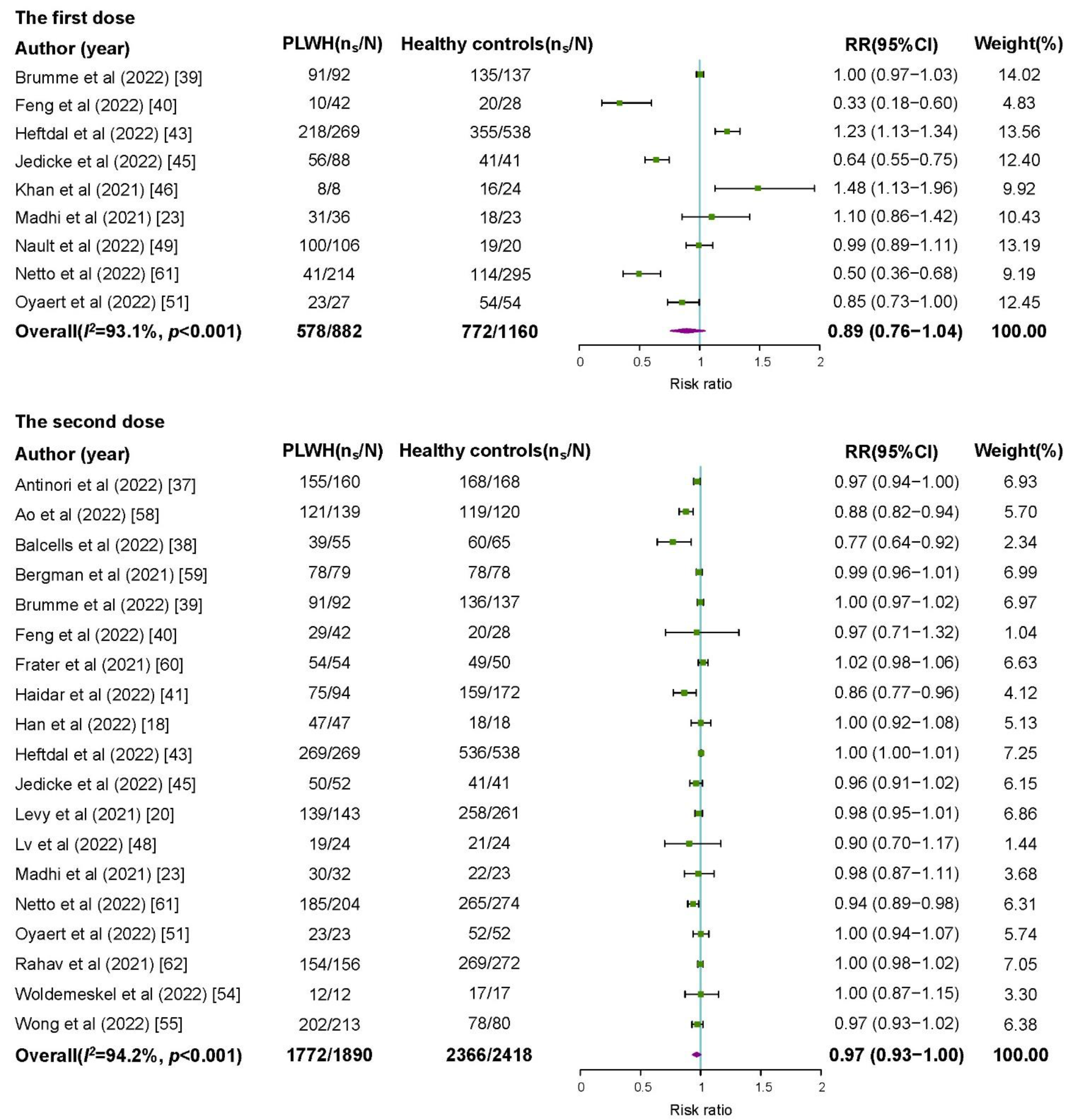
3.4. Geometric Mean Titers between PLWH and Healthy Controls
3.5. Safety of COVID-19 Vaccines among PLWH
3.6. Sensitivity Analysis and Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 27 May 2022).
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Mirzaei, H.; McFarland, W.; Karamouzian, M.; Sharifi, H. COVID-19 among People Living with HIV: A Systematic Review. AIDS Behav. 2021, 25, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Shields, A.M.; Burns, S.O.; Savic, S.; Richter, A.G. COVID-19 in patients with primary and secondary immunodeficiency: The United Kingdom experience. J. Allergy Clin. Immunol. 2021, 147, 870–875.e871. [Google Scholar] [CrossRef]
- Geretti, A.M.; Stockdale, A.J.; Kelly, S.H.; Cevik, M.; Collins, S.; Waters, L.; Villa, G.; Docherty, A.; Harrison, E.M.; Turtle, L.; et al. Outcomes of Coronavirus Disease 2019 (COVID-19) Related Hospitalization among People with Human Immunodeficiency Virus (HIV) in the ISARIC World Health Organization (WHO) Clinical Characterization Protocol (UK): A Prospective Observational Study. Clin. Infect. Dis. 2021, 73, e2095–e2106. [Google Scholar] [CrossRef]
- Ssentongo, P.; Heilbrunn, E.S.; Ssentongo, A.E.; Advani, S.; Chinchilli, V.M.; Nunez, J.J.; Du, P. Epidemiology and outcomes of COVID-19 in HIV-infected individuals: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 6283. [Google Scholar] [CrossRef]
- WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: Final results of the WHO Solidarity randomised trial and updated meta-analyses. Lancet 2022, 399, 1941–1953. [Google Scholar] [CrossRef]
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, X.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality: Systematic review and meta-analysis. BMJ 2021, 375, e068302. [Google Scholar] [CrossRef]
- Wang, J.; Lyu, Y.; Zhang, H.; Jing, R.; Lai, X.; Feng, H.; Knoll, M.D.; Fang, H. Willingness to pay and financing preferences for COVID-19 vaccination in China. Vaccine 2021, 39, 1968–1976. [Google Scholar] [CrossRef]
- Skowronski, D.M.; De Serres, G. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2021, 384, 1576–1577. [Google Scholar] [CrossRef] [PubMed]
- Moreira, E.D., Jr.; Kitchin, N.; Xu, X.; Dychter, S.S.; Lockhart, S.; Gurtman, A.; Perez, J.L.; Zerbini, C.; Dever, M.E.; Jennings, T.W.; et al. Safety and Efficacy of a Third Dose of BNT162b2 COVID-19 Vaccine. N. Engl. J. Med. 2022, 386, 1910–1921. [Google Scholar] [CrossRef] [PubMed]
- Dunkle, L.M.; Kotloff, K.L.; Gay, C.L.; Áñez, G.; Adelglass, J.M.; Barrat Hernández, A.Q.; Harper, W.L.; Duncanson, D.M.; McArthur, M.A.; Florescu, D.F.; et al. Efficacy and Safety of NVX-CoV2373 in Adults in the United States and Mexico. N. Engl. J. Med. 2022, 386, 531–543. [Google Scholar] [CrossRef]
- Vallée, A.; Fourn, E.; Majerholc, C.; Touche, P.; Zucman, D. COVID-19 Vaccine Hesitancy among French People Living with HIV. Vaccines 2021, 9, 302. [Google Scholar] [CrossRef]
- Bogart, L.M.; Ojikutu, B.O.; Tyagi, K.; Klein, D.J.; Mutchler, M.G.; Dong, L.; Lawrence, S.J.; Thomas, D.R.; Kellman, S. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy among Black Americans Living with HIV. J. Acquir. Immune Defic. Syndr. 2021, 86, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Chai, R.; Yang, J.; Zhang, X.; Huang, X.; Yu, M.; Fu, G.; Lan, G.; Qiao, Y.; Li, S.; Yao, Y.; et al. Reasons of COVID-19 Vaccine Hesitancy among Chinese People Living with HIV/AIDS: A Structural Equation Modeling Analysis. JMIR Public Health Surveill. 2022, 8, e33995. [Google Scholar] [CrossRef]
- Han, X.; Yu, X.; Han, Y.; Fang, Q.; Shen, C.; Liu, H.; Wang, P.; Wang, Y.; Li, X. Safety and Immunogenicity of Inactivated COVID-19 Vaccines among People Living with HIV in China. Infect. Drug Resist. 2022, 15, 2091–2100. [Google Scholar] [CrossRef]
- Touizer, E.; Alrubayyi, A.; Rees-Spear, C.; Fisher-Pearson, N.; Griffith, S.A.; Muir, L.; Pellegrino, P.; Waters, L.; Burns, F.; Kinloch, S.; et al. Failure to seroconvert after two doses of BNT162b2 SARS-CoV-2 vaccine in a patient with uncontrolled HIV. Lancet HIV 2021, 8, e317–e318. [Google Scholar] [CrossRef]
- Levy, I.; Wieder-Finesod, A.; Litchevsky, V.; Biber, A.; Indenbaum, V.; Olmer, L.; Huppert, A.; Mor, O.; Goldstein, M.; Levin, E.G.; et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in people living with HIV-1. Clin. Microbiol. Infect. 2021, 27, 1851–1855. [Google Scholar] [CrossRef]
- Noe, S.; Ochana, N.; Wiese, C.; Schabaz, F.; Von Krosigk, A.; Heldwein, S.; Rasshofer, R.; Wolf, E.; Jonsson-Oldenbuettel, C. Humoral response to SARS-CoV-2 vaccines in people living with HIV. Infection 2021, 50, 617–623. [Google Scholar] [CrossRef]
- González de Aledo, M.; Cañizares, A.; Vázquez-Rodríguez, P.; Castro, Á.; Moldes, L.; López, S.; Míguez, E.; Bou, G.; Mena, Á. Safety and Immunogenicity of SARS-CoV-2 vaccines in people with HIV. Aids 2022, 36, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Madhi, S.A.; Koen, A.L.; Izu, A.; Fairlie, L.; Cutland, C.L.; Baillie, V.; Padayachee, S.D.; Dheda, K.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in people living with and without HIV in South Africa: An interim analysis of a randomised, double-blind, placebo-controlled, phase 1B/2A trial. Lancet HIV 2021, 8, e568–e580. [Google Scholar] [CrossRef]
- Ruddy, J.A.; Boyarsky, B.J.; Bailey, J.R.; Karaba, A.H.; Garonzik-Wang, J.M.; Segev, D.L.; Durand, C.M.; Werbel, W.A. Safety and antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in persons with HIV. Aids 2021, 35, 2399–2401. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Zhang, Y.; Zeng, G.; Pan, H.; Li, C.; Hu, Y.; Chu, K.; Han, W.; Chen, Z.; Tang, R.; Yin, W.; et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: A randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2021, 21, 181–192. [Google Scholar] [CrossRef]
- Haas, J.W.; Bender, F.L.; Ballou, S.; Kelley, J.M.; Wilhelm, M.; Miller, F.G.; Rief, W.; Kaptchuk, T.J. Frequency of Adverse Events in the Placebo Arms of COVID-19 Vaccine Trials: A Systematic Review and Meta-analysis. JAMA Netw. Open 2022, 5, e2143955. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 12 April 2022).
- Rostom, A.; Dubé, C.; Cranney, A.; Saloojee, N.; Sy, R.; Garritty, C.; Sampson, M.; Zhang, L.; Yazdi, F.; Mamaladze, V.; et al. Appendix D. Quality Assessment Forms. In Celiac Disease; Evidence Reports/Technology Assessments, No. 104; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, September 2004. Available online: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (accessed on 24 May 2022).
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Muka, T.; Glisic, M.; Milic, J.; Verhoog, S.; Bohlius, J.; Bramer, W.; Chowdhury, R.; Franco, O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2020, 35, 49–60. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Beaudry, G.; Yu, R.; Perry, A.E.; Fazel, S. Effectiveness of psychological interventions in prison to reduce recidivism: A systematic review and meta-analysis of randomised controlled trials. Lancet Psychiatry 2021, 8, 759–773. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Antinori, A.; Cicalini, S.; Meschi, S.; Bordoni, V.; Lorenzini, P.; Vergori, A.; Lanini, S.; De Pascale, L.; Matusali, G.; Mariotti, D.; et al. Humoral and cellular immune response elicited by mRNA vaccination against SARS-CoV-2 in people living with HIV (PLWH) receiving antiretroviral therapy (ART) according with current CD4 T-lymphocyte count. Clin. Infect. Dis. 2022, 75, e552–e563. [Google Scholar] [CrossRef]
- Balcells, M.E.; Le Corre, N.; Durán, J.; Ceballos, M.E.; Vizcaya, C.; Mondaca, S.; Dib, M.; Rabagliati, R.; Sarmiento, M.; Burgos, P.I.; et al. Reduced immune response to inactivated SARS-CoV-2 vaccine in a cohort of immunocompromised patients in Chile. Clin. Infect. Dis. 2022, 75, e594–e602. [Google Scholar] [CrossRef] [PubMed]
- Brumme, Z.L.; Mwimanzi, F.; Lapointe, H.R.; Cheung, P.K.; Sang, Y.; Duncan, M.C.; Yaseen, F.; Agafitei, O.; Ennis, S.; Ng, K.; et al. Humoral immune responses to COVID-19 vaccination in people living with HIV receiving suppressive antiretroviral therapy. NPJ Vaccines 2022, 7, 28. [Google Scholar] [CrossRef]
- Feng, Y.; Zhang, Y.; He, Z.; Huang, H.; Tian, X.; Wang, G.; Chen, D.; Ren, Y.; Jia, L.; Wang, W.; et al. Immunogenicity of an inactivated SARS-CoV-2 vaccine in people living with HIV-1: A non-randomized cohort study. EClinicalMedicine 2022, 43, 101226. [Google Scholar] [CrossRef]
- Haidar, G.; Agha, M.; Bilderback, A.; Lukanski, A.; Linstrum, K.; Troyan, R.; Rothenberger, S.; McMahon, D.K.; Crandall, M.D.; Sobolewksi, M.D.; et al. Prospective evaluation of COVID-19 vaccine responses across a broad spectrum of immunocompromising conditions: The COVICS study. Clin. Infect. Dis. 2022, 75, e630–e644. [Google Scholar] [CrossRef] [PubMed]
- Hassold, N.; Brichler, S.; Ouedraogo, E.; Leclerc, D.; Carroue, S.; Gater, Y.; Alloui, C.; Carbonnelle, E.; Bouchaud, O.; Mechai, F.; et al. Impaired antibody response to COVID-19 vaccination in advanced HIV infection. Aids 2022, 36, F1–F5. [Google Scholar] [CrossRef]
- Heftdal, L.D.; Knudsen, A.D.; Hamm, S.R.; Hansen, C.B.; Møller, D.L.; Pries-Heje, M.; Fogh, K.; Hasselbalch, R.B.; Jarlhelt, I.; Pérez-Alós, L.; et al. Humoral response to two doses of BNT162b2 vaccination in people with HIV. J. Intern. Med. 2022, 291, 513–518. [Google Scholar] [CrossRef]
- Huang, X.; Yan, Y.; Su, B.; Xiao, D.; Yu, M.; Jin, X.; Duan, J.; Zhang, X.; Zheng, S.; Fang, Y.; et al. Comparing Immune Responses to Inactivated Vaccines against SARS-CoV-2 between People Living with HIV and HIV-Negative Individuals: A Cross-Sectional Study in China. Viruses 2022, 14, 277. [Google Scholar] [CrossRef] [PubMed]
- Jedicke, N.; Stankov, M.V.; Cossmann, A.; Dopfer-Jablonka, A.; Knuth, C.; Ahrenstorf, G.; Ramos, G.M.; Behrens, G.M.N. Humoral immune response following prime and boost BNT162b2 vaccination in people living with HIV on antiretroviral therapy. HIV Med. 2022, 23, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.; Lustig, G.; Bernstein, M.; Archary, D.; Cele, S.; Karim, F.; Smith, M.; Ganga, Y.; Jule, Z.; Reedoy, K.; et al. Immunogenicity of SARS-CoV-2 infection and Ad26.CoV2.S vaccination in people living with HIV. Clin. Infect. Dis. 2021, 75, e857–e864. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Han, J.; Li, X.; Chen, D.; Zhao, X.; Qiu, Y.; Zhang, L.; Xiao, J.; Li, B.; Zhao, H. COVID-19 Vaccination in People Living with HIV (PLWH) in China: A Cross Sectional Study of Vaccine Hesitancy, Safety, and Immunogenicity. Vaccines 2021, 9, 1458. [Google Scholar] [CrossRef]
- Lv, Z.; Li, Q.; Feng, Z.; Zheng, X.; Yin, N.; Yang, H.; Gu, Q.; Ying, S.; Qi, Y.; Li, X.; et al. Inactivated SARS-CoV-2 vaccines elicit immunogenicity and T-cell responses in people living with HIV. Int. Immunopharmacol. 2022, 102, 108383. [Google Scholar] [CrossRef]
- Nault, L.; Marchitto, L.; Goyette, G.; Tremblay-Sher, D.; Fortin, C.; Martel-Laferrière, V.; Trottier, B.; Richard, J.; Durand, M.; Kaufmann, D.; et al. COVID-19 vaccine immunogenicity in people living with HIV-1. Vaccine 2022, 40, 3633–3637. [Google Scholar] [CrossRef]
- Ogbe, A.; Pace, M.; Bittaye, M.; Tipoe, T.; Adele, S.; Alagaratnam, J.; Aley, P.K.; Ansari, M.A.; Bara, A.; Broadhead, S.; et al. Durability of ChAdOx1 nCoV-19 vaccination in people living with HIV. JCI Insight 2022, 7, e157031. [Google Scholar] [CrossRef]
- Oyaert, M.; De Scheerder, M.A.; Van Herrewege, S.; Laureys, G.; Van Assche, S.; Cambron, M.; Naesens, L.; Hoste, L.; Claes, K.; Haerynck, F.; et al. Evaluation of Humoral and Cellular Responses in SARS-CoV-2 mRNA Vaccinated Immunocompromised Patients. Front. Immunol. 2022, 13, 858399. [Google Scholar] [CrossRef]
- Spinelli, M.A.; Peluso, M.J.; Lynch, K.L.; Yun, C.; Glidden, D.V.; Henrich, T.J.; Deeks, S.G.; Gandhi, M. Differences in Post-mRNA Vaccination SARS-CoV-2 IgG Concentrations and Surrogate Virus Neutralization Test Response by HIV Status and Type of Vaccine: A Matched Case-Control Observational Study. Clin. Infect. Dis. 2021, 75, e916–e919. [Google Scholar] [CrossRef]
- Tuan, J.J.; Zapata, H.; Critch-Gilfillan, T.; Ryall, L.; Turcotte, B.; Mutic, S.; Andrews, L.; Roh, M.E.; Friedland, G.; Barakat, L.; et al. Qualitative assessment of anti-SARS-CoV-2 spike protein immunogenicity (QUASI) after COVID-19 vaccination in older people living with HIV. HIV Med. 2022, 23, 178–185. [Google Scholar] [CrossRef]
- Woldemeskel, B.A.; Karaba, A.H.; Garliss, C.C.; Beck, E.J.; Wang, K.H.; Laeyendecker, O.; Cox, A.L.; Blankson, J.N. The BNT162b2 mRNA Vaccine Elicits Robust Humoral and Cellular Immune Responses in People Living with Human Immunodeficiency Virus (HIV). Clin. Infect. Dis. 2022, 74, 1268–1270. [Google Scholar] [CrossRef] [PubMed]
- Wong, N.S.; Wong, B.C.K.; Chan, J.M.C.; Wong, K.H.; Tsang, O.T.Y.; Mok, C.K.P.; Hui, D.S.C.; Lee, S.S.; Chan, D.P.C. Surrogate neutralisation responses following SARS-CoV-2 vaccination in people living with HIV—Comparison between inactivated and mRNA vaccine. Aids 2022, 36, 1255–1264. [Google Scholar] [CrossRef] [PubMed]
- Milano, E.; Ricciardi, A.; Casciaro, R.; Pallara, E.; De Vita, E.; Bavaro, D.F.; Larocca, A.M.V.; Stefanizzi, P.; Tafuri, S.; Saracino, A. Immunogenicity and safety of the BNT162b2 COVID-19 mRNA vaccine in PLWH: A monocentric study in Bari, Italy. J. Med. Virol. 2022, 94, 2230–2236. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Zhang, Y.; Ming, F.; Zou, S.; Wu, M.; Guo, W.; Tang, W.; Liang, K. Adverse events of inactivated COVID-19 vaccine in HIV-infected adults. AIDS Res. Ther. 2021, 18, 92. [Google Scholar] [CrossRef] [PubMed]
- Ao, L.; Lu, T.; Cao, Y.; Chen, Z.; Wang, Y.; Li, Z.; Ren, X.; Xu, P.; Peng, M.; Chen, M.; et al. Safety and immunogenicity of inactivated SARS-CoV-2 vaccines in people living with HIV. Emerg. Microbes Infect. 2022, 11, 1126–1134. [Google Scholar] [CrossRef]
- Bergman, P.; Blennow, O.; Hansson, L.; Mielke, S.; Nowak, P.; Chen, P.; Söderdahl, G.; Österborg, A.; Smith, C.I.E.; Wullimann, D.; et al. Safety and efficacy of the mRNA BNT162b2 vaccine against SARS-CoV-2 in five groups of immunocompromised patients and healthy controls in a prospective open-label clinical trial. EBioMedicine 2021, 74, 103705. [Google Scholar] [CrossRef]
- Frater, J.; Ewer, K.J.; Ogbe, A.; Pace, M.; Adele, S.; Adland, E.; Alagaratnam, J.; Aley, P.K.; Ali, M.; Ansari, M.A.; et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: A single-arm substudy of a phase 2/3 clinical trial. Lancet HIV 2021, 8, e474–e485. [Google Scholar] [CrossRef]
- Netto, L.C.; Ibrahim, K.Y.; Picone, C.M.; Alves, A.; Aniceto, E.V.; Santiago, M.R.; Parmejani, P.S.S.; Aikawa, N.E.; Medeiros-Ribeiro, A.C.; Pasoto, S.G.; et al. Safety and immunogenicity of CoronaVac in people living with HIV: A prospective cohort study. Lancet HIV 2022, 9, e323–e331. [Google Scholar] [CrossRef]
- Rahav, G.; Lustig, Y.; Lavee, J.; Ohad, B.; Magen, H.; Hod, T.; Noga, S.-T.; Shmueli, E.S.; Drorit, M.; Ben-Ari, Z.; et al. BNT162b2 mRNA COVID-19 vaccination in immunocompromised patients: A prospective cohort study. EClinicalMedicine 2021, 41, 101158. [Google Scholar] [CrossRef]
- Speich, B.; Chammartin, F.; Abela, I.A.; Amico, P.; Stoeckle, M.P.; Eichenberger, A.L.; Hasse, B.; Braun, D.L.; Schuurmans, M.M.; Müller, T.F.; et al. Antibody response in immunocompromised patients after the administration of SARS-CoV-2 vaccine BNT162b2 or mRNA-1273: A randomised controlled trial. Clin. Infect. Dis. 2022, 75, e585–e593. [Google Scholar] [CrossRef]
- Portillo, V.; Fedeli, C.; Ustero Alonso, P.; Petignat, I.; Mereles Costa, E.C.; Sulstarova, A.; Jaksic, C.; Yerly, S.; Calmy, A. Impact on HIV-1 RNA Levels and Antibody Responses Following SARS-CoV-2 Vaccination in HIV-Infected Individuals. Front. Immunol. 2021, 12, 820126. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Wong, S.Y.; Chai, L.Y.A.; Lee, S.C.; Lee, M.X.; Muthiah, M.D.; Tay, S.H.; Teo, C.B.; Tan, B.K.J.; Chan, Y.H.; et al. Efficacy of COVID-19 vaccines in immunocompromised patients: Systematic review and meta-analysis. BMJ 2022, 376, e068632. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Peng, Z.; Luo, W.; Si, S.; Mo, M.; Zhou, H.; Xin, X.; Liu, H.; Yu, Y. Efficacy and Safety of COVID-19 Vaccines in Phase III Trials: A Meta-Analysis. Vaccines 2021, 9, 582. [Google Scholar] [CrossRef] [PubMed]
- El Chaer, F.; El Sahly, H.M. Vaccination in the Adult Patient Infected with HIV: A Review of Vaccine Efficacy and Immunogenicity. Am. J. Med. 2019, 132, 437–446. [Google Scholar] [CrossRef]

| No. of Studies | No. of PLWH | Seroconversion Rate (%) (95%CI) | I2 (%) | p Value for Heterogeneity | Weight (%) | p Value for Subgroup Differences | |
|---|---|---|---|---|---|---|---|
| The first dose | |||||||
| Overall | 11 | 995 | 67.51 (49.09–85.93) | 99.0 | <0.001 | 100.0 | |
| Continent | <0.001 | ||||||
| Africa | 2 | 44 | 92.15 (78.66–100.00) | 52.6 | 0.147 | 17.9 | |
| Asia | 2 | 77 | 26.95 (17.08–36.83) | 0.0 | 0.457 | 17.7 | |
| Europe | 3 | 283 | 76.51 (64.51–88.51) | 80.9 | 0.005 | 27.3 | |
| North America | 3 | 276 | 85.19 (78.66–100.00) | 96.3 | <0.001 | 27.7 | |
| South America | 1 | 214 | 19.16 (13.89–24.43) | NA | NA | 9.3 | |
| Study design | 0.036 | ||||||
| Cross-sectional study | 2 | 113 | 45.14 (19.42–70.85) | 86.5 | 0.006 | 17.9 | |
| Cohort study | 6 | 796 | 73.71 (49.11–98.30) | 99.4 | <0.001 | 55.3 | |
| Non-randomized clinical trial | 2 | 50 | 61.81 (0.00–100.00) | 98.3 | <0.001 | 17.8 | |
| Randomized clinical trial | 1 | 36 | 86.11 (74.81–97.41) | NA | NA | 9.0 | |
| Vaccine type | <0.001 | ||||||
| Adenovirus vector vaccines | 2 | 44 | 92.15 (78.66–100.00) | 52.6 | 0.147 | 19.7 | |
| Inactivated virus vaccines | 3 | 291 | 21.69 (15.74–27.63) | 17.2 | 0.299 | 29.9 | |
| mRNA vaccines | 5 | 568 | 76.81 (64.23–89.38) | 93.4 | <0.001 | 50.4 | |
| Time interval between vaccination and antibody testing | 0.623 | ||||||
| < 28 days | 5 | 568 | 76.81 (64.23–89.38) | 93.4 | <0.001 | 50.1 | |
| ≥ 28 days | 5 | 392 | 65.55 (22.55–100.00) | 99.5 | <0.001 | 49.9 | |
| CD4+ T-cell counts | 0.369 | ||||||
| <500 cells/μL | 1 | 64 | 15.62 (6.73–24.52) | NA | NA | NA | |
| ≥500 cells/μL | 1 | 150 | 20.67 (14.19–27.15) | NA | NA | NA | |
| The second dose | |||||||
| Overall | 28 | 3432 | 96.65 (95.56–97.75) | 85.2 | <0.001 | 100.0 | |
| Continent | 0.011 | ||||||
| Africa | 1 | 32 | 93.75 (85.36–100.00) | NA | NA | 1.4 | |
| Asia | 9 | 913 | 94.83 (91.82–97.84) | 83.8 | <0.001 | 31.1 | |
| Europe | 11 | 1890 | 98.87 (97.96–99.77) | 74.1 | 0.007 | 50.3 | |
| North America | 5 | 338 | 93.11 (86.66–99.56) | 85.9 | <0.001 | 12.9 | |
| South America | 2 | 259 | 81.64 (62.33–100.00) | 89.4 | 0.002 | 4.3 | |
| Study design | 0.014 | ||||||
| Cross-sectional study | 6 | 1059 | 97.74 (95.80–99.67) | 72.3 | 0.003 | 26.4 | |
| Cohort study | 14 | 1659 | 95.55 (93.45–97.65) | 87.4 | <0.001 | 51.3 | |
| Case-control study | 1 | 100 | 88.00 (81.63–94.37) | NA | NA | 2.1 | |
| Non-randomized clinical trial | 5 | 241 | 90.53 (83.83–97.21) | 87.0 | <0.001 | 12.0 | |
| Randomized clinical trial | 2 | 373 | 98.34 (92.92–100.00) | 53.0 | 0.145 | 8.2 | |
| Vaccine type | <0.001 | ||||||
| Adenovirus vector vaccines | 3 | 128 | 93.68 (84.63–100.00) | 79.0 | 0.009 | 8.2 | |
| Inactivated virus vaccines | 9 | 734 | 88.62 (83.21–94.03) | 89.6 | <0.001 | 24.2 | |
| mRNA vaccines | 13 | 1614 | 99.14 (98.43–99.85) | 57.6 | 0.005 | 67.6 | |
| Time interval between vaccination and antibody testing | 0.011 | ||||||
| ≤14 days | 8 | 653 | 98.66 (96.78–100.00) | 73.7 | <0.001 | 38.8 | |
| 15–28 days | 6 | 620 | 95.34 (92.04–98.83) | 87.1 | <0.001 | 27.8 | |
| >28 days | 9 | 1070 | 92.89 (89.40–96.38) | 89.7 | <0.001 | 33.3 | |
| CD4+ T-cell counts | 0.044 | ||||||
| <500 cells/μL | 4 | 224 | 91.44 (85.77–97.11) | 58.6 | 0.064 | 42.6 | |
| ≥500 cells/μL | 3 | 270 | 97.99 (95.09–100.00) | 65.5 | 0.055 | 57.4 | |
| No. of Studies | No. of PLWH | RR (95%CI) | I2 (%) | p Value for Heterogeneity | Weight (%) | p Value for Subgroup Differences | |
|---|---|---|---|---|---|---|---|
| The first dose | |||||||
| Overall | 9 | 882 | 0.89 (0.76–1.04) | 93.1 | <0.001 | 100.0 | |
| Continent | <0.001 | ||||||
| Africa | 2 | 44 | 1.27 (0.93–1.74) | 64.3 | 0.094 | 20.4 | |
| Asia | 1 | 42 | 0.33 (0.18–0.60) | NA | NA | 4.8 | |
| Europe | 3 | 384 | 0.88 (0.58–1.33) | 96.8 | <0.001 | 38.4 | |
| North America | 2 | 198 | 1.00 (0.97–1.03) | 0.0 | 0.827 | 27.2 | |
| South America | 1 | 214 | 0.50 (0.36–0.68) | NA | NA | 9.2 | |
| Study design | 0.291 | ||||||
| Cohort study | 6 | 796 | 0.87 (0.73–1.02) | 94.2 | <0.001 | 74.8 | |
| Non-randomized clinical trial | 2 | 50 | 0.71 (0.09–5.87) | 97.6 | <0.001 | 14.8 | |
| Randomized clinical trial | 1 | 36 | 1.10 (0.86–1.42) | NA | NA | 10.4 | |
| Vaccine type | <0.001 | ||||||
| Adenovirus vector vaccines | 2 | 44 | 1.27 (0.93–1.74) | 64.3 | 0.094 | 24.7 | |
| Inactivated virus vaccines | 2 | 256 | 0.44 (0.31–0.63) | 27.6 | 0.240 | 19.3 | |
| mRNA vaccines | 4 | 490 | 0.91 (0.69–1.20) | 95.2 | <0.001 | 56.0 | |
| Time interval between vaccination and antibody testing | 0.753 | ||||||
| <28 days | 4 | 490 | 0.91 (0.69–1.20) | 95.2 | <0.001 | 51.6 | |
| ≥28 days | 5 | 392 | 0.78 (0.31–1.94) | 98.8 | <0.001 | 48.4 | |
| CD4+ T-cell count | 0.421 | ||||||
| <500 cells/μL | 1 | 64 | 0.40 (0.22–0.73) | NA | NA | 25.7 | |
| ≥500 cells/μL | 1 | 150 | 0.53 (0.38–0.76) | NA | NA | 74.3 | |
| The second dose | |||||||
| Overall | 19 | 1890 | 0.97 (0.93–1.00) | 94.2 | <0.001 | 100.0 | |
| Continent | 0.643 | ||||||
| Africa | 1 | 32 | 0.98 (0.87–1.11) | NA | NA | 3.7 | |
| Asia | 7 | 764 | 0.97 (0.93–1.01) | 69.8 | 0.003 | 33.5 | |
| Europe | 6 | 637 | 0.99 (0.97–1.02) | 81.6 | <0.001 | 39.7 | |
| North America | 3 | 198 | 0.95 (0.78–1.16) | 92.9 | <0.001 | 14.4 | |
| South America | 2 | 259 | 0.86 (0.70–1.07) | 80.5 | 0.024 | 8.7 | |
| Study design | 0.342 | ||||||
| Cohort study | 14 | 1659 | 0.96 (0.92–1.00) | 96.1 | <0.001 | 80.2 | |
| Non-randomized clinical trial | 4 | 199 | 1.00 (0.97–1.03) | 17.9 | 0.301 | 16.1 | |
| Randomized clinical trial | 1 | 32 | 0.98 (0.87–1.11) | NA | NA | 3.7 | |
| Vaccine type | 0.013 | ||||||
| Adenovirus vector vaccines | 2 | 86 | 1.02 (0.98–1.06) | 0.0 | 0.444 | 10.8 | |
| Inactivated virus vaccines | 7 | 585 | 0.92 (0.87–0.97) | 47.7 | 0.075 | 25.4 | |
| mRNA vaccines | 9 | 1033 | 0.99 (0.97–1.00) | 72.9 | <0.001 | 63.8 | |
| Time interval between vaccination and antibody testing | 0.689 | ||||||
| ≤14 days | 7 | 598 | 0.98 (0.93–1.04) | 43.8 | <0.001 | 43.8 | |
| 15–28 days | 4 | 480 | 0.96 (0.90–1.02) | 84.9 | <0.001 | 22.8 | |
| >28 days | 6 | 587 | 0.95 (0.91–1.00) | 81.9 | <0.001 | 33.4 | |
| CD4+ T-cell count | 0.178 | ||||||
| <500 cells/μL | 3 | 170 | 0.93 (0.86–1.01) | 69.0 | 0.040 | 48.9 | |
| ≥500 cells/μL | 2 | 219 | 0.98 (0.96–1.01) | 0.0 | 0.501 | 51.1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, L.; Shang, W.; Gao, P.; Wang, Y.; Liu, J.; Liu, M. Immunogenicity and Safety of COVID-19 Vaccines among People Living with HIV: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 1569. https://doi.org/10.3390/vaccines10091569
Kang L, Shang W, Gao P, Wang Y, Liu J, Liu M. Immunogenicity and Safety of COVID-19 Vaccines among People Living with HIV: A Systematic Review and Meta-Analysis. Vaccines. 2022; 10(9):1569. https://doi.org/10.3390/vaccines10091569
Chicago/Turabian StyleKang, Liangyu, Weijing Shang, Peng Gao, Yaping Wang, Jue Liu, and Min Liu. 2022. "Immunogenicity and Safety of COVID-19 Vaccines among People Living with HIV: A Systematic Review and Meta-Analysis" Vaccines 10, no. 9: 1569. https://doi.org/10.3390/vaccines10091569
APA StyleKang, L., Shang, W., Gao, P., Wang, Y., Liu, J., & Liu, M. (2022). Immunogenicity and Safety of COVID-19 Vaccines among People Living with HIV: A Systematic Review and Meta-Analysis. Vaccines, 10(9), 1569. https://doi.org/10.3390/vaccines10091569








