Intent among Parents to Vaccinate Children before Pediatric COVID-19 Vaccine Recommendations, Minnesota and Los Angeles County, California—May–September 2021
Abstract
:1. Introduction
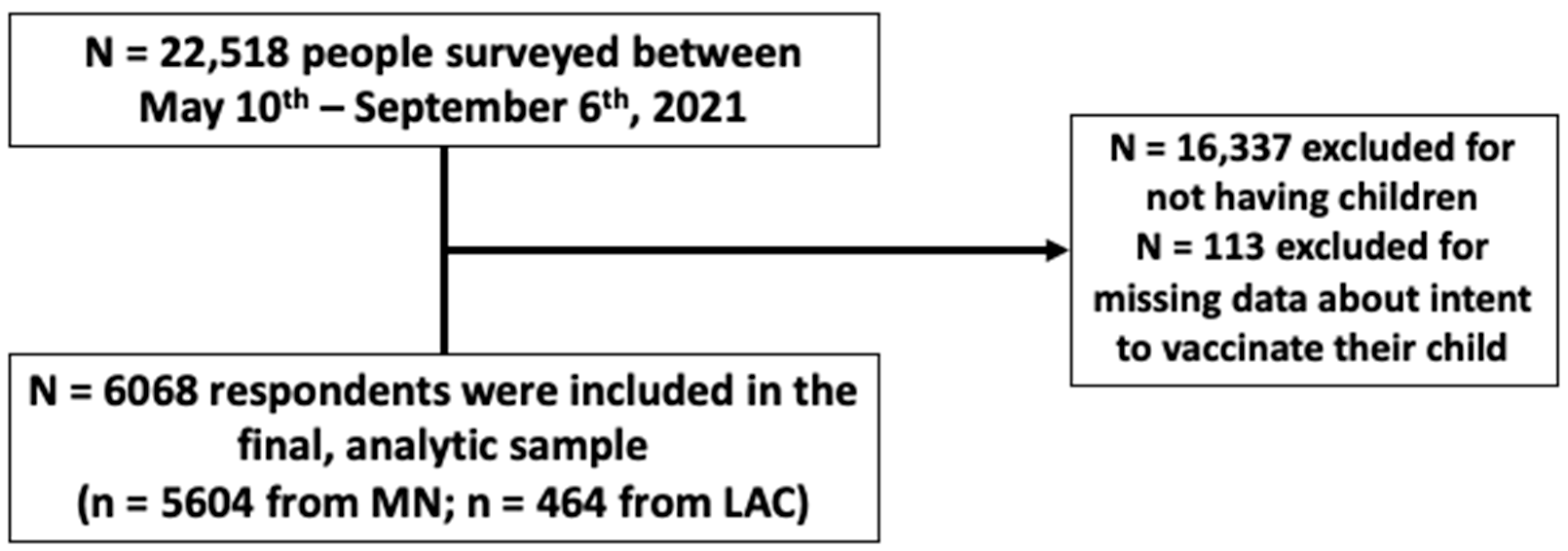
2. Methods
2.1. Data Collection
- 1.
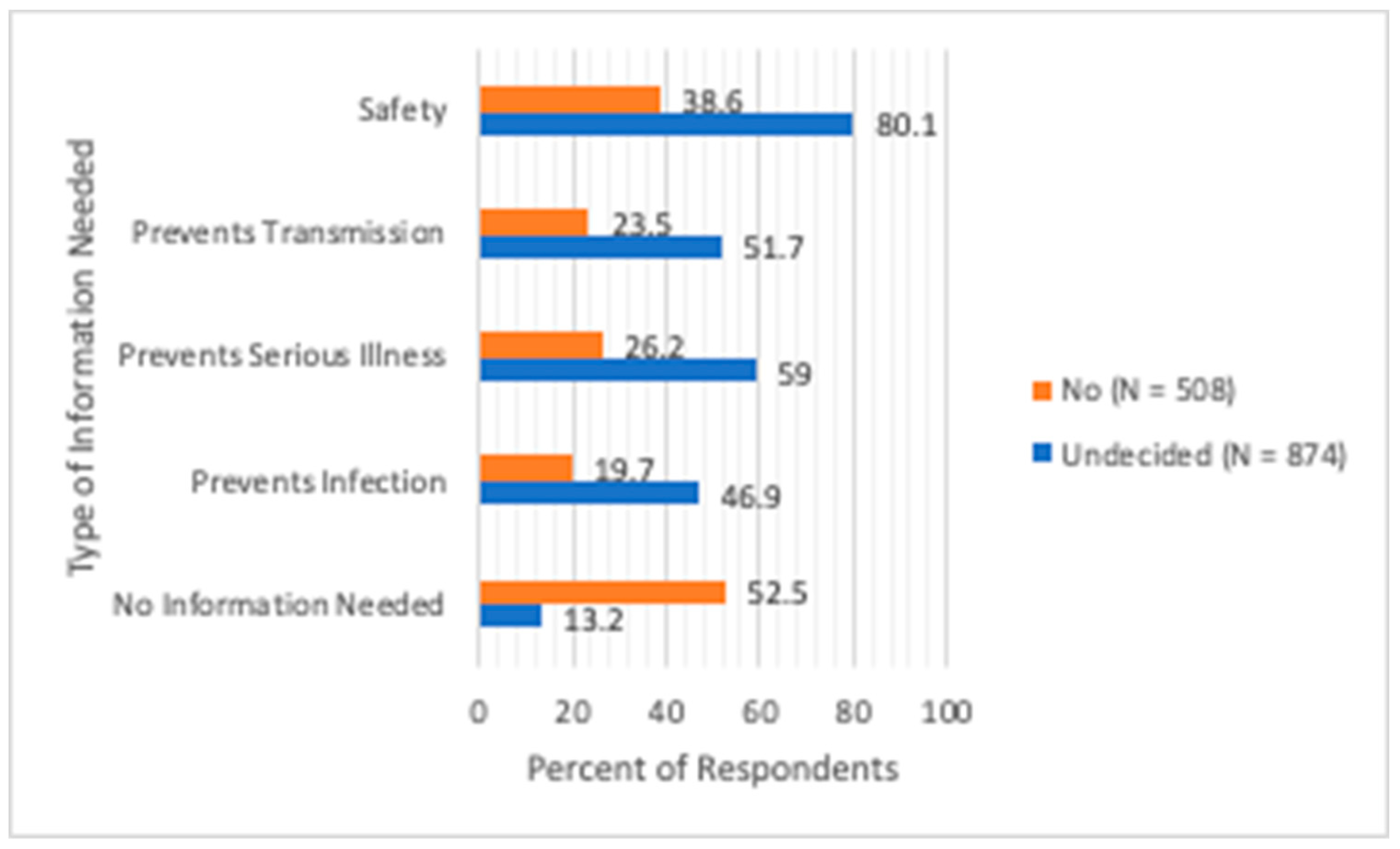
- “What information would influence your decision to have your child get the COVID-19 vaccine?” Possible responses (more than one choice allowed) were:
- Information about whether the vaccine is safe for children;
- Evidence that vaccination prevents children from getting infected with the COVID-19 virus;
- Evidence that the vaccine prevents children from getting serious illness due to COVID-19;
- Evidence that vaccinated children are less likely to transmit the COVID-19 virus to others;
- I have all the information I need about COVID-19 vaccines.
- 2.
- “Over the past month, did your child or children (select all that apply)” Possible choices were:
- Attend in-person classes;
- Attend in-person childcare;
- Participate in a sports team;
- Participate in another in-person extracurricular activity;
- Have indoor visits with friends;
- Attend in-person religious or community activities;
- My child or children did not do any in-person activities.
- 3.
- For children attending school or childcare, parents were asked “Which of the following helped to inform your decision to have your child or children attend in-person classes or childcare?”Possible responses (more than one choice allowed) were:
- The school or childcare facility does not provide an option for virtual learning;
- I have challenges in providing virtual learning for my child or children;
- Low numbers of COVID-19 cases in my community;
- Vaccination of students, teachers, and staff;
- Availability of school-based COVID-19 testing;
- Symptom screening for students and staff;
- Indoor mask requirements for students and staff;
- Maintenance of other COVID-19 prevention measures, including physical distancing; use of physical barriers; and smaller classrooms.
- 4.
- For children NOT attending school or childcare, parents were asked “Which of the following helped to inform your decision to have your child or children NOT attend in-person classes or childcare?”Possible responses (more than one choice allowed) to this multiple-choice question were:
- My child or children would not be attending school or childcare anyway;
- The school or childcare facility does not provide an option for in-person learning;
- Low numbers of COVID-19 cases in my community;
- Vaccination of students, teachers, and staff before the school year begins;
- Availability of school-based COVID-19 testing;
- Symptom screening for students and staff;
- Indoor mask requirements for students and staff;
- Maintenance of other COVID-19 prevention measures, including physical distancing, use of physical barriers, and smaller classrooms;
- None of these.
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Delahoy, M.J.; Ujamaa, D.; Whitaker, M.; O’Halloran, A.; Anglin, O.; Burns, E.; Cummings, C.; Holstein, R.; Kambhampati, A.K.; Milucky, J.; et al. Hospitalizations Associated with COVID-19 Among Children and Adolescents—COVID-NET, 14 States, March 1, 2020–August 14, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1255–1260. [Google Scholar] [CrossRef] [PubMed]
- Siegel, D.A.; Reses, H.E.; Cool, A.J.; Shapiro, C.N.; Hsu, J.; Boehmer, T.K.; Cornwell, C.R.; Gray, E.B.; Henley, S.J.; Lochner, K.; et al. Trends in COVID-19 Cases, Emergency Department Visits, and Hospital Admissions Among Children and Adolescents Aged 0–17 Years—United States, August 2020–August 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1249–1254. [Google Scholar] [CrossRef] [PubMed]
- Honein, M.A.; Barrios, L.C.; Brooks, J.T. Data and Policy to Guide Opening Schools Safely to Limit the Spread of SARS-CoV-2 Infection. JAMA 2021, 325, 823–824. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.M.; Newhams, M.M.; Halasa, N.B.; Price, A.M.; Boom, J.A.; Sahni, L.C.; Pannaraj, P.S.; Irby, K.; Walker, T.C.; Schwartz, S.P.; et al. Effectiveness of BNT162b2 Vaccine against Critical Covid-19 in Adolescents. N. Engl. J. Med. 2022, 386, 713–723. [Google Scholar] [CrossRef]
- Wallace, M.; Woodworth, K.R.; Gargano, J.W.; Scobie, H.M.; Blain, A.E.; Moulia, D.; Chamberland, M.; Reisman, N.; Hadler, S.C.; MacNeil, J.R.; et al. The Advisory Committee on Immunization Practices’ Interim Recommendation for Use of Pfizer-BioNTech COVID-19 Vaccine in Adolescents Aged 12–15 Years—United States, May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 749–752. [Google Scholar] [CrossRef]
- CDC. COVID Data Tracker. Centers for Disease Control and Prevention. 2020. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 24 April 2022).
- Scherer, A.M.; Gedlinske, A.M.; Parker, A.M.; Gidengil, C.A.; Askelson, N.M.; Petersen, C.A.; Woodworth, K.R.; Lindley, M.C. Acceptability of Adolescent COVID-19 Vaccination Among Adolescents and Parents of Adolescents—United States, April 15–23, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 997–1003. [Google Scholar] [CrossRef]
- National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. Science Brief: Transmission of SARS-CoV-2 in K-12 Schools and Early Care and Education Programs—Updated. In CDC COVID-19 Science Briefs; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2020. Available online: http://www.ncbi.nlm.nih.gov/books/NBK570438/ (accessed on 24 April 2022).
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental health impacts of the COVID-19 pandemic on children and youth—A systematic review. Child Adolesc. Ment. Health 2022, 27, 173–189. [Google Scholar] [CrossRef]
- Matthias, J.; Patrick, S.; Wiringa, A.; Pullman, A.; Hinton, S.; Campos, J.; Belville, T.; Sinner, M.M.; Buchanan, T.T.; Sim, B.; et al. Epidemiologically Linked COVID-19 Outbreaks at a Youth Camp and Men’s Conference—Illinois, June–July 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1223–1227. [Google Scholar] [CrossRef]
- Atherstone, C.; Siegel, M.; Schmitt-Matzen, E.; Sjoblom, S.; Jackson, J.; Blackmore, C.; Neatherlin, J. SARS-CoV-2 Transmission Associated with High School Wrestling Tournaments—Florida, December 2020–January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 141–143. [Google Scholar] [CrossRef]
- Yin, S.; Barnes, K.; Fisher, R.; Terashita, D.; Kim, A.A. COVID-19 Case Rates in Transitional Kindergarten through Grade 12 Schools and in the Community—Los Angeles County, California, September 2020–March 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1220–1222. [Google Scholar] [CrossRef]
- Szablewski, C.M.; Chang, K.T.; Brown, M.M.; Chu, V.T.; Yousaf, A.R.; Anyalechi, N.; Aryee, P.A.; Kirking, H.L.; Lumsden, M.; Mayweather, E.; et al. SARS-CoV-2 Transmission and Infection Among Attendees of an Overnight Camp—Georgia, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1023–1025. [Google Scholar] [CrossRef] [PubMed]
- Parks, S.E.; Zviedrite, N.; Budzyn, S.E.; Panaggio, M.J.; Raible, E.; Papazian, M.; Magid, J.; Ahmed, F.; Uzicanin, A.; Barrios, L.C. COVID-19-Related School Closures and Learning Modality Changes—United States, August 1–September 17, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1374–1376. [Google Scholar] [CrossRef] [PubMed]
- STROBE_checklist_v4_combined.pdf. Available online: https://www.equator-network.org/wp-content/uploads/2015/10/STROBE_checklist_v4_combined.pdf (accessed on 24 April 2022).
- Bourque, S.L.; Weikel, B.W.; Palmer, C.; Blackwell, S.; Cataldi, J.R.; Hwang, S.S. Prevalence and Predictors of Pediatric COVID-19 Vaccine Acceptance. Am. J. Perinatol. 2022, 1850–3199. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.B.; Gray, A.; Sheck, I. COVID-19 Pediatric Vaccine Hesitancy among Racially Diverse Parents in the United States. Vaccines 2021, 10, 31. [Google Scholar] [CrossRef] [PubMed]
- Gray, A.; Fisher, C.B. Determinants of COVID-19 Vaccine Uptake in Adolescents 12–17 Years Old: Examining Pediatric Vaccine Hesitancy Among Racially Diverse Parents in the United States. Front. Public Health 2022, 10, 844310. [Google Scholar] [CrossRef]
- Chen, F.; He, Y.; Shi, Y. Parents’ and Guardians’ Willingness to Vaccinate Their Children against COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 179. [Google Scholar] [CrossRef]
- Letterie, M.C.; Patrick, S.W.; Halvorson, A.E.; Dupont, W.D.; Carroll, K.N.; Zickafoose, J.S.; Williams, S.E. Factors Associated with Parental COVID-19 Vaccination Acceptance. Clin. Pediatr. 2022, 61, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Baumann, B.M.; Rodriguez, R.M.; DeLaroche, A.M.; Rayburn, D.; Eucker, S.A.; Nadeau, N.L.; Drago, L.A.; Cullen, D.; Meskill, S.D.; Bialeck, S.; et al. Factors Associated with Parental Acceptance of COVID-19 Vaccination: A Multicenter Pediatric Emergency Department Cross-Sectional Analysis. Ann. Emerg. Med. 2022, 80, 130–142. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 vaccine literacy: A preliminary online survey. Hum. Vaccin Immunother. 2021, 17, 1304–1312. [Google Scholar] [CrossRef]
- Usman, S.; Bologna, L.; Stamidis, K.V. The CORE Group Partners Project in North East Nigeria: Community Engagement Strategies to Combat Skepticism and Build Trust for Vaccine Acceptance. Am. J. Trop. Med. Hyg. 2019, 101 (Suppl. S4), 68–73. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.; Pink, S.; Willer, R. Religious Identity Cues Increase Vaccination Intentions and Trust in Medical Experts among American Christians. Proc. Natl. Acad. Sci. USA 2021, 118, e2106481118. [Google Scholar] [CrossRef] [PubMed]
- Hast, M.; Swanson, M.; Scott, C.; Oraka, E.; Espinosa, C.; Burnett, E.; Kukielka, E.A.; Rice, M.E.; Mehari, L.; McCloud, J.; et al. Prevalence of risk behaviors and correlates of SARS-CoV-2 positivity among in-school contacts of confirmed cases in a Georgia school district in the pre-vaccine era, December 2020–January 2021. BMC Public Health 2022, 22, 101. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, P.G.; Shah, M.D.; Delgado, J.R.; Thomas, K.; Vizueta, N.; Cui, Y.; Vangala, S.; Shetgiri, R.; Kapteyn, A. Parents’ Intentions and Perceptions about COVID-19 Vaccination for Their Children: Results from a National Survey. Pediatrics 2021, 148, e2021052335. [Google Scholar] [CrossRef]
- Moore, J.E.; Millar, B.C. Improving COVID-19 vaccine-related health literacy and vaccine uptake in patients: Comparison on the readability of patient information leaflets of approved COVID-19 vaccines. J. Clin. Pharm. Ther. 2021, 46, 1498–1500. [Google Scholar] [CrossRef]
- Olson, O.; Berry, C.; Kumar, N. Addressing Parental Vaccine Hesitancy towards Childhood Vaccines in the United States: A Systematic Literature Review of Communication Interventions and Strategies. Vaccines 2020, 8, 590. [Google Scholar] [CrossRef]
- Nyathi, S.; Karpel, H.C.; Sainani, K.L.; Maldonado, Y.; Hotez, P.J.; Bendavid, E.; Lo, N.C. The 2016 California policy to eliminate nonmedical vaccine exemptions and changes in vaccine coverage: An empirical policy analysis. PLoS Med. 2019, 16, e1002994. [Google Scholar] [CrossRef]
- Mello, M.M.; Studdert, D.M.; Parmet, W.E. Shifting Vaccination Politics—The End of Personal-Belief Exemptions in California. N. Engl. J. Med. 2015, 373, 785–787. [Google Scholar] [CrossRef]
- Bill Text—SB-277 Public Health: Vaccinations. Available online: https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201520160SB277 (accessed on 24 April 2022).
- Newsom Issues Nation’s First COVID Vaccine Mandate for All Schoolchildren. Available online: https://www.cbsnews.com/losangeles/news/covid-vaccine-mandate-california-students/ (accessed on 24 April 2022).
- 1/3 of Parents in 3 States May Not Send Children to School Because of COVID-19. University of Michigan. Available online: https://labblog.uofmhealth.org/rounds/13-of-parents-3-states-may-not-send-children-to-school-because-of-covid-19 (accessed on 16 May 2022).
- Anna, S.; Rapaport, A.; Dan, S. Why Some Parents Are Sticking with Remote Learning—Even as Schools Reopen. Brookings. 2021. Available online: https://www.brookings.edu/blog/brown-center-chalkboard/2021/06/08/why-some-parents-are-sticking-with-remote-learning-even-as-schools-reopen/ (accessed on 16 May 2022).
- Klosky, J.V.; Gazmararian, J.A.; Casimir, O.; Blake, S.C. Effects of Remote Education During the COVID-19 Pandemic on Young Children’s Learning and Academic Behavior in Georgia: Perceptions of Parents and School Administrators. J. Sch. Health 2022, 92, 656–664. [Google Scholar] [CrossRef]
- Verlenden, J.V.; Pampati, S.; Rasberry, C.N.; Liddon, N.; Hertz, M.; Kilmer, G.; Viox, M.H.; Lee, S.; Cramer, N.K.; Barrios, L.C.; et al. Association of Children’s Mode of School Instruction with Child and Parent Experiences and Well-Being During the COVID-19 Pandemic—COVID Experiences Survey, United States, October 8–November 13, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 369–376. [Google Scholar] [CrossRef]
- CDC. 6 Ways Schools Can Promote COVID-19 Vaccines. Centers for Disease Control and Prevention. 22 June 2022. Available online: https://www.cdc.gov/vaccines/covid-19/planning/school-located-clinics/how-schools-can-support.html (accessed on 25 August 2022).
- Godoy, M. Meet Maryland’s Secret Weapon in the Battle to Close the Latino Vaccination Gap. NPR. 7 July 2021. Available online: https://www.npr.org/sections/health-shots/2021/07/07/1012502246/meet-marylands-secret-weapon-in-the-battle-to-close-the-latino-vaccination-gap (accessed on 25 August 2022).
- Bixler, D. SARS-CoV-2–Associated Deaths Among Persons Aged 21 Years—United States, February 12–July 31, 2020. MMWR Morb Mortal Wkly Rep. 2020, 69. [Google Scholar] [CrossRef]
| Respondent Characteristics | Respondents with Children <12 Years (N = 6068) | Responses to Survey Question Regarding Intention to Vaccinate Children Aged <12 Years | |||
|---|---|---|---|---|---|
| Intending to Vaccinate Children (N = 4686) | Undecided to Vaccinate Children (N = 874) | Not Intending to Vaccinate Children (N = 508) | p-Value | ||
| Study area—n (%) | <0.001 | ||||
| Los Angeles County, California | 464 (7.6) | 300 (64.7) | 108 (23.3) | 56 (12.1) | |
| State of Minnesota | 5604 (92.4) | 4386 (78.3) | 766 (13.7) | 452 (8.1) | |
| Combined MN and LA | 6068 (100) | 4686 (77.2) | 874 (14.4) | 508 (8.4) | |
| Age in years, median—years (min, max) | 40 (18, 66) | 40 (18, 65) | 37 (18, 65) | 37 (18, 66) | <0.001 |
| Age group in years—n (%) | <0.01 | ||||
| 18–29 | 399 (6.6) | 128 (4.6) | 62 (11.8) | 53 (17.3) | |
| 30–44 | 4192 (69.1) | 1842 (65.6) | 369 (70.0) | 192 (62.5) | |
| 45–59 | 1392 (22.9) | 804 (28.6) | 82 (15.6) | 58 (18.9) | |
| ≥60 | 85 (1.4) | 36 (1.3) | 14 (2.7) | 4 (1.3) | |
| Gender—n (%) | 0.007 | ||||
| Male | 1605 (26.5) | 1283 (27.4) | 217 (24.8) | 105 (20.7) | |
| Female | 4420 (72.8) | 3367 (71.9) | 654 (74.8) | 399 (78.5) | |
| Transgender/Other | 43 (0.7) | 36 (0.8) | 3 (0.3) | 4 (0.8) | |
| Combined Race and Ethnicity—n (%) | <0.001 | ||||
| Asian, non-Hispanic | 228 (3.8) | 179 (3.8) | 40 (4.6) | 9 (1.8) | |
| Black, non-Hispanic | 125 (2.1) | 70 (1.5) | 36 (4.1) | 19 (3.7) | |
| Hispanic or Latino, any race or races | 423 (7.0) | 274 (5.8) | 92 (10.5) | 57 (10.5) | |
| Multiple races, non-Hispanic | 147 (2.4) | 109 (2.3) | 23 (2.6) | 15 (3.0) | |
| Other race, non-Hispanic | 84 (1.4) | 49 (1.0) | 13 (1.5) | 22 (4.3) | |
| White, non-Hispanic | 5061 (83.4) | 4005 (79.1) | 670 (76.7) | 386 (76.0) | |
| Household Income—n (%) | <0.001 | ||||
| Less than $25,000 | 215 (3.5) | 105 (2.2) | 71 (8.1) | 39 (7.7) | |
| $25,000–$49,000 | 505 (8.3) | 297 (6.3) | 124 (14.2) | 84 (16.5) | |
| $50,000–$99,999 | 1445 (23.8) | 1046 (22.3) | 236 (27.0) | 163 (32.1) | |
| $100,000 or more | 3576 (58.9) | 3024 (64.5) | 375 (42.9) | 177 (34.8) | |
| Unknown | 327 (5.4) | 214 (4.6) | 68 (7.8) | 45 (8.9) | |
| Education—n (%) | <0.01 | ||||
| High school degree or less | 221 (3.6) | 106 (2.3) | 70 (8.0) | 45 (8.9) | |
| Some college or bachelor’s degree | 3261 (53.7) | 2309 (49.3) | 581 (66.5) | 371 (73.0) | |
| Professional or doctoral degree | 2586 (42.6) | 2271 (48.5) | 223 (25.5) | 92 (18.1) | |
| Currently employed—n (%) | 0.004 | ||||
| Yes | 5213 (85.9) | 4062 (86.7) | 733 (83.9) | 418 (82.3) | |
| No | 855 (14.1) | 624 (13.3) | 141 (16.1) | 90 (17.7) | |
| Received one or more COVID-19 vaccines—n (%) | <0.001 | ||||
| Yes | 5555 (91.5) | 4635 (98.9) | 734 (84.0) | 186 (36.6) | |
| No | 513 (8.5) | 51 (1.1) | 140 (16.0) | 322 (63.4) | |
| Number of household members—mean (min, max) | 4 (2, 16) | 4 (2, 16) | 4 (2, 16) | 503 (2, 14) | <0.001 |
| Number of children aged <12 years—median (min, max) | 2 (1, 8) | 2 (1, 8) | 2 (1, 8) | 2 (1, 7) | <0.01 |
| Child Activities | Intention to Vaccinate Children (N = 4686) n (%) | Undecided to Vaccinate Children (N = 874) n (%) | aOR (95% CI) * | No Intention to Vaccinate Children (N = 508) n (%) | aOR (95% CI) * |
|---|---|---|---|---|---|
| Attended in-person classes | 1453 (31.0) | 266 (30.4) | 1.04 (0.88, 1.23) | 163 (32.1) | 1.16 (0.90, 1.50) |
| Attended in-person childcare | 1669 (35.6) | 319 (36.5) | 1.17 (0.99, 1.38) | 154 (30.3) | 1.03 (0.80, 1.34) |
| Participated in sports | 1819 (38.8) | 277 (31.7) | 1.01 (0.86, 1.19) | 190 (37.4) | 1.51 (1.17, 1.95) |
| Other in-person extracurricular activities | 1932 (31.8) | 286 (32.7) | 0.92 (0.79, 1.09) | 195 (38.4) | 1.35 (1.05, 1.73) |
| Indoor visits with friends | 2629 (56.1) | 471 (53.9) | 1.19 (1.02, 1.39) | 336 (66.1) | 2.31 (1.78, 2.99) |
| In-person faith or community activities | 670 (14.3) | 194 (22.2) | 1.90 (1.58, 2.29) | 206 (40.6) | 4.71 (3.62, 6.11) |
| No in-person activities | 464 (9.9) | 126 (14.4) | 0.92 (0.72, 1.17) | 56 (11.0) | 0.55 (0.37, 0.81) |
| Intending to Vaccinate (N = 2686) | Undecided (N = 490) | No Intention to Vaccinate (N = 265) | Overall (N = 3441) | |
|---|---|---|---|---|
| No Virtual Learning Option | 16.7 | 16.9 | 15.1 | 16.6 |
| Parental Challenges to Provide Virtual Learning | 19.2 | 16.9 | 11.7 a,c | 18.3 |
| Low Local COVID Levels | 28.5 | 22.2 a | 18.1 b | 26.8 |
| Vaccinated Teachers/Staff/Students | 63.6 | 43.5 b | 13.6 b,d | 56.9 |
| Available Onsite COVID Testing | 8.2 | 5.9 | 3.4 a | 7.5 |
| Onsite Symptoms Screening | 40.9 | 30.0 b | 17.7 b,d | 37.6 |
| Indoor Masking Requirements for Staff/Students | 59.6 | 36.1 b | 19.6 b,d | 53.2 |
| Other Prevention Measures * | 50.0 | 34.7 b | 18.9 b,d | 45.4 |
| None of the above | 23.3 | 46.4 b | 9.6 b,d | 14.4 |
| Intending to Vaccinate (N = 2000) | Undecided (N = 384) | No Intention to Vaccinate d (N = 243) | Overall (N = 2627) | |
|---|---|---|---|---|
| Indoor Masking Requirements for Staff/Students | 13.3 | 6.5 c | 6.6 c | 11.7 |
| Onsite Symptoms Screening | 7.7 | 3.9 c | 3.3 c | 6.7 |
| Available Onsite COVID Testing | 4.8 | 3.1 a | 1.6 b | 4.3 |
| Vaccinated Teachers/Staff/Students | 11.1 | 4.7 c | 2.5 c | 9.4 |
| Low Local COVID Levels | 4.8 | 3.9 | 2.1 | 4.4 |
| No In-Person Learning | 2.5 | 3.1 | 2.1 | 2.6 |
| Additional Prevention Measures * | 15.5 | 8.9 c | 8.6 c | 13.9 |
| Factors Other Than Above | 36.2 | 52.1 c | 52.7 c | 40.0 |
| Would Not attend School/Childcare Anyway | 43.5 | 32.8 c | 34.2 b | 41.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suvada, K.A.; Quan, S.F.; Weaver, M.D.; Sreedhara, M.; Czeisler, M.É.; Como-Sabetti, K.; Lynfield, R.; Grounder, P.; Traub, E.; Amoon, A.; et al. Intent among Parents to Vaccinate Children before Pediatric COVID-19 Vaccine Recommendations, Minnesota and Los Angeles County, California—May–September 2021. Vaccines 2022, 10, 1441. https://doi.org/10.3390/vaccines10091441
Suvada KA, Quan SF, Weaver MD, Sreedhara M, Czeisler MÉ, Como-Sabetti K, Lynfield R, Grounder P, Traub E, Amoon A, et al. Intent among Parents to Vaccinate Children before Pediatric COVID-19 Vaccine Recommendations, Minnesota and Los Angeles County, California—May–September 2021. Vaccines. 2022; 10(9):1441. https://doi.org/10.3390/vaccines10091441
Chicago/Turabian StyleSuvada, Kara A., Stuart F. Quan, Matthew D. Weaver, Meera Sreedhara, Mark É. Czeisler, Kathy Como-Sabetti, Ruth Lynfield, Prabhu Grounder, Elizabeth Traub, Aryana Amoon, and et al. 2022. "Intent among Parents to Vaccinate Children before Pediatric COVID-19 Vaccine Recommendations, Minnesota and Los Angeles County, California—May–September 2021" Vaccines 10, no. 9: 1441. https://doi.org/10.3390/vaccines10091441
APA StyleSuvada, K. A., Quan, S. F., Weaver, M. D., Sreedhara, M., Czeisler, M. É., Como-Sabetti, K., Lynfield, R., Grounder, P., Traub, E., Amoon, A., Ladva, C. N., Howard, M. E., Czeisler, C. A., Rajaratnam, S. M. W., Ekwueme, D. U., Flannery, B., & Lane, R. I. (2022). Intent among Parents to Vaccinate Children before Pediatric COVID-19 Vaccine Recommendations, Minnesota and Los Angeles County, California—May–September 2021. Vaccines, 10(9), 1441. https://doi.org/10.3390/vaccines10091441








