Quantitative RT-PCR Assays for Quantification of Undesirable Mutants in the Novel Type 2 Oral Poliovirus Vaccine
Abstract
1. Introduction
2. Materials and Methods
2.1. Plasmids and Viruses
2.2. Recovery of nOPV2-c1 Mutant Variants
2.3. Primers and TaqMan Oligo Probes Used for nOPV2-c1 Mutant Variant Detection and Quantification
2.4. qmosRT-PCR Amplification
2.5. Quantitative RT-PCR for Virus Genome Copy Number Determination
2.6. Deep Sequencing Analysis
3. Results
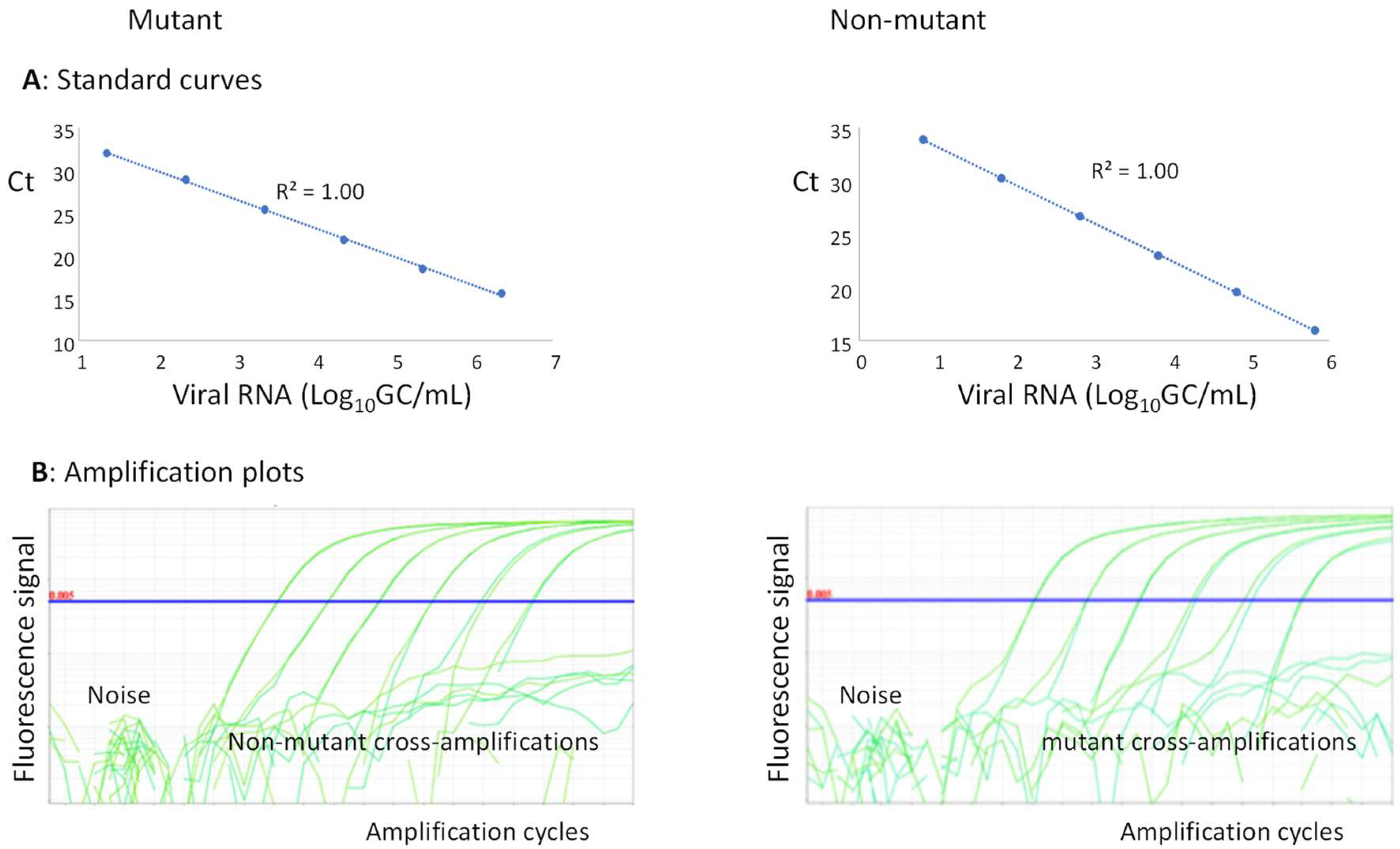
3.1. Assay Design
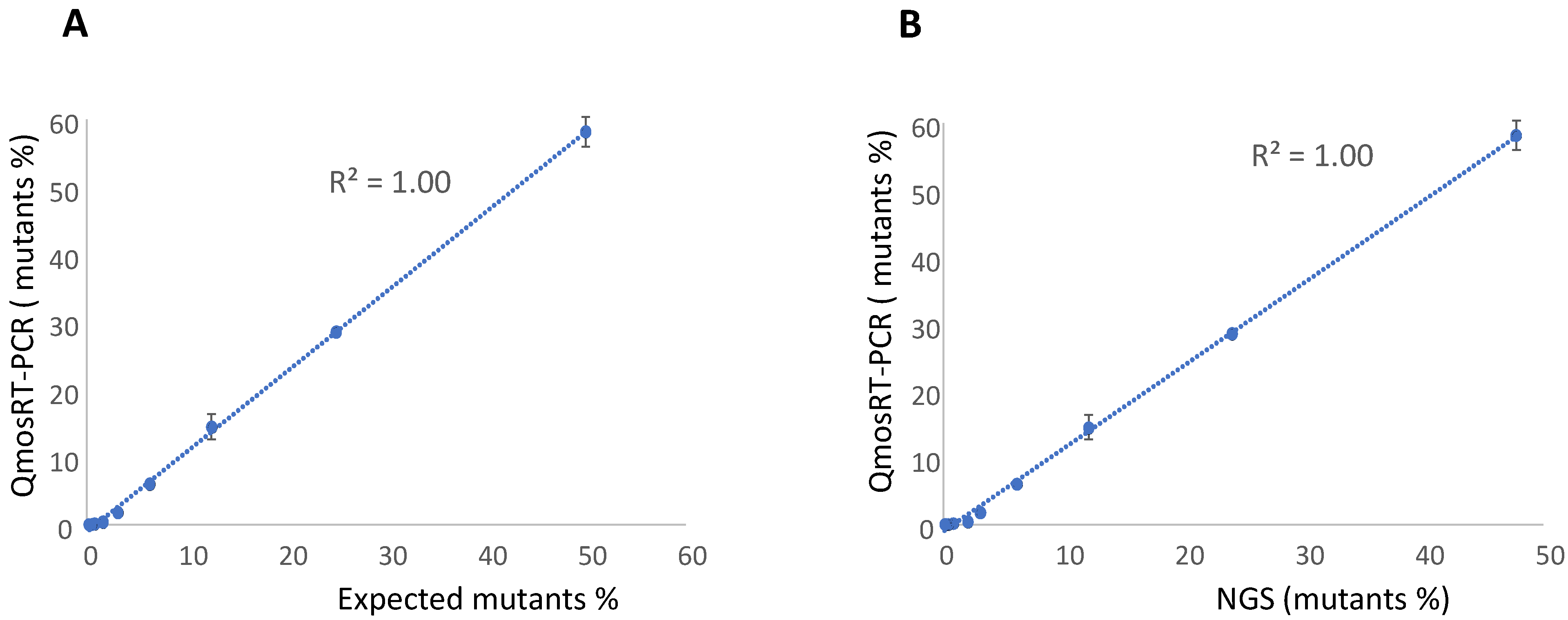
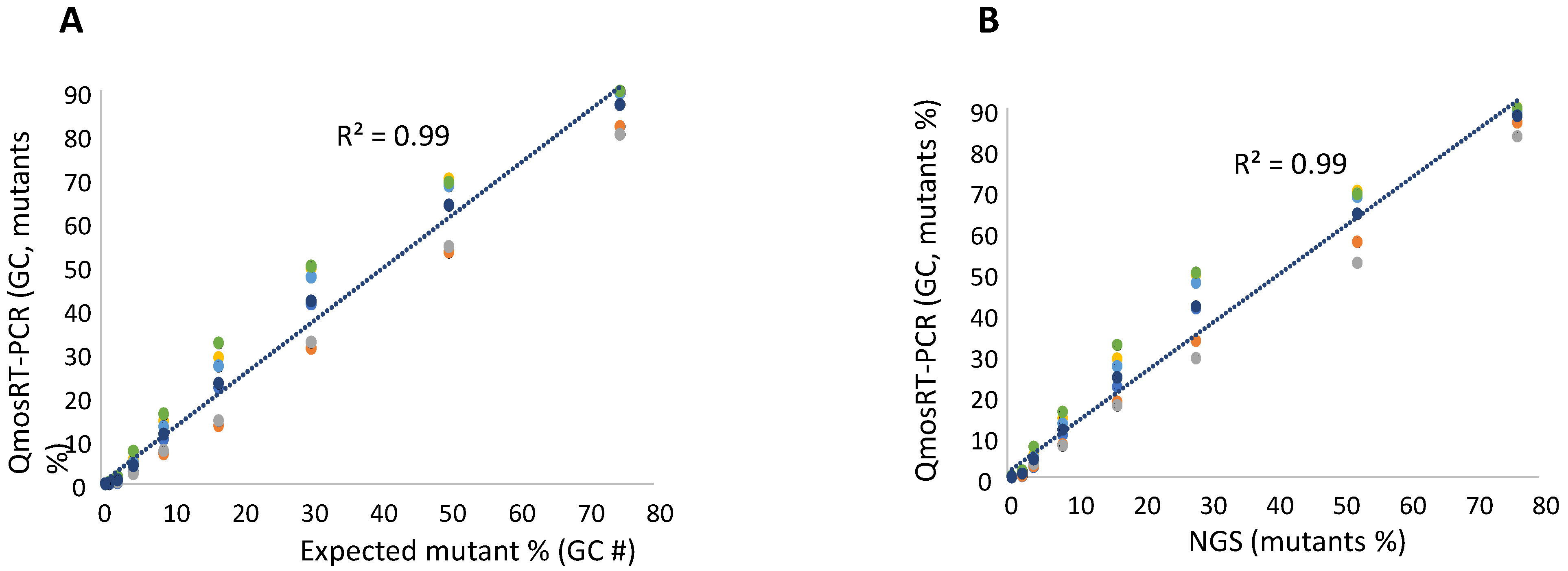
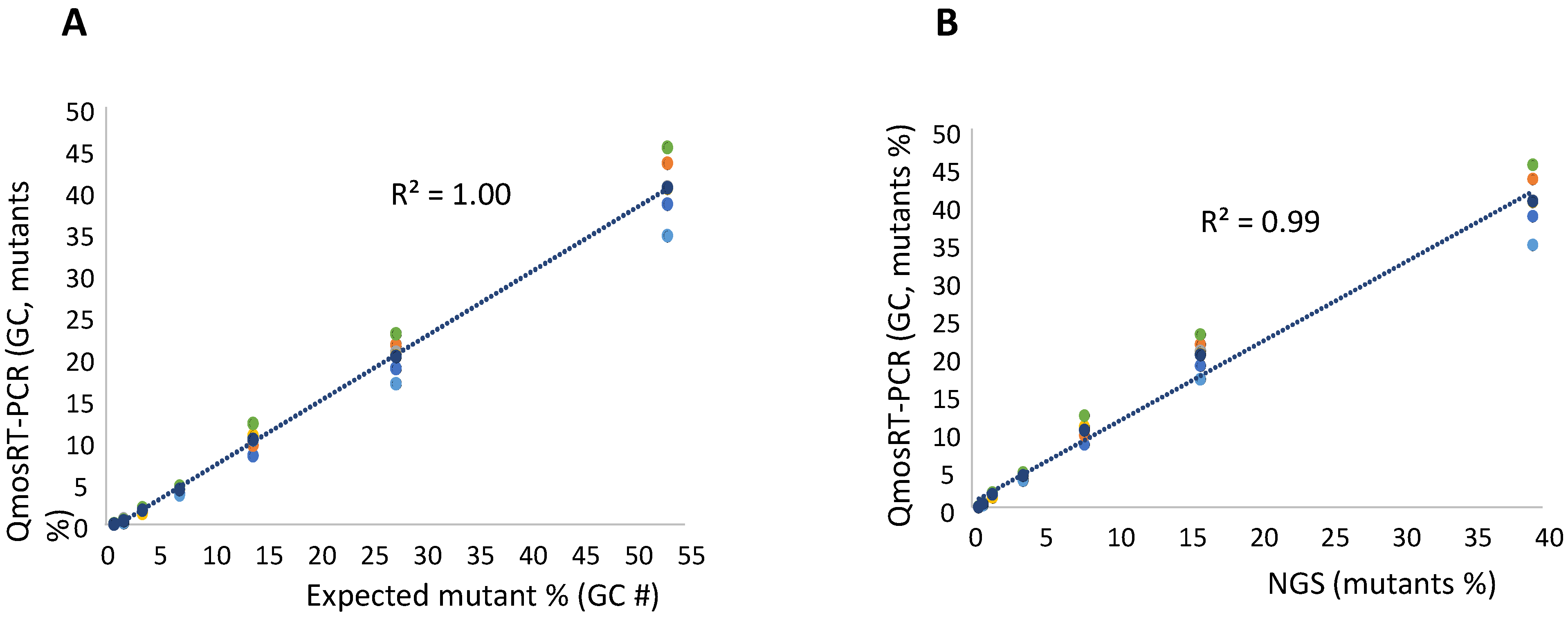
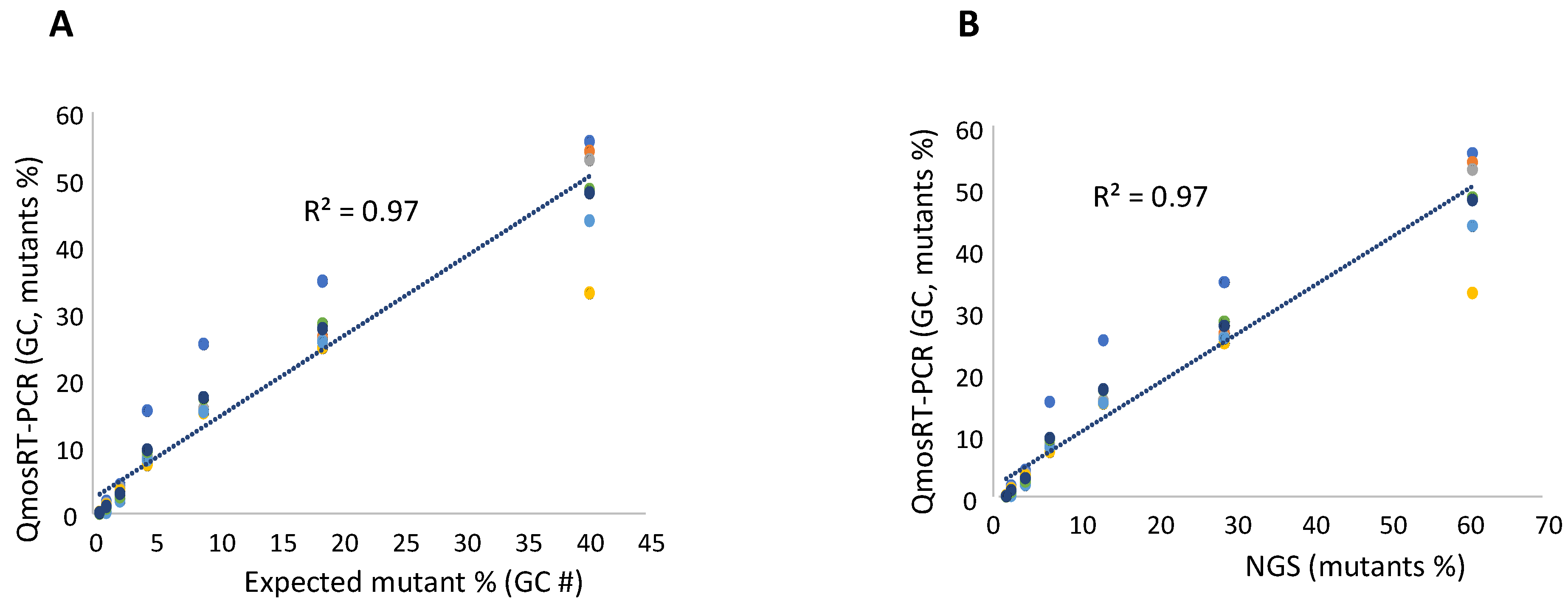
3.2. Evaluation of the Sensitivity and Linearity and Comparison between Mutant Variant Quantifications Using qmosRT-PCR and NGS
3.3. Evaluation of the Level of Mutant Variants in nOPV2 Vaccine Lots
| nOPV2 Lots | nOPV2_295 Mutants, % ± SD | nOPV2_143 Mutants, % ± SD | nOPV2_171 Mutants, % ± SD | ||||||
|---|---|---|---|---|---|---|---|---|---|
| NGS | qmosRT-PCR | R2 | NGS | qmosRT-PCR | R2 | NGS | qmosRT-PCR | R2 | |
| nPOL2056C-c2 | 14.82 ± 0.89 | 27.49 ± 0.35 | 0.97 | ND | ND | 0.85 | ND | ND | 0.99 |
| nPOL2018C | 14.61 ± 0.52 | 23.98 ± 0.17 | 1.67 ± 0.08 | 1.44 ± 0.68 | 9.31 ± 0.27 | 7.71 ± 0.05 | |||
| nPOL2038C-c2 | 2.07 ± 0.13 | 0.08 ± 0.03 | ND | ND | ND | 0.02 ± 0.00 | |||
| nPOL2016C | 45.83 ± 1.17 | 62.49 ± 2.16 | 0.21 ± 0.08 | ND | 0.9 ± 0.08 | 0.14 ± 0.08 | |||
| nPOL2B0419 | 32.71 ± 0.40 | 55.44 ± 1.02 | 1.19 ± 0.04 | 0.34 ± 0.16 | 24.18 ± 0.30 | 25.72 ± 0.72 | |||
| nPOL2B0519 | 37.92 ± 0.60 | 60.36 ± 1.24 | 1.11 ± 0.10 | 0.50 ± 0.24 | 28.83 ± 0.65 | 29.17 ± 3.48 | |||
| nPOL2-119C | 4.97 ± 0.24 | 4.21 ± 0.69 | 0.99 ± 0.14 | 0.42 ± 0.37 | 3.7 ± 0.31 | 1.49 ± 0.36 | |||
| nPOL2-219C | 7.37 ± 0.48 | 7.86 ± 0.77 | 1.93 ± 0.29 | 1.60 ± 0.30 | 5.26 ± 0.34 | 2.30 ± 0.79 | |||
| nPOL2-319C | 7.35 ± 0.40 | 7.89 ± 0.57 | 1.63 ± 0.15 | 1.14 ± 0.52 | 5.23 ± 0.47 | 2.25 ± 0.65 | |||
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sutter, R.W.; Kew, O.M.; Cochi, S.L.; Aylward, R.B. Poliovirus vaccine—Live. In Vaccines, 6th ed.; Plotkin, S.A., Orenstein, W.A., Offit, P.A., Eds.; Elsevier: Amsterdam, The Netherlands, 1993; pp. 598–645. [Google Scholar]
- John, J.; Giri, S.; Karthikeyan, A.S.; Iturriza-Gomara, M.; Muliyil, J.; Abraham, A.; Grassly, N.C.; Kang, G. Effect of a single inactivated poliovirus vaccine dose on intestinal immunity against poliovirus in children previously given oral vaccine: An open-label, randomised controlled trial. Lancet 2014, 384, 1505–1512. [Google Scholar] [CrossRef]
- Rubin, J.; Ottosen, A.; Ghazieh, A.; Fournier-Caruana, J.; Ntow, A.K.; Gonzalez, A.R. Managing the Planned Cessation of a Global Supply Market: Lessons Learned from the Global Cessation of the Trivalent Oral Poliovirus Vaccine Market. J. Infect. Dis. 2017, 216 (Suppl. 1), S40–S45. [Google Scholar] [CrossRef][Green Version]
- Brickley, E.B.; Strauch, C.B.; Wieland-Alter, W.F.; Connor, R.I.; Lin, S.; Weiner, J.A.; Ackerman, M.E.; Arita, M.; Oberste, M.S.; Weldon, W.C.; et al. Intestinal Immune Responses to Type 2 Oral Polio Vaccine (OPV) Challenge in Infants Previously Immunized with Bivalent OPV and Either High-Dose or Standard Inactivated Polio Vaccine. J. Infect. Dis. 2018, 217, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.M.; Duintjer Tebbens, R.J. Lessons from the Polio Endgame: Overcoming the Failure to Vaccinate and the Role of Subpopulations in Maintaining Transmission. J. Infect. Dis. 2017, 216 (Suppl. 1), S176–S182. [Google Scholar] [CrossRef] [PubMed]
- Wright, P.F.; Connor, R.I.; Wieland-Alter, W.F.; Hoen, A.G.; Boesch, A.W.; Ackerman, M.E.; Oberste, M.S.; Gast, C.; Brickley, E.B.; Asturias, E.J.; et al. Vaccine-induced mucosal immunity to poliovirus: Analysis of cohorts from an open-label, randomised controlled trial in Latin American infants. Lancet Infect. Dis. 2016, 16, 1377–1384. [Google Scholar] [CrossRef]
- Wang, H. Why Have cVDPV2 Outbreaks Increased Globally after the Polio Immunization Strategy Switch: Challenges for the Polio Eradication Endgame. China CDC Wkly. 2020, 2, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Blake, I.M.; Pons-Salort, M.; Molodecky, N.A.; Diop, O.M.; Chenoweth, P.; Bandyopadhyay, A.S.; Zaffran, M.; Sutter, R.W.; Grassly, N.C. Type 2 Poliovirus Detection after Global withdrawal of Trivalent Oral Vaccine. N. Engl. J. Med. 2018, 379, 834–845. [Google Scholar] [CrossRef] [PubMed]
- Jorba, J.; Diop, O.M.; Iber, J.; Henderson, E.; Zhao, K.; Quddus, A.; Sutter, R.; Vertefeuille, J.F.; Wenger, J.; Wassilak, S.G.F.; et al. Update on Vaccine-Derived Poliovirus Outbreaks—Worldwide, January 2018–June 2019. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 1024–1028. [Google Scholar] [CrossRef]
- Evans, D.M.; Dunn, G.; Minor, P.D.; Schild, G.C.; Cann, A.J.; Stanway, G.; Almond, J.W.; Currey, K.; Maizel, J.V., Jr. Increased neurovirulence associated with a single nucleotide change in a noncoding region of the Sabin type 3 poliovaccine genome. Nature 1985, 314, 548–550. [Google Scholar] [CrossRef]
- Macadam, A.J.; Ferguson, G.; Burlison, J.; Stone, D.; Skuce, R.; Almond, J.W.; Minor, P.D. Correlation of RNA secondary structure and attenuation of Sabin vaccine strains of poliovirus in tissue culture. Virology 1992, 189, 415–422. [Google Scholar] [CrossRef]
- Macadam, A.J.; Stone, D.M.; Almond, J.W.; Minor, P.D. The 5′ noncoding region and virulence of poliovirus vaccine strains. Trends Microbiol. 1994, 2, 449–454. [Google Scholar] [CrossRef]
- Stern, A.; Yeh, M.T.; Zinger, T.; Smith, M.; Wright, C.; Ling, G.; Nielsen, R.; Macadam, A.; Andino, R. The Evolutionary Pathway to Virulence of an RNA Virus. Cell 2017, 169, 35–46.e19. [Google Scholar] [CrossRef] [PubMed]
- Dunn, G.; Begg, N.T.; Cammack, N.; Minor, P.D. Virus excretion and mutation by infants following primary vaccination with live oral poliovaccine from two sources. J. Med. Virol. 1990, 32, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Laassri, M.; Dragunsky, E.; Enterline, J.; Eremeeva, T.; Ivanova, O.; Lottenbach, K.; Belshe, R.; Chumakov, K. Genomic analysis of vaccine-derived poliovirus strains in stool specimens by combination of full-length PCR and oligonucleotide microarray hybridization. J. Clin. Microbiol. 2005, 43, 2886–2894. [Google Scholar] [CrossRef]
- Laassri, M.; Lottenbach, K.; Belshe, R.; Rennels, M.; Plotkin, S.; Chumakov, K. Analysis of reversions in the 5′-untranslated region of attenuated poliovirus after sequential administration of inactivated and oral poliovirus vaccines. J. Infect. Dis. 2006, 193, 1344–1349. [Google Scholar] [CrossRef]
- Konopka-Anstadt, J.L.; Campagnoli, R.; Vincent, A.; Shaw, J.; Wei, L.; Wynn, N.T.; Smithee, S.E.; Bujaki, E.; Te Yeh, M.; Laassri, M.; et al. Development of a new oral poliovirus vaccine for the eradication end game using codon deoptimization. NPJ Vaccines 2020, 5, 26. [Google Scholar] [CrossRef]
- Yeh, M.T.; Bujaki, E.; Dolan, P.T.; Smith, M.; Wahid, R.; Konz, J.; Weiner, A.J.; Bandyopadhyay, A.S.; Van Damme, P.; De Coster, I.; et al. Engineering the Live-Attenuated Polio Vaccine to Prevent Reversion to Virulence. Cell Host Microbe 2020, 27, 736–751.e738. [Google Scholar] [CrossRef]
- Macadam, A.J.; Ferguson, G.; Stone, D.M.; Meredith, J.; Knowlson, S.; Auda, G.; Almond, J.W.; Minor, P.D. Rational design of genetically stable, live-attenuated poliovirus vaccines of all three serotypes: Relevance to poliomyelitis eradication. J. Virol. 2006, 80, 8653–8663. [Google Scholar] [CrossRef]
- WHO. WHO: Meeting of Strategic Advisory Group of Experts on Immunization, October 2021: Conclusions and Recommendations; WHO: Geneva, Switzerland, 2021; Volume 50, pp. 613–632.
- Konz, J.O.; Schofield, T.; Carlyle, S.; Wahid, R.; Ansari, A.; Strating, J.; Yeh, M.T.; Manukyan, H.; Smits, S.L.; Tritama, E.; et al. Evaluation and validation of next-generation sequencing to support lot release for a novel type 2 oral poliovirus vaccine. Vaccine X 2021, 8, 100102. [Google Scholar] [CrossRef]
- Van Damme, P.; De Coster, I.; Revets, H.; Bandyopadhyay, A.S. Poliopolis. Lancet 2019, 394, 115. [Google Scholar] [CrossRef]
- Simonyan, V.; Mazumder, R. High-Performance Integrated Virtual Environment (HIVE) Tools and Applications for Big Data Analysis. Genes 2014, 5, 957–981. [Google Scholar] [CrossRef] [PubMed]
- Laassri, M.; Cherkasova, E.; Abu-Asab, M.S.; Chumakov, K. Microarray Techniques for Evaluation of Genetic Stability of Live Viral Vaccines. In Viral Genomes—Molecular Structure, Diversity, Gene Expression Mechanisms and Host-Virus Interactions; Book Series; Garcia, M., Ed.; IntechOpen: London, UK, 2012. [Google Scholar]
- Manukyan, H.; Rodionova, E.; Zagorodnyaya, T.; Lin, T.L.; Chumakov, K.; Laassri, M. Multiplex PCR-based titration (MPBT) assay for determination of infectious titers of the three Sabin strains of live poliovirus vaccine. Virol. J. 2019, 16, 122. [Google Scholar] [CrossRef] [PubMed]
- Gambaryan, A.S.; Marinina, V.P.; Tuzikov, A.B.; Bovin, N.V.; Rudneva, I.A.; Sinitsyn, B.V.; Shilov, A.A.; Matrosovich, M.N. Effects of host-dependent glycosylation of hemagglutinin on receptor-binding properties on H1N1 human influenza A virus grown in MDCK cells and in embryonated eggs. Virology 1998, 247, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.T.; McGregor, M.; Suzuki, T.; Suzuki, Y.; Kawaoka, Y. Adaptation of influenza A viruses to cells expressing low levels of sialic acid leads to loss of neuraminidase activity. J. Virol. 2001, 75, 3766–3770. [Google Scholar] [CrossRef] [PubMed]
- Schild, G.C.; Oxford, J.S.; de Jong, J.C.; Webster, R.G. Evidence for host-cell selection of influenza virus antigenic variants. Nature 1983, 303, 706–709. [Google Scholar] [CrossRef]
- Cann, A.J.; Stanway, G.; Hughes, P.J.; Minor, P.D.; Evans, D.M.; Schild, G.C.; Almond, J.W. Reversion to neurovirulence of the live-attenuated Sabin type 3 oral poliovirus vaccine. Nucleic Acids Res. 1984, 12, 7787–7792. [Google Scholar] [CrossRef]
- Macadam, A.J.; Pollard, S.R.; Ferguson, G.; Skuce, R.; Wood, D.; Almond, J.W.; Minor, P.D. Genetic basis of attenuation of the Sabin type 2 vaccine strain of poliovirus in primates. Virology 1993, 192, 18–26. [Google Scholar] [CrossRef]
- Christodoulou, C.; Colbere-Garapin, F.; Macadam, A.; Taffs, L.F.; Marsden, S.; Minor, P.; Horaud, F. Mapping of mutations associated with neurovirulence in monkeys infected with Sabin 1 poliovirus revertants selected at high temperature. J. Virol. 1990, 64, 4922–4929. [Google Scholar] [CrossRef]
- Chumakov, K.M. Molecular consistency monitoring of oral poliovirus vaccine and other live viral vaccines. Dev. Biol. Stand. 1999, 100, 67–74. [Google Scholar]
- Chumakov, K.M.; Powers, L.B.; Noonan, K.E.; Roninson, I.B.; Levenbook, I.S. Correlation between amount of virus with altered nucleotide sequence and the monkey test for acceptability of oral poliovirus vaccine. Proc. Natl. Acad. Sci. USA 1991, 88, 199–203. [Google Scholar] [CrossRef]
- Bidzhieva, B.; Laassri, M.; Chumakov, K. Allele-specific PCR for quantitative analysis of mutants in live viral vaccines. J. Virol. Methods 2014, 201, 86–92. [Google Scholar] [CrossRef]
- Delobel, P.; Saliou, A.; Nicot, F.; Dubois, M.; Trancart, S.; Tangre, P.; Aboulker, J.P.; Taburet, A.M.; Molina, J.M.; Massip, P.; et al. Minor HIV-1 variants with the K103N resistance mutation during intermittent efavirenz-containing antiretroviral therapy and virological failure. PLoS ONE 2011, 6, e21655. [Google Scholar] [CrossRef] [PubMed]
- Germer, S.; Holland, M.J.; Higuchi, R. High-throughput SNP allele-frequency determination in pooled DNA samples by kinetic PCR. Genome Res. 2000, 10, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Kianianmomeni, A.; Schwarz, G.; Felsenstein, F.G.; Wenzel, G. Validation of a real-time PCR for the quantitative estimation of a G143A mutation in the cytochrome bc1 gene of Pyrenophora teres. Pest Manag. Sci. 2007, 63, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Punia, P.; Cane, P.; Teo, C.G.; Saunders, N. Quantitation of hepatitis B lamivudine resistant mutants by real-time amplification refractory mutation system PCR. J. Hepatol. 2004, 40, 986–992. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, G.; Baumler, S.; Block, A.; Felsenstein, F.G.; Wenzel, G. Determination of detection and quantification limits for SNP allele frequency estimation in DNA pools using real time PCR. Nucleic Acids Res. 2004, 32, e24. [Google Scholar] [CrossRef][Green Version]
- Taira, C.; Matsuda, K.; Saito, S.; Sakashita, K.; Sugano, M.; Okumura, N.; Honda, T. Application of allele-specific quantitative PCR using genomic DNA to monitor minimal residual disease based on mutant gene levels following allogeneic hematopoietic stem cell transplantation in patients with hematological malignancies: Comparison of mutant levels with autologous DNA percentage by short tandem repeat-PCR. Clin. Chim. Acta 2012, 413, 516–519. [Google Scholar]
- Wahid, R.; Mercer, L.; Gast, C.; De Leon, T.; Saez-Llorens, X.; Fix, A.; Macadam, A.; Stephens, L.; Chumakov, K.; Smits, S.L.; et al. Evaluating stability of attenuated Sabin and two novel type 2 oral poliovirus vaccines in children. NPJ Vaccines 2022, 7, 19. [Google Scholar] [CrossRef]
| Name of Oligos | Sequence 5′-->3′ | Tm (Basic) | Oligo Size | Amplicon Size (bp) |
|---|---|---|---|---|
| Oligonucleotides for detection of VP1-I143T nOPV2-c1 mutant variants | ||||
| Pr143s-2938F (forward) | GGAGTTCACTTTTGTGGTCACCTC | 56 | 24 | 74 |
| Pr143s-3011R (reverse) | TCTGATAAACTTGGTTCAATGCATGTCCGT | 59 | 30 | |
| Prb143Cs12 FAM (mutant probe) | FAM-ACTACACTGATG–MGBNFQ | 34 | 12 | |
| Prb143Aa13 VIC (non-mutant probe) | VIC-GCATCAATGTAGT–MGBNFQ | 36 | 13 | |
| Oligonucleotides for detection of N171D nOPV2-c1 mutant variants | ||||
| nOPV2c1_3021F (forward) | TACCACCCGGAGCACCTATC | 56 | 20 | 60 |
| nOPV2c1_3080R (reverse) | TAGAGGACGTCTGCCACGTA | 54 | 20 | |
| Prb171G-a12FAM (mutant probe) | FAM-TCATCCCATTTA-MGBNFQ | 36 | 12 | |
| Prb171T-12VIC (non-mutant probe) | VIC-TCATTCCATTTA-MGBNFQ | 30 | 12 | |
| Oligonucleotides for detection of E295K nOPV2-c1 mutant variants | ||||
| Sab2_3396R (reverse) | GTGTCCAAATCCATAAGTCG | 50 | 20 | 61 |
| Sab2_3336F (forward) | TTATAAAGATGGGCTCACCC | 50 | 20 | |
| PrbA11VIC (mutant probe) | VIC-TACCAAAAAAG-MGBNFQ | 28 | 11 | |
| Prb295Ca13FAM (non-mutant probe) | FAM-CCTTTTCTGGTAG-MGBNFQ | 38 | 13 | |
| Spiked Mutants % | Observed Mutants % | |
|---|---|---|
| NGS | qmosRT-PCR | |
| 50.00 | 47.73 | 58.19 ± 2.22 |
| 25.00 | 24.06 | 28.53 ± 0.42 |
| 12.50 | 12.12 | 14.47 ± 1.84 |
| 6.30 | 6.17 | 6.01 ± 0.17 |
| 3.10 | 3.11 | 1.78 ± 0.22 |
| 1.60 | 2.07 | 0.41 ± 0.05 |
| 0.80 | 0.87 | 0.13 ± 0.02 |
| 0.40 | 0.42 | 0.01 ± 0.00 |
| 0.20 | 0.24 | ND |
| 0.10 | 0.13 | ND |
| Expected Mutant % (GC #) | NGS (Set 1 and Set 2) | qmosRT-PCR Runs-Mutant % | ||||||
|---|---|---|---|---|---|---|---|---|
| Set 1 of Spiked Samples | Set 2 of Spiked Samples | Average ± SD | ||||||
| Mutant % ± SD | Run 1 | Run 2 | Run 3 | Run 4 | Run 5 | Run 6 | ||
| 75.12 | 76.69 ± 0.27 | 89.68 | 81.88 | 80.04 | 89.98 | 89.42 | 89.96 | 86.83 ± 4.59 |
| 50.34 | 52.63 ± 2.25 | 68.42 | 53.02 | 54.33 | 69.74 | 68.30 | 69.08 | 63.81 ± 7.88 |
| 30.41 | 28.37 ± 0.59 | 41.17 | 31.03 | 32.49 | 49.39 | 47.39 | 49.81 | 41.88 ± 8.44 |
| 17.00 | 16.51 ± 1.08 | 22.07 | 13.31 | 14.46 | 28.88 | 27.00 | 32.27 | 23.00 ± 7.80 |
| 9.03 | 8.28 ± 0.02 | 10.25 | 6.94 | 7.63 | 14.37 | 13.09 | 15.99 | 11.38 ± 3.69 |
| 4.67 | 3.94 ± 0.26 | 2.56 | 2.36 | 2.27 | 5.47 | 4.86 | 7.49 | 4.17 ± 2.13 |
| 2.37 | 2.22 ± 0.35 | 0.28 | 0.55 | 0.42 | 1.24 | 1.07 | 1.68 | 0.87 ± 0.54 |
| 1.20 | 0.63 ± 0.21 | 0.01 | 0.12 | 0.07 | 0.16 | 0.13 | 0.34 | 0.14 ± 0.11 |
| 0.60 | 0.66 ± 0.29 | ND | 0.005 | 0.01 | 0.02 | 0.01 | 0.02 | 0.01 ± 0.01 |
| 0.30 | 0.42 ± 0.10 | ND | ND | ND | ND | ND | ND | ND |
| 0.15 | ND | ND | ND | ND | ND | ND | ND | ND |
| Expected Mutant % (GC #) | NGS (Set 1 and Set 2) | qmosRT-PCR Runs | ||||||
|---|---|---|---|---|---|---|---|---|
| Set 1 of Spiked Samples | Set 2 of Spiked Samples | Average ± SD | ||||||
| Mutant % ± SD | Run 1 | Run 2 | Run 3 | Run 4 | Run 5 | Run 6 | ||
| 53.29 | 39.28 ± 2.36 | 38.404 | 43.317 | 40.463 | 40.320 | 34.621 | 45.197 | 40.39 ± 3.71 |
| 27.60 | 16.00 ± 2.17 | 18.693 | 21.507 | 20.613 | 20.178 | 16.869 | 22.819 | 20.11 ± 2.10 |
| 14.06 | 7.89 ± 0.12 | 8.239 | 9.495 | 10.461 | 10.638 | 10.124 | 12.092 | 10.17 ± 1.28 |
| 7.09 | 3.56 ± 0.14 | 3.732 | 4.525 | 4.532 | 4.143 | 3.517 | 4.581 | 4.17 ± 0.46 |
| 3.56 | 1.45 ± 0.15 | 1.859 | 1.547 | 1.747 | 1.270 | 1.815 | 1.965 | 1.70 ± 0.25 |
| 1.79 | 0.76 ± 0.05 | 0.286 | 0.579 | 0.615 | 0.386 | 0.197 | 0.470 | 0.42 ± 0.16 |
| 0.89 | 0.46 ± 0.48 | 0.004 | 0.054 | 0.017 | 0.024 | 0.008 | 0.071 | 0.03 ± 0.03 |
| 0.45 | ND | ND | ND | ND | ND | ND | ND | ND |
| Expected Mutant % (GC #) | NGS (Set 1 and Set 2) | qmosRT-PCR Runs—Mutants % | ||||||
|---|---|---|---|---|---|---|---|---|
| Set 1 of Spiked Samples | Set 2 of Spiked Samples | Average ± SD | ||||||
| Mutant % ± SD | Run 1 | Run 2 | Run 3 | Run 4 | Run 5 | Run 6 | ||
| 40.42 | 60.98 ± 9.81 | 55.58 | 54.10 | 52.89 | 32.96 | 43.76 | 48.40 | 47.95 ± 8.52 |
| 18.68 | 29.03 ± 4.00 | 34.70 | 26.44 | 25.87 | 24.77 | 25.63 | 28.32 | 27.62 ± 3.67 |
| 9.02 | 13.48 ± 3.30 | 25.31 | 15.51 | 15.66 | 15.03 | 15.16 | 17.17 | 17.31 ± 4.00 |
| 4.44 | 6.52 ± 1.48 | 15.33 | 8.52 | 8.48 | 7.25 | 7.96 | 9.24 | 9.46 ± 2.95 |
| 2.20 | 3.42 ± 1.24 | 4.29 | 1.96 | 3.75 | 3.40 | 1.85 | 2.44 | 2.95 ± 1.01 |
| 1.10 | 1.59 ± 0.96 | 1.79 | 0.80 | 1.41 | 1.26 | 0.13 | 0.75 | 1.02 ± 0.59 |
| 0.55 | 0.94 ± 0.14 | 0.17 | 0.03 | 0.15 | 0.18 | 0.02 | 0.01 | 0.09 ± 0.08 |
| 0.27 | 2.38 ± 2.60 | ND | ND | ND | ND | ND | ND | ND |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manukyan, H.; Wahid, R.; Ansari, A.; Tritama, E.; Macadam, A.; Konz, J.; Chumakov, K.; Laassri, M. Quantitative RT-PCR Assays for Quantification of Undesirable Mutants in the Novel Type 2 Oral Poliovirus Vaccine. Vaccines 2022, 10, 1394. https://doi.org/10.3390/vaccines10091394
Manukyan H, Wahid R, Ansari A, Tritama E, Macadam A, Konz J, Chumakov K, Laassri M. Quantitative RT-PCR Assays for Quantification of Undesirable Mutants in the Novel Type 2 Oral Poliovirus Vaccine. Vaccines. 2022; 10(9):1394. https://doi.org/10.3390/vaccines10091394
Chicago/Turabian StyleManukyan, Hasmik, Rahnuma Wahid, Azeem Ansari, Erman Tritama, Andrew Macadam, John Konz, Konstantin Chumakov, and Majid Laassri. 2022. "Quantitative RT-PCR Assays for Quantification of Undesirable Mutants in the Novel Type 2 Oral Poliovirus Vaccine" Vaccines 10, no. 9: 1394. https://doi.org/10.3390/vaccines10091394
APA StyleManukyan, H., Wahid, R., Ansari, A., Tritama, E., Macadam, A., Konz, J., Chumakov, K., & Laassri, M. (2022). Quantitative RT-PCR Assays for Quantification of Undesirable Mutants in the Novel Type 2 Oral Poliovirus Vaccine. Vaccines, 10(9), 1394. https://doi.org/10.3390/vaccines10091394






