COVID-19 Vaccination and Mental Health Outcomes among Greek Adults in 2021: Preliminary Evidence
Abstract
:1. Introduction
2. Methods
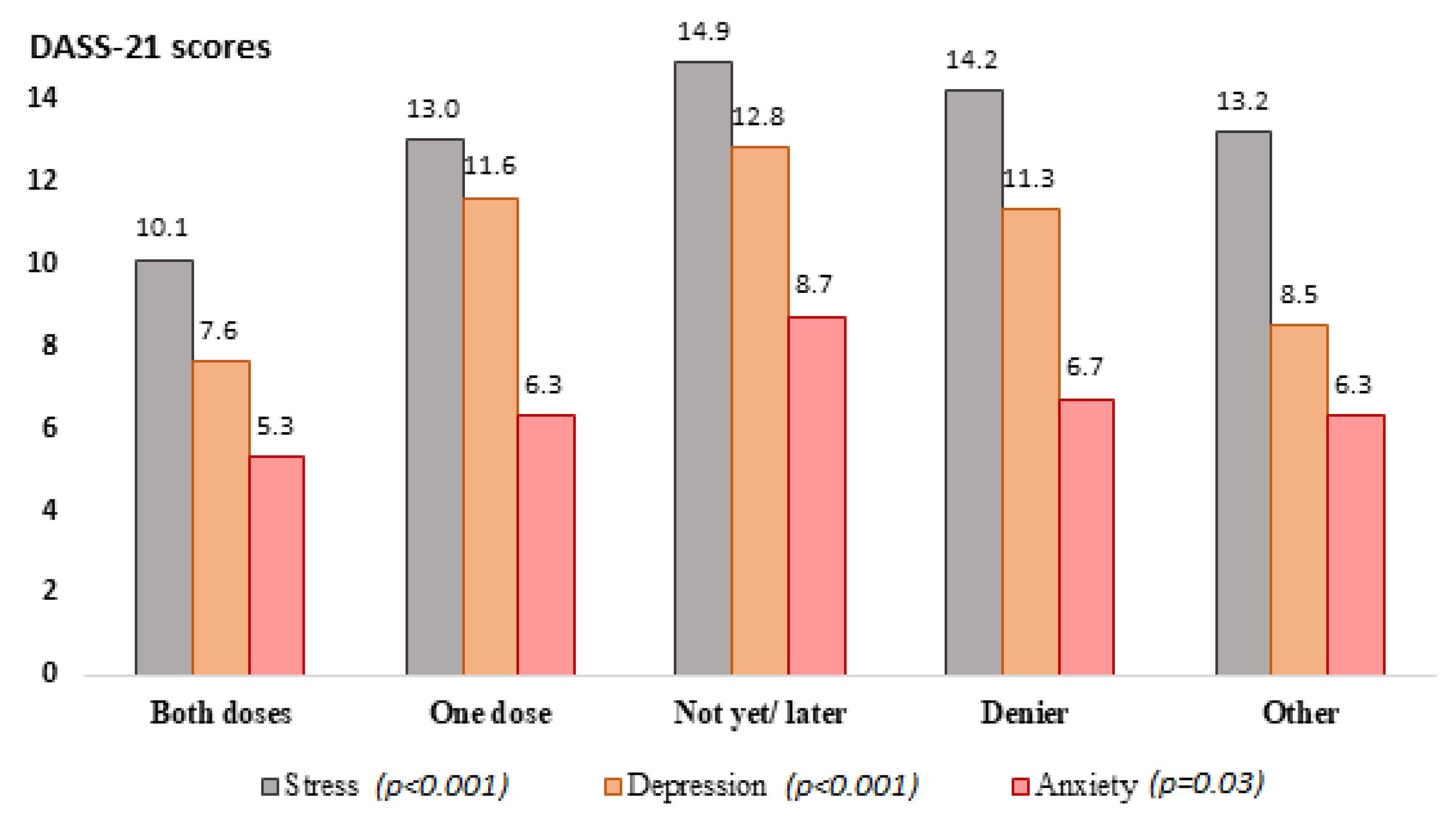
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taquet, M.; Luciano, S.; Geddes, J.R.; Harrison, P.J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2021, 8, 130–140. [Google Scholar] [CrossRef]
- Ghebreyesus, T.A. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Ferracuti, S.; Da Molin, G.; Diella, G.; Montagna, M.T.; Orsi, G.B.; Liguori, G.; Napoli, C. Knowledge and Lifestyle Behaviors Related to COVID-19 Pandemic in People over 65 Years Old from Southern Italy. Int. J. Environ. Res. Public Health 2021, 18, 10872. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, S.A.M.; Swilam, M.M.; El-Wahed, A.A.A.; Du, M.; El-Seedi, H.H.R.; Kai, G.; Masry, S.H.D.; Abdel-Daim, M.M.; Zou, X.; Halabi, M.F.; et al. Beyond the Pandemic: COVID-19 Pandemic Changed the Face of Life. Int. J. Environ. Res. Public Health 2021, 18, 5645. [Google Scholar] [CrossRef]
- Shiina, A.; Niitsu, T.; Kobori, O.; Idemoto, K.; Hashimoto, T.; Sasaki, T.; Igarashi, Y.; Shimizu, E.; Nakazato, M.; Hashimoto, K.; et al. Relationship between perception and anxiety about COVID-19 infection and risk behaviors for spreading infection: A national survey in Japan. Brain Behav. Immun. Health 2020, 6, 100–101. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China Brain. Behav. Immun. Health 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Nivette, A.; Ribeaud, D.; Murray, A.; Steinhoff, A.; Bechtiger, L.; Hepp, U.; Shanahan, L.; Eisner, M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc. Sci. Med. 2021, 268, 113370. [Google Scholar] [CrossRef]
- Lurie, N.; Saville, M.; Hatchett, R.; Halton, J. Developing COVID-19 Vaccines at Pandemic Speed. N. Engl. J. Med. 2020, 382, 1969–1973. [Google Scholar] [CrossRef] [PubMed]
- Giannouchos, T.V.; Steletou, E.; Saridi, M.; Souliotis, K. Mandatory vaccination support and intentions to get vaccinated for COVID-19: Results from a nationally representative general population survey in October 2020 in Greece. J. Eval. Clin. Pract. 2021, 27, 996–1003. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.-L.; Luo, W.; Li, H.-M.; Zhang, Q.-Q.; Liu, X.-G.; Li, W.-T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Al-Hasan, A.; Yim, D.; Khuntia, J. Citizens’ Adherence to COVID-19 Mitigation Recommendations by the Government: A 3-Country Comparative Evaluation Using Web-Based Cross-Sectional Survey Data. J. Med. Internet Res. 2020, 22, e20634. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef]
- Lyrakos, G.; Arvaniti, C.; Smyrnioti, M.; Kostopanagiotou, G. Translation and validation study of the depression anxiety stress scale in the greek general population and in a psychiatric patient’s sample. Eur. Psychiatry 2011, 26, 1731. [Google Scholar] [CrossRef]
- Pezirkianidis, C.; Karakasidou, E.; Lakioti, A.; Stalikas, A.; Galanakis, M. Psychometric Properties of the Depression, Anxiety, Stress Scales-21 (DASS-21) in a Greek Sample. Psychology 2018, 9, 2933–2950. [Google Scholar] [CrossRef] [Green Version]
- Souliotis, K.; Peppou, L.; Samara, M.; Giannouchos, T.; Nimatoudis, J.; Papageorgiou, C.; Leucht, S.; Economou, M. Knowledge, perceptions and mental health impact of the COVID-19 pandemic in the Greek general population. Arch. Hell. Med. 2021, 32, 271–281. [Google Scholar]
- Souliotis, K.; Giannouchos, T.V.; Peppou, L.E.; Samara, M.T.; Nimatoudis, J.; Papageorgiou, C.; Economou, M. Public Health Behaviors during the COVID-19 Pandemic in Greece and Associated Factors: A Nationwide Cross-sectional Survey. Inq. J. Health Care Organ. Provis. Financ. 2021, 58, 00469580211022913. [Google Scholar] [CrossRef]
- Solomou, I.; Constantinidou, F. Prevalence and Predictors of Anxiety and Depression Symptoms during the COVID-19 Pandemic and Compliance with Precautionary Measures: Age and Sex Matter. Int. J. Environ. Res. Public Health 2020, 17, 4924. [Google Scholar] [CrossRef] [PubMed]
- Steimer, T. The biology of fear- and anxiety-related behaviors. Dialogues Clin. Neurosci. 2002, 4, 231–249. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C. The Effects of Stressful Life Events on Depression. Annu. Rev. Psychol. 1997, 48, 191–214. [Google Scholar] [CrossRef]
- Savas, E.; Tanriverdi, D. Knowledge, attitudes and anxiety towards influenza A/H1N1 vaccination of healthcare workers in Turkey. BMC Infect. Dis. 2010, 10, 281. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, T.; Zubatsky, M.; Meyer, D. The association between mental health diagnoses and influenza vaccine receipt among older primary care patients. Psychol. Health Med. 2020, 25, 1083–1093. [Google Scholar] [CrossRef]
- Thorpe, J.M.; Thorpe, C.T.; Kennelty, K.A.; Pandhi, N. Patterns of perceived barriers to medical care in older adults: A latent class analysis. BMC Health Serv. Res. 2011, 11, 181. [Google Scholar] [CrossRef] [Green Version]
- Geldsetzer, P. Knowledge and perceptions of COVID-19 among the general public in the United States and the United King-dom: A cross-sectional onlne survey. Ann. Intern. Med. 2020, 173, M20-0912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hermans, L.; van den Broucke, S.; Gisle, L.; Demarest, S.; Charafeddine, R. Mental health, compliance with measures and health prospects during the COVID-19 pandemic: The role of health literacy. BMC Public Health 2021, 21, 1365. [Google Scholar] [CrossRef]
- World Health Organization. World Mental Health Report: Transforming Mental Health for All; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Economou, M.; Bergiannaki, J.D.; Peppou, L.E.; Karayanni, I.; Skalkotos, G.; Patelakis, A.; Souliotis, K.; Stefanis, C. Attitudes towards depression, psychiatric medication and help-seeking intentions amid financial crisis: Findings from Athens area. Int. J. Soc. Psychiatry 2016, 62, 243–251. [Google Scholar] [CrossRef]
| Depression | Anxiety | Stress | |
|---|---|---|---|
| Normal | 0–4 | 0–3 | 0–7 |
| Mild | 5–6 | 4–5 | 8–9 |
| Moderate | 7–10 | 6–7 | 10–12 |
| Severe | 11–13 | 8–9 | 13–16 |
| Extremely severe | 14+ | 10+ | 17+ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souliotis, K.; Peppou, L.E.; Giannouchos, T.V.; Samara, M.; Sifaki-Pistolla, D.; Economou, M.; Maltezou, H.C. COVID-19 Vaccination and Mental Health Outcomes among Greek Adults in 2021: Preliminary Evidence. Vaccines 2022, 10, 1371. https://doi.org/10.3390/vaccines10081371
Souliotis K, Peppou LE, Giannouchos TV, Samara M, Sifaki-Pistolla D, Economou M, Maltezou HC. COVID-19 Vaccination and Mental Health Outcomes among Greek Adults in 2021: Preliminary Evidence. Vaccines. 2022; 10(8):1371. https://doi.org/10.3390/vaccines10081371
Chicago/Turabian StyleSouliotis, Kyriakos, Lily E. Peppou, Theodoros V. Giannouchos, Myrto Samara, Dimitra Sifaki-Pistolla, Marina Economou, and Helena C. Maltezou. 2022. "COVID-19 Vaccination and Mental Health Outcomes among Greek Adults in 2021: Preliminary Evidence" Vaccines 10, no. 8: 1371. https://doi.org/10.3390/vaccines10081371
APA StyleSouliotis, K., Peppou, L. E., Giannouchos, T. V., Samara, M., Sifaki-Pistolla, D., Economou, M., & Maltezou, H. C. (2022). COVID-19 Vaccination and Mental Health Outcomes among Greek Adults in 2021: Preliminary Evidence. Vaccines, 10(8), 1371. https://doi.org/10.3390/vaccines10081371









