Understanding the Role of Psychosocial Factors in Pakistani Parents’ Hesitancy to Vaccinate Their Kids: The Mediating Role of Knowledge and Mistrust of Science about the COVID-19 Vaccine
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants
2.2. Measures
2.3. Predicting and Predictor Variables
2.3.1. Parents’ Intention towrds COVID-19 Vaccine
2.3.2. Mistrust in Science about COVID-19
2.3.3. Vaccine Knowledge
2.3.4. Risk Perception
2.3.5. Self-Efficacy
2.3.6. COVID-19 Vaccine Safety
2.3.7. Conspiracy Beliefs
2.4. Statistical Analysis
3. Result
3.1. Descriptive Statistics
3.2. Measurement Model
3.2.1. Exploratory Factor Analysis (EFA)
3.2.2. Confirmatory Factor Analysis (CFA)
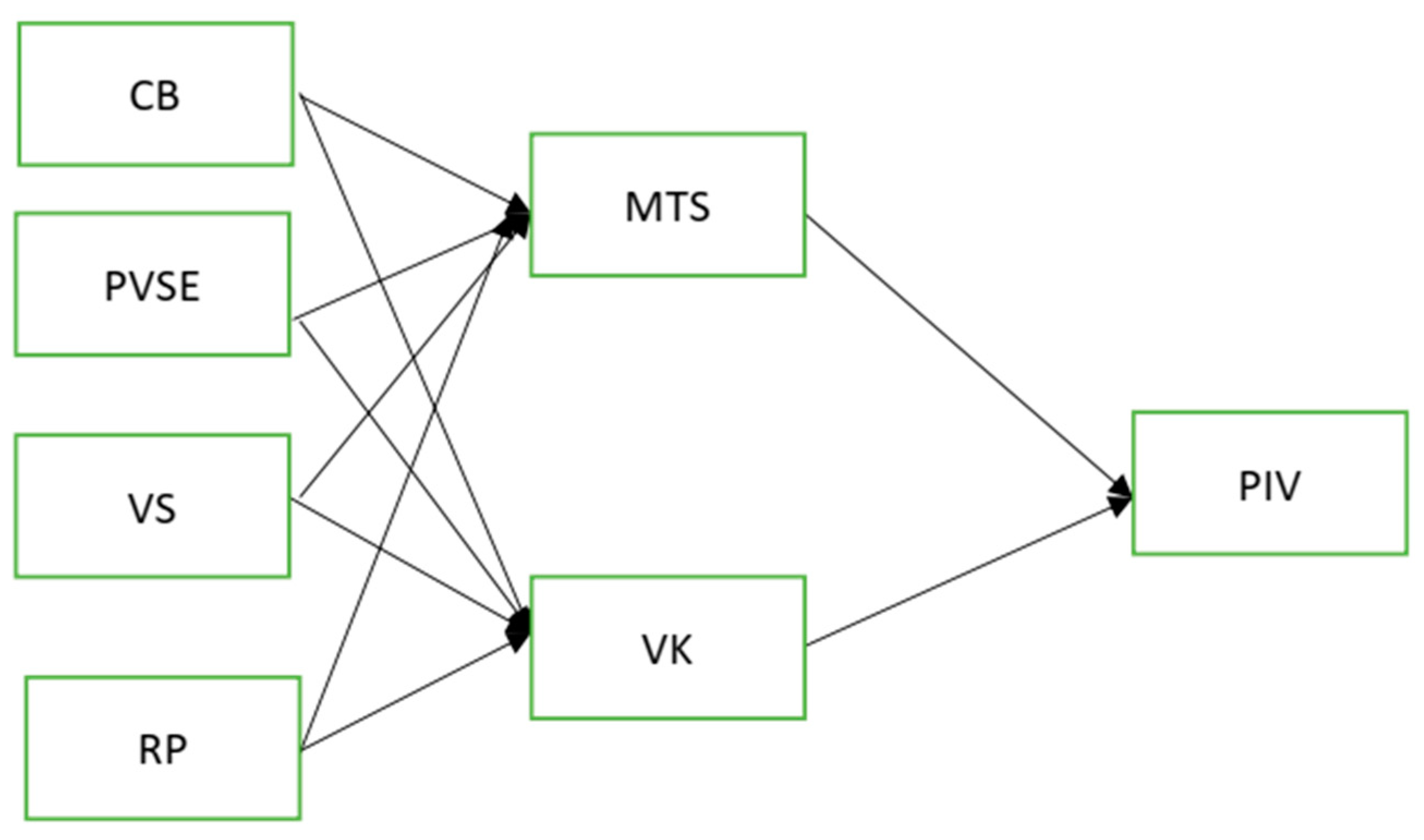
3.3. Structural Equation Modeling
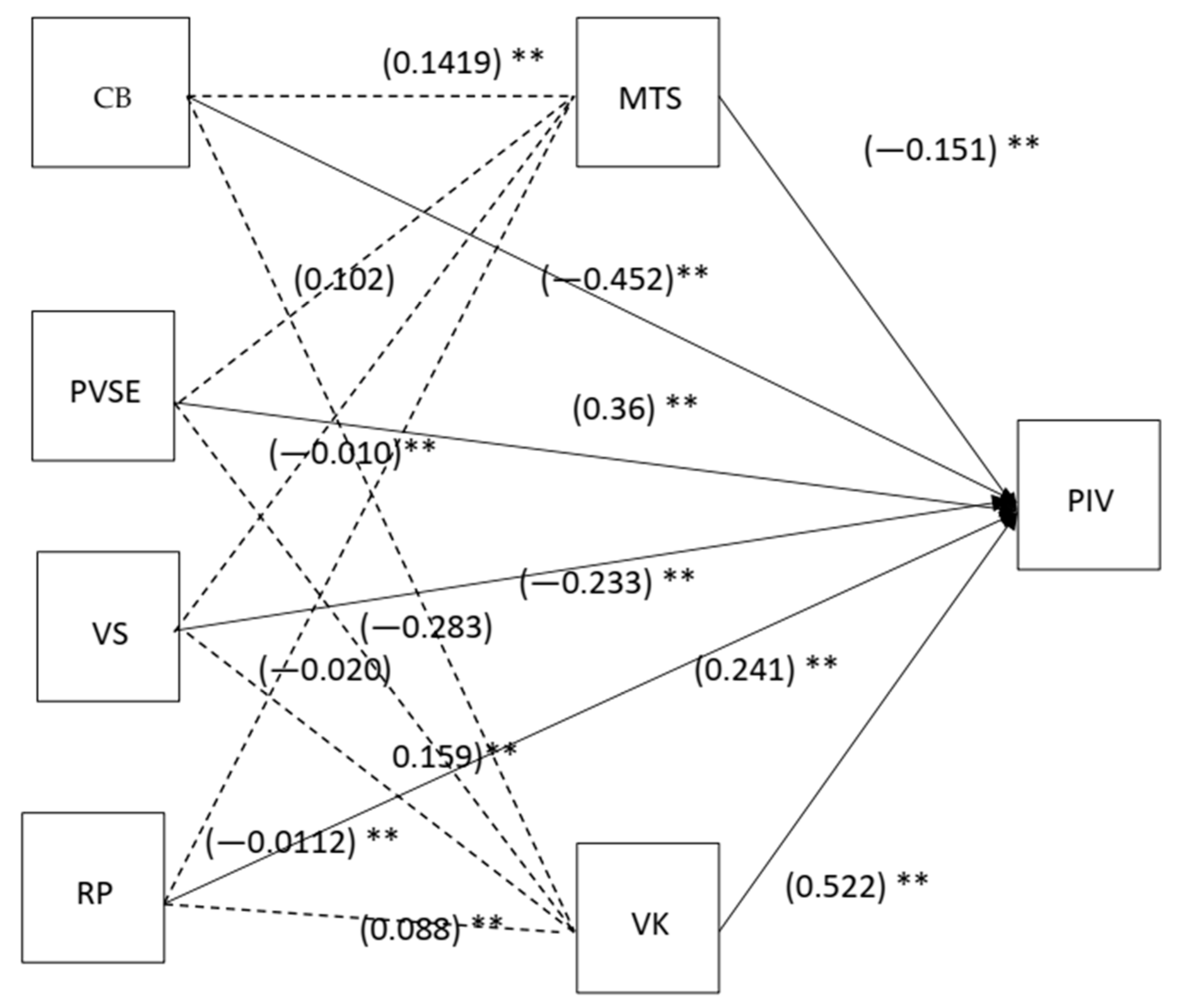
Mediation Test
4. Discussion
4.1. Mediating Effects of Vaccine Knowledge
4.2. Mediating Role of Mistrust in Science
5. Limitations
6. Implications
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Truong, J.; Bakshi, S.; Wasim, A.; Ahmad, M.; Majid, U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot. Int. 2021, 37, daab105. [Google Scholar] [CrossRef] [PubMed]
- Bärnighausen, T.; Bloom, D.E.; Cafiero-Fonseca, E.T.; O’Brien, J.C. Valuing vaccination. Proc. Natl. Acad. Sci. USA 2014, 111, 12313–12319. [Google Scholar] [CrossRef] [Green Version]
- Hill, H.A.; Elam-Evans, L.D.; Yankey, D.; Singleton, J.A.; Kang, Y. Vaccination coverage among children aged 19–35 months—United States, 2017. Morb. Mortal. Wkly. Rep. 2018, 67, 1123. [Google Scholar] [CrossRef] [PubMed]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 2015, 33, D66–D71. [Google Scholar] [CrossRef]
- Mellerson, J.L.; Maxwell, C.B.; Knighton, C.L.; Kriss, J.L.; Seither, R.; Black, C.L. Vaccination coverage for selected vaccines and exemption rates among children in kindergarten—United States, 2017–2018 school year. Morb. Mortal. Wkly. Rep. 2018, 67, 1115. [Google Scholar] [CrossRef] [PubMed]
- Omer, S.B.; Porter, R.M.; Allen, K.; Salmon, D.A.; Bednarczyk, R.A. Trends in kindergarten rates of vaccine exemption and state-level policy, 2011–2016. In Open Forum Infectious Diseases; Oxford University Press: Oxford, MI, USA, 2018. [Google Scholar]
- Rosen, J.B.; Arciuolo, R.J.; Khawja, A.M.; Fu, J.; Giancotti, F.R.; Zucker, J.R. Public health consequences of a 2013 measles outbreak in New York City. JAMA Pediatr. 2018, 172, 811–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atwell, J.E.; Van Otterloo, J.; Zipprich, J.; Winter, K.; Harriman, K.; Salmon, D.A.; Halsey, N.A.; Omer, S.B. Nonmedical vaccine exemptions and pertussis in California, 2010. Pediatrics 2013, 132, 624–630. [Google Scholar] [CrossRef] [Green Version]
- Gust, D.A.; Strine, T.W.; Maurice, E.; Smith, P.; Yusuf, H.; Wilkinson, M.; Battaglia, M.; Wright, R.; Schwartz, B. Underimmunization among children: Effects of vaccine safety concerns on immunization status. Pediatrics 2004, 114, e16–e22. [Google Scholar] [CrossRef] [Green Version]
- Ruggiero, K.M.; Wong, J.; Sweeney, C.F.; Avola, A.; Auger, A.; Macaluso, M.; Reidy, P. Parents’ intentions to vaccinate their children against COVID-19. J. Pediatr. Health Care 2021, 35, 509–517. [Google Scholar] [CrossRef]
- Santibanez, T.A.; Nguyen, K.H.; Greby, S.M.; Fisher, A.; Scanlon, P.; Bhatt, A.; Srivastav, A.; Singleton, J.A. Parental vaccine hesitancy and childhood influenza vaccination. Pediatrics 2020, 146, e2020007609. [Google Scholar] [CrossRef]
- Elkin, L.E.; Pullon, S.R.; Stubbe, M.H. Should I vaccinate my child? comparing the displayed stances of vaccine information retrieved from Google, Facebook and YouTube. Vaccine 2020, 38, 2771–2778. [Google Scholar] [CrossRef] [PubMed]
- Guidry, J.P.; Carlyle, K.; Messner, M.; Jin, Y. On pins and needles: How vaccines are portrayed on Pinterest. Vaccine 2015, 33, 5051–5056. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J. The state of vaccine confidence. Lancet 2018, 392, 2244–2246. [Google Scholar] [CrossRef]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the vaccine confidence gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2014, 14, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Renkewitz, F.; Betsch, T.; Ulshöfer, C. The influence of vaccine-critical websites on perceiving vaccination risks. J. Health Psychol. 2010, 15, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Woolfolk, A.; Shaughnessy, M.F. An interview with Anita Woolfolk: The educational psychology of teacher efficacy. Educ. Psychol. Rev. 2004, 16, 153–176. [Google Scholar]
- Bandura, A.; Freeman, W.H.; Lightsey, R. Self-Efficacy: The Exercise of Control; Springer: Berlin/Heidelberg, Germany, 1999. [Google Scholar]
- Larson, H.J.; De Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Ban, H.-J.; Kim, H.-S. Applying the modified health belief model (HBM) to Korean medical tourism. Int. J. Environ. Res. Public Health 2020, 17, 3646. [Google Scholar] [CrossRef]
- Wijaya, D.; Misnaniarti, M.; Sitorus, R.J. Analysis of Wearing Masks Compliance among Palembang Residents during the COVID-19 Pandemic using the Health Belief Model (HBM) Construct. Aloha Int. J. Multidiscip. Adv. (AIJMU) 2022, 4, 23–28. [Google Scholar]
- Đorđević, J.M.; Mari, S.; Vdović, M.; Milošević, A. Links between conspiracy beliefs, vaccine knowledge, and trust: Anti-vaccine behavior of Serbian adults. Soc. Sci. Med. 2021, 277, 113930. [Google Scholar] [CrossRef] [PubMed]
- Shahnazi, H.; Abdolaliyan, N.; Kzemi, A.; Hasanzadeh, A. Determinants of the self-efficacy of physical activity for maintaining weight during pregnancy: The application of the health belief model. J. Educ. Health Promot. 2017, 6, 93. [Google Scholar] [CrossRef]
- Noar, S.M.; Zimmerman, R.S. Health behavior theory and cumulative knowledge regarding health behaviors: Are we moving in the right direction? Health Educ. Res. 2005, 20, 275–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caso, D.; Capasso, M.; Fabbricatore, R.; Conner, M. Understanding the psychosocial determinants of Italian parents’ intentions not to vaccinate their children: An extended theory of planned behaviour model. Psychol. Health 2021, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Dryhurst, S.; Schneider, C.R.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; van der Bles, A.M.; Spiegelhalter, D.; van der Linden, S. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020, 23, 994–1006. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of influenza vaccination intention and behavior—A systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Allison, M.A.; Reyes, M.; Young, P.; Calame, L.; Sheng, X.; Weng, H.-Y.C.; Byington, C.L. Parental attitudes about influenza immunization and school-based immunization for school-aged children. Pediatr. Infect. Dis. J. 2010, 29, 751–755. [Google Scholar] [CrossRef]
- Offutt-Powell, T.N.; Ojha, R.P.; Qualls-Hampton, R.; Stonecipher, S.; Singh, K.P.; Cardarelli, K.M. Parental risk perception and influenza vaccination of children in daycare centres. Epidemiol. Infect. 2013, 142, 134–141. [Google Scholar] [CrossRef] [Green Version]
- Flood, E.M.; Rousculp, M.D.; Ryan, K.J.; Beusterien, K.M.; Divino, V.M.; Toback, S.L.; Sasané, M.; Block, S.L.; Hall, M.C.; Mahadevia, P.J. Parents’ decision-making regarding vaccinating their children against influenza: A web-based survey. Clin. Ther. 2010, 32, 1448–1467. [Google Scholar] [CrossRef]
- Cori, L.; Bianchi, F.; Cadum, E.; Anthonj, C. Risk Perception and COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3114. [Google Scholar] [CrossRef]
- Andrade, G.E.; Hussain, A. Polio in Pakistan: Political, sociological, and epidemiological factors. Cureus 2018, 10, e3502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ittefaq, M.; Baines, A.; Abwao, M.; Shah, S.F.A.; Ramzan, T. Does Pakistan still have polio cases? Exploring discussions on polio and polio vaccine in online news comments in Pakistan. Vaccine 2021, 39, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Kanozia, R.; Arya, R. “Fake news”, religion, and COVID-19 vaccine hesitancy in India, Pakistan, and Bangladesh. Media Asia 2021, 48, 313–321. [Google Scholar] [CrossRef]
- Ejaz, W.; Ittefaq, M.; Seo, H.; Naz, F. Factors associated with the belief in COVID-19 related conspiracy theories in Pakistan. Health Risk Soc. 2021, 23, 162–178. [Google Scholar] [CrossRef]
- Freeman, D.; Waite, F.; Rosebrock, L.; Petit, A.; Causier, C.; East, A.; Jenner, L.; Teale, A.-L.; Carr, L.; Mulhall, S.; et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. 2020, 52, 251–263. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Vikram, K.; Vanneman, R.; Desai, S. Linkages between maternal education and childhood immunization in India. Soc. Sci. Med. 2012, 75, 331–339. [Google Scholar] [CrossRef] [Green Version]
- Abdelhafiz, A.S.; Mohammed, Z.; Ibrahim, M.E.; Ziady, H.H.; Alorabi, M.; Ayyad, M.; Sultan, E.A. Knowledge, perceptions, and attitude of egyptians towards the novel coronavirus disease (COVID-19). J. Community Health 2020, 45, 881–890. [Google Scholar] [CrossRef]
- Allum, N.; Sturgis, P.; Tabourazi, D.; Brunton-Smith, I. Science knowledge and attitudes across cultures: A meta-analysis. Public Underst. Sci. 2008, 17, 35–54. [Google Scholar] [CrossRef] [Green Version]
- Hudson, A.; Montelpare, W. Predictors of vaccine hesitancy: Implications for COVID-19 public health messaging. Int. J. Environ. Res. Public Health 2021, 18, 8054. [Google Scholar] [CrossRef]
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Ren, J.; Huang, Z.; Contreras-Roldan, I.L.; Gebremeskel, B.; et al. Comparisons of vaccine hesitancy across five low- and middle-income countries. Vaccines 2019, 7, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dube, E.; Bettinger, J.A.; Halperin, B.; Bradet, R.; Lavoie, F.; Sauvageau, C.; Gilca, V.; Boulianne, N. Determinants of parents’ decision to vaccinate their children against rotavirus: Results of a longitudinal study. Health Educ. Res. 2012, 27, 1069–1080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Lier, A.; Ferreira, J.A.; Mollema, L.; Sanders, E.A.M.; de Melker, H.E. Intention to vaccinate universally against varicella, rotavirus gastroenteritis, meningococcal B disease and seasonal influenza among parents in the Netherlands: An internet survey. BMC Res. Notes 2017, 10, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Askelson, N.M.; Campo, S.; Lowe, J.B.; Smith, S.; Dennis, L.K.; Andsager, J. Using the theory of planned behavior to predict mothers’ intentions to vaccinate their daughters against HPV. J. Sch. Nurs. 2010, 26, 194–202. [Google Scholar] [CrossRef]
- Simione, L.; Vagni, M.; Gnagnarella, C.; Bersani, G.; Pajardi, D. Mistrust and beliefs in conspiracy theories differently mediate the effects of psychological factors on propensity for COVID-19 Vaccine. Front. Psychol. 2021, 12, 683684. [Google Scholar] [CrossRef] [PubMed]
- Ilogu, L.C.; Lugovska, O.; Vojtek, I.; Prugnola, A.; Callegaro, A.; Mazzilli, S.; Van Damme, P. The intent of students to vaccinate is influenced by cultural factors, peer network, and knowledge about vaccines. Hum. Vaccines Immunother. 2021, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.Y.; Chang, P.-J. The effect of coronavirus disease-19 (COVID-19) risk perception on behavioural intention towards ‘untact’ tourism in South Korea during the first wave of the pandemic (March 2020). Curr. Issues Tour. 2020, 24, 1017–1035. [Google Scholar] [CrossRef]
- Witte, K. Fear control and danger control: A test of the extended parallel process model (EPPM). Commun. Monogr. 1994, 61, 113–134. [Google Scholar] [CrossRef]
- Brabin, L.; Roberts, S.; Farzaneh, F.; Kitchener, H.C. Future acceptance of adolescent human papillomavirus vaccination: A survey of parental attitudes. Vaccine 2006, 24, 3087–3094. [Google Scholar] [CrossRef]
- Jolley, D.; Douglas, K.M. The social consequences of conspiracism: Exposure to conspiracy theories decreases intentions to engage in politics and to reduce one’s carbon footprint. Br. J. Psychol. 2014, 105, 35–56. [Google Scholar] [CrossRef]
- Francis, J.; Eccles, M.P.; Johnston, M.; Walker, A.E.; Grimshaw, J.M.; Foy, R.; Kaner EF, S.; Smith, L.; Bonetti, D. Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Services Researchers; Centre for Health Services Research, University of Newcastle upon Tyne: Tyne, UK, 2004. [Google Scholar]
- Bollen, K.; Lennox, R. Conventional wisdom on measurement: A structural equation perspective. Psychol. Bull. 1991, 11, 305. [Google Scholar] [CrossRef]
- Hu, L.-T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods 1998, 3, 424. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Lockwood, C.M.; Williams, J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar. Behav. Res. 2004, 39, 99–128. [Google Scholar] [CrossRef] [Green Version]
- Bryant, F.B.; Satorra, A. Principles and practice of scaled difference chi-square testing. Struct. Equ. Model. A Multidiscip. J. 2012, 19, 372–398. [Google Scholar] [CrossRef]
- Hayes, A.F. Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Commun. Monogr. 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Rucker, D.D.; Preacher, K.J.; Tormala, Z.L.; Petty, R. Mediation analysis in social psychology: Current practices and new recommendations. Soc. Pers. Psychol. Compass 2011, 5, 359–371. [Google Scholar] [CrossRef]
- Floyd, D.L.; Prentice-Dunn, S.; Rogers, R.W. A meta-analysis of research on protection motivation theory. J. Appl. Soc. Psychol. 2000, 30, 407–429. [Google Scholar] [CrossRef]
- Bish, A.; Michie, S. Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. Br. J. Health Psychol. 2010, 15, 797–824. [Google Scholar] [CrossRef] [Green Version]
- van der Weerd, W.; Timmermans, D.R.M.; Beaujean, D.J.M.A.; Oudhoff, J.; van Steenbergen, J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health 2011, 11, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Wise, T.; Zbozinek, T.D.; Michelini, G.; Hagan, C.C.; Mobbs, D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 2020, 7, 200742. [Google Scholar] [CrossRef]
- Thompson, R.N. Novel Coronavirus Outbreak in Wuhan, China, 2020: Intense surveillance is vital for preventing sustained transmission in new locations. J. Clin. Med. 2020, 9, 498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sobkow, A.; Zaleskiewicz, T.; Petrova, D.; Garcia-Retamero, R.; Traczyk, J. Worry, Risk Perception, and Controllability Predict Intentions Toward COVID-19 Preventive Behaviors. Front. Psychol. 2020, 11, 582720. [Google Scholar] [CrossRef] [PubMed]
- Lipschitz, D.L.; Kuhn, R.; Kinney, A.Y.; Donaldson, G.W.; Nakamura, Y. Reduction in salivary α-amylase levels following a mind–body intervention in cancer survivors—An exploratory study. Psychoneuroendocrinology 2013, 38, 1521–1531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, H.; Liu, S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Educ. Couns. 2021, 104, 1878–1886. [Google Scholar] [CrossRef] [PubMed]
- Henrich, N.; Holmes, B. The public’s acceptance of novel vaccines during a pandemic: A focus group study and its application to influenza H1N1. Emerg. Health Threat. J. 2009, 2, 7088. [Google Scholar] [CrossRef]
- Cordina, M.; Lauri, M.A.; Lauri, J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm. Pract. (Granada) 2021, 19, 2317. [Google Scholar] [CrossRef]
- Zhou, M.; Zhao, L.; Kong, N.; Campy, K.S.; Qu, S.; Wang, S. Factors influencing behavior intentions to telehealth by Chinese elderly: An extended TAM model. Int. J. Med Inform. 2019, 126, 118–127. [Google Scholar] [CrossRef]
- Gangarosa, E.; Galazka, A.; Wolfe, C.; Phillips, L.; Miller, E.; Chen, R. Impact of anti-vaccine movements on pertussis control: The untold story. Lancet 1998, 351, 356–361. [Google Scholar] [CrossRef]
- Sunstein, C.R.; Vermeule, A. Conspiracy Theories; Harvard Law School: Cambridge, MA, USA, 2008. [Google Scholar]
- Reuben, R.; Aitken, D.; Freedman, J.L.; Einstein, G. Mistrust of the medical profession and higher disgust sensitivity predict parental vaccine hesitancy. PLoS ONE 2020, 15, e0237755. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Danis, K.; Georgakopoulou, T.; Stavrou, T.; Laggas, D.; Panagiotopoulos, T. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: A cross-sectional study in Greece. Vaccine 2010, 28, 1861–1869. [Google Scholar] [CrossRef]
- Sondagar, C.; Xu, R.; MacDonald, N.E.; Dubé, E. Nosocomial infection surveillance: Vaccine acceptance: How to build and maintain trust in immunization. Can. Commun. Dis. Rep. 2020, 46, 155. [Google Scholar] [CrossRef] [PubMed]
- van Prooijen, J.-W.; Kuijper, S.M. A comparison of extreme religious and political ideologies: Similar worldviews but different grievances. Personal. Individ. Differ. 2020, 159, 109888. [Google Scholar] [CrossRef]
- Green, R.; Douglas, K.M. Anxious attachment and belief in conspiracy theories. Pers. Individ. Differ. 2018, 125, 30–37. [Google Scholar] [CrossRef]
- Li, X.-H.; Chen, L.; Pan, Q.-N.; Liu, J.; Zhang, X.; Yi, J.-J.; Chen, C.-M.; Luo, Q.-H.; Tao, P.-Y.; Pan, X.; et al. Vaccination status, acceptance, and knowledge toward a COVID-19 vaccine among healthcare workers: A cross-sectional survey in China. Hum. Vaccines Immunother. 2021, 17, 4065–4073. [Google Scholar] [CrossRef] [PubMed]
- Freimuth, V.S.; Musa, D.; Hilyard, K.; Quinn, S.C.; Kim, K. Trust during the early stages of the 2009 H1N1 pandemic. J. Health Commun. 2013, 19, 321–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mesch, G.S.; Schwirian, K.P. Social and political determinants of vaccine hesitancy: Lessons learned from the H1N1 pandemic of 2009-2010. Am. J. Infect. Control 2015, 43, 1161–1165. [Google Scholar] [CrossRef] [PubMed]
- Myers, L.B.; Goodwin, R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health 2011, 11, 15. [Google Scholar] [CrossRef] [Green Version]
- Determann, D.; de Bekker-Grob, E.W.; French, J.; Voeten, H.A.; Richardus, J.H.; Das, E.; Korfage, I.J. Future pandemics and vaccination: Public opinion and attitudes across three European countries. Vaccine 2016, 34, 803–808. [Google Scholar] [CrossRef] [Green Version]
- Börjesson, M.; Enander, A. Perceptions and sociodemographic factors influencing vaccination uptake and precautionary behaviours in response to the A/H1N1 influenza in Sweden. Scand. J. Public Health 2013, 42, 215–222. [Google Scholar] [CrossRef]
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014, 112, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubé, E.; Gagnon, D.; Macdonald, N.; Bocquier, A.; Peretti-Watel, P.; Verger, P. Underlying factors impacting vaccine hesitancy in high income countries: A review of qualitative studies. Expert Rev. Vaccines 2018, 17, 989–1004. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M.; Omer, S.B.; Bednarczyk, R.A.; Halsey, N.A.; Moulton, L.H.; Salmon, D.A. Parents’ source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv. Prev. Med. 2012, 2012, 932741. [Google Scholar] [CrossRef] [PubMed]
- Caso, D.; Carfora, V.; Starace, C.; Conner, M. Key factors influencing italian mothers’ intention to vaccinate sons against hpv: The influence of trust in health authorities, anticipated regret and past behaviour. Sustainability 2019, 11, 6879. [Google Scholar] [CrossRef] [Green Version]
- Azjen, I. Understanding Attitudes and Predicting Social Behavior; University of Michigan: Ann Arbor, MI, USA, 1980. [Google Scholar]
- Majid, U.; Ahmad, M. The factors that promote vaccine hesitancy, rejection, or delay in parents. Qual. Health Res. 2020, 30, 1762–1776. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Frequency | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 310 | 68.3 |
| Female | 144 | 31.7 |
| Parent’s Education | ||
| High School | 38 | 8.4 |
| College and Diploma | 14 | 3.1 |
| Graduation | 117 | 25.8 |
| Masters | 249 | 54.8 |
| No. of Kids | ||
| 1–2 | 294 | 64.8 |
| 3–5 | 119 | 26.2 |
| 6–8 | 32 | 7 |
| More then 8 | 9 | 2 |
| Kid’s Age | ||
| Less than one year | 105 | 23.1 |
| 1–3 year | 144 | 31.7 |
| 4–6 year | 90 | 19.8 |
| 7–9 year | 55 | 12.1 |
| Parent’s Income (Annual) | ||
| $1000–10,000 | 380 | 83.7 |
| $11,000–15,000 | 13 | 7.7 |
| $16,000–20,000 | 35 | 5.7 |
| Above $20,000 | 26 | 2.9 |
| Parent’s Profession | ||
| Educationist | 99 | 21.8 |
| HCWs | 36 | 7.9 |
| Engineers | 154 | 33.9 |
| Govt. Employee | 52 | 11.4 |
| Manager | 54 | 11.9 |
| Others | 38 | 8.4 |
| Urbanicity | ||
| Rural | 128 | 28.2 |
| Urban | 326 | 71.8 |
| Religion | ||
| Islam | 441 | 97.1 |
| Christian | 7 | 1.5 |
| Others | 6 | 1.3 |
| Past Vaccine Experience | ||
| Yes | 291 | 64.2 |
| No | 163 | 35.8 |
| Construct | Items | Loadings | CA |
|---|---|---|---|
| Parental Vaccine Intention (PVI) | PIV1 | 0.73 | 0.845 |
| PIV2 | 0.692 | ||
| PIV3 | 0.643 | ||
| PIV4 | 0.744 | ||
| Conspiracy Belief (CB) | CB2 | 0.725 | 0.908 |
| CB3 | 0.739 | ||
| CB4 | 0.909 | ||
| CB6 | 0.886 | ||
| CB7 | 0.73 | ||
| CB9 | 0.79 | ||
| CB10 | 0.874 | ||
| CB11 | 0.779 | ||
| Risk Perception(RP) | RP1 | 0.715 | 0.958 |
| RP2 | 0.744 | ||
| RP3 | 0.846 | ||
| RP4 | 0.894 | ||
| RP5 | 0.93 | ||
| RP6 | 0.962 | ||
| RP7 | 0.985 | ||
| Vaccine Knowledge(VK) | VK2 | 0.752 | 0.902 |
| VK3 | 0.889 | ||
| VK4 | 0.925 | ||
| VK5 | 0.894 | ||
| VK6 | 0.679 | ||
| Vaccine Safety Concerns(VS) | VS1 | 0.898 | 0.875 |
| VS2 | 0.914 | ||
| VS3 | 0.748 | ||
| VS4 | 0.664 | ||
| Mistrust in Science(MTS) | MTS1 | 0.539 | 0.710 |
| MTS2 | 0.673 | ||
| MTS3 | 0.797 | ||
| MTS4 | 0.847 | ||
| MTS5 | 0.597 | ||
| Perceived Vaccine Self Efficacy(PVSE) | PVSE1 | 0.865 | 0.745 |
| PVSE2 | 0.968 | ||
| PVSE3 | 0.904 | ||
| PVSE4 | 0.623 |
| . | CR | AVE | CB | VK | VS | RP | PIV | PVSE | MTS |
|---|---|---|---|---|---|---|---|---|---|
| CB | 0.942 | 0.700 | 0.837 | ||||||
| VK | 0.904 | 0.653 | −0.067 | 0.808 | |||||
| VS | 0.880 | 0.652 | −0.054 | 0.552 *** | 0.807 | ||||
| RP | 0.943 | 0.808 | −0.729 *** | 0.025 | 0.010 | 0.899 | |||
| PIV | 0.860 | 0.615 | −0.125 * | 0.364 *** | −0.218 *** | −0.170 *** | 0.784 | ||
| PVSE | 0.753 | 0.680 | −0.030 | −0.154 ** | −0.191 *** | −0.076 | 0.131 * | 0.728 | |
| MTS | 0.724 | 0.64 | 0.089† | −0.270 *** | −0.153 ** | −0.046 | 0.193 *** | 0.090 | 0.696 |
| RP | CB | MTS | VK | VS | PVSE | PIV | |
|---|---|---|---|---|---|---|---|
| RP | 1 | ||||||
| CB | 0.654 ** | 1 | |||||
| MTS | 0.283 *** | 0.382 * | 1 | ||||
| VK | −0.365 * | -0.25 ** | −0.208 ** | 1 | |||
| VS | 0.329 * | 0.42 ** | 0.105 * | −0.459 ** | 1 | ||
| PVSE | −0.488 * | -0.426 ** | −0.288 | 0.437 ** | 0.354 ** | 1 | |
| PIV | −0.451 ** | -0.495 *** | −0.324 ** | 0.520 ** | −0.218 ** | 0.487 ** | 1 |
| Direct Effect | Beta | SE | CR | p-Value |
|---|---|---|---|---|
| CB→PIV | −0.452 | 0.042 | 2.967 | 0.01 ** |
| PVSE→PIV | 0.368 | 0.041 | 1.969 | 0.090 |
| VS→PIV | −0.233 | 0.046 | 2.889 | 0.075 |
| RP→PIV | 0.241 | 0.056 | 4.135 | 0.005 * |
| VK→PIV | 0.522 | 0.055 | 14.343 | *** |
| MTS→PIV | −0.151 | 0.056 | 4.135 | *** |
| Total Effect | Direct Effect | Indirect Effects | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Beta | p-Value | Beta(β) | p-Value | Beta (β) | p-Value | CI 95% | Decision | ||
| CB→PIV | −0.475 | 0.046 * | −0.192 | 0.073 | CB →VK→PIV | −0.283 | 0.002 ** | [−0.127,−0.06] | Full |
| PVSE→PIV | 0.261 | 0.002 ** | 0.102 | 0.006 ** | PVSE→VK→PIV | 0.159 | 0.015 * | [0.099,0.234] | partial |
| VS→PIV | −0.226 | 0.002 ** | −0.206 | 0.001 *** | VS→VK→PIV | −0.020 | 0.619 | [−0.063,0.019] | No medition |
| RP→PIV | 0.137 | 0.014 ** | 0.097 | 0.100 | RP→VK→PIV | 0.088 | 0.002 ** | [0.042,0.139] | Full |
| CB→PIV | 0.215 | 0.038 * | 0.074 | 0.059 | CB→MTS→PIV | 0.1419 | 0.031 * | [0.02,0.263] | Full |
| PVSE→PIV | 0.275 | 0.002 ** | 0.173 | 0.002 ** | PVSE→MTS→PIV | 0.102 | 0.110 | [−0.245,0.356] | No medition |
| VS→PIV | −0.205 | 0.001 *** | −0.195 | 0.002 ** | VS→MTS→PIV | −0.010 | 0.047 * | [−0.341,−0.031] | Partial |
| RP→PIV | −0.149 | 0.011 ** | −0.138 | 0.014 ** | RP→MTS→PIV | −0.0112 | 0.042 * | [−0.36,−0.062] | Partial |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahani, R.; Chu, J.; Rufai, O.H.; Zawar, A.; Muhideen, S.; Dilawar, S.; Amosun, T.S. Understanding the Role of Psychosocial Factors in Pakistani Parents’ Hesitancy to Vaccinate Their Kids: The Mediating Role of Knowledge and Mistrust of Science about the COVID-19 Vaccine. Vaccines 2022, 10, 1260. https://doi.org/10.3390/vaccines10081260
Shahani R, Chu J, Rufai OH, Zawar A, Muhideen S, Dilawar S, Amosun TS. Understanding the Role of Psychosocial Factors in Pakistani Parents’ Hesitancy to Vaccinate Their Kids: The Mediating Role of Knowledge and Mistrust of Science about the COVID-19 Vaccine. Vaccines. 2022; 10(8):1260. https://doi.org/10.3390/vaccines10081260
Chicago/Turabian StyleShahani, Riffat, Jianxun Chu, Olayemi Hafeez Rufai, Asma Zawar, Sayibu Muhideen, Sana Dilawar, and Tunde Simeon Amosun. 2022. "Understanding the Role of Psychosocial Factors in Pakistani Parents’ Hesitancy to Vaccinate Their Kids: The Mediating Role of Knowledge and Mistrust of Science about the COVID-19 Vaccine" Vaccines 10, no. 8: 1260. https://doi.org/10.3390/vaccines10081260
APA StyleShahani, R., Chu, J., Rufai, O. H., Zawar, A., Muhideen, S., Dilawar, S., & Amosun, T. S. (2022). Understanding the Role of Psychosocial Factors in Pakistani Parents’ Hesitancy to Vaccinate Their Kids: The Mediating Role of Knowledge and Mistrust of Science about the COVID-19 Vaccine. Vaccines, 10(8), 1260. https://doi.org/10.3390/vaccines10081260






