Attitudes towards Vaccines, Intent to Vaccinate and the Relationship with COVID-19 Vaccination Rates in Individuals with Schizophrenia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Assessments
2.3. Procedure
2.4. Statistical Analysis
3. Results
3.1. Preliminary Analyses
3.2. Demographic Variables
3.3. Clinical and Cognitive Assessments
3.4. Vaccination Status, Health-Related Indicators, and Intention to Vaccinate
3.5. Vaccination Status, Demographic Variables, Health-Related Indicators, and Clinical and Cognitive Assessments
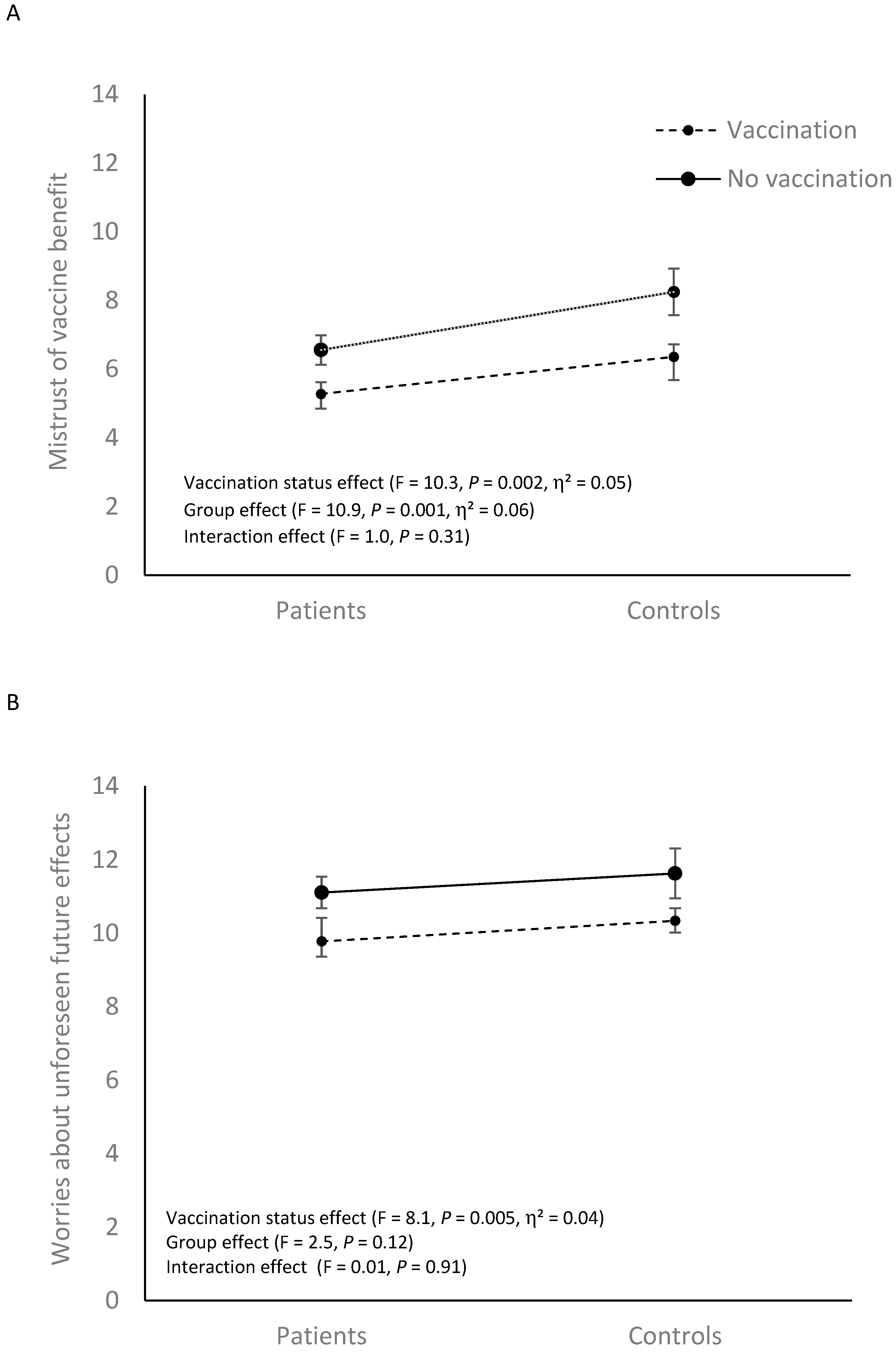
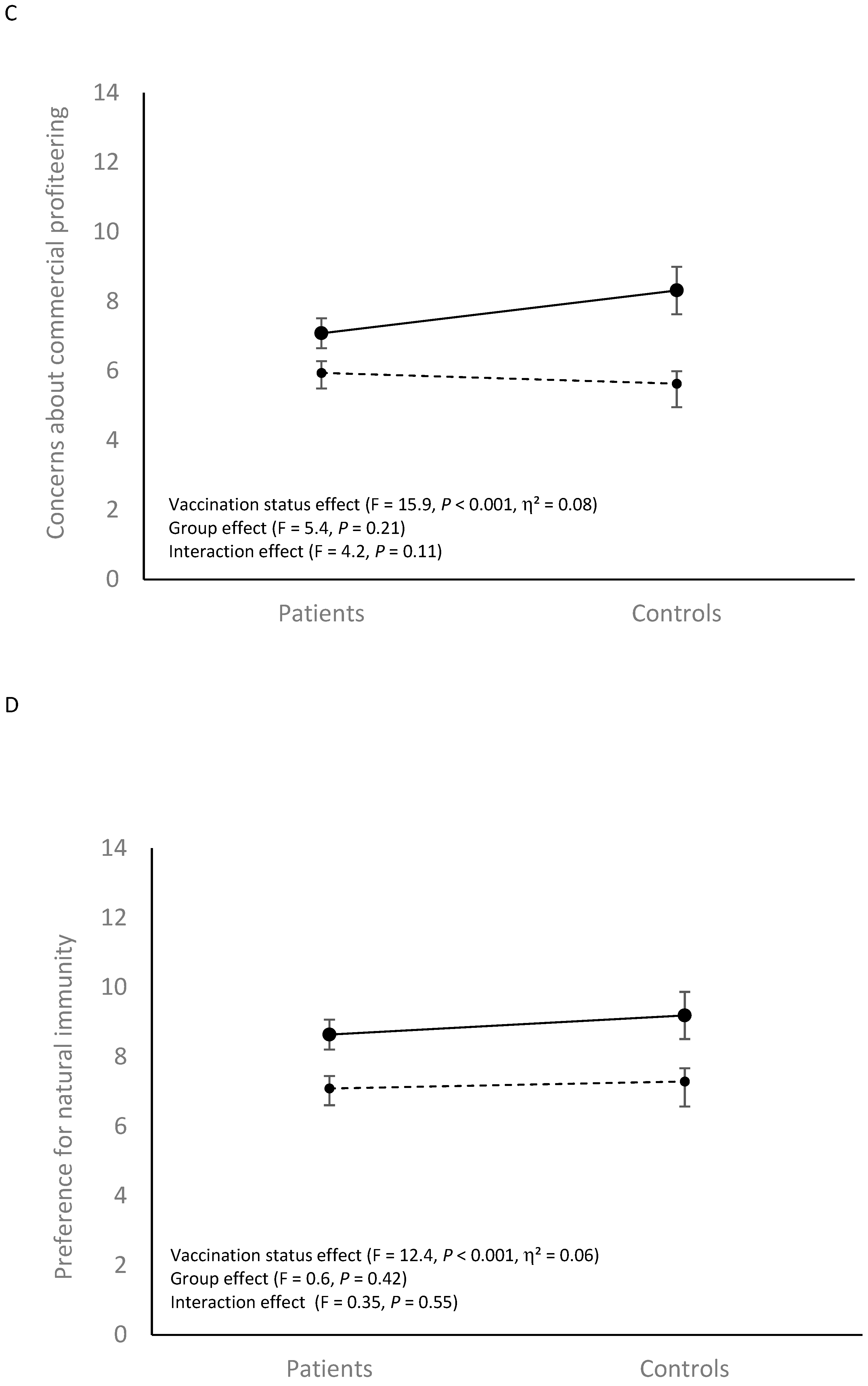
3.6. Vaccination Status, Attitudes towards Vaccines, Trust in Institutions, and COVID-19 Related Questionnaires
3.7. Associations between Attitudes towards Vaccines, COVID-19 Related Questionnaires, Demographic Variables, Health-Related Indicators, and Clinical and Cognitive Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bitan, D.T.; Krieger, I.; Kridin, K.; Komantscher, D.; Scheinman, Y.; Weinstein, O.; Cohen, A.D.; Cicurel, A.A.; Feingold, D. COVID-19 Prevalence and Mortality Among Schizophrenia Patients: A Large-Scale Retrospective Cohort Study. Schizophr. Bull. 2021, 47, 1211–1217. [Google Scholar] [CrossRef] [PubMed]
- Fond, G.; Pauly, V.; Leone, M.; Llorca, P.M.; Orleans, V.; Loundou, A.; Lancon, C.; Auquier, P.; Baumstarck, K.; Boyer, L. Disparities in Intensive Care Unit Admission and Mortality among Patients with Schizophrenia and COVID-19: A National Cohort Study. Schizophr. Bull. 2021, 47, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.L.; Kwon, J.S.; Park, S.H.; Shin, J.Y. Association of mental disorders with SARS-CoV-2 infection and severe health outcomes: Nationwide cohort study. Br. J. Psychiatry 2021, 218, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Xu, R.; Volkow, N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States. World Psychiatry 2021, 20, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Warren, N.; Kisely, S.; Siskind, D. Maximising the uptake of a COVID-19 vaccine in people with severe mental illness: A public health priority. JAMA Psychiatry 2020, 78, 589–590. [Google Scholar] [CrossRef] [PubMed]
- Hassan, L.; Sawyer, C.; Peek, N.; Lovell, K.; Carvalho, A.F.; Solmi, M.; Tilston, G.; Sperrin, M.; Firth, J. COVID-19 vaccination uptake in people with severe mental illness: A UK-based cohort study. World Psychiatry 2022, 21, 153–154. [Google Scholar] [CrossRef]
- Bitan, D.T.; Kridin, K.; Cohen, A.D.; Weinstein, O. COVID-19 hospitalisation, mortality, vaccination, and postvaccination trends among people with schizophrenia in Israel: A longitudinal cohort study. Lancet Psychiatry 2021, 8, 901–908. [Google Scholar] [CrossRef]
- Lorenz, R.A.; Norris, M.M.; Norton, L.C.; Westrick, S.C. Factors associated with influenza vaccination decisions among patients with mental illness. Int. J. Psychiatry Med. 2013, 46, 1–13. [Google Scholar] [CrossRef]
- Miles, L.W.; Williams, N.; Luthy, K.E.; Eden, L. Adult Vaccination Rates in the Mentally Ill Population: An Outpatient Improvement Project. J. Am. Psychiatr. Nurses Assoc. 2020, 26, 172–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Fisk, R.J. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: Experience from the United States. Glob Health J. 2021, 5, 51–55. [Google Scholar] [CrossRef]
- Breckler, S.J. Empirical validation of affect, behavior, and cognition as distinct components of attitude. J. Personal. Soc. Psychol. 1984, 47, 1191–1205. [Google Scholar] [CrossRef]
- Chaiklin, H. Attitudes, behavior, and social practice. J. Soc. Soc. Welfare 2011, 38, 31. [Google Scholar]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- Martin LRPetrie, K.J. Understanding the Dimensions of Anti-Vaccination Attitudes: The Vaccination Attitudes Examination (VAX) Scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef]
- Freeman, D.; Waite, F.; Rosebrock, L.; Petit, A.; Causier, C.; East, A.; Jenner, L.; Teale, A.L.; Carr, L.; Mulhall, S.; et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. 2020, 21, 1–13. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Raffard, S.; Bayard, S.; Eisenblaetter, M.; Tattard, P.; Attal, J.; Laraki, Y.; Capdevielle, D. Mental capacity to consent to COVID 19 vaccination in individuals with schizophrenia: An explorative study (submitted for publication). Diminished capacity to make treatment decision for COVID-19 vaccination in schizophrenia. Eur. Arch Psychiatry Clin. Neurosci. 2022, in press. [Google Scholar] [CrossRef]
- Maguire, P.A.; Reay, R.E.; Looi, J.C. Nothing to sneeze at—Uptake of protective measures against an influenza pandemic by people with schizophrenia: Willingness and perceived barriers. Australas Psychiatry 2019, 27, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Hao, F.; Wang, B.; Tan, W.; Husain, S.F.; McIntyre, R.S.; Tang, X.; Zhang, L.; Han, X.; Jiang, L.; Chew, N.W.S.; et al. Attitudes toward COVID-19 vaccination and willingness to pay: Comparison of people with and without mental disorders in China. BJPsych Open. 2021, 7, e146. [Google Scholar] [CrossRef]
- Danenberg, R.; Shemesh, S.; Tzur Bitan, D.; Maoz, H.; Saker, T.; Dror, C.; Hertzberg, L.; Bloch, Y. Attitudes of patients with severe mental illness towards COVID-19 vaccinations: A preliminary report from a public psychiatric hospital. J. Psychiatr. Res. 2021, 143, 16–20. [Google Scholar] [CrossRef]
- Bai, W.; Cai, H.; Jin, Y.; Zhang, Q.; Cheung, T.; Su, Z.; Tang, Y.L.; Ng, C.H.; Xiang, Y.T. COVID-19 vaccine hesitancy in community-dwelling and hospitalized patients with severe mental illness. Psychol. Med. 2021, 17, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Mazereel, V.; Van Assche, K.; Detraux, J.; De Hert, M. COVID-19 vaccination for people with severe mental illness: Why, what, and how? Lancet Psychiatry 2021, 8, 860–861. [Google Scholar] [CrossRef]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.; Verkuilen, J. Green et al. Paranoid Thoughts Scale: French validation and development of a brief version. Personal. Individ. Differ. 2021, 171, 110554. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Eisenblaetter, M.; Madiouni, C.; Laraki, Y.; Capdevielle, D.; Raffard, S. French validation of the Vaccination Attitudes Examination (VAX) Scale. Vaccine 2022. submitted for publication. [Google Scholar]
- Weston, R.; Gore, P.A., Jr. A brief guide to structural equation modeling. Couns. Psychol. 2006, 34, 719–751. [Google Scholar] [CrossRef]
- Tabachnik, B.G.; Fidell, S.L. Multicollinearity and singularity. In Using Multivariate Statistics; Pearson Education Inc.: Boston, MA, USA, 2013; Volume 2, pp. 88–91. [Google Scholar]
- Suhas, S. COVID-19 vaccination of persons with schizophrenia in India—Need for imperative action! Schizophr. Res. 2021, 231, 49–50. [Google Scholar] [CrossRef]
- Stead, M.; Jessop, C.; Angus, K.; Bedford, H.; Ussher, M.; Ford, A.; Eadie, D.; MacGregor, A.; Hunt, K.; MacKintosh, A.M. National survey of attitudes towards and intentions to vaccinate against COVID-19: Implications for communications. BMJ Open 2021, 11, e055085. [Google Scholar] [CrossRef]
- Jefsen, O.H.; Kølbæk, P.; Gil, Y.; Speed, M.; Dinesen, P.T.; Sønderskov, K.M.; Østergaard, S.D. COVID-19 vaccine willingness amongst patients with mental illness compared with the general population. Acta Neuropsychiatr. 2021, 33, 273–276. [Google Scholar] [CrossRef]
- Al Shurman, B.A.; Khan, A.F.; Mac, C.; Majeed, M.; Butt, Z.A. What Demographic, Social, and Contextual Factors Influence the Intention to Use COVID-19 Vaccines: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 9342. [Google Scholar] [CrossRef]
- Robinson, E.; Jones, A.; Lesser, I.; Daly, M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 2021, 39, 2024–2034. [Google Scholar] [CrossRef] [PubMed]
- Njoku, A.; Joseph, M.; Felix, R. Changing the Narrative: Structural Barriers and Racial and Ethnic Inequities in COVID-19 Vaccination. Int. J. Environ. Res. Public Health 2021, 18, 9904. [Google Scholar] [CrossRef] [PubMed]
- Seminog, O.O.; Goldacre, M.J. Risk of pneumonia and pneumococcal disease in people with severe mental illness: English record linkage studies. Thorax 2013, 68, 171–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Q.; Yue, N.; Zheng, M.; Wang, D.; Duan, C.; Yu, X.; Zhang, X.; Bao, C.; Jin, H. Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: A meta-analysis. Vaccine 2018, 36, 7262–7269. [Google Scholar] [CrossRef]
- Cordina, M.; Lauri, M.A.; Lauri, J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm. Pract. 2021, 19, 2317. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Fervaha, G.; Foussias, G.; Agid, O.; Remington, G. Impact of primary negative symptoms on functional outcomes in schizophrenia. Eur. Psychiatry 2014, 29, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Kerr, J.R.; Schneider, C.R.; Recchia, G.; Dryhurst, S.; Sahlin, U.; Dufouil, C.; Arwidson, P.; Freeman, A.L.; van der Linden, S. Correlates of intentedCOVID-19 vaccine acceptance across time and countries: Results from a series of cross-sectional surveys. BMJ Open 2021, 11, e048025. [Google Scholar] [CrossRef]
- Santirocchi, A.; Spataro, P.; Costanzi, M.; Doricchi, F.; Rossi-Arnaud, C.; Cestari, V. Predictors of the Intention to Be Vaccinated against COVID-19 in a Sample of Italian Respondents at the Start of the Immunization Campaign. J. Pers. Med. 2022, 12, 111. [Google Scholar] [CrossRef]
- Viswanath, K.; Bekalu, M.; Dhawan, D.; Pinnamaneni, R.; Lang, J.; McLoud, R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health 2021, 21, 818. [Google Scholar] [CrossRef] [PubMed]
- Veerman, S.R.T.; Moscou, T.; Bogers, J.P.A.M.; Cohen, D.; Schulte, P.F.J. Clozapine and COVID-19 Vaccination: Effects on blood levels and leukocytes. An observational cohort study. Acta Psychiatr. Scand. 2022, 146, 168–178. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; Mazereel, V.; Detraux, J.; Van Assche, K. Prioritising COVID-19 vaccination for people with severe mental illness. World Psychiatry 2021, 20, 54–55. [Google Scholar] [CrossRef] [PubMed]
- Mazereel, V.; Vanbrabant, T.; Desplenter, F.; De Hert, M. COVID-19 vaccine uptake in patients with psychiatric disorders admitted to or residing in a university psychiatric hospital. Lancet Psychiatry 2021, 8, 860–861. [Google Scholar] [CrossRef]
| Patients | Controls | Statistics | p-Value | |
|---|---|---|---|---|
| N (%)/mean (SD) | N = 100 | N = 72 | ||
| Demographic variables | ||||
| Age | 40.6 (12.4) | 32.7 (12.6) | t = −4.09 | <0.001 |
| Gender, female | 37.50% | 26% | χ2 = 2.09 | 0.15 |
| Years of scholarship, mean | 12.7 (2.7) | 14.1 (2.2) | t = 3.76 | <0.001 |
| Clinical and cognitive assessments | ||||
| Patients under treatment | 100% | |||
| Duration of the disease | 16.5 (11.3) | |||
| PANSS total | 63.9 (17.7) | |||
| PANSS positive | 13.7 (5.7) | |||
| PANSS negative | 16.8 (5.6) | |||
| PANSS general psychopathology | 33.2 (8.5) | |||
| Green Paranoid Thoughts Scale | 16.1 (8.6) | 13.4 (6.9) | t = −2.16 | 0.02 |
| Montreal Cognitive Assessment | 23.9 (4.1) | 27.1 (2.4) | t = 6.33 | <0.001 |
| Vaccination status and health-related indicators | ||||
| COVID-19 vaccination, yes | 64% | 77.80% | χ2 = 3.14 | 0.07 |
| COVID-19 infection, yes | 15% | 23.60% | χ2 = 2.1 | 0.15 |
| Underlying health condition, yes | 22% | 8.30% | χ2 = 5.74 | 0.01 |
| Intend to take a COVID-19 vaccine 1 | 41.7%% | 12.50% | χ2 = 4.28 | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raffard, S.; Bayard, S.; Eisenblaetter, M.; Attal, J.; Andrieu, C.; Chereau, I.; Fond, G.; Leignier, S.; Mallet, J.; Tattard, P.; et al. Attitudes towards Vaccines, Intent to Vaccinate and the Relationship with COVID-19 Vaccination Rates in Individuals with Schizophrenia. Vaccines 2022, 10, 1228. https://doi.org/10.3390/vaccines10081228
Raffard S, Bayard S, Eisenblaetter M, Attal J, Andrieu C, Chereau I, Fond G, Leignier S, Mallet J, Tattard P, et al. Attitudes towards Vaccines, Intent to Vaccinate and the Relationship with COVID-19 Vaccination Rates in Individuals with Schizophrenia. Vaccines. 2022; 10(8):1228. https://doi.org/10.3390/vaccines10081228
Chicago/Turabian StyleRaffard, Stéphane, Sophie Bayard, Margot Eisenblaetter, Jérôme Attal, Christelle Andrieu, Isabelle Chereau, Guillaume Fond, Sylvain Leignier, Jasmina Mallet, Philippe Tattard, and et al. 2022. "Attitudes towards Vaccines, Intent to Vaccinate and the Relationship with COVID-19 Vaccination Rates in Individuals with Schizophrenia" Vaccines 10, no. 8: 1228. https://doi.org/10.3390/vaccines10081228
APA StyleRaffard, S., Bayard, S., Eisenblaetter, M., Attal, J., Andrieu, C., Chereau, I., Fond, G., Leignier, S., Mallet, J., Tattard, P., Urbach, M., Misdrahi, D., Laraki, Y., & Capdevielle, D. (2022). Attitudes towards Vaccines, Intent to Vaccinate and the Relationship with COVID-19 Vaccination Rates in Individuals with Schizophrenia. Vaccines, 10(8), 1228. https://doi.org/10.3390/vaccines10081228









