Evaluation of Safety and Immunogenicity of BNT162B2 mRNA COVID-19 Vaccine in IBD Pediatric Population with Distinct Immune Suppressive Regimens
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Safety
2.3. Sample Collection and Storage
2.4. Humoral Response
2.5. Quantification and Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Safety of 2 Doses of BNT162B2 mRNA COVID-19 Vaccine
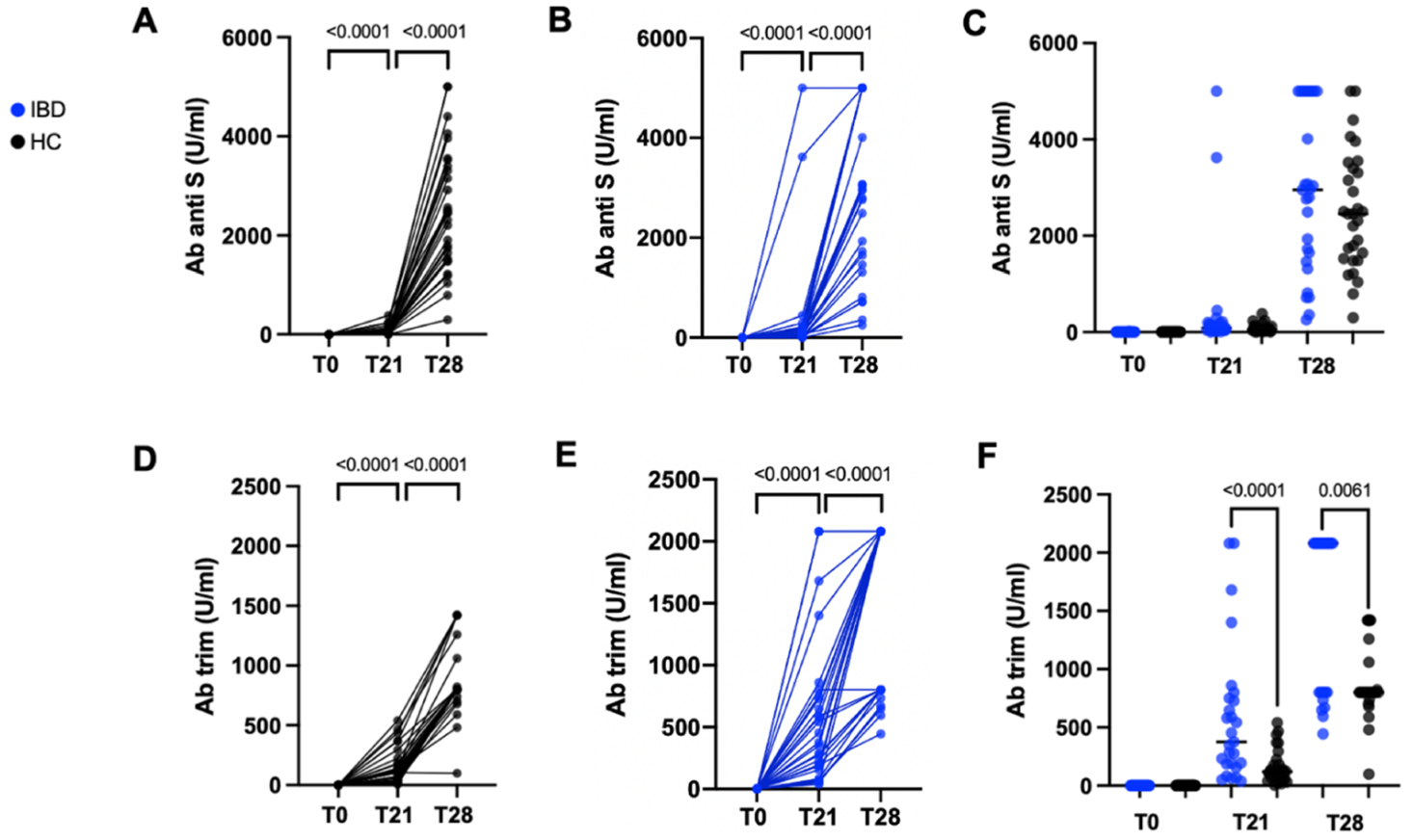
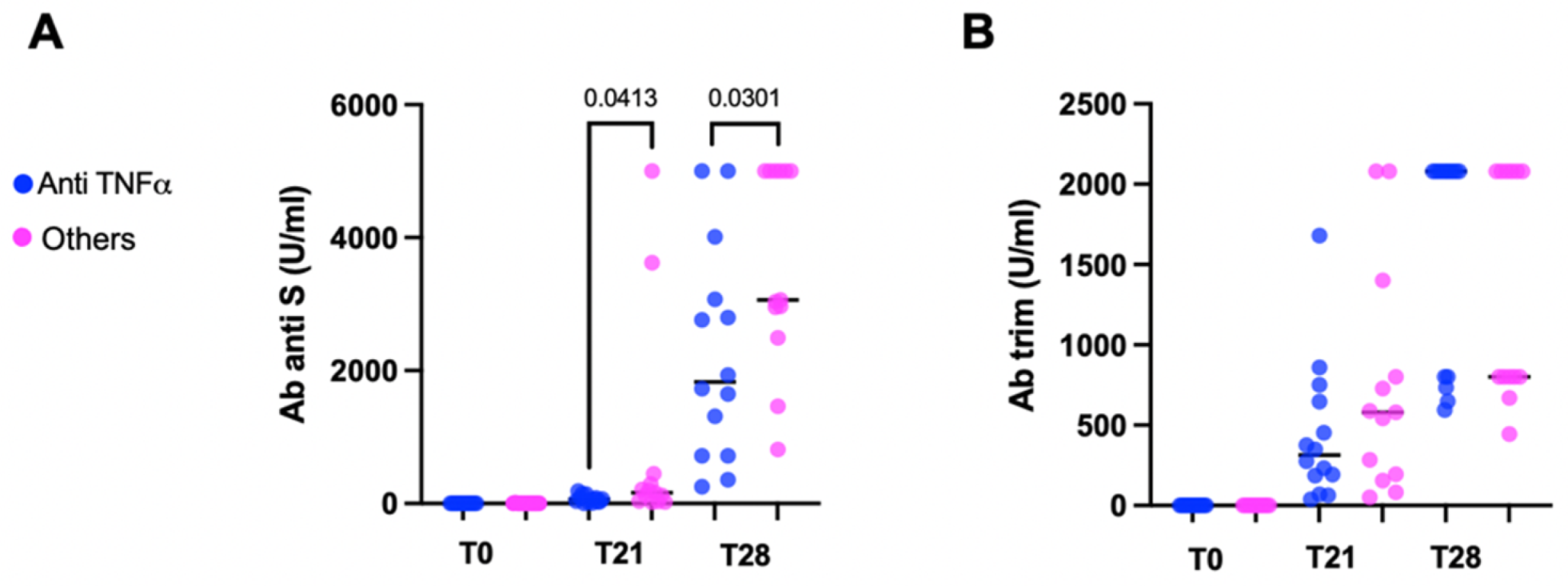
3.3. Serologic Response
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alatab, S.; Sepanlou, S.G.; Ikuta, K.; Vahedi, H.; Bisignano, C.; Safiri, S.; Sadeghi, A.; Nixon, M.R.; Abdoli, A.; Abolhassani, H.; et al. The Global, Regional, and National Burden of Inflammatory Bowel Disease in 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, S.B.; Monteiro, I.M. Diagnosis and Management of Inflammatory Bowel Disease in Children. BMJ 2017, 357, j2083. [Google Scholar] [CrossRef] [PubMed]
- Desalermos, A.; Pimienta, M.; Kalligeros, M.; Shehadeh, F.; Diamantopoulos, L.; Karamanolis, G.; Caldera, F.; Farraye, F.A. Safety of Immunizations for the Adult Patient with Inflammatory Bowel Disease—A Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2021, izab266. [Google Scholar] [CrossRef] [PubMed]
- Pratt, P.K.; David, N.; Weber, H.C.; Little, F.F.; Kourkoumpetis, T.; Patts, G.J.; Weinberg, J.; Farraye, F.A. Antibody Response to Hepatitis B Virus Vaccine Is Impaired in Patients with Inflammatory Bowel Disease on Infliximab Therapy. Inflamm. Bowel Dis. 2018, 24, 380–386. [Google Scholar] [CrossRef] [Green Version]
- Fiorino, G.; Peyrin-Biroulet, L.; Naccarato, P.; Szabò, H.; Sociale, O.R.; Vetrano, S.; Fries, W.; Montanelli, A.; Repici, A.; Malesci, A.; et al. Effects of Immunosuppression on Immune Response to Pneumococcal Vaccine in Inflammatory Bowel Disease: A Prospective Study. Inflamm. Bowel Dis. 2012, 18, 1042–1047. [Google Scholar] [CrossRef]
- Melmed, G.Y.; Agarwal, N.; Frenck, R.W.; Ippoliti, A.F.; Ibanez, P.; Papadakis, K.A.; Simpson, P.; Barolet-Garcia, C.; Ward, J.; Targan, S.R.; et al. Immunosuppression Impairs Response to Pneumococcal Polysaccharide Vaccination in Patients with Inflammatory Bowel Disease. Am. J. Gastroenterol. 2010, 105, 148–154. [Google Scholar] [CrossRef]
- Mamula, P.; Markowitz, J.E.; Piccoli, D.A.; Klimov, A.; Cohen, L.; Baldassano, R.N. Immune Response to Influenza Vaccine in Pediatric Patients with Inflammatory Bowel Disease. Clin. Gastroenterol. Hepatol. 2007, 5, 851–856. [Google Scholar] [CrossRef]
- Park, S.H.; Yang, S.-K.; Park, S.-K.; Kim, J.W.; Yang, D.-H.; Jung, K.W.; Kim, K.-J.; Ye, B.D.; Byeon, J.-S.; Myung, S.-J.; et al. Efficacy of Hepatitis A Vaccination and Factors Impacting on Seroconversion in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2014, 20, 69–74. [Google Scholar] [CrossRef]
- Hagihara, Y.; Ohfuji, S.; Watanabe, K.; Yamagami, H.; Fukushima, W.; Maeda, K.; Kamata, N.; Sogawa, M.; Shiba, M.; Tanigawa, T.; et al. Infliximab and/or Immunomodulators Inhibit Immune Responses to Trivalent Influenza Vaccination in Adults with Inflammatory Bowel Disease. J. Crohn’s Colitis 2014, 8, 223–233. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Jacobson, D.L.; Ashworth, L.A.; Grand, R.J.; Meyer, A.L.; McNeal, M.M.; Gregas, M.C.; Burchett, S.K.; Bousvaros, A. Immune Response to Influenza Vaccine in Children with Inflammatory Bowel Disease. Am. J. Gastroenterol. 2009, 104, 444–453. [Google Scholar] [CrossRef]
- Andrisani, G.; Frasca, D.; Romero, M.; Armuzzi, A.; Felice, C.; Marzo, M.; Pugliese, D.; Papa, A.; Mocci, G.; De Vitis, I.; et al. Immune Response to Influenza A/H1N1 Vaccine in Inflammatory Bowel Disease Patients Treated with Anti TNF-α Agents: Effects of Combined Therapy with Immunosuppressants. J. Crohn’s Colitis 2013, 7, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Cullen, G.; Bader, C.; Korzenik, J.R.; Sands, B.E. Serological Response to the 2009 H1N1 Influenza Vaccination in Patients with Inflammatory Bowel Disease. Gut 2012, 61, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, N.A.; Lin, S.; Goodhand, J.R.; Chanchlani, N.; Hamilton, B.; Bewshea, C.; Nice, R.; Chee, D.; Cummings, J.F.; Fraser, A.; et al. Infliximab Is Associated with Attenuated Immunogenicity to BNT162b2 and ChAdOx1 NCoV-19 SARS-CoV-2 Vaccines in Patients with IBD. Gut 2021, 70, 1884–1893. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.-Y.; Dixon, R.; Martinez Pazos, V.; Gnjatic, S.; Colombel, J.-F.; Cadwell, K.; Gold, S.; Helmus, D.; Neil, J.A.; Sota, S.; et al. Serologic Response to Messenger RNA Coronavirus Disease 2019 Vaccines in Inflammatory Bowel Disease Patients Receiving Biologic Therapies. Gastroenterology 2021, 161, 715–718e4. [Google Scholar] [CrossRef]
- Alexander, J.L.; Kennedy, N.A.; Ibraheim, H.; Anandabaskaran, S.; Saifuddin, A.; Castro Seoane, R.; Liu, Z.; Nice, R.; Bewshea, C.; D’Mello, A.; et al. COVID-19 Vaccine-Induced Antibody Responses in Immunosuppressed Patients with Inflammatory Bowel Disease (VIP): A Multicentre, Prospective, Case-Control Study. Lancet Gastroenterol. Hepatol. 2022, 7, 342–352. [Google Scholar] [CrossRef]
- Edelman-Klapper, H.; Zittan, E.; Bar-Gil Shitrit, A.; Rabinowitz, K.M.; Goren, I.; Avni-Biron, I.; Ollech, J.E.; Lichtenstein, L.; Banai-Eran, H.; Yanai, H.; et al. Lower Serologic Response to COVID-19 MRNA Vaccine in Patients with Inflammatory Bowel Diseases Treated with Anti-TNFα. Gastroenterology 2022, 162, 454–467. [Google Scholar] [CrossRef] [PubMed]
- Kappelman, M.D.; Weaver, K.N.; Zhang, X.; Dai, X.; Watkins, R.; Adler, J.; Dubinsky, M.C.; Kastl, A.; Bousvaros, A.; Strople, J.A.; et al. Factors Affecting Initial Humoral Immune Response to SARS-CoV-2 Vaccines Among Patients with Inflammatory Bowel Diseases. Am. J. Gastroenterol. 2022, 117, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Caldera, F.; Knutson, K.L.; Saha, S.; Wald, A.; Phan, H.S.; Chun, K.; Grimes, I.; Lutz, M.; Hayney, M.S.; Farraye, F.A. Humoral Immunogenicity of MRNA COVID-19 Vaccines Among Patients with Inflammatory Bowel Disease and Healthy Controls. Am. J. Gastroenterol. 2022, 117, 176–179. [Google Scholar] [CrossRef]
- Hindson, J. Immunosuppressive IBD Drugs and COVID-19 Vaccine Immunogenicity. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 216. [Google Scholar] [CrossRef]
- Frenck, R.W.; Klein, N.P.; Kitchin, N.; Gurtman, A.; Absalon, J.; Lockhart, S.; Perez, J.L.; Walter, E.B.; Senders, S.; Bailey, R.; et al. Safety, Immunogenicity, and Efficacy of the BNT162b2 COVID-19 Vaccine in Adolescents. N. Engl. J. Med. 2021, 385, 239–250. [Google Scholar] [CrossRef]
- Dailey, J.; Kozhaya, L.; Dogan, M.; Hopkins, D.; Lapin, B.; Herbst, K.; Brimacombe, M.; Grandonico, K.; Karabacak, F.; Schreiber, J.; et al. Antibody Responses to SARS-CoV-2 After Infection or Vaccination in Children and Young Adults with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2021, 28, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Spencer, E.A.; Klang, E.; Dolinger, M.; Pittman, N.; Dubinsky, M.C. Seroconversion Following SARS-CoV-2 Infection or Vaccination in Pediatric IBD Patients. Inflamm. Bowel Dis. 2021, 27, 1862–1864. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Huang, Y.; Martín-de-Carpi, J.; Aloi, M.; Focht, G.; Kang, B.; Zhou, Y.; Sanchez, C.; Kappelman, M.D.; Uhlig, H.H.; et al. Corona Virus Disease 2019 and Paediatric Inflammatory Bowel Diseases: Global Experience and Provisional Guidance (March 2020) from the Paediatric IBD Porto Group of European Society of Paediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Veereman, G.; Bronsky, J. Severe Acute Respiratory Syndrome Coronavirus 2 Vaccination for Paediatric Patients with Inflammatory Bowel Diseases. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 433–436. [Google Scholar] [CrossRef] [PubMed]
- Sahin, U.; Muik, A.; Vogler, I.; Derhovanessian, E.; Kranz, L.M.; Vormehr, M.; Quandt, J.; Bidmon, N.; Ulges, A.; Baum, A.; et al. BNT162b2 Vaccine Induces Neutralizing Antibodies and Poly-Specific T Cells in Humans. Nature 2021, 595, 572–577. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Zaffina, S.; Alteri, C.; Ruggiero, A.; Cotugno, N.; Vinci, M.R.; Camisa, V.; Santoro, A.P.; Brugaletta, R.; Deriu, G.; Piano Mortari, E.; et al. Induction of Immune Response after SARS-CoV-2 MRNA BNT162b2 Vaccination in Healthcare Workers. J. Virus Erad. 2021, 7, 100046. [Google Scholar] [CrossRef]
- Bridge, P.D.; Sawilowsky, S.S. Increasing Physicians’ Awareness of the Impact of Statistics on Research Outcomes: Comparative Power of the t-Test and and Wilcoxon Rank-Sum Test in Small Samples Applied Research. J. Clin. Epidemiol. 1999, 52, 229–235. [Google Scholar] [CrossRef]
- Ellul, P.; Revés, J.; Abreu, B.; Chaparro, M.; Gisbert, J.P.; Allocca, M.; Fiorino, G.; Barberio, B.; Zingone, F.; Pisani, A.; et al. Implementation and Short-Term Adverse Events of Anti-SARS-CoV-2 Vaccines in Inflammatory Bowel Disease Patients: An International Web-Based Survey. J. Crohn’s Colitis 2022, 16, i558. [Google Scholar] [CrossRef]
- Botwin, G.J.; Li, D.; Figueiredo, J.; Cheng, S.; Braun, J.; McGovern, D.P.B.; Melmed, G.Y. Adverse Events After SARS-CoV-2 MRNA Vaccination Among Patients with Inflammatory Bowel Disease. Am. J. Gastroenterol. 2021, 116, 1746. [Google Scholar] [CrossRef]
- Weaver, K.N.; Zhang, X.; Dai, X.; Watkins, R.; Adler, J.; Dubinsky, M.C.; Kastl, A.; Bousvaros, A.; Strople, J.A.; Cross, R.K.; et al. Impact of SARS-CoV-2 Vaccination on Inflammatory Bowel Disease Activity and Development of Vaccine-Related Adverse Events: Results From PREVENT-COVID. Inflamm. Bowel Dis. 2021, izab302. [Google Scholar] [CrossRef] [PubMed]
- Hadi, Y.B.; Thakkar, S.; Shah-Khan, S.M.; Hutson, W.; Sarwari, A.; Singh, S. COVID-19 Vaccination Is Safe and Effective in Patients with Inflammatory Bowel Disease: Analysis of a Large Multi-Institutional Research Network in the United States. Gastroenterology 2021, 161, 1336–1339.e3. [Google Scholar] [CrossRef] [PubMed]
- Lev-Tzion, R.; Focht, G.; Lujan, R.; Mendelovici, A.; Friss, C.; Greenfeld, S.; Kariv, R.; Ben-Tov, A.; Matz, E.; Nevo, D.; et al. COVID-19 Vaccine Is Effective in Inflammatory Bowel Disease Patients and Is Not Associated with Disease Exacerbation. Clin. Gastroenterol. Hepatol. 2021, 20, e1263–e1282. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, N.A.; Jones, G.-R.; Lamb, C.A.; Appleby, R.; Arnott, I.; Beattie, R.M.; Bloom, S.; Brooks, A.J.; Cooney, R.; Dart, R.J.; et al. British Society of Gastroenterology Guidance for Management of Inflammatory Bowel Disease during the COVID-19 Pandemic. Gut 2020, 69, 984–990. [Google Scholar] [CrossRef]
- Dalal, R.S.; McClure, E.; Marcus, J.; Winter, R.W.; Hamilton, M.J.; Allegretti, J.R. COVID-19 Vaccination Intent and Perceptions Among Patients with Inflammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2021, 19, 1730–1732. [Google Scholar] [CrossRef]
- Collier, D.A.; Ferreira, I.A.T.M.; Kotagiri, P.; Datir, R.P.; Lim, E.Y.; Touizer, E.; Meng, B.; Abdullahi, A.; The CITIID-NIHR BioResource COVID-19 Collaboration; Principal Investigators; et al. Age-Related Immune Response Heterogeneity to SARS-CoV-2 Vaccine BNT162b2. Nature 2021, 596, 417–422. [Google Scholar] [CrossRef]
- Valentini, D.; Cotugno, N.; Scoppola, V.; Di Camillo, C.; Colagrossi, L.; Manno, E.C.; Perno, C.F.; Russo, C.; Palma, P.; Rossi, P.; et al. Safety and Long-Term Immunogenicity of BNT162b2 Vaccine in Individuals with Down Syndrome. J. Clin. Med. 2022, 11, 694. [Google Scholar] [CrossRef]
- Cotugno, N.; Pighi, C.; Morrocchi, E.; Ruggiero, A.; Amodio, D.; Medri, C.; Colagrossi, L.; Russo, C.; Di Cesare, S.; Santilli, V.; et al. BNT162B2 MRNA COVID-19 Vaccine in Heart and Lung Transplanted Young Adults: Is an Alternative SARS-CoV-2 Immune Response Surveillance Needed? Transplantation 2022, 106, e158–e160. [Google Scholar] [CrossRef]
| pIBD N = 27 | HC N = 30 | |
| Females, N (%) | 8 (29.6) | 21 (70) |
| Age (years), Median (Range) | 15.7 (12.25–20.2) | 36 (23.8–42.5) |
IBD Subtype, N (%)
| 15 (55.6) 12 (44.4) | n.a. |
| VEO-IBD, N (%) | 2 (7.4) | n.a. |
Crohn’s Disease Location, N (%)
| 3 (20) 1 (6.7) 11 (73.3) 0 | n.a. |
Ulcerative Colitis, N (%)
| 1 (6.7) 4 (26.7) 7 (46.7) | n.a. |
IBD Therapy, N (%)
| 2 (7.4) 4 (14.8) 8 (29.6) 4 (14.8) 8 (29.6) 1 (3.7) | n.a. |
| first Dose, N = 27 | second Dose, N = 27 | |
| Local Adverse Events, N (%) | 16 (59.2) | 17 (62.9) |
| Pain in the site of injection | 16 | 15 |
| Itch | 1 | 1 |
| Hyperemia | 0 | 1 |
| Edema | 1 | 2 |
| Systemic adverse events, N (%) | 11 (40.7) | 11 (40.7) |
| Fever | 0 | 2 |
| Cold-like symptoms | 6 | 5 |
| Asthenia | 5 | 9 |
| Myalgia | 7 | 6 |
| Headache | 4 | 6 |
| Pharyngodynia | 3 | 1 |
| Vomit | 0 | 3 |
| Lymphadenopathy | 0 | 1 |
| Self administered antiinflammatory or antipyretic treatment | 1 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cotugno, N.; Franzese, E.; Angelino, G.; Amodio, D.; Romeo, E.F.; Rea, F.; Faraci, S.; Tambucci, R.; Profeti, E.; Manno, E.C.; et al. Evaluation of Safety and Immunogenicity of BNT162B2 mRNA COVID-19 Vaccine in IBD Pediatric Population with Distinct Immune Suppressive Regimens. Vaccines 2022, 10, 1109. https://doi.org/10.3390/vaccines10071109
Cotugno N, Franzese E, Angelino G, Amodio D, Romeo EF, Rea F, Faraci S, Tambucci R, Profeti E, Manno EC, et al. Evaluation of Safety and Immunogenicity of BNT162B2 mRNA COVID-19 Vaccine in IBD Pediatric Population with Distinct Immune Suppressive Regimens. Vaccines. 2022; 10(7):1109. https://doi.org/10.3390/vaccines10071109
Chicago/Turabian StyleCotugno, Nicola, Enrica Franzese, Giulia Angelino, Donato Amodio, Erminia Francesca Romeo, Francesca Rea, Simona Faraci, Renato Tambucci, Elisa Profeti, Emma Concetta Manno, and et al. 2022. "Evaluation of Safety and Immunogenicity of BNT162B2 mRNA COVID-19 Vaccine in IBD Pediatric Population with Distinct Immune Suppressive Regimens" Vaccines 10, no. 7: 1109. https://doi.org/10.3390/vaccines10071109
APA StyleCotugno, N., Franzese, E., Angelino, G., Amodio, D., Romeo, E. F., Rea, F., Faraci, S., Tambucci, R., Profeti, E., Manno, E. C., Santilli, V., Rotulo, G. A., Pighi, C., Medri, C., Morrocchi, E., Colagrossi, L., Pascucci, G. R., Valentini, D., Villani, A., ... Palma, P. (2022). Evaluation of Safety and Immunogenicity of BNT162B2 mRNA COVID-19 Vaccine in IBD Pediatric Population with Distinct Immune Suppressive Regimens. Vaccines, 10(7), 1109. https://doi.org/10.3390/vaccines10071109







