Fear of Illness and Convenient Access to Vaccines Appear to Be the Missing Keys to Successful Vaccination Campaigns: Analysis of the Factors Influencing the Decisions of Hospital Staff in Poland concerning Vaccination against Influenza and COVID-19
Abstract
:1. Introduction
2. Materials and Methods
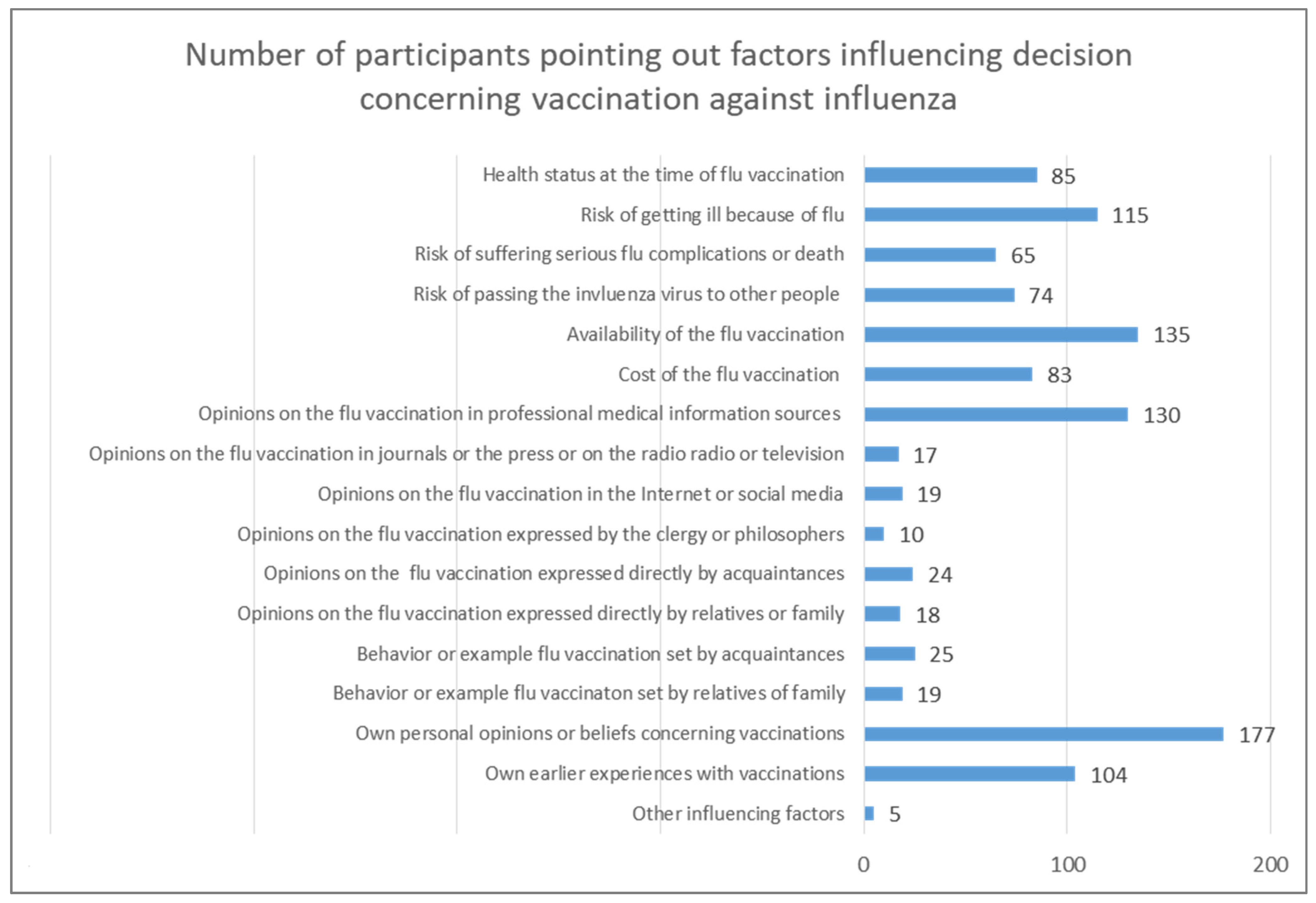
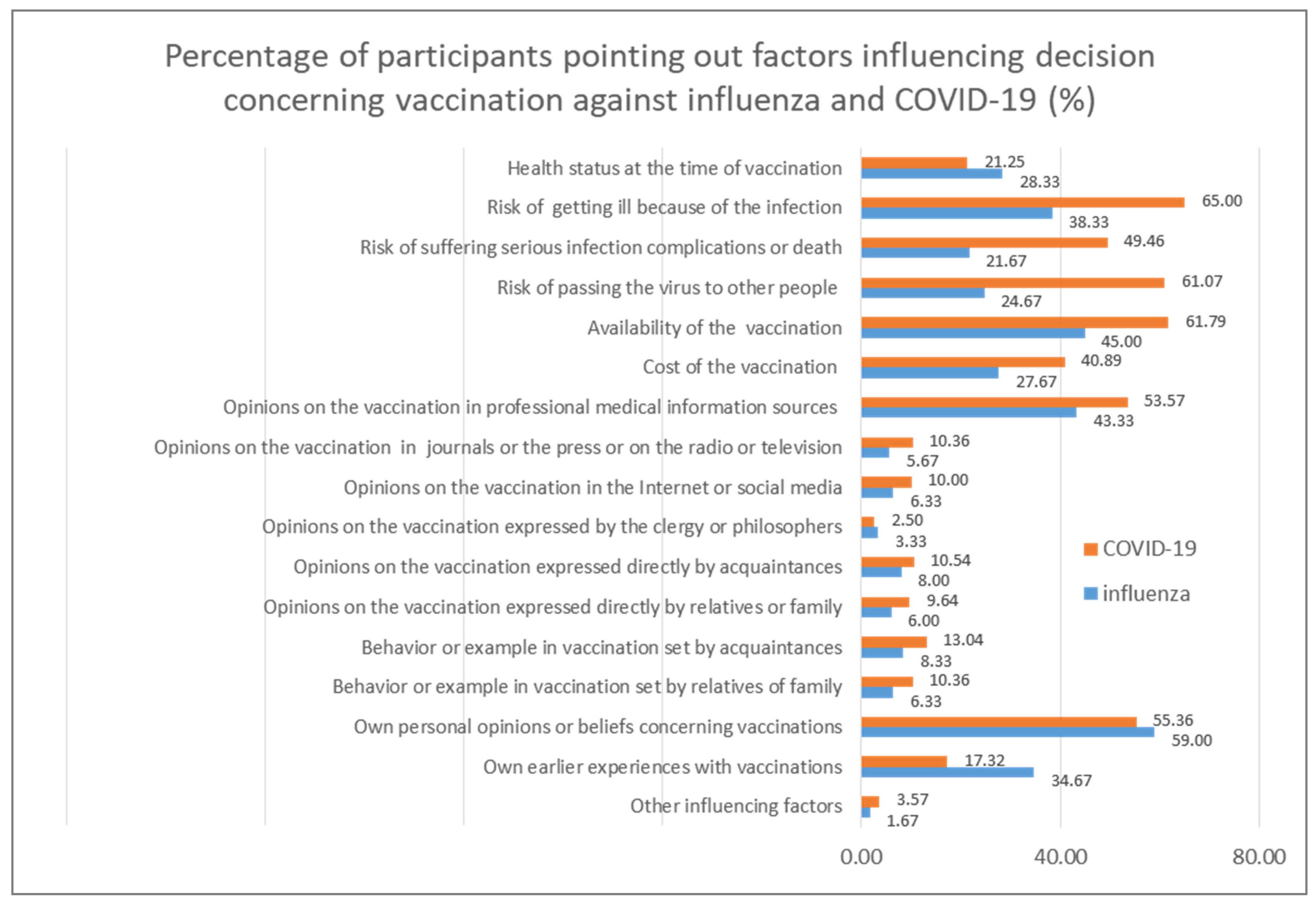
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leithäuser, N.; Schneider, J.; Johann, S.; Krumke, S.; Schmidt, E.; Streicher, M. Quantifying COVID-19-vaccine location strategies for Germany. BMC Health Serv. Res. 2021, 21, 780. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Sibal, A.; Malani, A.; Kar, S.; Kiran, S.V.; Reddy, S.; Kamineni, S.; Reddy, S.; Reddy, P.; Reddy, P.C. Symptomatic post-vaccination SARS-CoV-2 infections in healthcare workers—A multicenter cohort study. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102306. [Google Scholar] [CrossRef] [PubMed]
- Pascucci, D.; Nurchis, M.; Sapienza, M.; Castrini, F.; Beccia, F.; D’ambrosio, F. Evaluation of the effectiveness and safety of the bnt162b2 covid-19 vaccine in the vaccination campaign among the health workers of fondazione policlinico universitario agostino gemelli irccs. Int. J. Environ. Res. Public Health 2021, 18, 11098. [Google Scholar] [CrossRef] [PubMed]
- Gharpure, R.; Yi, S.; Li, R.; Jacobs Slifka, K.; Tippins, A.; Jaffe, A. COVID-19 Vaccine Uptake Among Residents and Staff Members of Assisted Living and Residential Care Communities—Pharmacy Partnership for Long-Term Care Program, December 2020–April 2021. J. Am. Med. Dir. Assoc. 2021, 22, 2016–2020.e2. [Google Scholar] [CrossRef]
- Scardina, G.; Ceccarelli, L.; Casigliani, V.; Mazzilli, S.; Napoletano, M.; Padovan, M. Evaluation of flu vaccination coverage among healthcare workers during a 3 years’ study period and attitude towards influenza and potential covid-19 vaccination in the context of the pandemic. Vaccines 2021, 9, 769. [Google Scholar] [CrossRef]
- Spinewine, A.; Pétein, C.; Evrard, P.; Vastrade, C.; Laurent, C.; Delaere, B. Attitudes towards covid-19 vaccination among hospital staff—understanding what matters to hesitant people. Vaccines 2021, 9, 469. [Google Scholar] [CrossRef]
- Kuter, B.; Browne, S.; Momplaisir, F.; Feemster, K.; Shen, A.; Green-McKenzie, J. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia. Vaccine 2021, 39, 1693–1700. [Google Scholar] [CrossRef]
- Maltezou, H.; Pavli, A.; Dedoukou, X.; Georgakopoulou, T.; Raftopoulos, V.; Drositis, I. Determinants of intention to get vaccinated against COVID-19 among healthcare personnel in hospitals in Greece. Infect. Dis. Health 2021, 26, 189–197. [Google Scholar] [CrossRef]
- Nohl, A.; Abdallah, H.; Weichert, V.; Zeiger, S.; Ohmann, T.; Dudda, M. A local survey of COVID-19: Vaccine potential acceptance rate among personnel in a level 1 trauma center without severe COVID-19 cases. Healthcare 2021, 9, 1616. [Google Scholar] [CrossRef]
- Huynh, G.; Tran, T.; Nguyen, H.; Pham, L. COVID-19 vaccination intention among healthcare workers in Vietnam. Asian Pac. J. Trop. Med. 2021, 14, 159–164. [Google Scholar] [CrossRef]
- Sirikalyanpaiboon, M.; Ousirimaneechai, K.; Phannajit, J.; Pitisuttithum, P.; Jantarabenjakul, W.; Chaiteerakij, R. COVID-19 vaccine acceptance, hesitancy, and determinants among physicians in a university-based teaching hospital in Thailand. BMC Infect. Dis. 2021, 21, 1174. [Google Scholar] [CrossRef] [PubMed]
- Myers, V.; Saban, M.; Ben-Shetrit, S.; Wilf-Miron, R. Uptake of COVID-19 vaccination among general hospital staff in Israel. Infect. Control Hosp. Epidemiol. 2021, 1, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Fotiadis, K.; Dadouli, K.; Avakian, I.; Bogogiannidou, Z.; Mouchtouri, V.; Gogosis, K. Factors associated with healthcare workers’ (HCWs) acceptance of COVID-19 vaccinations and indications of a role model towards population vaccinations from a cross-sectional survey in Greece, May 2021. Int. J. Environ. Res. Public Health 2021, 18, 10558. [Google Scholar] [CrossRef] [PubMed]
- Forgeschi, G.; Cavallo, G.; Lorini, C.; Balboni, F.; Sequi, F.; Bonaccorsi, G. Investigating adherence to COVID-19 vaccination and serum antibody concentration among hospital workers—The experience of an italian private hospital. Vaccines 2021, 9, 1332. [Google Scholar] [CrossRef]
- Drobnik, J.; Suslo, R.; Pobrotyn, P.; Fabich, E.; Magiera, V.; Diakowska, D.; Uchmanowicz, I. COVID-19 among healthcare workers in the University Clinical Hospital in Wroclaw, Poland. Int. J. Environ. Res. Public Health 2021, 18, 5600. [Google Scholar] [CrossRef]
- Gostin, L.; Salmon, D.; Larson, H. Mandating COVID-19 vaccines. JAMA 2021, 25, 532–533. [Google Scholar] [CrossRef]
- Olick, R.; Shaw, J.; Yang, Y. Ethical Issues in Mandating COVID-19 Vaccination for Health Care Personnel. Mayo Clin. Proc. 2021, 96, 2958–2962. [Google Scholar] [CrossRef]
- Mena, G.; Blanco, B.; Casas, I.; Huertas, A.; Sánchez, M.; Auñón, M. Attitudes of Spanish hospital staff towards COVID-19 vaccination and vaccination rates. PLoS ONE 2021, 16, e0257002. [Google Scholar] [CrossRef]
- Vignier, N.; Brureau, K.; Granier, S.; Breton, J.; Michaud, C.; Gaillet, M. Attitudes towards the COVID-19 vaccine and willingness to get vaccinated among healthcare workers in french guiana: The influence of geographical origin. Vaccines 2021, 9, 682. [Google Scholar] [CrossRef]
- Kara Esen, B.; Can, G.; Pirdal, B.; Aydin, S.; Ozdil, A.; Balkan, I. Covid-19 vaccine hesitancy in healthcare personnel: A university hospital experience. Vaccines 2021, 9, 1343. [Google Scholar] [CrossRef]
- Dugani, S.; Geyer, H.; Maniaci, M.; Fischer, K.; Croghan, I.; Coons, T. Hospitalist perspectives on barriers to recommend and potential benefit of the COVID-19 vaccine. Hosp. Pract. 2021, 49, 245–251. [Google Scholar] [CrossRef] [PubMed]
- El Kefi, H.; Kefi, K.; Krir, M.; Brahim, C.; Baatout, A.; Bouzouita, I. Acceptability of COVID-19 vaccine: A cross-sectional study in a Tunisian general hospital. Pan Afr. Med. J. 2021, 39, 245. [Google Scholar] [CrossRef] [PubMed]
- Robbins, T.; Kyrou, I.; Clark, C.; Sharma, K.; Laird, S.; Berry, L. Healthcare staff perceptions following inoculation with the bnt162b2 mrna covid-19 vaccine at university hospitals coventry & warwickshire nhs trust. Int. J. Environ. Res. Public Health 2021, 18, 9378. [Google Scholar] [CrossRef]
- Bauernfeind, S.; Hitzenbichler, F.; Huppertz, G.; Zeman, F.; Koller, M.; Schmidt, B. Brief report: Attitudes towards COVID-19 vaccination among hospital employees in a tertiary care university hospital in Germany in December 2020. Infection 2021, 49, 1307–1311. [Google Scholar] [CrossRef]
- Abuown, A.; Ellis, T.; Miller, J.; Davidson, R.; Kachwala, Q.; Medeiros, M. COVID-19 vaccination intent among London healthcare workers. Occup. Med. 2021, 71, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Miyatake, N.; Suzuki, H.; Okada, S.; Tanimoto, K. A text mining-based survey of pre-impressions of medical staff toward COVID-19 vaccination in a designated medical institution for class ii infectious diseases. Vaccines 2021, 9, 1282. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.; Marshall, C.; Patel, P.; Goss, C.; Jenkins, D.; Ellwood, C. SARS-CoV-2 vaccine uptake in a multi-ethnic UK healthcare workforce: A cross-sectional study. PLoS Med. 2021, 18, e1003823. [Google Scholar] [CrossRef]
- Huang, X.; Yu, M.; Fu, G.; Lan, G.; Li, L.; Yang, J. Willingness to Receive COVID-19 Vaccination among People Living with HIV and AIDS in China: Nationwide Cross-sectional Online Survey. JMIR Public Health Surveill. 2021, 7, e31125. [Google Scholar] [CrossRef]
- Kalbhenn, J.; Hammer, T.; Hug, M.; Dürschmied, D.; Wenz, F.; Steinmann, D. Subjective well-being and ability to work of hospital staff after SARS-CoV2 immunization with the mRNA vaccine BNT162b2. Dtsch. Med. Wochenschr. 2021, 146, e58–e64. [Google Scholar] [CrossRef]
- Rozporządzenie Rady Ministrów z Dnia 14 Grudnia 2021 r. Zmieniające Rozporządzenie w Sprawie Ustanowienia Określonych Ograniczeń, Nakazów i Zakazów w Związku z Wystąpieniem Stanu Epidemii (Dz.U. 2021 poz. 2311). Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20210002311/O/D20212311.pdf (accessed on 15 February 2022). (In Polish)
- Pfizer and Biontech Uzyskują Dopuszczenie do Obrotu w Unii Europejskiej Szczepionki Przeciw COVID-19. Pfizer 21 December 2020. Available online: https://www.pfizer.pl/files/12_21_Uzyskanie-dopuszczenia-do-obrotu-w-UE.pdf (accessed on 14 December 2021). (In Polish).
- Szarowska, A.; Zaczyński, A.; Szymański, P.; Borawska, B.; Szarek, I.; Szoszkiewicz, I.; Butkiewicz, S.; Szydlarska, D.; Gil, R.; Śliwczyński, A.; et al. The Central Clinical Hospital of the Ministry of Internal Affairs and Administration Program Coordination Group OBO. Initiation of the COVID-19 vaccination program in Poland: Vaccination of the patient “zero” and first experience from the Central Clinical Hospital of the Ministry of Internal Affairs and Administration. Pol. Arch. Intern. Med. 2021, 131, 101–102. [Google Scholar] [CrossRef]
- Naczelna Izba Lekarska. Szczepienia Lekarzy i Lekarzy Dentystów Przeciwko COVID-19 w Liczbach. 4 March 2021. Available online: https://nil.org.pl/aktualnosci/5359-szczepienia-lekarzy-i-lekarzy-dentystow-p-covid-19-w-liczbach (accessed on 14 December 2021). (In Polish).
- Dąbek, A. Ile Lekarzy i Pielęgniarek w Polsce Zostało Zaszczepionych? Medonet.pl. 7 July 2021. Available online: https://www.medonet.pl/porozmawiajmyoszczepionce,szczepienia-przeciw-covid-19--ilu-jest-zaszczepionych-lekarzy-w-polsce,artykul,32314696.html (accessed on 14 December 2021).
- Byhoff, E.; Paulus, J.; Guardado, R.; Zubiago, J.; Wurcel, A. Healthcare workers’ perspectives on coronavirus testing availability: A cross sectional survey. BMC Health Serv. Res. 2021, 21, 719. [Google Scholar] [CrossRef]
- Matejuk, T. Koronawirus we Wrocławiu, na Dolnym Śląsku, w Polsce. Wroclife.pl. 13 December 2021. Available online: https://wroclife.pl/nasze-miasto/koronawirus-wroclaw-2020/koronawirus-dolny-slask-13-grudnia-2021/ (accessed on 14 December 2021). (In Polish).
- Paplicki, M.; Susło, R.; Najjar, N.; Ciesielski, P.; Augustyn, J.; Drobnik, J. Conflict of individual freedom and community health safety: Legal conditions on mandatory vaccinations and changes in the judicial approach in the case of avoidance. Fam. Med. Prim. Care Rev. 2018, 20, 389–395. [Google Scholar] [CrossRef]
- Paplicki, M.; Susło, R.; Benedikt, A.; Drobnik, J. Effectively enforcing mandatory vaccination in Poland and worldwide. Fam. Med. Prim. Care Rev. 2020, 22, 252–256. [Google Scholar] [CrossRef]
- Central Statistical Office. Population: Size and Structure and Vital Statistics in Poland by Territorial Division in 2019; Zakład Wydawnictw Statystycznych: Warsaw, Poland, 2022; p. 23. Available online: https://stat.gov.pl/files/gfx/portalinformacyjny/pl/defaultaktualnosci/5468/6/27/1/ludnosc._stan_i_struktura_oraz_ruch_naturalny_w_przekroju_terytorialnym_na_31.12.2019.pdf (accessed on 15 February 2022).
- Central Statistical Office. Statistical Information and Elaborations—Health and Health Care in 2020, Medical Personnel; Zakład Wydawnictw Statystycznych: Warsaw, Poland, 2022; pp. 49–61. Available online: https://stat.gov.pl/download/gfx/portalinformacyjny/pl/defaultaktualnosci/5513/1/11/1/zdrowie_i_ochrona_zdrowia_2020_korekta.pdf (accessed on 15 February 2022).
- Polska na 23. Miejscu w UE pod Względem Odsetka Zaszczepionych Osób. 300gospodarka.pl. 13 February 2022. Available online: https://300gospodarka.pl/wykres-dnia/polska-miejsce-w-europie-szczepienia-covid-19 (accessed on 15 February 2022). (In Polish).
- Która z Polskich Uczelni ma Najwyższy Odsetek Zaszczepionych Studentów? Medexpress.pl. 13 February 2022. Available online: https://www.medexpress.pl/ktora-z-polskich-uczelni-ma-najwyzszy-odsetek-zaszczepionych-studentow/83748 (accessed on 15 February 2022). (In Polish).
- Rozporządzenie Ministra Zdrowia z Dnia 22 Grudnia 2021 r. Zmieniające Rozporządzenie w Sprawie Ogłoszenia na Obszarze Rzeczypospolitej Polskiej Stanu Epidemii (Dz. U. 2021 poz. 2398). Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20210002398/O/D20212398.pdf (accessed on 15 February 2022). (In Polish)
- Susło, R.; Pobrotyn, P.; Brydak, L.; Rypicz, Ł.; Grata-Borkowska, U.; Drobnik, J. Seasonal Influenza and Low Flu Vaccination Coverage as Important Factors Modifying the Costs and Availability of Hospital Services in Poland: A Retrospective Comparative Study. Int. J. Environ. Res. Public Health 2021, 18, 5173. [Google Scholar] [CrossRef] [PubMed]
- Peters, G.-J.; Ruiter, R.; Kok, G. Threatening communication: A critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychol. Rev. 2012, 7, S8–S31. [Google Scholar] [CrossRef]
- Halkjelsvik, T. Do disgusting and fearful anti-smoking advertisements increase or decrease support for tobacco control policies? Int. J. Drug Policy 2014, 25, 744–747. [Google Scholar] [CrossRef] [Green Version]
- Zarębska-Michaluk, D.; Rzymski, P.; Moniuszko-Malinowska, A.; Brzdęk, M.; Martonik, D.; Rorat, M.; Wielgat, J.; Kłos, K.; Musierowicz, W.; Wasilewski, P.; et al. Does Hospitalization Change the Perception of COVID-19 Vaccines among Unvaccinated Patients? Vaccines 2022, 10, 476. [Google Scholar] [CrossRef]
- Torres-Estrella, C.U.; Reyes-Montes, M.d.R.; Duarte-Escalante, E.; Sierra Martínez, M.; Frías-De-León, M.G.; Acosta-Altamirano, G. Vaccines Against COVID-19: A Review. Vaccines 2022, 10, 414. [Google Scholar] [CrossRef]
- Araujo da Silva, A.R.; de Carvalho, B.R.R.; Esteves, M.d.M.; Teixeira, C.H.; Souza, C.V. The Role of COVID-19 Vaccinal Status in Admitted Children during OMICRON Variant Circulation in Rio de Janeiro, City—Preliminary Report. Vaccines 2022, 10, 619. [Google Scholar] [CrossRef]
- McElfish, P.A.; Willis, D.E.; Shah, S.K.; Reece, S.; Andersen, J.A.; Schootman, M.; Richard-Davis, G.; Selig, J.P.; Warmack, T.S. Parents’ and Guardians’ Intentions to Vaccinate Children against COVID-19. Vaccines 2022, 10, 361. [Google Scholar] [CrossRef]
- Van Hoecke, A.L.; Sanders, J.G. An Online Experiment of NHS Information Framing on Mothers’ Vaccination Intention of Children against COVID-19. Vaccines 2022, 10, 720. [Google Scholar] [CrossRef] [PubMed]
- PZH-NIZP Zachorowania i podejrzenia zachorowań na grypę w Polsce. Państwowy Zakład Higieny—Narodowy Instytut Zdrowia Publicznego. Available online: http://wwwold.pzh.gov.pl/oldpage/epimeld/grypa/index.htm (accessed on 3 June 2022). (In Polish)
- Koronawirus w Polsce (SARS-CoV-2). Koronawirusunas.pl. Available online: https://koronawirusunas.pl/ (accessed on 3 June 2022). (In Polish).



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Susło, R.; Pobrotyn, P.; Mierzecki, A.; Drobnik, J. Fear of Illness and Convenient Access to Vaccines Appear to Be the Missing Keys to Successful Vaccination Campaigns: Analysis of the Factors Influencing the Decisions of Hospital Staff in Poland concerning Vaccination against Influenza and COVID-19. Vaccines 2022, 10, 1026. https://doi.org/10.3390/vaccines10071026
Susło R, Pobrotyn P, Mierzecki A, Drobnik J. Fear of Illness and Convenient Access to Vaccines Appear to Be the Missing Keys to Successful Vaccination Campaigns: Analysis of the Factors Influencing the Decisions of Hospital Staff in Poland concerning Vaccination against Influenza and COVID-19. Vaccines. 2022; 10(7):1026. https://doi.org/10.3390/vaccines10071026
Chicago/Turabian StyleSusło, Robert, Piotr Pobrotyn, Artur Mierzecki, and Jarosław Drobnik. 2022. "Fear of Illness and Convenient Access to Vaccines Appear to Be the Missing Keys to Successful Vaccination Campaigns: Analysis of the Factors Influencing the Decisions of Hospital Staff in Poland concerning Vaccination against Influenza and COVID-19" Vaccines 10, no. 7: 1026. https://doi.org/10.3390/vaccines10071026
APA StyleSusło, R., Pobrotyn, P., Mierzecki, A., & Drobnik, J. (2022). Fear of Illness and Convenient Access to Vaccines Appear to Be the Missing Keys to Successful Vaccination Campaigns: Analysis of the Factors Influencing the Decisions of Hospital Staff in Poland concerning Vaccination against Influenza and COVID-19. Vaccines, 10(7), 1026. https://doi.org/10.3390/vaccines10071026