1. Introduction
The severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) pandemic, which began at the end of 2019, created new challenges in different domains; this was especially the case for health care systems and their physicians as well as patients with immunosuppressant therapies. To date, the pandemic remains challenging, particularly regarding vaccinations and vaccination counseling for patients at risk. These include elderly patients, patients with comorbidities (e.g., diabetes, obesity and hypertension) or patients treated with immunotherapy or disease-modifying therapies (DMT). Anti-CD20 therapies are used in the treatment of, for example, rheumatological diseases, hematological malignancies or neurological disorders such as multiple sclerosis (MS) [
1,
2]. The aim of the therapy in patients with multiple sclerosis is to reduce disease activity [
2]. B cell depletion occurs up to 72 h hours after infusion and lasts up to 9 months and in some cases even longer. B cell repopulation can usually be expected after 9–12 months [
3,
4].
Until now, vaccination strategies have varied from country to country. Anti-CD20 treatments have repeatedly been shown to be associated with a decreased humoral immune response after a vaccination [
2,
5]. The superiority of the vaccination effects in patients treated with anti-CD20 treatments of either of the available mRNA vaccines, Moderna
® (mRNA-1273, Cambridge, MA, USA) and Pfizer/BioNTech
® (BNT162b2, Mainz, Rhineland-Palatinate, Germany), has not yet been demonstrated. A cohort study, including untreated multiple sclerosis (MS) patients and MS patients treated with several different disease-modifying therapies (DMTs), demonstrated in the total population by a multivariable analysis a higher antibody titer in patients vaccinated with mRNA-1273 compared with BNT162b2 [
6].
As anti-CD20-treated patients are particularly at risk of a reduced humoral response to mRNA vaccinations as well as a more severe course of COVID-19, our cohort study aimed to compare the antibody response after two vaccinations with either BNT162b2 or mRNA-1273 in MS patients treated with anti-CD20 therapies.
2. Materials and Methods
Anti-CD20-treated MS patients who had been vaccinated twice with either BNT162b2 or mRNA-1273 as indicated by SwissMedic were retrospectively identified by a medical chart review. Of the 74 included patients, 26 were identified at Bern University Hospital (ethical vote of NI registry study: 2017-01369, last amendment August 2020) and 48 were identified at the Cantonal Hospital of Lucerne (ethical vote: 2020-00044). Anti-spike IgG serum titers were assessed using an Abbott SARS-CoV-2 IgG assay (Abbott Laboratories, Chicago, IL, USA) and a Liaison SARS-CoV-2 S1/S2 IgG assay (Diasorin, Italy) in Bern and an Elecys® SARS-CoV-2 Ig assay (Roche, Switzerland) in Lucerne. According the manufacturer’s instructions, the Liason SARS-CoV-2 S1/S2 IgG assay was evaluated with a plaque reduction neutralization test (PRNT); 87% of the samples with a SARS-CoV-2 S1/S2 IgG result ≥ 80 AU/mL had a PRNT titer of ≥1:160. Therefore, we proposed a cut-off of 100 AU/mL and assumed at both centers an anti-spike titer of ≥100 AU/mL to be protective. B cell counts were analyzed in the main laboratory of each center (Bern and Lucerne, Switzerland) using fluorescence-activated cell sorting (FACS). The continuous variables were given as a mean and a 95% confidence interval (95% CI); the categorical variables were given as frequencies. A Mann–Whitney test and a Fisher’s exact test as well as a multivariable linear regression analysis with anti-spike IgG (AU/mL) as the dependent variable were run using SPSS Statistic 25 (IBM Corp., Amonk, NY, USA).
3. Results
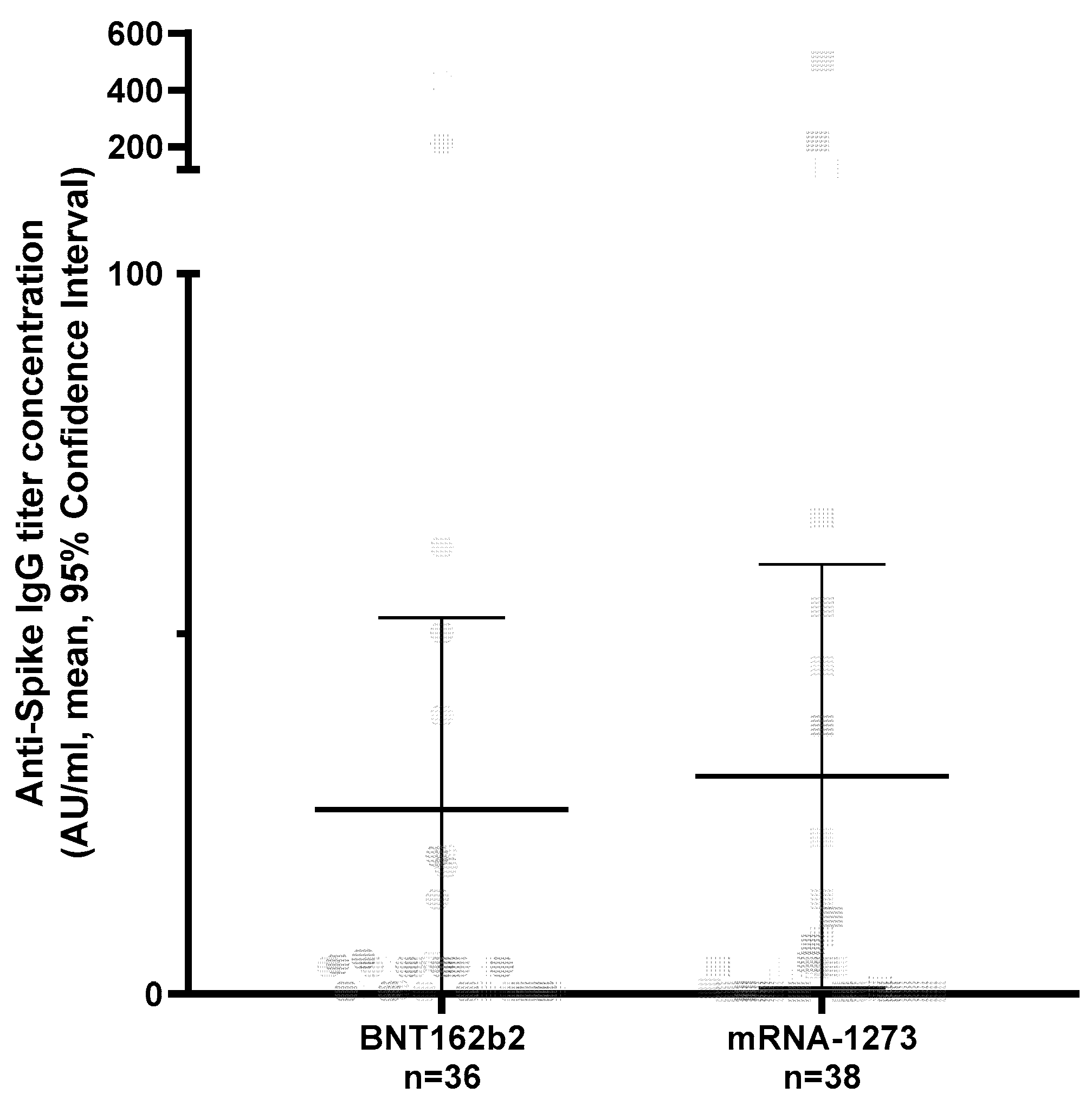
Of the 74 patients, 41 (63.51%) were female, the mean age was 46.6 years (95% CI 43.4–49.9) and a diagnosis of relapsing multiple sclerosis (RMS) was more frequent (57/74, 77.02%) than primary progressive MS (PPMS) (17/74, 23.61%). A total of 9/74 were treated with Rituximab (MabThera
®, Roche) and 65/74 with Ocrelizumab (Ocrevus
®, Roche). In total, 36/74 were vaccinated with BNT162b2 and 38/74 with mRNA-1273, following the national vaccination recommendations (mRNA-1273: 2 vaccinations (100 μg/0.5 mL per vaccination) with an interval of 28 days; BNT162b2: 2 vaccinations (30 μg/0.3 mL per vaccination) with an interval of 21 days;
Table S1) [
7]. In both vaccine groups, protective anti-spike IgG titers (≥100 AU/mL) were infrequently achieved (5/74: mRNA-1273 3/38; BNT162b2 2/36) (
Figure S1). The anti-spike IgG titer did not differ between the two vaccine types. In order to include the distribution of cohort characteristics in our analysis, we ran a multivariable linear regression analysis. This demonstrated no significant differences between both vaccines (
Figure 1;
Table 1). However, in this regression analysis, the time interval between the measurement of the humoral immune response and the second vaccination demonstrated a trend toward a reduction in anti-spike IgG serum titers over time in anti-CD20-treated MS patients (
Table 1). Furthermore, in patients treated with anti-CD20 medications, data on B cell counts were present in 68 cases. The mean percentage of B cells was 0.68% (95% CI 0.16–1.09). Overall, the anti-spike IgG titer showed a non-significant trend toward lower values in patients with a complete B cell depletion (0.0%, spike titer mean 95% CI 16.69; 5.9–39, 3) compared with those with an incomplete B cell depletion (>0.0%, spike titer 51.9; 6.58–97.22, Mann–Whitney test
p = 0.14), which became significant when comparing those with a protective anti-spike IgG titer level with patients without a protective antibody response (Chi2
p = 0.04;
Figure S1).
4. Discussion
In both vaccine groups, protective anti-spike IgG titers (≥100 AU/mL) were infrequently achieved. This was reasonable due to the mode of action of B cell-depleting drugs that destroy CD20+ B cells and, therefore, suppress antibody production—for example, after a vaccination. In greater detail, the anti-spike IgG responses between the two mRNA vaccines (BNTech-162b2 vs. mRNA-1273) did not differ in our cohort, either regarding the titer levels or regarding reaching the threshold for a protective humoral response. We observed a trend that anti-CD20-treated patients showed a drop in anti-spike IgG serum titers over time. This observation, which has also been shown by others [
6], bears therapeutic consequences as initial positive titers should be checked in case of an infection with the SARS-CoV-2 virus to identify patients who would benefit from an intravenous anti-spike IgG treatment against acute COVID-19. However, it has to be noted that it is unknown to what extent a drop of anti-spike IgG serum titer over time corresponds with a diminished immune response to COVID-19, which has to be shown in larger clinical trials. A reduced protection against the virus can, however, be anticipated by advocating booster vaccinations in these patients. The main limitation of our work in addition to the retrospective design was the small sample size, which affected the generalizability and power of our analysis. Furthermore, as this was a real-world study, different assays were used to detect the SARS-CoV-2 immune response run in the main laboratories of the respective centers. The assay used in Bern detected IgG whereas the assay run in Lucerne detected high-affinity Ig against the anti-spike region, which mainly consists of IgG but smaller amounts of IgM antibodies are also measured. To statistically adjust for this methodological shortcoming of this retrospective real-world study, the multivariable linear regression analysis was controlled for each center (Bern vs. Lucerne), which did not impact the anti-spike IgG level. The worldwide pandemic remains a major threat for our societies, calling for open data and data-sharing strategies to answer the major questions as a research community (see Data Availability Statement below).
5. Conclusions
We identified a trend that anti-CD20-treated patients showed a drop in anti-spike IgG serum titers over time despite the same anti-spike IgG responses between the two mRNA vaccines. This observation, which has also been shown by others, bears therapeutic consequences as initial positive titers should be checked in case of an infection with the SARS-CoV-2 virus to identify patients who would benefit from an intravenous anti-spike IgG treatment against acute COVID-19.
Supplementary Materials
The following are available online at
https://www.mdpi.com/article/10.3390/vaccines10060922/s1, Figure S1: Anti-spike IgG titers in anti-CD20-treated MS patients vaccinated twice with BNT162b2 or mRNA-1273 vaccines, following the SwissMedic recommendations; Table S1: Characteristics of MS patients treated with anti-CD20 drugs (Ocrelizumab, Rituximab).
Author Contributions
Conceptualization, H.H., R.H., C.P.K.; methodology, H.H., R.H., C.P.K., F.S.-R., S.L.L.; software, H.H., R.H., C.P.K.; validation, H.H., R.H., C.P.K.; formal analysis, H.H., R.H., C.P.K., F.S.-R., A.S., A.C., S.L.L.; investigation, H.H., R.H., C.P.K.; resources, H.H., R.H., C.P.K., F.S.-R., L.D., N.K.; data curation, H.H., R.H., C.P.K.; writing—original draft preparation, H.H., R.H., C.P.K., F.S.-R., S.L.L.; writing—review and editing, H.H., R.H., F.S.-R., L.D., N.K., S.L.L., A.C., C.P.K., A.S.; visualization, H.H., R.H., C.P.K., C.F., A.S.; supervision, H.H., R.H., C.P.K., F.S.-R.; project administration, H.H., R.H., C.P.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Kantonale Ethikkommission, Bern (ethical vote: 2017-01369, last amendment August 2020) and by the Ethics Committee of Nordwestschweiz und Zentralschweiz (EKNZ) (ethical vote: 2020-00044).
Informed Consent Statement
The study was approved by the Cantonal Ethics Committees. Because of the nature of the analysis with pseudonymised patient data using data available from clinical routine, separate informed consent was waived by the committee. This corresponds to the local legislation. For patients seen after the introduction of the general consent (February 2015), the patients’ consent status was checked before inclusion in the analysis.
Data Availability Statement
In terms of the further use of our data, we ask researchers to cite our paper in their Method section. Anonymized data are available via the corresponding author.
Conflicts of Interest
H.H. received research support and travel grants within the last 5 years from Biogen, Merck, Roche and Bristol Myers Squibb, Almirall. R.H. received speaker/advisor honoraria from Merck, Novartis, Roche, Biogen, Alexion, Sanofi, Janssen, Bristol-Myers Squibb and Almirall. He has received research support within the last 5 years from Roche, Merck, Sanofi, Biogen, Chiesi and Bristol-Myers Squibb. He also received research grants from the Swiss MS Society and is a member of the Advisory Board of the Swiss MS Society. He also serves as an associate editor for the Journal of Central Nervous System Disease. All conflicts are not related to this work. C.F. received speaker honoraria and/or travel compensation for activities with Biogen, Sanofi Genzyme, Novartis and Merck and research support from Chiesi not related to this work. S.L.L. received research support from the European Union and the Swiss National Foundation not related to this work. F.S.-R. received research support from the Swiss HIV Cohort Study and the Swiss Transplant Cohort Study not related to this work. L.D. received travel grants from Merck, Biogen, Roche and Bayer Schweiz. She also received speaker honoraria from Biogen and Merck. A.C. has received speaker/board honoraria from Actelion (Janssen/J&J), Almirall, Bayer, Biogen, Celgene (BMS), Genzyme, Merck KGaA (Darmstadt, Germany), Novartis, Roche and Teva all for hospital research funds. He has received research support from Biogen, Genzyme and UCB as well as the European Union and the Swiss National Foundation. He serves as an associate editor for the European Journal of Neurology and is on the editorial board for Clinical and Translational Neuroscience and is a topic editor for the Journal of International Medical Research. A.S. received speaker honoraria and/or travel compensation for activities with Bristol Myers Squibb, Novartis and Roche as well as research support from Baasch Medicus Foundation and the Swiss MS Society. She serves on the editorial board of Frontiers in Neurology: Multiple Sclerosis and Neuroimmunology all not related to this work. C.P.K. has received honoraria for lectures as well as research support from Biogen, Novartis, Almirall, Teva, Merck, Sanofi Genzyme, Roche, Eli Lilly, Janssen, Celgene and the Swiss MS Society (SMSG).
References
- Gaitzsch, E.; Passerini, V.; Khatamzas, E.; Strobl, C.D.; Muenchhoff, M.; Scherer, C.; Osterman, A.; Heide, M.; Reischer, A.; Subklewe, M.; et al. COVID-19 in patients receiving CD20-depleting immunochemotherapy for B-cell lymphoma. Hemasphere 2021, 7, e603. [Google Scholar] [CrossRef] [PubMed]
- Apostolidis, S.A.; Kakara, M.; Painter, M.M.; Goel, R.R.; Mathew, D.; Lenzi, K.; Rezk, A.; Patterson, K.R.; Espinoza, D.A.; Kadri, J.C.; et al. Cellular and Humoral Immune Responses Following SARS-CoV-2 MRNA Vaccination in Patients with Multiple Sclerosis on Anti-CD20 Therapy; Springer: New York, NY, USA, 2021; Volume 27. [Google Scholar] [CrossRef]
- Petra, R.; Arumugam, P.; Christian, K.; Thomas, D.; Tony, H.-P. Rgeneration of B cell subsets after transient B cells depletion using anti-CD20 antibodies in rheumatoid arthritis. Arthritis Rheum Arthritis Care Res. 2006, 54, 2377–2386. [Google Scholar] [CrossRef]
- Gelfand, J.M.; Cree, B.A.C.; Hauser, S.L. Ocrelizumab and Other CD20+ B-Cell-Depleting Therapies in Multiple Sclerosis. Neurotherapeutics 2017, 14, 835–841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Louapre, C.; Ibrahim, M.; Maillart, E.; Abdi, B.; Papeix, C.; Stankoff, B.; Dubessy, A.; Bensa-Koscher, C.; Créange, A.; Chamekh, Z.; et al. Anti-CD20 therapies decrease humoral immune response to SARS-CoV-2 in patients with multiple sclerosis or neuromyelitis optica spectrum disorders. J. Neurol. Neurosurg. Psychiatry 2022, 93, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Sormani, M.P.; Inglese, M.; Schiavetti, I.; Carmisciano, L.; Laroni, A.; Lapucci, C.; da Rin, G.; Serrati, C.; Gandoglia, I.; Tassinari, T.; et al. Effect of SARS-CoV-2 mRNA vaccination in MS patients treated with disease modifying therapies. eBioMedicine 2021, 72, 103581. [Google Scholar] [CrossRef] [PubMed]
- Einwilligung, I.; Impfziele, S.; Impfziele, S. Impfempfehlung für mRNA-Impfstoffe Gegen COVID-19; Zielgruppe 3; Bundesamt für Gesundheit (BAG) und Eidgenössische Kommission für Impffragen (EKIF): Bern, Switzerland, 2022; pp. 1–53. [Google Scholar]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).