Medics as a Positive Deviant in Influenza Vaccination: The Role of Vaccine Beliefs, Self-Efficacy and Contextual Variables
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
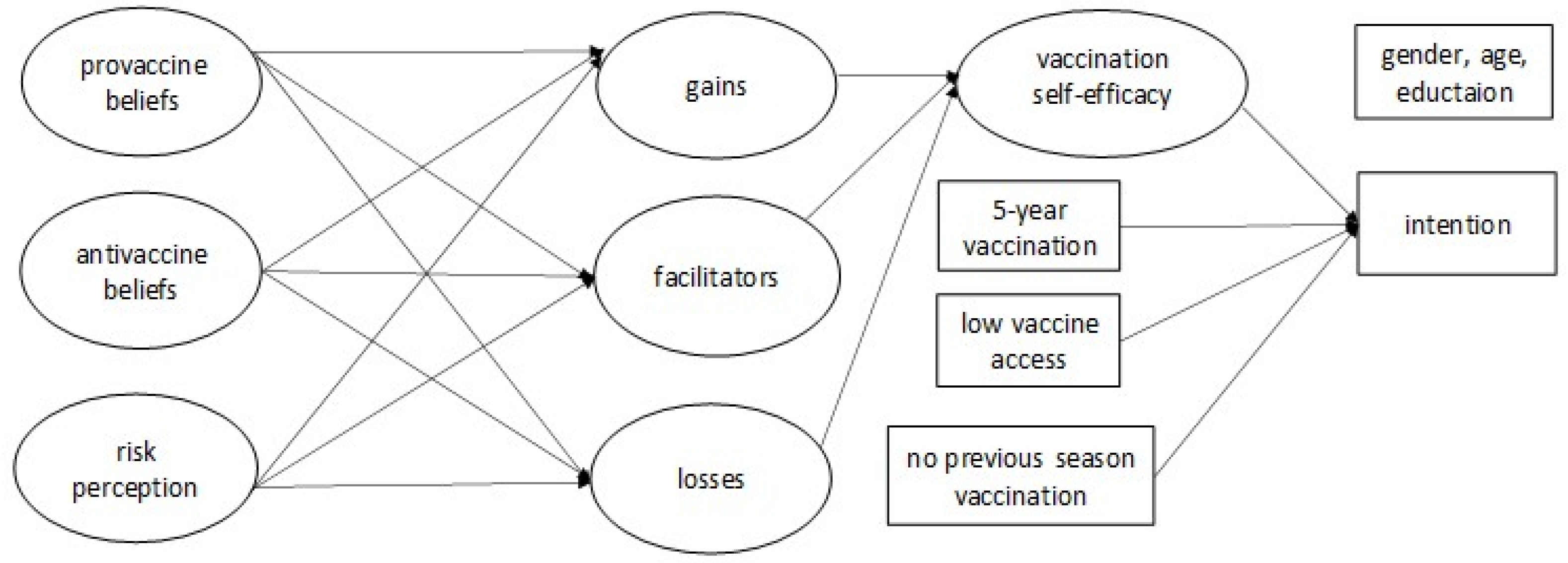
2.4. Statistical Analysis
3. Results
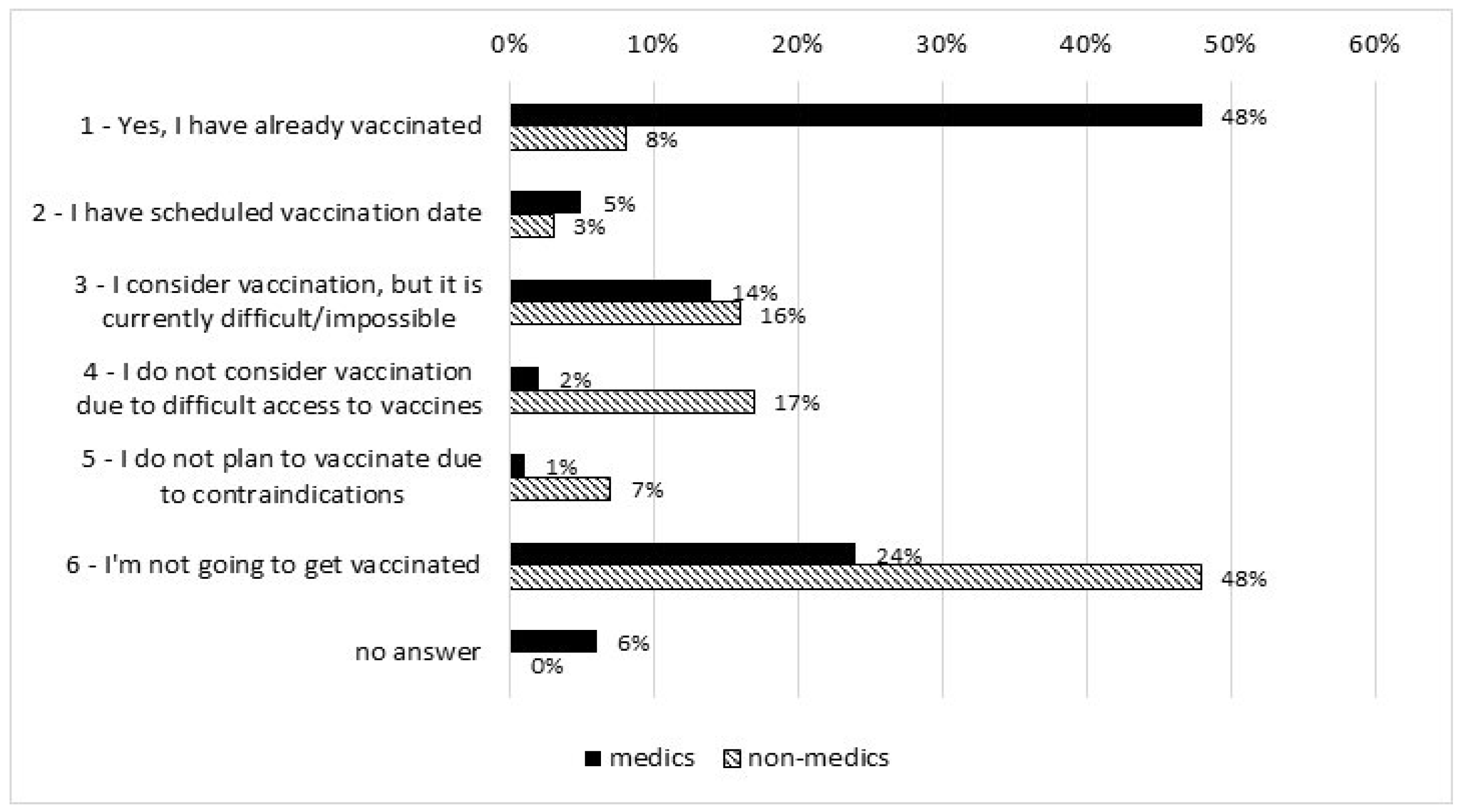
3.1. Differences between Groups in Studied Variables
3.2. Verification of the Model
3.3. Comparison of the Model in Medics and Non-Medics
3.4. Direct Predictors of Vaccination Intention/Implementation and Self-Efficacy
3.5. Indirect Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (2019). Recommendations on Influenza Vaccination during the 2019–2020 Winter Season: October 2019 (No. WHO/EURO: 2019-3718-43477-61074); Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Mereckiene, J. Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States: Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2018. [Google Scholar] [CrossRef]
- Sas, A. Number of Influenza Vaccinations in Poland from 2001 to 2020. Available online: https://www.statista.com/statistics/1086732/poland-number-of-influenza-vaccinations/#statisticContainer (accessed on 10 January 2022).
- Baxter, R.; Taylor, N.; Kellar, I.; Lawton, R. What methods are used to apply positive deviance within healthcare organisations? A systematic review. BMJ Qual. Saf. 2016, 25, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- Le Marechal, M.; Fressard, L.; Agrinier, N.; Verger, P.; Pulcini, C. General practitioners’ perceptions of vaccination controversies: A French nationwide cross-sectional study. Clin. Microbiol. Infect. 2018, 24, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Larson, H. The paradox of vaccine hesitancy among healthcare professionals. Clin. Microbiol. Infect. 2018, 24, 799–800. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Jędrzejek, M.J.; Mastalerz-Migas, A. Influenza vaccination in healthcare workers: Vaccination coverage, determinants, possible interventions. Med. Pr. 2021, 72, 305–319. [Google Scholar] [CrossRef]
- Abraham, C.; Sheeran, P. The health belief model. In Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models, 3rd ed.; Conner, M., Norman, P., Eds.; Open University Press: Maidenhead, UK, 2015; pp. 30–69. [Google Scholar]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Luszczynska, A.; Schwarzer, R. Social cognitive theory. In Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models, 3rd ed.; Conner, M., Norman, P., Eds.; Open University Press: Maidenhead, UK, 2015; pp. 225–251. [Google Scholar]
- Zhang, C.-Q.; Zhang, R.; Schwarzer, R.; Hagger, M.S. A meta-analysis of the health action process approach. Health Psychol. 2019, 38, 623–637. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions, 1st ed.; Silverback Publishing: Sutton, UK, 2014; pp. 1003–1010. [Google Scholar]
- Sniehotta, F.F.; Aunger, R. Stage Models of Behaviour Change. Health Psychology, 2nd ed.French, D.P., Kaptein, A., Vedhara, K., Weinman, J., Eds.; Blackwell: Oxford, UK, 2010; (in press). [Google Scholar]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef]
- Schwarzer, R.; Sniehotta, F.F.; Lippke, S.; Luszczynska, A.; Scholz, U.; Schüz, B.; Wegner, M.; Ziegelmann, J.P. On the Assessment and Analysis of Variables in the Health Action Process Approach Conducting An Investigation. 2013. Available online: http://userpage.fu-berlin.de/gesund/hapa_web.pdf (accessed on 10 March 2022).
- Schwarzer, R. Health Action Process Approach (HAPA) as a theoretical framework to understand behavior change. Actualidades En Psicol. 2016, 30, 119–130. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Klimiuk, K.; Czoska, A.; Biernacka, K.; Balwicki, Ł. Vaccine misinformation on social media: Topic-based content and sentiment analysis of Polish vaccine: Deniers’ comments on Facebook. Hum. Vaccines Immunother. 2021, 17, 2026–2035. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Vézina-Im, L.-A.; Naccache, H. Determinants of Influenza Vaccination among Healthcare Workers. Infect. Control Hosp. Epidemiology 2010, 31, 689–693. [Google Scholar] [CrossRef]
- Fall, E.; Izaute, M.; Chakroun-Baggioni, N. How can the health belief model and self-determination theory predict both influenza vaccination and vaccination intention ? A longitudinal study among university students. Psychol. Health 2018, 33, 746–764. [Google Scholar] [CrossRef]
- Boey, L.; Bral, C.; Roelants, M.; De Schryver, A.; Godderis, L.; Hoppenbrouwers, K.; Vandermeulen, C. Attitudes, believes, determinants and organisational barriers behind the low seasonal influenza vaccination uptake in healthcare workers—A cross-sectional survey. Vaccine 2018, 36, 3351–3358. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, P.G.; Albertin, C.; Casillas, A.; Valderrama, R.; Duru, O.K.; Ong, M.K.; Vangala, S.; Tseng, C.-H.; Rand, C.M.; Humiston, S.G.; et al. Effect of Patient Portal Reminders Sent by a Health Care System on Influenza Vaccination Rates. JAMA Intern. Med. 2020, 180, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Prematunge, C.; Corace, K.; McCarthy, A.; Nair, R.C.; Pugsley, R.; Garber, G. Factors influencing pandemic influenza vaccination of healthcare workers—A systematic review. Vaccine 2012, 30, 4733–4743. [Google Scholar] [CrossRef] [PubMed]
- Yeung, M.P.S.; Lam, F.L.; Coker, R. Factors associated with the uptake of seasonal influenza vaccination in adults: A systematic review. J. Public Health 2016, 38, 746–753. [Google Scholar] [CrossRef]
- Brondi, L.; Higgins, M.; Gorman, D.; McCormick, D.; McCallum, A.; Fisken, S. Review of the Scientific Literature on Drivers and Barriers of Seasonal Influenza Coverage in the EU/EEA. Stockh. Eur. Cent. Dis. Prev. Control. 2013. [Google Scholar] [CrossRef][Green Version]
- Schwarzer, R.; Luszczynska, A. Health Action Process Approach. In Predicting Health Behaviour, 3rd ed.; Conner, M., Norman, P., Eds.; McGraw Hill Open University Press: Maidenhead, UK, 2015; pp. 252–278. [Google Scholar]
- Zhou, G.; Gan, Y.; Ke, Q.; Knoll, N.; Lonsdale, C.; Schwarzer, R. Avoiding exposure to air pollution by using filtering facemask respirators: An application of the health action process approach. Health Psychol. 2016, 35, 141–147. [Google Scholar] [CrossRef]
- Ajzen, I. Attitudes and persuasion. In The Oxford Handbook of Personality and Social Psychology; Deaux, K., Snyder, M., Eds.; Oxford University Press: Oxford, UK, 2012; pp. 367–393. [Google Scholar]
- Albarracín, D.; Chan, M.P.S.; Jiang, D. Attitudes and attitude change: Social and personality considerations about specific and general patterns of behavior. In The Oxford Handbook of Personality and Social Psychology, 2nd ed.; Oxford University Press: Oxford, UK, 2018; pp. 439–464. [Google Scholar]
- Ajzen, I. Constructing a TPB Questionnaire: Conceptual and Methodological Considerations. 2002. Available online: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.601.956&rep=rep1&type=pdf (accessed on 10 November 2021).
- Conner, M. Social cognitions in health behaviour. In Assessment in Health Psychology; Benyamini, Y., Johnston, M., Karademas, E.C., Eds.; Hogrefe Publishing: Gottingen, Germany, 2016. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Soper, D.S. A-priori Sample Size Calculator for Structural Equation Models. 2021. Available online: https://www.danielsoper.com/statcalc (accessed on 10 November 2021).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Westland, J.C. Lower bounds on sample size in structural equation modeling. Electron. Commer. Res. Appl. 2010, 9, 476–487. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 8th ed.; Cengage Learning: Andover, UK, 2018. [Google Scholar]
- Lubiewska, K.; Głogowska, K. Zastosowanie analizy równoważności pomiarowej w badaniach psychologicznych. Pol. Forum Psychol. 2018, 23, 330–356. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of Goodness of Fit Indexes to Lack of Measurement Invariance. Struct. Equ. Model. A Multidiscip. J. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Jöreskog, K.G. Simultaneous factor analysis in several populations. Psychometrika 1971, 36, 409–426. [Google Scholar] [CrossRef]
- Sorbom, D. A general method for studying differences in factor means and factor structures between groups. Br. J. Math. Stat. Psychol. 1974, 27, 229–239. [Google Scholar] [CrossRef]
- Rachiotis, G.; Papagiannis, D.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Daniil, Z.; Gourgoulianis, K.I. Determinants of Influenza Vaccination Coverage among Greek Health Care Workers amid COVID-19 Pandemic. Infect. Dis. Rep. 2021, 13, 71. [Google Scholar] [CrossRef]
- Bachtiger, P.; Adamson, A.; Chow, J.-J.; Sisodia, R.; Quint, J.K.; Peters, N.S. The Impact of the COVID-19 Pandemic on the Uptake of Influenza Vaccine: UK-Wide Observational Study. JMIR Public Health Surveill. 2021, 7, e26734. [Google Scholar] [CrossRef]
- Karafillakis, E.; Larson, H.J. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine 2017, 35, 4840–4850. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Losada, M.F. Positive Affect and the Complex Dynamics of Human Flourishing. Am. Psychol. 2005, 60, 678–686. [Google Scholar] [CrossRef]
- Sabey, C.V.; Charlton, C.; Charlton, S.R. The “Magic” Positive-to-Negative Interaction Ratio: Benefits, Applications, Cautions, and Recommendations. J. Emot. Behav. Disord. 2018, 27, 154–164. [Google Scholar] [CrossRef]
- De Langhe, B.; Puntoni, S. Bang for the Buck: Gain-Loss Ratio as a Driver of Judgment and Choice. Manag. Sci. 2015, 61, 1137–1163. [Google Scholar] [CrossRef]
- Wansink, B.; Pope, L. When do gain-framed health messages work better than fear appeals? Nutr. Rev. 2014, 73, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Keller, P.A.; Lehmann, D.R. Designing Effective Health Communications: A Meta-Analysis. J. Public Policy Mark. 2008, 27, 117–130. [Google Scholar] [CrossRef]
- Weinstein, N.D.; Sandman, P.M. A model of the precaution adoption process: Evidence from home radon testing. Health Psychol. 1992, 11, 170–180. [Google Scholar] [CrossRef]
- Bhugra, P.; Grandhi, G.R.; Mszar, R.; Satish, P.; Singh, R.; Blaha, M.; Blankstein, R.; Virani, S.S.; Cainzos-Achirica, M.; Nasir, K. Determinants of Influenza Vaccine Uptake in Patients With Cardiovascular Disease and Strategies for Improvement. J. Am. Heart Assoc. 2021, 10, e019671. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Ortiz-Sánchez, E.; Velando-Soriano, A.; Pradas-Hernández, L.; Vargas-Román, K.; Gómez-Urquiza, J.L.; La Fuente, G.A.C.-D.; Albendín-García, L. Analysis of the Anti-Vaccine Movement in Social Networks: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5394. [Google Scholar] [CrossRef]
- Ling, M.; Kothe, E.J.; Mullan, B. Predicting intention to receive a seasonal influenza vaccination using Protection Motivation Theory. Soc. Sci. Med. 2019, 233, 87–92. [Google Scholar] [CrossRef]
- Real, K.; Kim, S.; Conigliaro, J. Using a validated health promotion tool to improve patient safety and increase health care personnel influenza vaccination rates. Am. J. Infect. Control. 2013, 41, 691–696. [Google Scholar] [CrossRef]
- Hollmeyer, H.G.; Hayden, F.; Poland, G.; Buchholz, U. Influenza vaccination of health care workers in hospitals—A review of studies on attitudes and predictors. Vaccine 2009, 27, 3935–3944. [Google Scholar] [CrossRef]
- Johansen, L.J.; Stenvig, T.; Wey, H. The Decision to Receive Influenza Vaccination Among Nurses in North and South Dakota. Public Health Nurs. 2012, 29, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, B.A.; Ruiter, R.A.C.; Wicker, S.; Chapman, G.; Kok, G. Medical students’ attitude towards influenza vaccination. BMC Infect. Dis. 2015, 15, 185. [Google Scholar] [CrossRef] [PubMed]
- Sprengholz, P.; Felgendreff, L.; Böhm, R.; Betsch, C. Vaccination policy reactance: Predictors, consequences, and countermeasures. 2021. Available online: https://psyarxiv.com/98e4t/download?format=pdf (accessed on 10 November 2021).
- Cameron, C.D.; Brown-Iannuzzi, J.L.; Payne, B.K. Sequential Priming Measures of Implicit Social Cognition. Pers. Soc. Psychol. Rev. 2012, 16, 330–350. [Google Scholar] [CrossRef] [PubMed]

| Variable | Group | M (SD) | t | df | p |
|---|---|---|---|---|---|
| Pro-vaccine beliefs | Medics | 4.44 (0.85) | 15.10 | 702.86 | <0.001 |
| Non-medics | 3.36 (1.06) | ||||
| Antivaccine beliefs | Medics | 1.67 (0.89) | −15.33 | 681.59 | <0.001 |
| Non-medics | 2.76 (1.00) | ||||
| Risk perception | Medics | 2.62 (0.88) | −0.94 | 707 | 0.346 |
| Non-medics | 2.68 (0.83) | ||||
| Perceived gains | Medics | 4.16 (0.89) | 12.55 | 706 | <0.001 |
| Non-medics | 3.25 (0.93) | ||||
| Perceived losses | Medics | 2.10 (0.82) | −14.24 | 642.14 | <0.001 |
| Non-medics | 2.99 90.81) | ||||
| Facilitators’ relevance | Medics | 3.36 (1.06) | 4.30 | 632.35 | <0.001 |
| Non-medics | 3.02 (1.02) | ||||
| Vaccination self-efficacy | Medics | 3.69 (1.48) | 10.10 | 546.64 | <0.001 |
| Non-medics | 3.02 (1.02) |
| Chi-Square | RMSEA | Probability RMSEA ≤ 0.05 | CFI | TLI | SRMR | |
|---|---|---|---|---|---|---|
| Medics | 1844.897 ***, df = 1076 | 0.049 | 0.708 | 0.922 | 0.916 | 0.063 |
| Non-medics | 2162.701 ***, df = 1076 | 0.050 | 0.549 | 0.926 | 0.920 | 0.066 |
| Effect (From–To) | Group | Estimate | SE | P |
|---|---|---|---|---|
| FacRel–VacSE–Intention/vac | Medics | 0.235 | 0.076 | 0.002 |
| Non-medics | 0.260 | 0.043 | <0.001 | |
| VacPros–VacGains–VacSE | Medics | 1.764 | 0.453 | <0.001 |
| Non-medics | 0.239 | 0.066 | <0.001 | |
| VacPros–FacRel–VacSE | Medics | 1.120 | 0.531 | 0.035 |
| Non-medics | 0.296 | 0.048 | <0.001 | |
| VacCons–VacGains–VacSE | Medics | 0.798 | 0.390 | 0.040 |
| Non-medics | −0.042 | 0.022 | 0.056 | |
| VacCons–VacLosses–VacSE | Medics | – | – | – |
| Non-medics | −0.286 | 0.085 | 0.001 | |
| VacCons–FacRel–VacSE | Medics | – | – | – |
| Non-medics | −0.107 | 0.040 | 0.007 | |
| Risk–VacLosses–VacSE | Medics | – | – | – |
| Non-medics | 0.083 | 0.030 | 0.006 | |
| Risk–FacRel–VacSE | Medics | – | – | – |
| Non-medics | 0.249 | 0.052 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Włodarczyk, D.; Ziętalewicz, U. Medics as a Positive Deviant in Influenza Vaccination: The Role of Vaccine Beliefs, Self-Efficacy and Contextual Variables. Vaccines 2022, 10, 723. https://doi.org/10.3390/vaccines10050723
Włodarczyk D, Ziętalewicz U. Medics as a Positive Deviant in Influenza Vaccination: The Role of Vaccine Beliefs, Self-Efficacy and Contextual Variables. Vaccines. 2022; 10(5):723. https://doi.org/10.3390/vaccines10050723
Chicago/Turabian StyleWłodarczyk, Dorota, and Urszula Ziętalewicz. 2022. "Medics as a Positive Deviant in Influenza Vaccination: The Role of Vaccine Beliefs, Self-Efficacy and Contextual Variables" Vaccines 10, no. 5: 723. https://doi.org/10.3390/vaccines10050723
APA StyleWłodarczyk, D., & Ziętalewicz, U. (2022). Medics as a Positive Deviant in Influenza Vaccination: The Role of Vaccine Beliefs, Self-Efficacy and Contextual Variables. Vaccines, 10(5), 723. https://doi.org/10.3390/vaccines10050723







