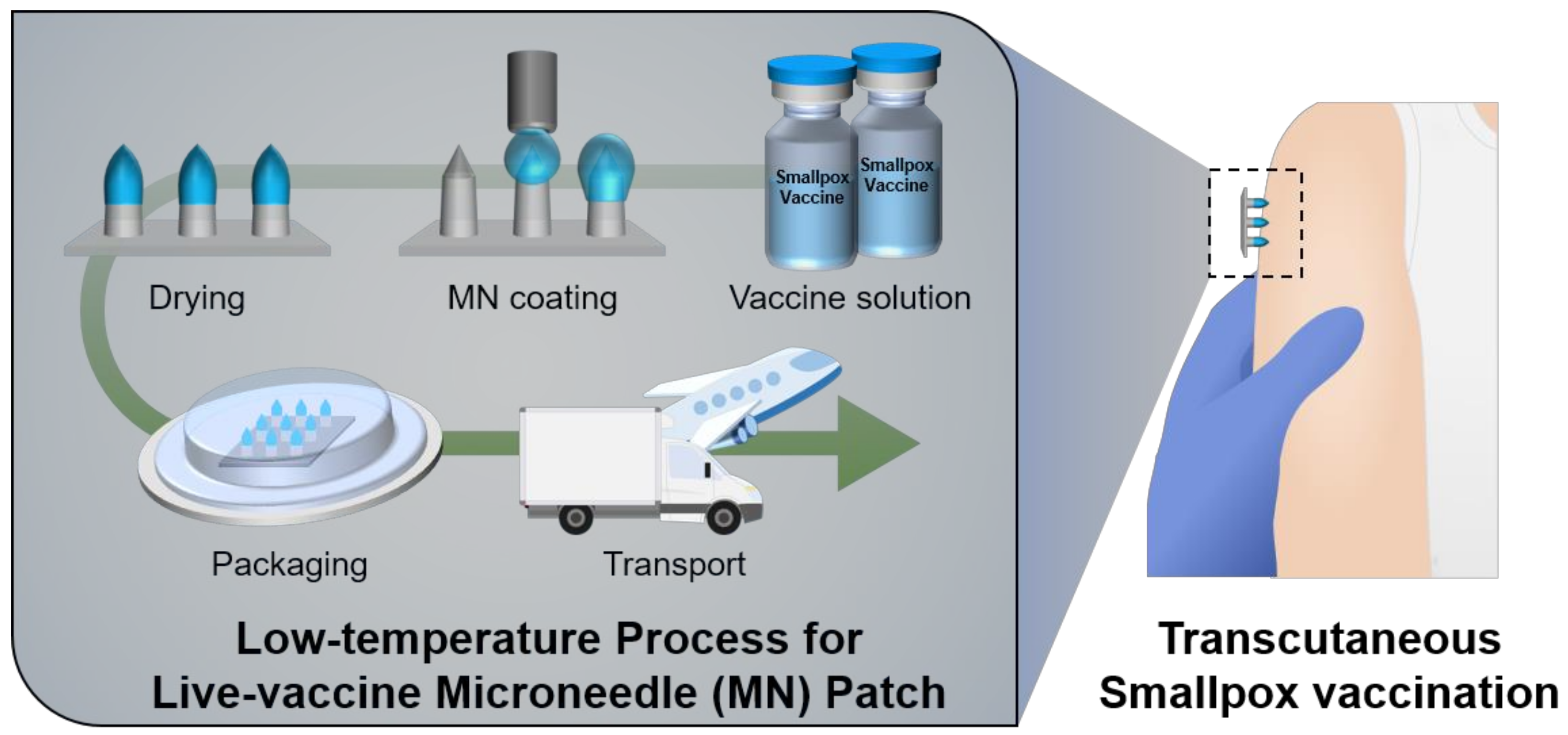
Low-Temperature Multiple Micro-Dispensing on Microneedles for Accurate Transcutaneous Smallpox Vaccination
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Coating Solutions
2.2. Fabrication of Coated MNs Using Contact Dispensing System
2.3. Plaque Assay
2.4. Animals and Care
2.5. In Vivo Vaccination Test
2.6. Analysis of Neutralizing Antibody Responses after Vaccination
2.7. Enzyme-Linked Immunosorbent Spot (ELISPOT) Assay
2.8. Long-Term Storage Tests
2.9. Statistical Analysis
3. Results and Discussion
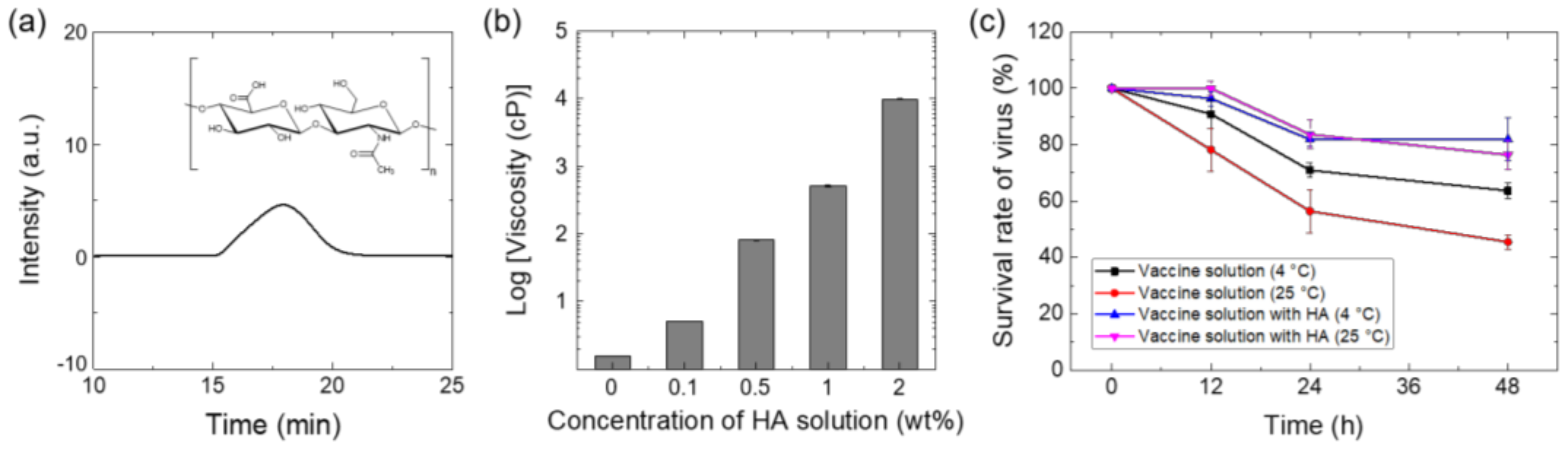
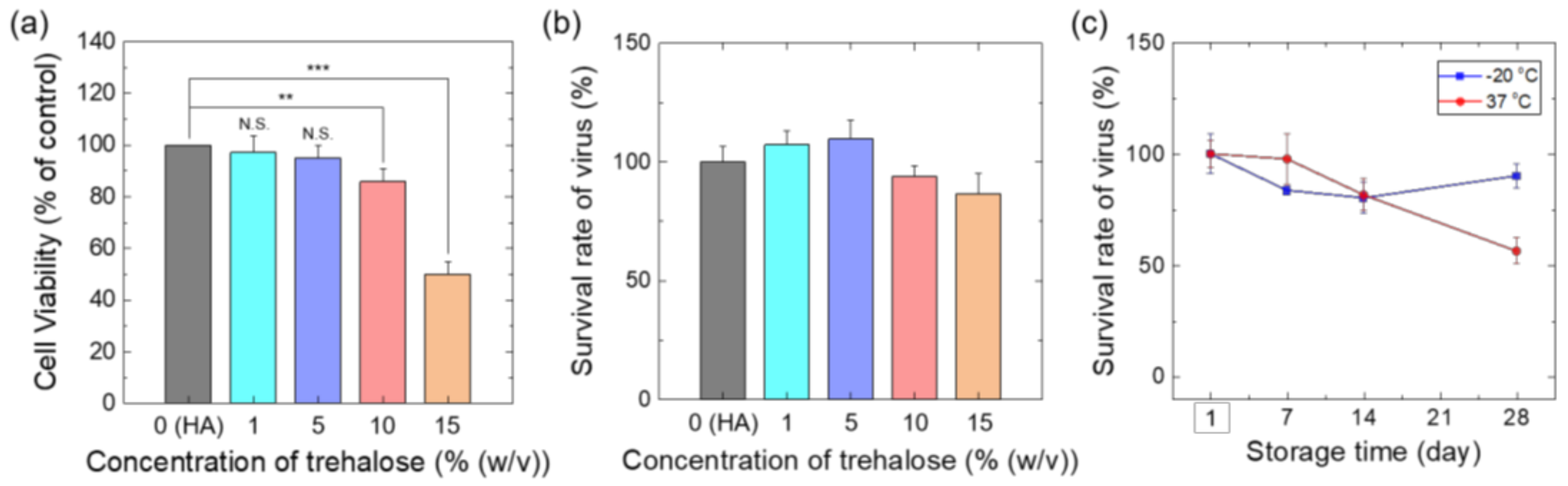
3.1. Preparation of Vaccine Coating Solutions
3.2. Selective and Precise Vaccine Coating on MN Tips Using Low-Temperature Multiple Dispensing System
3.3. In Vivo Smallpox Vaccination Tests Using Live Vaccina-Coated MN Patches
3.4. Storage Stability Test of MN Vaccines
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Behbehani, A.M. The smallpox story: Life and death of an old disease. Microbiol. Rev. 1983, 47, 455–509. [Google Scholar] [CrossRef] [PubMed]
- Henderson, D.A. Smallpox: Clinical and epidemiologic features. Emerg. Infect. Dis. 1999, 5, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Halloran, M.E.; Longini, I.M., Jr.; Nizam, A.; Yang, Y. Containing Bioterrorist Smallpox. Science 2002, 298, 1428–1432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, Z.S.; Seward, J.F.; Lane, J.M. Smallpox. Lancet 2006, 367, 425–435. [Google Scholar] [CrossRef]
- Ferguson, N.; Keeling, M.; Edmunds, W.J.; Gani, R.; Grenfell, B.T.; Anderson, R.M.; Leach, S. Planning for smallpox outbreaks. Nature 2003, 425, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Longini, I.M., Jr.; Halloran, M.E.; Nizam, A.; Yang, Y.; Xu, S.; Burke, D.S.; Cummings, D.A.; Epstein, J.M. Containing a large bioterrorist smallpox attack: A computer simulation approach. Int. J. Infect. Dis. 2007, 11, 98–108. [Google Scholar] [CrossRef] [Green Version]
- Artenstein, A.W.; Johnson, C.; Marbury, T.C.; Morrison, D.; Blum, P.S.; Kemp, T.; Nichols, R.; Balser, J.P.; Currie, M.; Monath, T.P. A novel, cell culture-derived smallpox vaccine in vaccinia-naive adults. Vaccine 2005, 23, 3301–3309. [Google Scholar] [CrossRef]
- Fulginiti, V.A.; Papier, A.; Lane, J.M.; Neff, J.M.; Henderson, D.A. Smallpox vaccination: A review, part II. Adverse events. Clin. Infect. Dis. 2003, 37, 251–271. [Google Scholar] [CrossRef] [Green Version]
- Slifka, M.K.; Hanifin, J.M. Smallpox: The basics. Dermatol. Clin. 2004, 22, 263–274. [Google Scholar] [CrossRef]
- Lofquist, J.M.; Weimert, N.A.; Hayney, M.S. Smallpox: A review of clinical disease and vaccination. Am. J. Health Syst. Pharm. 2003, 60, 749–756. [Google Scholar] [CrossRef]
- Fenner, F.; Henderson, D.A.; Arita, I.; Jezek, Z.; Ladnyi, I.D. Smallpox and Its Eradication; WHO: Geneva, Switzerland, 1988. [Google Scholar]
- Breman, J.G.; Henderson, D.A. Diagnosis and Management of Smallpox. N. Engl. J. Med. 2002, 346, 1300–1308. [Google Scholar] [CrossRef] [PubMed]
- Henderson, D.A.; Inglesby, T.V.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Jahrling, P.B.; Hauer, J.; Layton, M.; McDade, J.; Osterholm, M.T.; et al. Smallpox as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 1999, 281, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- Phelps, A.; Gates, A.J.; Eastaugh, L.; Hillier, M.; Ulaeto, D.O. Comparative Efficacy of Intramuscular and Scarification Routes of Administration of Live Smallpox Vaccine in a Murine Challenge Model. Vaccine 2017, 35, 3889–3896. [Google Scholar] [CrossRef]
- Weltzin, R.; Liu, J.; Pugachev, K.; Myers, G.A.; Coughlin, B.; Blum, P.S.; Nichols, R.; Johnson, C.; Cruz, J.; Kennedy, J.S.; et al. Clonal vaccinia virus grown in cell culture as a new smallpox vaccine. Nat. Med. 2003, 9, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Nagao, S.; Inaba, S.; Iijima, S. Langerhans cells at the sites of vaccinia virus inoculation. Arch. Dermatol. Res. 1976, 256, 23–31. [Google Scholar] [CrossRef]
- Baxby, D. Smallpox vaccination techniques; from knives and forks to needles and pins. Vaccine 2002, 20, 2140–2149. [Google Scholar] [CrossRef]
- Monath, T.P.; Caldwell, J.R.; Mundt, W.; Fusco, J.; Johnson, C.S.; Buller, M.; Liu, J.; Gardner, B.; Downing, G.; Blum, P.S. ACAM2000 clonal Vero cell culture vaccinia virus (New York City Board of Health strain)–a second-generation smallpox vaccine for biological defense. Int. J. Infect. Dis. 2004, 8, 31–44. [Google Scholar] [CrossRef] [Green Version]
- Rogers, B.; Dennison, K.; Adepoju, N.; Dowd, S.; Uedoi, K. Vaccine cold chain: Part 1. proper handling and storage of vaccine. AAOHN J. 2010, 58, 337. [Google Scholar] [CrossRef] [Green Version]
- Lloyd, J.; Cheyne, J. The origins of the vaccine cold chain and a glimpse of the future. Vaccine 2017, 35, 2115–2120. [Google Scholar] [CrossRef]
- Liu, L.; Zhong, Q.; Tian, T.; Dubin, K.; Athale, S.K.; Kupper, T.S. Epidermal injury and infection during poxvirus immunization is crucial for the generation of highly protective T cell-mediated immunity. Nat. Med. 2010, 16, 224–227. [Google Scholar] [CrossRef] [Green Version]
- Rice, A.D.; Adams, M.M.; Lindsey, S.F.; Swetnam, D.M.; Manning, B.R.; Smith, A.J.; Burrage, A.M.; Wallace, G.; MacNeill, A.L.; Moyer, R.W. Protective properties of vaccinia virus-based vaccines: Skin scarification promotes a nonspecific immune response that protects against orthopoxvirus disease. J. Virol. 2014, 88, 7753–7763. [Google Scholar] [CrossRef] [Green Version]
- Millar, J.D.; Roberto, R.R.; Wulff, H.; Wenner, H.A.; Henderson, D.A. Smallpox vaccination by intradermal jet injection. I. Introduction, background and results of pilot studies. Bull. World Health Organ. 1969, 41, 749–760. [Google Scholar] [PubMed]
- Neff, J.M.; Millar, J.D.; Roberto, R.R.; Wulff, H. Smallpox vaccination by intradermal jet injection. 3. Evaluation in a well-vaccinated population. Bull. World Health Organ. 1969, 41, 771–778. [Google Scholar]
- Orenstein, W.; Offit, P.; Edwards, K.M.; Plotkin, S. Plotkin’s Vaccines, 7th ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 1001–1030. [Google Scholar]
- Barolet, D.; Benohanian, A. Current trends in needle-free jet injection: An update. Clin. Cosmet. Investig. Dermatol. 2018, 1, 231–238. [Google Scholar] [CrossRef] [Green Version]
- Prausnitz, M.R.; Mikszta, J.A.; Cormier, M.; Andrianov, A.K. Microneedle-based vaccines. Curr. Top. Microbiol. Immunol. 2009, 333, 369–393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Maaden, K.; Jiskoot, W.; Bouwstra, J. Microneedle technologies for (trans)dermal drug and vaccine delivery. J. Control. Release 2012, 161, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.C.; Park, J.H.; Prausnitz, M.R. Microneedles for drug and vaccine delivery. Adv. Drug Deliv. Rev. 2012, 64, 1547–1568. [Google Scholar] [CrossRef] [Green Version]
- Suh, H.; Shin, J.; Kim, Y.C. Microneedle patches for vaccine delivery. Clin. Exp. Vaccine Res. 2014, 3, 42–49. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, S.; Koutsonanos, D.; del Pilar Martin, M.; Lee, J.W.; Zarnitsyn, V.; Choi, S.O.; Murthy, N.; Compans, R.W.; Skountzou, I.; Prausnitz, M.R. Dissolving polymer microneedle patches for influenza vaccination. Nat. Med. 2010, 16, 915–920. [Google Scholar] [CrossRef]
- Marshall, S.; Sahm, L.J.; Moore, A.C. The success of microneedle-mediated vaccine delivery into skin. Hum. Vaccin. Immunother. 2016, 12, 2975–2983. [Google Scholar] [CrossRef] [Green Version]
- Hiraishi, Y.; Nandakumar, S.; Choi, S.O.; Lee, J.W.; Kim, Y.C.; Posey, J.E.; Sable, S.B.; Prausnitz, M.R. Bacillus Calmette-Guérin vaccination using a microneedle patch. Vaccine 2011, 29, 2626–2636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edens, C.; Collins, M.L.; Ayers, J.; Rota, P.A.; Prausnitz, M.R. Measles vaccination using a microneedle patch. Vaccine 2013, 31, 3403–3409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menon, I.; Bagwe, P.; Gomes, K.B.; Bajaj, L.; Gala, R.; Uddin, M.N.; D’Souza, M.J.; Zughaier, S.M. Microneedles: A New Generation Vaccine Delivery System. Micromachines 2021, 12, 435. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.T.M.; Gavitt, T.D.; Farrell, N.J.; Curry, E.J.; Mara, A.B.; Patel, A.; Brown, L.; Kilpatrick, S.; Piotrowska, R.; Mishra, N.; et al. Transdermal microneedles for the programmable burst release of multiple vaccine payloads. Nat. Biomed. Eng. 2021, 5, 998–1007. [Google Scholar] [CrossRef]
- Choi, I.J.; Kang, A.; Ahn, M.H.; Jun, H.; Baek, S.K.; Park, J.H.; Na, W.; Choi, S.O. Insertion-responsive microneedles for rapid intradermal delivery of canine influenza vaccine. J. Control. Release 2018, 286, 460–466. [Google Scholar] [CrossRef]
- McGrath, M.G.; Vrdoljak, A.; O’Mahony, C.; Oliveira, J.C.; Moore, A.C.; Crean, A.M. Determination of parameters for successful spray coating of silicon microneedle arrays. Int. J. Pharm. 2011, 415, 140–149. [Google Scholar] [CrossRef] [Green Version]
- Ingrole, R.S.J.; Gill, H.S. Microneedle Coating Methods: A Review with a Perspective. J. Pharmacol. Exp. Ther. 2019, 370, 555–569. [Google Scholar] [CrossRef]
- Ameri, M.; Fan, S.C.; Maa, Y.F. Parathyroid hormone PTH(1-34) formulation that enables uniform coating on a novel transdermal microprojection delivery system. Pharm. Res. 2010, 27, 303–313. [Google Scholar] [CrossRef]
- Baek, S.H.; Shin, J.H.; Kim, Y.C. Drug-coated microneedles for rapid and painless local anesthesia. Biomed. Microdevices 2017, 19, 2. [Google Scholar] [CrossRef]
- Zhang, Y.; Brown, K.; Siebenaler, K.; Determan, A.; Dohmeier, D.; Hansen, K. Development of lidocaine-coated microneedle product for rapid, safe, and prolonged local analgesic action. Pharm. Res. 2012, 29, 170–177. [Google Scholar] [CrossRef]
- Uddin, M.J.; Scoutaris, N.; Klepetsanis, P.; Chowdhry, B.; Prausnitz, M.R.; Douroumis, D. Inkjet printing of transdermal microneedles for the delivery of anticancer agents. Int. J. Pharm. 2015, 494, 593–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, X.; Coulman, S.A.; Hanna, S.J.; Wong, F.S.; Dayan, C.M.; Birchall, J.C. Formulation of hydrophobic peptides for skin delivery via coated microneedles. J. Control. Release 2017, 265, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Choi, S.J.; Park, W.B.; Kim, H.B.; Kim, N.J.; Oh, M.D.; Choe, K.W. Detailed kinetics of immune responses to a new cell culture-derived smallpox vaccine in vaccinia-naive adults. Vaccine 2007, 25, 6287–6291. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.J.; Cha, H.R.; Hwang, S.J.; Baek, S.K.; Lee, J.M.; Choi, S.O. Live Vaccinia Virus-Coated Microneedle Array Patches for Smallpox Vaccination and Stockpiling. Pharmaceutics 2021, 13, 209. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.Y.; Yim, S.-G.; Hwang, Y. Implantable Microneedle and Manufacturing Method of the Implantable Microneedle. South Korea Patent No. 10-2238033 2 April 2021. [Google Scholar]
- Zehentbauer, F.M.; Moretto, C.; Stephen, R.; Thevar, T.; Gilchrist, J.R.; Pokrajac, D.; Richard, K.L.; Kiefer, J. Fluorescence spectroscopy of Rhodamine 6G: Concentration and solvent effects. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2014, 121, 147–151. [Google Scholar] [CrossRef]
- Tauber, E.; Kollaritsch, H.; Korinek, M.; Rendi-Wagner, P.; Jilma, B.; Firbas, C.; Schranz, S.; Jong, E.; Klingler, A.; Dewasthaly, S.; et al. Safety and immunogenicity of a Vero-cell-derived, inactivated Japanese encephalitis vaccine: A non-inferiority, phase III, randomised controlled trial. Lancet 2007, 370, 1847–1853. [Google Scholar] [CrossRef]
- Huang, G.; Huang, H. Application of hyaluronic acid as carriers in drug delivery. Drug Deliv. 2018, 25, 766–772. [Google Scholar] [CrossRef]
- Snetkov, P.; Zakharova, K.; Morozkina, S.; Olekhnovich, R.; Uspenskaya, M. Hyaluronic Acid: The Influence of Molecular Weight on Structural, Physical, Physico-Chemical, and Degradable Properties of Biopolymer. Polymers 2020, 12, 1800. [Google Scholar] [CrossRef]
- World Health Organization Summary Report on First, Second and Third Generation Smallpox Vaccines. Available online: http://www.who.int/immunization/sage/meetings/2013/november/2_Smallpox_vaccine_review_updated_11_10_13.pdf (accessed on 1 November 2016).
- Poland, G.A.; Grabenstein, J.D.; Neff, J.M. The US smallpox vaccination program: A review of a large modern era smallpox vaccination implementation program. Vaccine 2005, 23, 2078–2081. [Google Scholar] [CrossRef]
- Overton, E.T.; Lawrence, S.J.; Wagner, E.; Nopora, K.; Rösch, S.; Young, P.; Schmidt, D.; Kreusel, C.; De Carli, S.; Meyer, T.P.; et al. Immunogenicity and safety of three consecutive production lots of the non replicating smallpox vaccine MVA: A randomised, double blind, placebo controlled phase III trial. PLoS ONE 2018, 13, e0195897. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonilla-Guerrero, R.; Poland, G.A. Smallpox vaccines: Current and future. J. Lab. Clin. Med. 2003, 142, 252–257. [Google Scholar] [CrossRef]
- Malonis, R.J.; Lai, J.R.; Vergnolle, O. Peptide-Based Vaccines: Current Progress and Future Challenges. Chem. Rev. 2020, 120, 3210–3229. [Google Scholar] [CrossRef] [Green Version]
- Lim, H.; In, H.J.; Kim, Y.J.; Jang, S.; Lee, Y.H.; Kim, S.H.; Lee, S.H.; Park, J.H.; Yang, H.J.; Yoo, J.S.; et al. Development of an attenuated smallpox vaccine candidate: The KVAC103 strain. Vaccine 2021, 39, 5214–5223. [Google Scholar] [CrossRef] [PubMed]
- Tran, L.G.; Park, W.T. Rapid biodegradable microneedles with allergen reservoir for skin allergy test. Micro Nano Syst. Lett. 2020, 8, 11. [Google Scholar] [CrossRef]
- Ohtake, S.; Wang, Y.J. Trehalose: Current use and future applications. J. Pharm. Sci. 2011, 100, 2020–2053. [Google Scholar] [CrossRef] [PubMed]
- Leung, V.; Mapletoft, J.; Zhang, A.; Lee, A.; Vahedi, F.; Chew, M.; Szewczyk, A.; Jahanshahi-Anbuhi, S.; Ang, J.; Cowbrough, B.; et al. Thermal Stabilization of Viral Vaccines in Low-Cost Sugar Films. Sci. Rep. 2019, 9, 7631. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.J.; Bondy, B.J.; Yoo, D.G.; Compans, R.W.; Kang, S.M.; Prausnitz, M.R. Stability of whole inactivated influenza virus vaccine during coating onto metal microneedles. J. Control. Release 2013, 166, 159–171. [Google Scholar] [CrossRef] [Green Version]
- Kolluru, C.; Gomaa, Y.; Prausnitz, M.R. Development of a thermostable microneedle patch for polio vaccination. Drug Deliv. Transl. Res. 2019, 9, 192–203. [Google Scholar] [CrossRef] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yim, S.-G.; Hwang, Y.-H.; An, S.; Seong, K.-Y.; Kim, S.-Y.; Kim, S.; Lee, H.; Lee, K.-O.; Kim, M.-Y.; Kim, D.; et al. Low-Temperature Multiple Micro-Dispensing on Microneedles for Accurate Transcutaneous Smallpox Vaccination. Vaccines 2022, 10, 561. https://doi.org/10.3390/vaccines10040561
Yim S-G, Hwang Y-H, An S, Seong K-Y, Kim S-Y, Kim S, Lee H, Lee K-O, Kim M-Y, Kim D, et al. Low-Temperature Multiple Micro-Dispensing on Microneedles for Accurate Transcutaneous Smallpox Vaccination. Vaccines. 2022; 10(4):561. https://doi.org/10.3390/vaccines10040561
Chicago/Turabian StyleYim, Sang-Gu, Yun-Ho Hwang, Seonyeong An, Keum-Yong Seong, Seo-Yeon Kim, Semin Kim, Hyeseon Lee, Kang-Oh Lee, Mi-Young Kim, Dokeun Kim, and et al. 2022. "Low-Temperature Multiple Micro-Dispensing on Microneedles for Accurate Transcutaneous Smallpox Vaccination" Vaccines 10, no. 4: 561. https://doi.org/10.3390/vaccines10040561
APA StyleYim, S.-G., Hwang, Y.-H., An, S., Seong, K.-Y., Kim, S.-Y., Kim, S., Lee, H., Lee, K.-O., Kim, M.-Y., Kim, D., Kim, Y.-J., & Yang, S.-Y. (2022). Low-Temperature Multiple Micro-Dispensing on Microneedles for Accurate Transcutaneous Smallpox Vaccination. Vaccines, 10(4), 561. https://doi.org/10.3390/vaccines10040561




