Real World Estimate of Vaccination Protection in Individuals Hospitalized for COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects and Methods
2.3. Statistical Analyses
2.4. Ethics Consideration
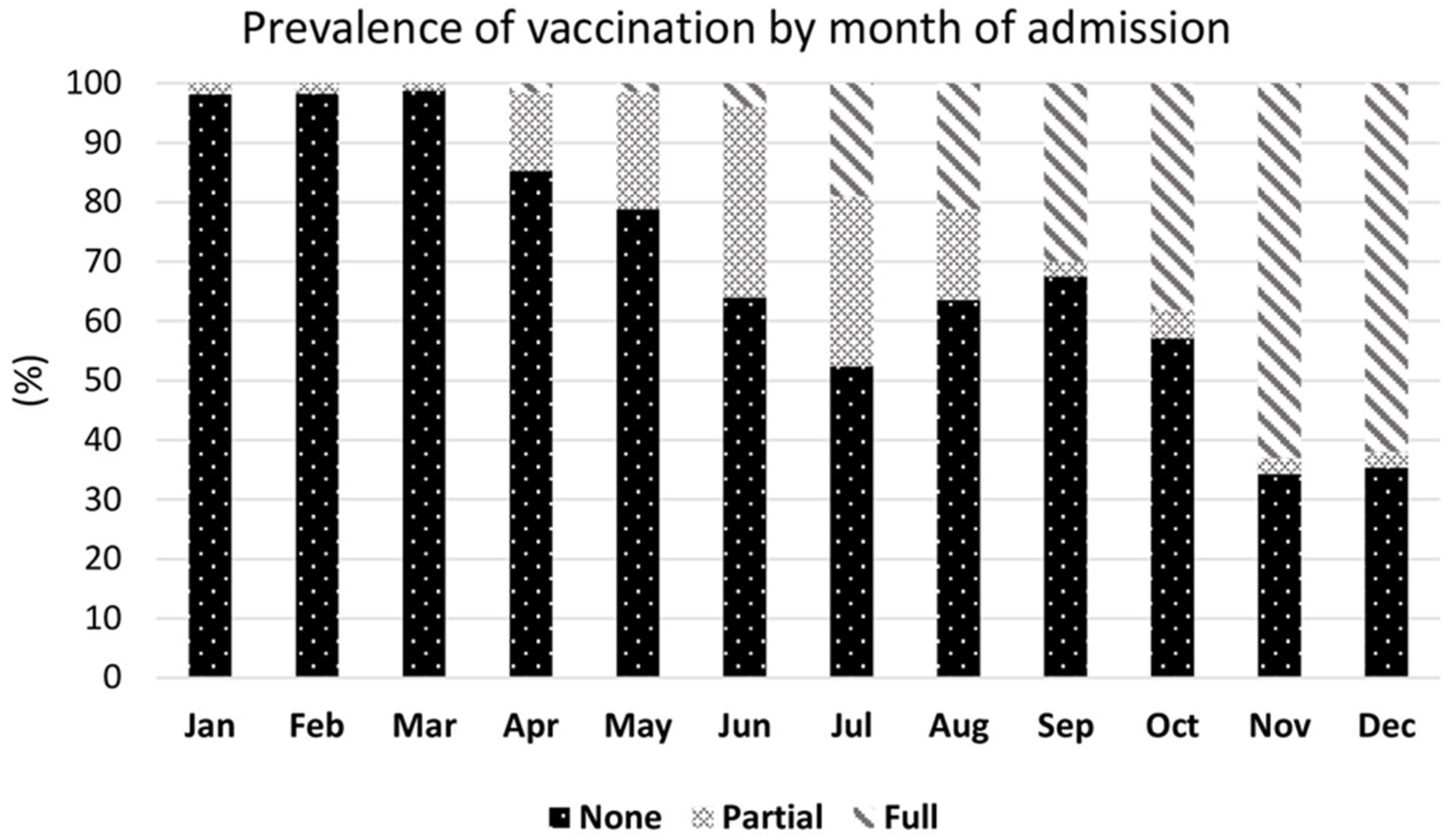
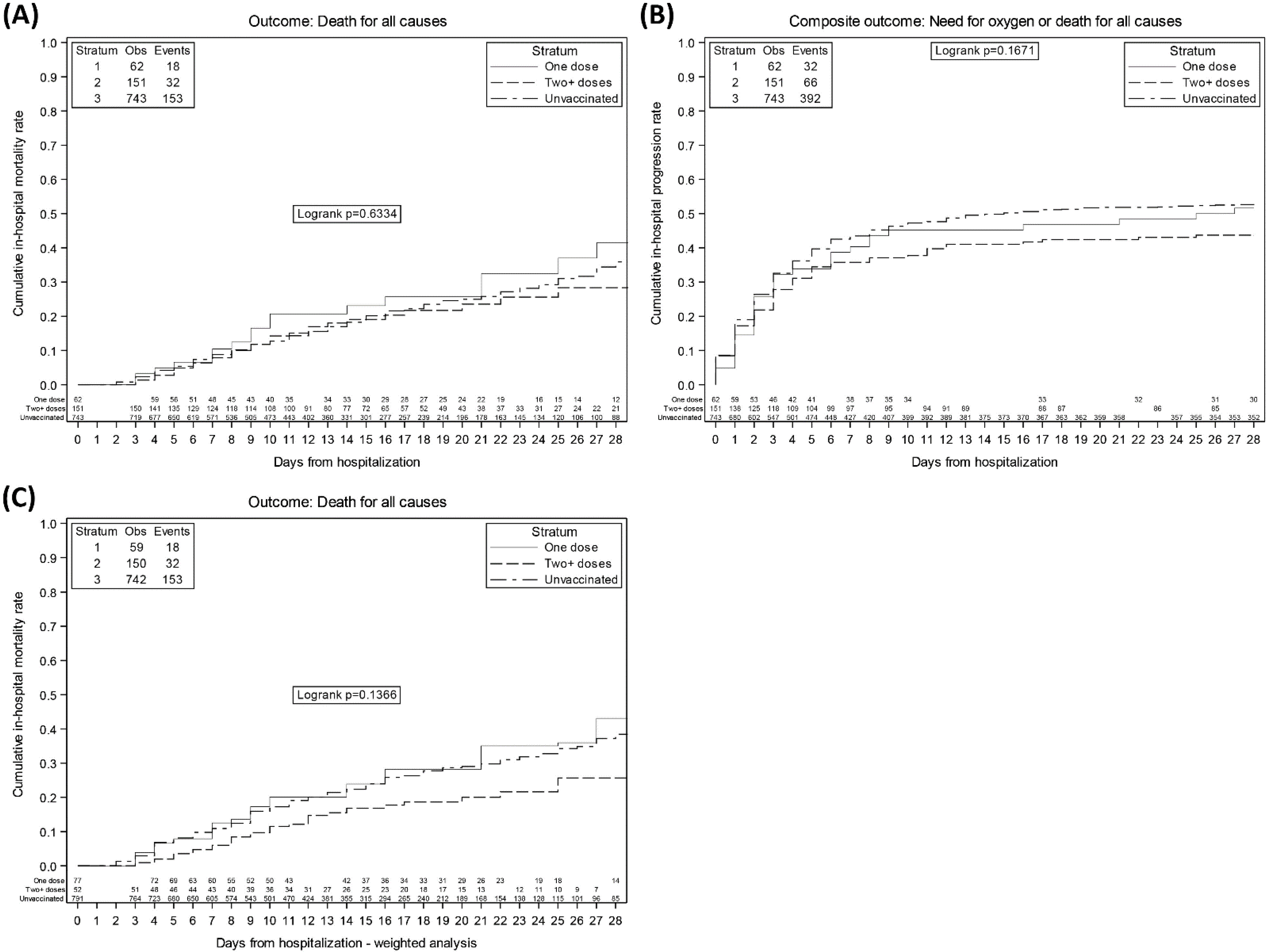
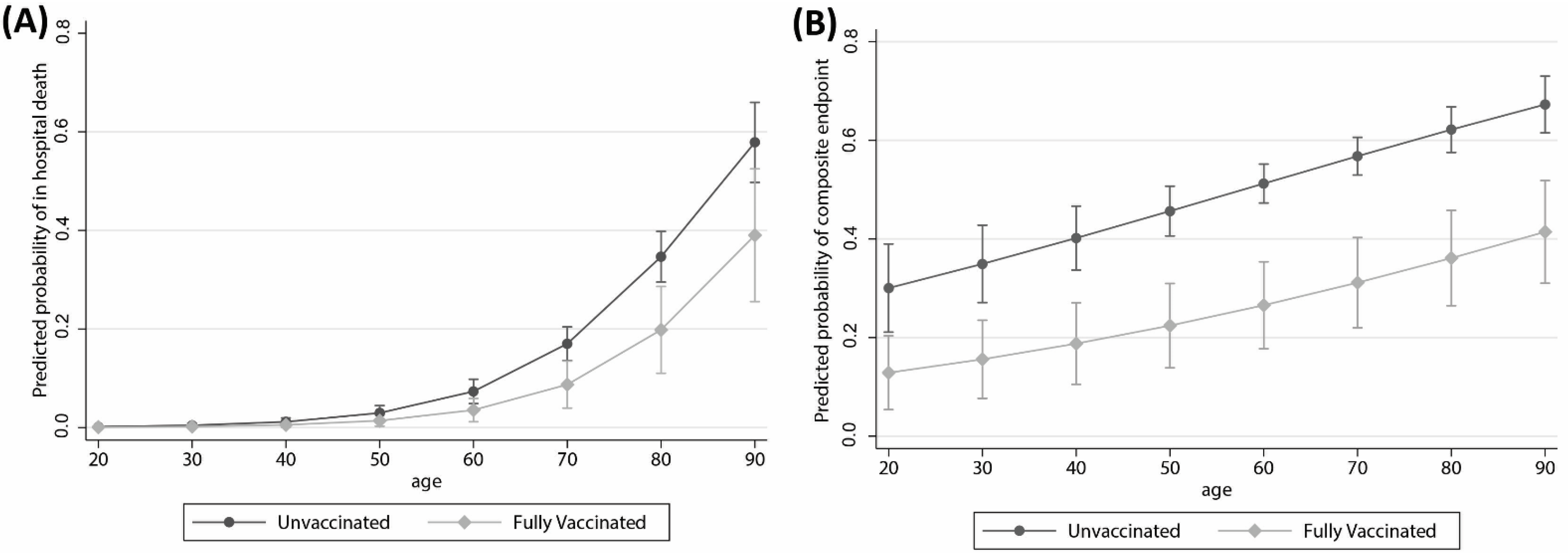
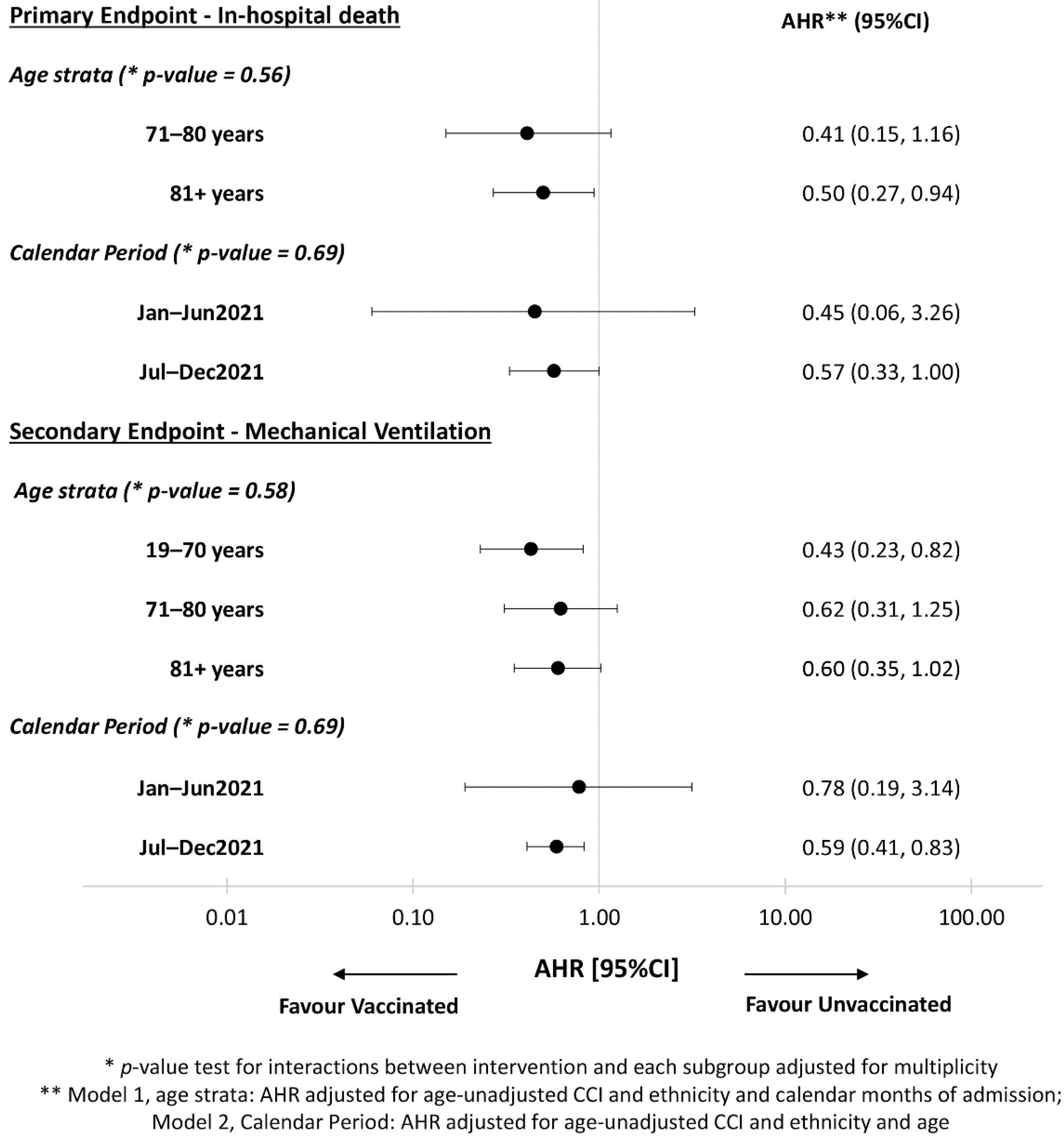
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Weekly Epidemiological Update on COVID-19-28 December 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-COVID-19---28-december-2021 (accessed on 8 February 2022).
- European Centre for Disease Prevention and Control. SARS-CoV-2 Variants of Concern as of 03 February 2022. Available online: https://www.ecdc.europa.eu/en/COVID-19/variants-concern (accessed on 8 February 2022).
- Scobie, H.M.; Johnson, A.G.; Suthar, A.B.; Severson, R.; Alden, N.B.; Balter, S.; Bertolino, D.; Blythe, D.; Brady, S.; Cadwell, B.; et al. Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status—13 U.S. Jurisdictions, April 4–July 17, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1284. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Voysey, M.; Costa Clemens, S.A.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomized controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Sadoff, J.; Gray, G.; Vandebosch, A.; Cárdenas, V.; Shukarev, G.; Grinsztejn, B.; Goepfert, P.A.; Truyers, C.; Fennema, H.; Spiessens, B.; et al. Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against COVID-19. N. Engl. J. Med. 2021, 384, 2187–2201. [Google Scholar] [CrossRef]
- EMA: COVID-19 Vaccines: Studies for Approval. Available online: https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-COVID-19/treatments-vaccines/vaccines-COVID-19/COVID-19-vaccines-studies-approval (accessed on 8 February 2022).
- Dal-Ré, F.; Bekker, L.G.; Gluud, C.; Holm, S.; Jha, V.; A Poland, G.; Rosendaal, F.R.; Schwarzer-Daum, B.; Sevene, E.; Tinto, H.; et al. Ongoing and future COVID-19 vaccine clinical trials: Challenges and opportunities. Lancet Infec. Dis. 2021, 21, e342–e347. [Google Scholar] [CrossRef]
- Meslé, M.M.; Brown, J.; Mook, P.; Hagan, J.; Pastore, R.; Bundle, N.; Spiteri, G.; Ravasi, G.; Nicolay, N.; Andrews, N.; et al. Estimated number of deaths directly averted in people 60 years and older as a result of COVID-19 vaccination in the WHO European Region, December 2020 to November 2021. Eurosurveillance 2021, 26, 2101021. [Google Scholar] [CrossRef]
- Wolter, N.; Jassat, W.; Walaza, S.; Welch, R.; Moultrie, H.; Groome, M.; Amoako, D.G.; Everatt, J.; Bhiman, J.N.; Scheepers, C.; et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: A data linkage study. Lancet 2022, 399, 437–446. [Google Scholar] [CrossRef]
- Ledford, H. How severe are Omicron infections? Nature 2021, 600, 577–578. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- D’Arminio Monforte, A.; Tavelli, A.; Bai, F.; Tomasoni, D.; Falcinella, C.; Castoldi, R.; Barbanotti, D.; Mulè, G.; Allegrini, M.; Suardi, E.; et al. Declining Mortality Rate of Hospitalised Patients in the Second Wave of the COVID-19 Epidemics in Italy: Risk Factors and the Age-Specific Patterns. Life 2021, 11, 979. [Google Scholar] [CrossRef]
- Ben-Yehuda, A.; Weksler, M.E. Immune senescence: Mechanisms and clinical implications. Cancer Investig. 1992, 10, 525–531. [Google Scholar] [CrossRef]
- Macedo, A.; Goncalves, N.; Febra, C. COVID-19 fatality rates in hospitalized patients: Systematic review and meta-analysis. Ann. Epidemiol. 2021, 57, 14–21. [Google Scholar] [CrossRef]
- Odone, A.; Delmonte, D.; Scognamiglio, T.; Signorelli, C. COVID-19 deaths in Lombardy, Italy: Data in context. Lancet Public Health 2020, 5, e310. [Google Scholar] [CrossRef]
- De Angelis, E.; Renzetti, S.; Volta, M.L.; Donato, F.; Calza, S.; Placidi, D.; Lucchini, R.G.; Rota, M. COVID-19 incidence and mortality in Lombardy, Italy: An ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ. Res. 2021, 195, 110777. [Google Scholar] [CrossRef]
- d’Arminio Monforte, A.; Tavelli, A.; Bai, F.; Tomasoni, D.; Falcinella, C.; Castoldi, R.; Barbanotti, D.; Mulè, G.; Allegrini, M.; Tesoro, D.; et al. The importance of patients’ case-mix for the correct interpretation of the hospital fatality rate in COVID-19 disease. Int. J. Infect. Dis. 2020, 100, 67–74. [Google Scholar] [CrossRef]
- van Halem, K.; Bruyndonckx, R.; van der Hilst, J. Risk factors for mortality in hospitalized patients with COVID-19 at the start of the pandemic in Belgium: A retrospective cohort study. BMC Infect. Dis. 2020, 20, 897. [Google Scholar] [CrossRef]
- Barda, N.; Dagan, N.; Cohen, C.; Hernán, M.A.; Lipsitch, M.; Kohane, I.S.; Reis, B.Y.; Balicer, R.D. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: An observational study. Lancet 2021, 398, 2093–2100. [Google Scholar] [CrossRef]
- Thompson, M.G.; Natarajan, K.; Irving, S.A.; Rowley, E.A.; Griggs, E.P.; Gaglani, M.; Klein, N.P.; Grannis, S.J.; DeSilva, M.B.; Stenehjem, E.; et al. Effectiveness of a Third Dose of mRNA Vaccines Against COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults during Periods of Delta and Omicron Variant Predominance-VISION Network, 10 States, August 2021–January 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 139–145. [Google Scholar]
- Prevalenza e Distribuzione Delle Varianti del Virus SARS-CoV-2 di Interesse Per la Sanità Pubblica in Italia. Available online: https://www.epicentro.iss.it/coronavirus/pdf/sars-cov-2-monitoraggio-varianti-rapporti-periodici-23-luglio-2021.pdf (accessed on 24 March 2022).
- Cicalini, S.; Vergori, A.; Cozzi-Lepri, A.; Meschi, S.; Bordoni, V.; Lanini, S.; Lapa, D.; Mariotti, D.; De Pascale, L.; D’aquila, V.; et al. Durability of SARS-CoV-2 mRNA Vaccine immune response in PLWH with advanced disease. In Proceedings of the 29th Conference on Retroviruses on Opportunistic Infections, Online, 12–16 February 2022; Abstract n. 291. Available online: https://www.croiconference.org/abstract/durability-of-sars-cov-2-mrna-vaccine-immune-response-in-plwh-with-advanced-disease/ (accessed on 24 March 2022).
- Tenforde, M.W.; Self, W.H.; Adams, K.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Ghamande, S.; Douin, D.J.; Keipp Talbot, H.; Casey, J.D.; et al. Influenza and Other Viruses in the Acutely Ill (IVY) Network. Association Between mRNA Vaccination and COVID-19 Hospitalization and Disease Severity. JAMA 2021, 326, 2043–2054. [Google Scholar] [CrossRef]
- Whittaker, R.; Kristofferson, A.B.; Salamanca, B.V.; Seppälä, E.; Golestani, K.; Kvåle, R.; Watle, S.V.; Buanes, E.A. Length of hospital stay and risk of intensive care admission and in hospital death among COVID-19 patients in Norway: A register-based cohort study comparing patients fully vaccinated with an mRNA vaccine to unvaccinated patients. Clin. Microbiol. Infect. 2022; in press. [Google Scholar] [CrossRef]
- Abu-Raddad, J.L.; Chemaitelly, H.; Bertollini, R. Severity of SARS-CoV-2 Reinfections as Compared with Primary Infections. N. Engl. J. Med. 2021, 385, 2487–2489. [Google Scholar] [CrossRef] [PubMed]
- Christie, B. COVID-19: Early studies give hope omicron is milder than other variants. BMJ 2021, 375, n3144. [Google Scholar] [CrossRef] [PubMed]
- Callaway, E.; Ledford, H. How bad is Omicron? What scientists know so far. Nature 2021, 600, 197–199. [Google Scholar] [CrossRef]
- Regione Lombardia. Dati COVID Aggiornati. Available online: https://www.regione.lombardia.it/wps/portal/istituzionale/HP/coronavirus/dati (accessed on 8 February 2022).
- Arbel, R.; Hammerman, A.; Sergienko, R.; Friger, M.; Peretz, A.; Netzer, D.; Yaron, S. BNT162b2 Vaccine Booster and Mortality Due to COVID-19. N. Engl. J. Med. 2021, 385, 2413–2420. [Google Scholar] [CrossRef]
| Anti COVID-19 Vaccination | |||||
|---|---|---|---|---|---|
| Characteristics | None | 1 Dose | 2+ Doses | p-Value * | Total |
| N = 743 | N = 62 | N = 151 | N = 956 | ||
| Age, years | <0.001 | ||||
| Median (IQR) | 67 (54, 80) | 76 (62, 84) | 80 (69, 84) | 71 (56, 81) | |
| Gender, n(%) | 0.994 | ||||
| Female | 297 (40.0%) | 25 (40.3%) | 61 (40.4%) | 383 (40.1%) | |
| Ethnicity, n(%) | 0.056 | ||||
| Caucasian | 650 (87.6%) | 50 (82.0%) | 145 (96.7%) | 845 (88.7%) | |
| Black | 1 (0.1%) | 0 (0.0%) | 0 (0.0%) | 1 (0.1%) | |
| Asian | 17 (2.3%) | 2 (3.3%) | 0 (0.0%) | 19 (2.0%) | |
| Ispanic | 28 (3.8%) | 2 (3.3%) | 1 (0.7%) | 31 (3.3%) | |
| Other | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Comorbidity, n(%) | |||||
| Obesity | 100 (45.5%) | 3 (42.9%) | 16 (28.6%) | 0.074 | 119 (42.0%) |
| Cancer | 52 (7.0%) | 5 (8.1%) | 29 (19.2%) | <0.001 | 86 (9.0%) |
| Cerebro-vascular disease | 39 (5.2%) | 2 (3.2%) | 13 (8.6%) | 0.184 | 54 (5.6%) |
| Chronic kidney failure | 51 (6.9%) | 4 (6.5%) | 22 (14.6%) | 0.006 | 77 (8.1%) |
| Congestive failure | 21 (2.8%) | 0 (0.0%) | 2 (1.3%) | 0.242 | 23 (2.4%) |
| Connective tissue disease | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Chronic respiratory disease | 59 (7.9%) | 6 (9.7%) | 28 (18.5%) | <0.001 | 93 (9.7%) |
| Dementia | 44 (5.9%) | 9 (14.5%) | 15 (9.9%) | 0.014 | 68 (7.1%) |
| Diabetes mellitus | 145 (19.5%) | 9 (14.5%) | 36 (23.8%) | 0.264 | 190 (19.9%) |
| End stage liver disease | 7 (0.9%) | 0 (0.0%) | 1 (0.7%) | 0.713 | 8 (0.8%) |
| Hematologic disease | 5 (0.7%) | 0 (0.0%) | 5 (3.3%) | 0.010 | 10 (1.0%) |
| HIV/AIDS | 7 (0.9%) | 0 (0.0%) | 2 (1.3%) | 0.662 | 9 (0.9%) |
| Arterial hypertension | 324 (43.6%) | 29 (46.8%) | 86 (57.0%) | 0.011 | 439 (45.9%) |
| Age-unadjusted Charlson Comorbidity Index, mean (SD) | 0.9 (1.8) | 0.7 (1.0) | 1.6 (1.7) | <0.001 | 1.0 (1.8) |
| PO2 | 0.988 | ||||
| Median (IQR) | 70 (61, 83) | 70 (62, 86) | 70 (61, 83) | ||
| Baseline PaO2/FiO2, mmHg | 0.270 | ||||
| Median (IQR) | 300 (243, 348) | 314 (267, 354) | 309 (250, 357) | 302 (248, 348) | |
| 0–250, n(%) | 183 (27.0%) | 12 (22.2%) | 33 (25.0%) | 0.696 | 228 (26.4%) |
| 0–150, n(%) | 57 (8.4%) | 4 (7.4%) | 14 (10.6%) | 0.671 | 75 (8.7%) |
| FiO2 | 0.331 | ||||
| Median (IQR) | 0.2 (0.2, 0.3) | 0.2 (0.2, 0.2) | 0.2 (0.2, 0.3) | 0.2 (0.2, 0.3) | |
| Main delays | |||||
| Days from symptoms onset to hospitalization, median(IQR) | 5 (2, 8) | 5 (3, 6) | 4 (2, 7) | 0.602 | 5 (2, 8) |
| Days from last vaccine dose to symptoms onset, median (IQR) | 7 (2, 18) | 176 (131, 200) | <0.001 | 157 (23, 203) | |
| Type of vaccine: | |||||
| BNT162b2 | 37 (60.0%) | 108 (71.5%) | 145 (68.0%) | ||
| mRNA-1273 | 12 (19.0%) | 10 (6.6%) | 22 (10.3%) | ||
| ChAdOx1 | 13 (21.0%) | 25 (16.6%) | 38 (18.0%) | ||
| mRNA-mRNA | 3 (2.0%) | 3 (1.4%) | |||
| Anti-COVID-19 Vaccination | |||||
|---|---|---|---|---|---|
| Blood Tests | None | 1 Dose | 2+ Doses | p-Value * | Total |
| N = 473 | N = 47 | N = 145 | N = 665 | ||
| Markers, Median (IQR) | |||||
| Haemoglobin, g/dL | 13.5 (12.1, 14.7) | 13.7 (11.7, 15.0) | 12.6 (11.0, 14.1) | 0.002 | 13.2 (11.8, 14.5) |
| White Blood Cells, g/dL | 6.8 (4.7, 9.4) | 6.1 (4.7, 9.7) | 6.5 (4.9, 8.8) | 0.850 | 6.7 (4.8, 9.3) |
| Lymphocytes, 103/mm3 | 1.0 (0.7, 1.4) | 1.2 (0.8, 2.1) | 0.9 (0.6, 1.4) | 0.018 | 1.0 (0.7, 1.5) |
| Alanine amino-transferase (ALT), U/L | 29.0 (19.0, 49.0) | 25.0 (15.5, 44.0) | 23.0 (17.0, 41.0) | 0.016 | 28.0 (18.0, 46.0) |
| Creatine Kinase, U/L | 83.0 (51.0, 180.0) | 93.0 (44.0, 157.0) | 81.0 (44.0, 175.0) | 0.866 | 84.5 (49.5, 179.5) |
| Creatinine, mg/dL | 0.8 (0.7, 1.1) | 0.9 (0.7, 1.4) | 1.0 (0.8, 1.4) | <0.001 | 0.9 (0.7, 1.2) |
| D-dimer, mg/L | 322.0 (217.0, 616.0) | 361.5 (149.0, 535.0) | 324.5 (204.0, 633.0) | 0.709 | 322.0 (213.0, 626.0) |
| Lactate dehydrogenase, U/L | 288.0 (227.0, 384.0) | 286.0 (209.0, 393.0) | 250.0 (200.0, 321.0) | 0.002 | 280.0 (219.0, 372.0) |
| C-reactive protein, mg/dL | 49.8 (20.6, 82.1) | 36.0 (17.1, 59.6) | 55.1 (24.1, 95.6) | 0.049 | 49.7 (21.7, 82.0) |
| Platelets, 103/mm3 | 196.0 (154.0, 250.0) | 176.0 (119.0, 262.0) | 189.0 (140.0, 254.0) | 0.279 | 193.0 (150.0, 252.0) |
| Procalcitonin, | 0.2 (0.1, 0.9) | 0.2 (0.1, 9.0) | 0.2 (0.2, 0.3) | 0.538 | 0.2 (0.1, 1.0) |
| Anti COVID-19 Vaccination | |||||
|---|---|---|---|---|---|
| Therapies | None | 1 Dose | 2+ Doses | p-Value * | Total |
| N = 743 | N = 62 | N = 151 | N = 956 | ||
| Monoclonal antibodies, n(%) | 30 (4.0%) | 4 (6.5%) | 38 (25.2%) | <0.001 | 72 (7.5%) |
| Heparin, n(%) | 579 (77.9%) | 45 (72.6%) | 110 (72.8%) | 0.291 | 734 (76.8%) |
| Remdesivir, n(%) | 186 (25.1%) | 18 (29.0%) | 5 (3.3%) | <0.001 | 209 (21.9%) |
| Glucocorticoids, n(%) | 586 (78.9%) | 44 (71.0%) | 112 (74.2%) | 0.194 | 742 (77.6%) |
| Immunomodulants, n(%) | 50 (6.7%) | 4 (6.5%) | 2 (1.3%) | 0.035 | 56 (5.9%) |
| Anti COVID-19 Vaccination | |||||
|---|---|---|---|---|---|
| Outcomes | None | 1 Dose | 2+ Doses | p-Value * | Total |
| N = 743 | N = 62 | N = 151 | N = 956 | ||
| No Oxygen, n(%) | 101 (13.6%) | 13 (21.0%) | 20 (13.2%) | 0.263 | 134 (14.0%) |
| Low flow Oxygen, n(%) | 234 (31.5%) | 16 (25.8%) | 46 (30.5%) | 0.642 | 296 (31.0%) |
| High flow Oxygen, n(%) | 50 (6.7%) | 8 (12.9%) | 29 (19.2%) | <0.001 | 87 (9.1%) |
| CPAP, n(%) | 251 (33.8%) | 22 (35.5%) | 39 (25.8%) | 0.146 | 312 (32.6%) |
| NIV, n(%) | 78 (10.5%) | 2 (3.2%) | 15 (9.9%) | 0.185 | 95 (9.9%) |
| Invasive mechanical ventilation (IMV), n(%) | 29 (3.9%) | 1 (1.6%) | 2 (1.3%) | 0.203 | 32 (3.3%) |
| Mechanical ventilation $ or death, n(%) | 392 (52.8%) | 32 (51.6%) | 66 (43.7%) | 0.146 | 490 (51.3%) |
| In-hospital death, n(%) | 153 (20.6%) | 18 (29.0%) | 32 (21.2%) | 0.185 | 203 (21.2%) |
| Follow-up time, days Median (IQR) | 12 (7, 20) | 14 (7, 24) | 14 (9, 21) | 0.213 | 12 (7, 20) |
| Follow-up time in those who died, days Median (IQR) | 10 (6, 16) | 10 (7, 21) | 10 (6, 15) | 0.885 | 10 (6, 16) |
| (a) Unadjusted and adjusted relative hazards of in hospital death | ||||
| Unadjusted HR (95% CI) | p-Value | Adjusted * HR (95% CI) | p-Value | |
| Unvaccinated | 1 | 1 | ||
| One dose | 1.25 (0.76, 2.03) | 0.377 | 1.04 (0.63, 1.71) | 0.869 |
| 2+ doses | 0.96 (0.65, 1.40) | 0.825 | 0.50 (0.30, 0.84) | 0.009 |
| (b) Unadjusted and adjusted relative hazards of composite endpoint | ||||
| Unadjusted HR (95% CI) | p-Value | Adjusted * HR (95% CI) | p-Value | |
| Unvaccinated | 1 | |||
| One dose | 0.94 (0.66, 1.35) | 0.756 | 0.83 (0.57, 1.19) | 0.303 |
| 2+ doses | 0.79 (0.60, 1.02) | 0.069 | 0.49 (0.35, 0.69) | <0.001 |
| (c) Unadjusted and adjusted relative hazards of composite endpoint | ||||
| Unadjusted HR (95% CI) | p-Value | Adjusted * HR (95% CI) | p-Value | |
| Unvaccinated | 1 | 1 | ||
| One dose | 0.94 (0.66, 1.35) | 0.756 | 0.90 (0.62, 1.29) | 0.565 |
| 2+ doses since less than 180 days | 0.82 (0.57, 1.18) | 0.274 | 0.61 (0.40, 0.92) | 0.017 |
| 2+ doses for more than 180 days | 0.76 (0.54, 1.07) | 0.120 | 0.54 (0.36, 0.82) | 0.004 |
| (d) Unadjusted and adjusted relative hazards of in hospital death -after removing those who received 3 doses | ||||
| Unadjusted HR (95% CI) | p-Value | Adjusted * HR (95% CI) | p-Value | |
| Unvaccinated | 1 | 1 | ||
| One dose | 1.24 (0.76, 2.02) | 0.389 | 1.03 (0.63, 1.70) | 0.896 |
| 2 doses | 1.08 (0.73, 1.59) | 0.693 | 0.55 (0.33, 0.92) | 0.024 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
d’Arminio Monforte, A.; Tavelli, A.; De Benedittis, S.; Bai, F.; Tincati, C.; Gazzola, L.; Viganò, O.; Allegrini, M.; Mondatore, D.; Tesoro, D.; et al. Real World Estimate of Vaccination Protection in Individuals Hospitalized for COVID-19. Vaccines 2022, 10, 550. https://doi.org/10.3390/vaccines10040550
d’Arminio Monforte A, Tavelli A, De Benedittis S, Bai F, Tincati C, Gazzola L, Viganò O, Allegrini M, Mondatore D, Tesoro D, et al. Real World Estimate of Vaccination Protection in Individuals Hospitalized for COVID-19. Vaccines. 2022; 10(4):550. https://doi.org/10.3390/vaccines10040550
Chicago/Turabian Styled’Arminio Monforte, Antonella, Alessandro Tavelli, Sara De Benedittis, Francesca Bai, Camilla Tincati, Lidia Gazzola, Ottavia Viganò, Marina Allegrini, Debora Mondatore, Daniele Tesoro, and et al. 2022. "Real World Estimate of Vaccination Protection in Individuals Hospitalized for COVID-19" Vaccines 10, no. 4: 550. https://doi.org/10.3390/vaccines10040550
APA Styled’Arminio Monforte, A., Tavelli, A., De Benedittis, S., Bai, F., Tincati, C., Gazzola, L., Viganò, O., Allegrini, M., Mondatore, D., Tesoro, D., Barbanotti, D., Mulé, G., Castoldi, R., De Bona, A., Bini, T., Chiumello, D., Centanni, S., Passarella, S., Orfeo, N., ... for the SPID Group. (2022). Real World Estimate of Vaccination Protection in Individuals Hospitalized for COVID-19. Vaccines, 10(4), 550. https://doi.org/10.3390/vaccines10040550







