Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland
Abstract
1. Introduction
2. Methods
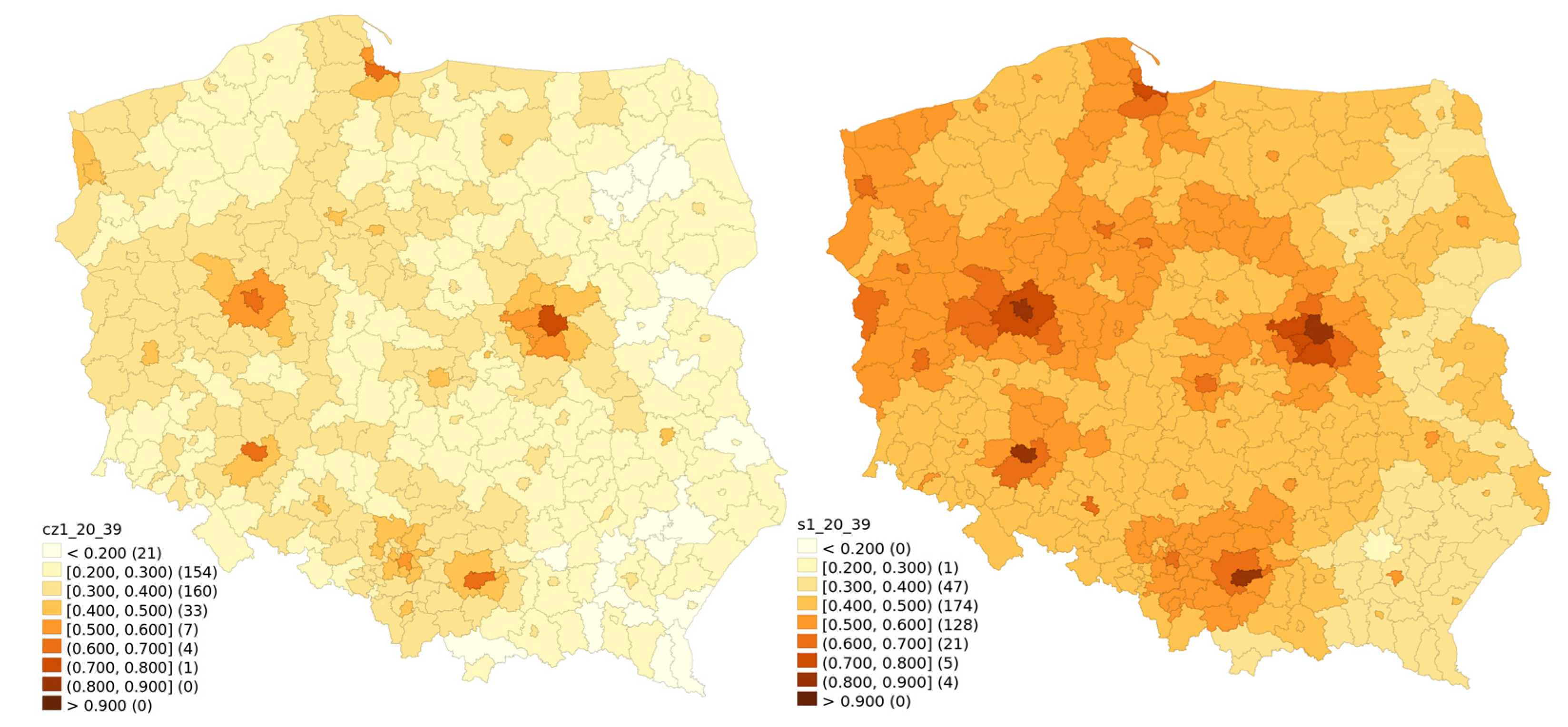
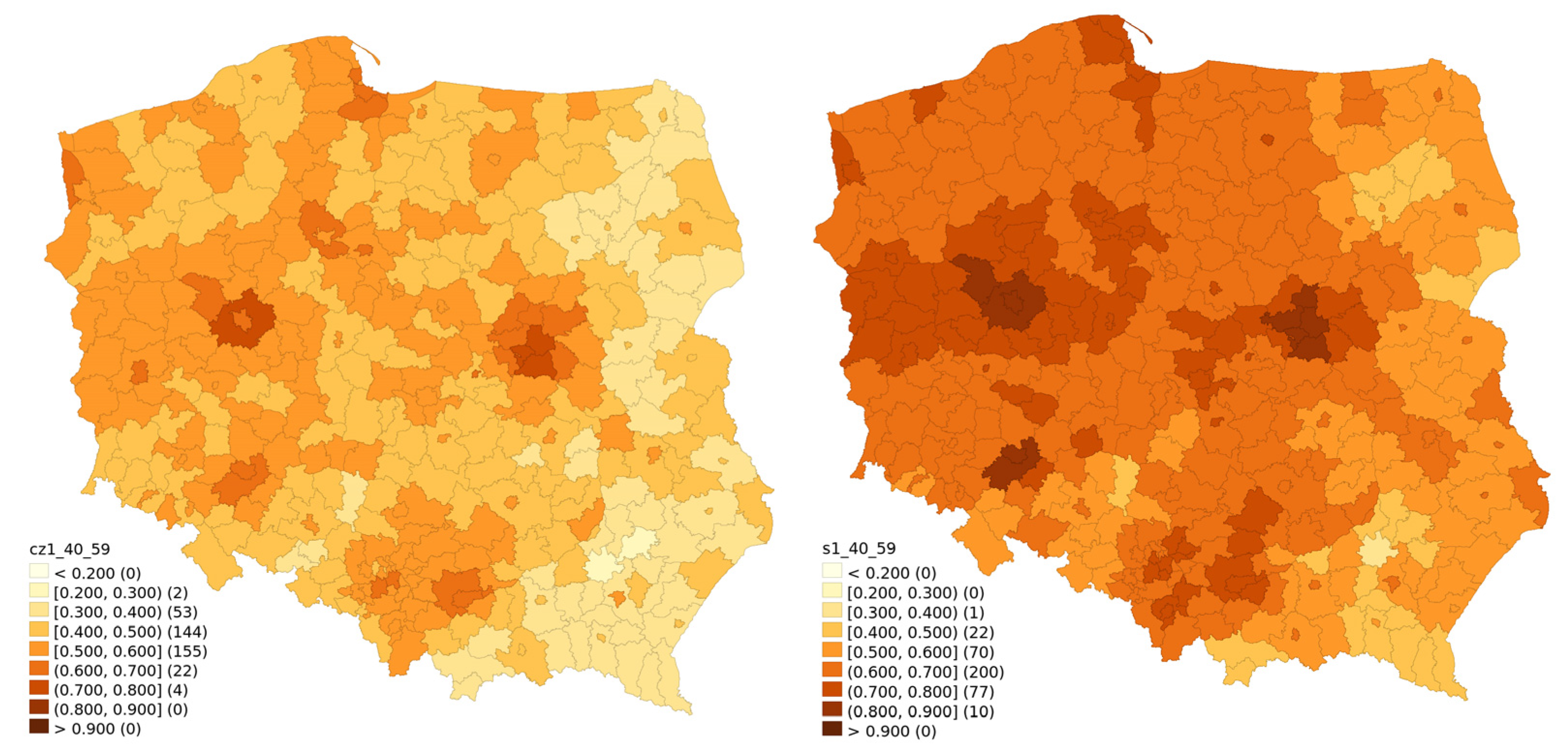
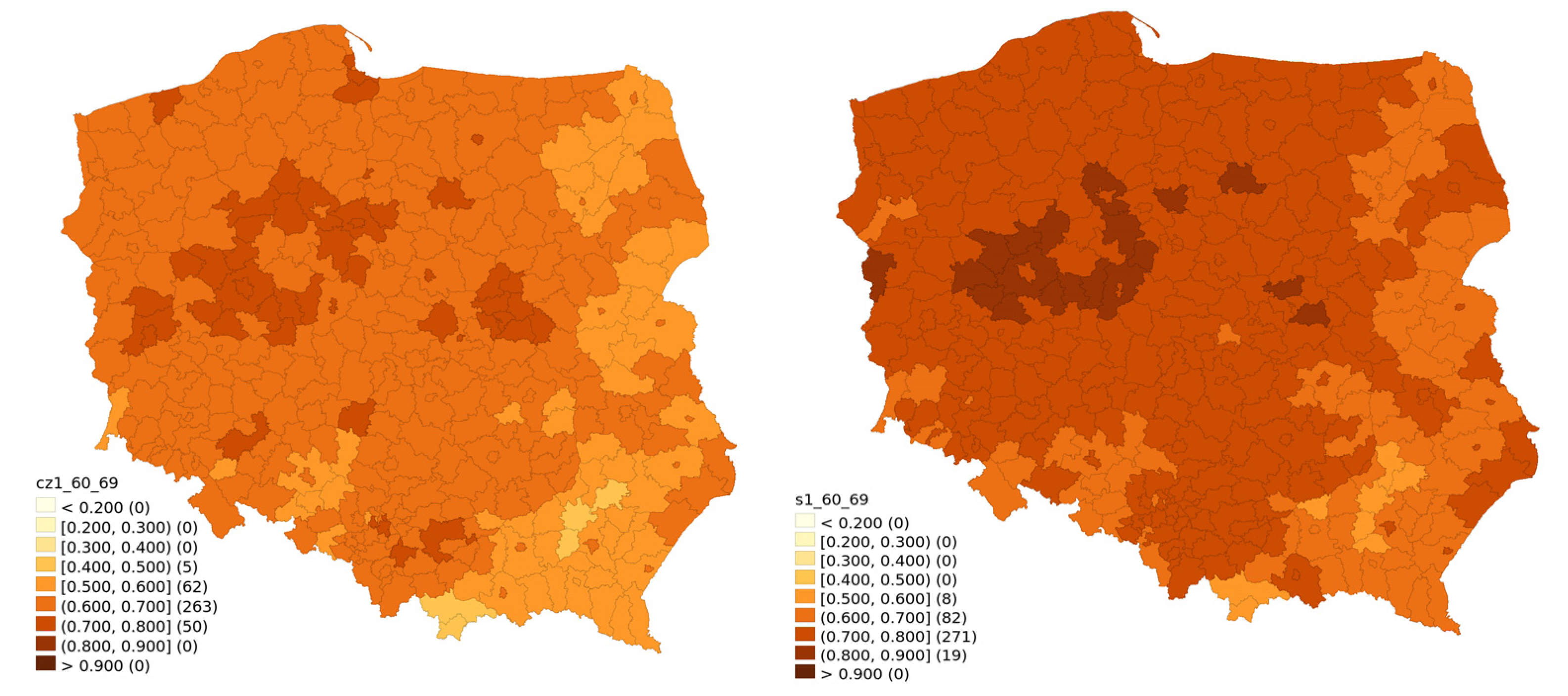
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Raport Szczepień Przeciwko COVID-19—Portal Gov.pl. Available online: https://www.gov.pl/web/szczepimysie/raport-szczepien-przeciwko-covid-19 (accessed on 27 February 2022).
- Walkowiak, M.P.; Walkowiak, J.B.; Walkowiak, D. COVID-19 Passport as a Factor Determining the Success of National Vaccination Campaigns: Does It Work? The Case of Lithuania vs. Poland. Vaccines 2021, 9, 1498. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, J.; Witkowska, N.; Bidzan, L. Letter to the Editor: Excess All-Cause Mortality during Second Wave of COVID-19—The Polish Perspective. Eurosurveillance 2021, 26, 2100117. [Google Scholar] [CrossRef] [PubMed]
- Centrum Badania Opinii Społecznej [Centre for Public Opinion Research]. Polacy o Szczepieniach Przeciw COVID-19 [The Poles on the COVID-19 Vacciantion]. 2021. Available online: https://www.cbos.pl/SPISKOM.POL/2021/K_075_21.PDF (accessed on 27 February 2022).
- Walkowiak, M.P.; Walkowiak, D. Predictors of COVID-19 Vaccination Campaign Success: Lessons Learnt from the Pandemic So Far. A Case Study from Poland. Vaccines 2021, 9, 1153. [Google Scholar] [CrossRef] [PubMed]
- Sowa, P.; Kiszkiel, Ł.; Laskowski, P.P.; Alimowski, M.; Szczerbiński, Ł.; Paniczko, M.; Moniuszko-Malinowska, A.; Kamiński, K. COVID-19 Vaccine Hesitancy in Poland—Multifactorial Impact Trajectories. Vaccines 2021, 9, 876. [Google Scholar] [CrossRef] [PubMed]
- Jarynowski, A.; Wójta-Kempa, M.; Płatek, D.; Czopek, K. Attempt to Understand Public-Health Relevant Social Dimensions of Covid-19 Outbreak in Poland. SSRN 2020, 4, 7–44. [Google Scholar] [CrossRef]
- Harada, T.; Watanabe, T. Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors. Vaccines 2021, 10, 25. [Google Scholar] [CrossRef]
- Le Maréchal, M.; Batel, A.; Bouvier, S.; Mahdhaoui, H.; Margotton, M.; Vittoz, J.-P.; Brudieu, E.; Chevallier, C.; Bedouch, P.; Touati, S.; et al. “When Did You Decide to Receive the Covid-19 Vaccine?” Survey in a High-Volume Vaccination Center. Hum. Vaccines Immunother. 2022, 17, 5099–5104. [Google Scholar] [CrossRef]
- Chaudhuri, K.; Chakrabarti, A.; Chandan, J.S.; Bandyopadhyay, S. COVID-19 Vaccine Hesitancy in the UK: A Longitudinal Household Cross-Sectional Study. BMC Public Health 2022, 22, 104. [Google Scholar] [CrossRef]
- Goodwin, R.; Ben-Ezra, M.; Takahashi, M.; Luu, L.-A.N.; Borsfay, K.; Kovács, M.; Hou, W.K.; Hamama-Raz, Y.; Levin, Y. Psychological Factors Underpinning Vaccine Willingness in Israel, Japan and Hungary. Sci. Rep. 2022, 12, 439. [Google Scholar] [CrossRef]
- Rane, M.S.; Kochhar, S.; Poehlein, E.; You, W.; Robertson, M.K.M.; Zimba, R.; Westmoreland, D.A.; Romo, M.L.; Kulkarni, S.G.; Chang, M.; et al. Determinants and Trends of COVID-19 Vaccine Hesitancy and Vaccine Uptake in a National Cohort of U.S. Adults: A Longitudinal Study. Am. J. Epidemiol. 2022, kwab293. [Google Scholar] [CrossRef]
- Purvis, R.S.; Hallgren, E.; Moore, R.A.; Willis, D.E.; Hall, S.; Gurel-Headley, M.; McElfish, P.A. Trusted Sources of COVID-19 Vaccine Information among Hesitant Adopters in the United States. Vaccines 2021, 9, 1418. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E.B.; Daoust, J.-F.; Vikse, J.; Nelson, V. “Until I Know It’s Safe for Me”: The Role of Timing in COVID-19 Vaccine Decision-Making and Vaccine Hesitancy. Vaccines 2021, 9, 1417. [Google Scholar] [CrossRef] [PubMed]
- Bajos, N.; Spire, A.; Silberzan, L.; EPICOV study group. The Social Specificities of Hostility toward Vaccination against Covid-19 in France. PLoS ONE 2022, 17, e0262192. [Google Scholar] [CrossRef] [PubMed]
- Yousuf, H.; van der Linden, S.; van Essen, T.; Gommers, D.; Scherder, E.; Narula, J.; Hofstra, L. Dutch Perspectives toward Governmental Trust, Vaccination, Myths, and Knowledge about Vaccines and COVID-19. JAMA Netw. Open 2021, 4, e2140529. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 Vaccine among Adults in the United States: How Many People Would Get Vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and Vaccine Hesitancy: A Longitudinal Study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors Associated with US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef]
- Basiw. Available online: https://basiw.mz.gov.pl/index.html#/visualisation?id=3653 (accessed on 27 February 2022).
- GUS—Bank Danych Lokalnych. Available online: https://bdl.stat.gov.pl/BDL/dane/podgrup/temat (accessed on 27 February 2022).
- Zhang, E.J.; Chughtai, A.A.; Heywood, A.; MacIntyre, C.R. Influence of Political and Medical Leaders on Parental Perception of Vaccination: A Cross-Sectional Survey in Australia. BMJ Open 2019, 9, e025866. [Google Scholar] [CrossRef]
- Albrecht, D. Vaccination, Politics and COVID-19 Impacts. BMC Public Health 2022, 22, 96. [Google Scholar] [CrossRef]
- Huynh, H.P.; Zsila, Á.; Martinez-Berman, L. Psychosocial Predictors of Intention to Vaccinate Against the Coronavirus (COVID-19). Behav. Med. 2021, 1–15. [Google Scholar] [CrossRef]
- Walkowiak, M.P.; Walkowiak, D. Underestimation in Reporting Excess COVID-19 Death Data in Poland during the First Three Pandemic Waves. Int. J. Environ. Res. Public Health 2022, 19, 3692. [Google Scholar] [CrossRef] [PubMed]
- Contoli, B.; Possenti, V.; Minardi, V.; Binkin, N.J.; Ramigni, M.; Carrozzi, G.; Masocco, M. What Is the Willingness to Receive Vaccination against COVID-19 among the Elderly in Italy? Data from the PASSI d’Argento Surveillance System. Front. Public Health 2021, 9, 736976. [Google Scholar] [CrossRef] [PubMed]
- Salali, G.D.; Uysal, M.S. Effective Incentives for Increasing COVID-19 Vaccine Uptake. Psychol. Med. 2021, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Lai, A.H.Y.; Wang, J.; Asim, S.; Chan, P.S.-F.; Wang, Z.; Yeoh, E.K. Multilevel Determinants of COVID-19 Vaccine Uptake Among South Asian Ethnic Minorities in Hong Kong: Cross-Sectional Web-Based Survey. JMIR Public Health Surveill. 2021, 7, e31707. [Google Scholar] [CrossRef] [PubMed]
- Furman, F.M.; Zgliczyński, W.S.; Jankowski, M.; Baran, T.; Szumowski, Ł.; Pinkas, J. The State of Vaccine Confidence in Poland: A 2019 Nationwide Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 4565. [Google Scholar] [CrossRef]
- Kubicek, P. Martin Åberg and Mikael Sandberg, Social Capital and Democratisation: Roots of Trust in Post-Communist Poland and Ukraine (Aldershot: Ashgate, 2003), Xvi, 332 Pp. + Maps, Figures. Natl. Pap. 2003, 31, 517–518. [Google Scholar] [CrossRef]
- Civil Society and Social Capital in Post-Communist Eastern Europe. Available online: https://www.routledge.com/Civil-Society-and-Social-Capital-in-Post-Communist-Eastern-Europe/Cox/p/book/9781138953666 (accessed on 22 February 2022).
- GUS Jakość Życia i Kapitał Społeczny w Polsce. Wyniki Badania Spójności Społecznej. 2018. Available online: https://stat.gov.pl/obszary-tematyczne/warunki-zycia/dochody-wydatki-i-warunki-zycia-ludnosci/jakosc-zycia-i-kapital-spoleczny-w-polsce-wyniki-badania-spojnosci-spolecznej-2018,4,3.html (accessed on 27 February 2022).
- Domaradzki, J.; Walkowiak, D. Medical Students’ Voluntary Service During the COVID-19 Pandemic in Poland. Front. Public Health 2021, 9, 618608. [Google Scholar] [CrossRef]
- Domaradzki, J.; Walkowiak, D. Does Religion Influence the Motivations of Future Healthcare Professionals to Volunteer during the COVID-19 Pandemic in Poland? An Exploratory Study. J. Relig. Health 2021, 60, 1507–1520. [Google Scholar] [CrossRef]
- Lewenstein, B. Społeczeństwo rodzin czy obywateli—kapitał społeczny Polaków okresu transformacji. In Societas/Communitas; Instytut Stosowanych Nauk Społecznych Uniwersytetu Warszawskiego: Warsaw, Poland, 2006; Volume 1, pp. 163–196. [Google Scholar]
- Centrum Badania Opinii Społecznej [Centre for Public Opinion Research]. O Nieufności i Zaufaniu [On Mistrust and Trust]. 2018. Available online: https://www.cbos.pl/SPISKOM.POL/2018/K_035_18.PDF (accessed on 27 February 2022).
- Centrum Badania Opinii Społecznej [Centre for Public Opinion Research]. Zaufanie Społeczne [Social Trust]. 2020. Available online: https://www.cbos.pl/SPISKOM.POL/2020/K_043_20.PDF (accessed on 27 February 2022).
- Podemski, K. Społeczeństwo obywatelskie w Polsce 25 lat po wielkiej zmianie. Ruch Praw. Ekon. I Socjol. 2014, 76, 89–108. [Google Scholar] [CrossRef]
- Zybała, A. Społeczeństwo obywatelskie i polityka publiczna. Społeczeństwo Ob. 2015, 2, 35–53. [Google Scholar]
- Jasnosz, K. Kształtowanie się społeczeństwa obywatelskiego w Polsce po 1989 roku i jego obecna kondycja. Rocz. Adm. Publicznej 2020, 2020, 177–202. [Google Scholar] [CrossRef]
- Hawe, P.; Shiell, A. Social Capital and Health Promotion: A Review. Soc. Sci. Med. 2000, 51, 871–885. [Google Scholar] [CrossRef]
- Eriksson, M. Social Capital and Health—Implications for Health Promotion. Glob. Health Action 2011, 4, 5611. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C. Social Capital, Social Movements and Global Public Health: Fighting for Health-Enabling Contexts in Marginalised Settings. Soc. Sci. Med. 2020, 257, 112153. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.L.; Ronan, K. Combinations of Social Participation and Trust and Association with Health Status—An Australian Perspective. Health Promot. Int. 2014, 29, 608–620. [Google Scholar] [CrossRef][Green Version]
- Nieminen, T.; Martelin, T.; Koskinen, S.; Aro, H.; Alanen, E.; Hyyppä, M.T. Social Capital as a Determinant of Self-Rated Health and Psychological Well-Being. Int. J. Public Health 2010, 55, 531–542. [Google Scholar] [CrossRef]
- Nieminen, T.; Prättälä, R.; Martelin, T.; Härkänen, T.; Hyyppä, M.T.; Alanen, E.; Koskinen, S. Social Capital, Health Behaviours and Health: A Population-Based Associational Study. BMC Public Health 2013, 13, 613. [Google Scholar] [CrossRef]
- Poortinga, W. Do Health Behaviors Mediate the Association between Social Capital and Health? Prev. Med. 2006, 43, 488–493. [Google Scholar] [CrossRef]
- Rönnerstrand, B. Social Capital and Immunization against the 2009 A(H1N1) Pandemic in the American States. Public Health 2014, 128, 709–715. [Google Scholar] [CrossRef]
- Rönnerstrand, B. Social Capital and Immunisation against the 2009 A(H1N1) Pandemic in Sweden. Scand. J. Public Health 2013, 41, 853–859. [Google Scholar] [CrossRef]
- Chuang, Y.-C.; Huang, Y.-L.; Tseng, K.-C.; Yen, C.-H.; Yang, L. Social Capital and Health-Protective Behavior Intentions in an Influenza Pandemic. PLoS ONE 2015, 10, e0122970. [Google Scholar] [CrossRef]
- Blair, R.A.; Morse, B.S.; Tsai, L.L. Public Health and Public Trust: Survey Evidence from the Ebola Virus Disease Epidemic in Liberia. Soc. Sci. Med. 2017, 172, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Bartscher, A.K.; Seitz, S.; Siegloch, S.; Slotwinski, M.; Wehrhöfer, N. Social Capital and the Spread of Covid-19: Insights from European Countries. J. Health Econ. 2021, 80, 102531. [Google Scholar] [CrossRef] [PubMed]
- Bylok, F. Impact of Social Capital on Health Safety during the SARS-CoV-2 Flu Pandemic. Syst. Saf. Hum. Tech. Facil. Environ. 2021, 3, 304–311. [Google Scholar] [CrossRef]
- Imbulana Arachchi, J.; Managi, S. The Role of Social Capital in COVID-19 Deaths. BMC Public Health 2021, 21, 434. [Google Scholar] [CrossRef]
- Makridis, C.A.; Wu, C. How Social Capital Helps Communities Weather the COVID-19 Pandemic. PLoS ONE 2021, 16, e0245135. [Google Scholar] [CrossRef]
- Borgonovi, F.; Andrieu, E. Bowling Together by Bowling Alone: Social Capital and COVID-19. Soc. Sci. Med. 2020, 265, 113501. [Google Scholar] [CrossRef]
- Ferwana, I.; Varshney, L.R. Social Capital Dimensions Are Differentially Associated with COVID-19 Vaccinations, Masks, and Physical Distancing. PLoS ONE 2021, 16, e0260818. [Google Scholar] [CrossRef]
- James, E.K.; Bokemper, S.E.; Gerber, A.S.; Omer, S.B.; Huber, G.A. Persuasive Messaging to Increase COVID-19 Vaccine Uptake Intentions. Vaccine 2021, 39, 7158–7165. [Google Scholar] [CrossRef]

| Variable | Model without Lag | Model with Time Lag | Model with Spatial Lag |
|---|---|---|---|
| Const | 0.218 (0.0393) *** | 0.241 (0.0290) *** | 0.163 (0.0301) *** |
| Time lag | 0.430 (0.0373) *** | ||
| Spatial lag | 0.547 (0.0494) *** | ||
| Vote for Law and Justice | −0.155 (0.0217) *** | −0.0510 (0.0210) * | −0.0762 (0.0201) *** |
| Vote for Confederation | −1.534 (0.207) *** | −0.964 (0.188) *** | −0.810 (0.185) *** |
| Vote for Kukiz | −0.491 (0.0772) *** | −0.541 (0.066) *** | −0.378 (0.0688) *** |
| Voter turnout | 0.129 (0.0606) * | ||
| COVID−19 only deaths until 2021-06-30 | 0.0146 (0.00504) ** | 0.0119 (0.00457) ** | |
| Higher education | 0.164 (0.0591) ** | −0.152 (0.0542) *** | 0.290 (0.0443) *** |
| Employment rate | 0.473 (0.0637) *** | 0.177 (0.0532) *** | 0.193 (0.0370) *** |
| Adjusted R2 | 56.5% | 67.4% | 66.1% |
| Variable | Model without Lag | Model with Time Lag | Model with Spatial Lag |
|---|---|---|---|
| Const | 0.0734 (0.0490) | 0.0156 (0.0307) | −0.0687 (0.0283) * |
| Time lag | 0.661 (0.0367) *** | ||
| Spatial lag | 0.699 (0.0376) *** | ||
| Vote for Law and Justice | −0.198 (0.0271) *** | −0.0568 (0.0163) *** | |
| Vote for Confederation | −2.096 (0.258) *** | −1.038 (0.212) *** | −0.896 (0.193) *** |
| Vote for Kukiz | −0.295 (0.0964) ** | −0.429 (0.0729) *** | |
| Voter turnout | 0.448 (0.0756) *** | 0.207 (0.0408) *** | |
| COVID-19 only deaths until 2021-06-30 | 0.0228 (0.00629) *** | 0.00962 (0.00485) * | |
| Higher education | −0.222 (0.0738) ** | −0.294 (0.0532) *** | |
| Employment rate | 0.568 (0.0795) *** | 0.334 (0.0619) *** | |
| Adjusted R2 | 57.4% | 71.8% | 75.9% |
| Variable | Model without Lag | Model with Time Lag | Model with Spatial Lag |
|---|---|---|---|
| Const | 0.376 (0.0415) *** | −0.00192 (0.0429) | 0.112 (0.0241) *** |
| Time lag | 0.682 (0.0459) *** | ||
| Spatial lag | 0.568 (0.0505) *** | ||
| Vote for Law and Justice | −0.0728 (0.0267) ** | ||
| Vote for Confederation | −0.750 (0.258) ** | 0.693 (0.203) *** | −0.466 (0.180) *** |
| Vote for Kukiz | −0.299 (0.0948) ** | −0.391 (0.0739) *** | |
| Voter turnout | 0.107 (0.0539) * | ||
| COVID-19 only deaths until 2021-06-30 | |||
| Higher education | −0.772 (0.0625) *** | −0.844 (0.0523) *** | −0.687 (0.0459) *** |
| Employment rate | 0.219 (0.0654) *** | 0.216 (0.0412) *** | |
| Adjusted R2 | 39.2% | 60.5% | 55.0% |
| Variable | Model without Lag | Model with Time Lag | Model With Spatial Lag |
|---|---|---|---|
| Const | 0.796 (0.0949) *** | −1.072 (0.0803) *** | 0.299 (0.0909) *** |
| Time lag | 2.301 (0.0772) *** | ||
| Spatial lag | 0.541 (0.0489) *** | ||
| Vote for Law and Justice | −0.997 (0.0634) *** | −0.239 (0.0449) *** | −0.537 (0.0686) *** |
| Vote for Confederation | −3.483 (0.611) *** | −1.4776 (0.544) ** | |
| Vote for Kukiz | |||
| Voter turnout | 0.958 (0.153) *** | 0.270 (0.0913) *** | 0.475 (0.139) *** |
| COVID-19 only deaths until 2021-06-30 | 0.0581 (0.0159) *** | 0.0327 (0.0141) * | |
| Higher education | −0.499 (0.179) ** | −0.755 (0.0990) *** | 0.407 (0.163) ** |
| Employment rate | |||
| Adjusted R2 | 64.1% | 87.9% | 72.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walkowiak, M.P.; Domaradzki, J.; Walkowiak, D. Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines 2022, 10, 528. https://doi.org/10.3390/vaccines10040528
Walkowiak MP, Domaradzki J, Walkowiak D. Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines. 2022; 10(4):528. https://doi.org/10.3390/vaccines10040528
Chicago/Turabian StyleWalkowiak, Marcin Piotr, Jan Domaradzki, and Dariusz Walkowiak. 2022. "Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland" Vaccines 10, no. 4: 528. https://doi.org/10.3390/vaccines10040528
APA StyleWalkowiak, M. P., Domaradzki, J., & Walkowiak, D. (2022). Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines, 10(4), 528. https://doi.org/10.3390/vaccines10040528







