COVID-19 Vaccine Booster Hesitancy among Healthcare Workers: A Retrospective Observational Study in Singapore
Abstract
:1. Introduction
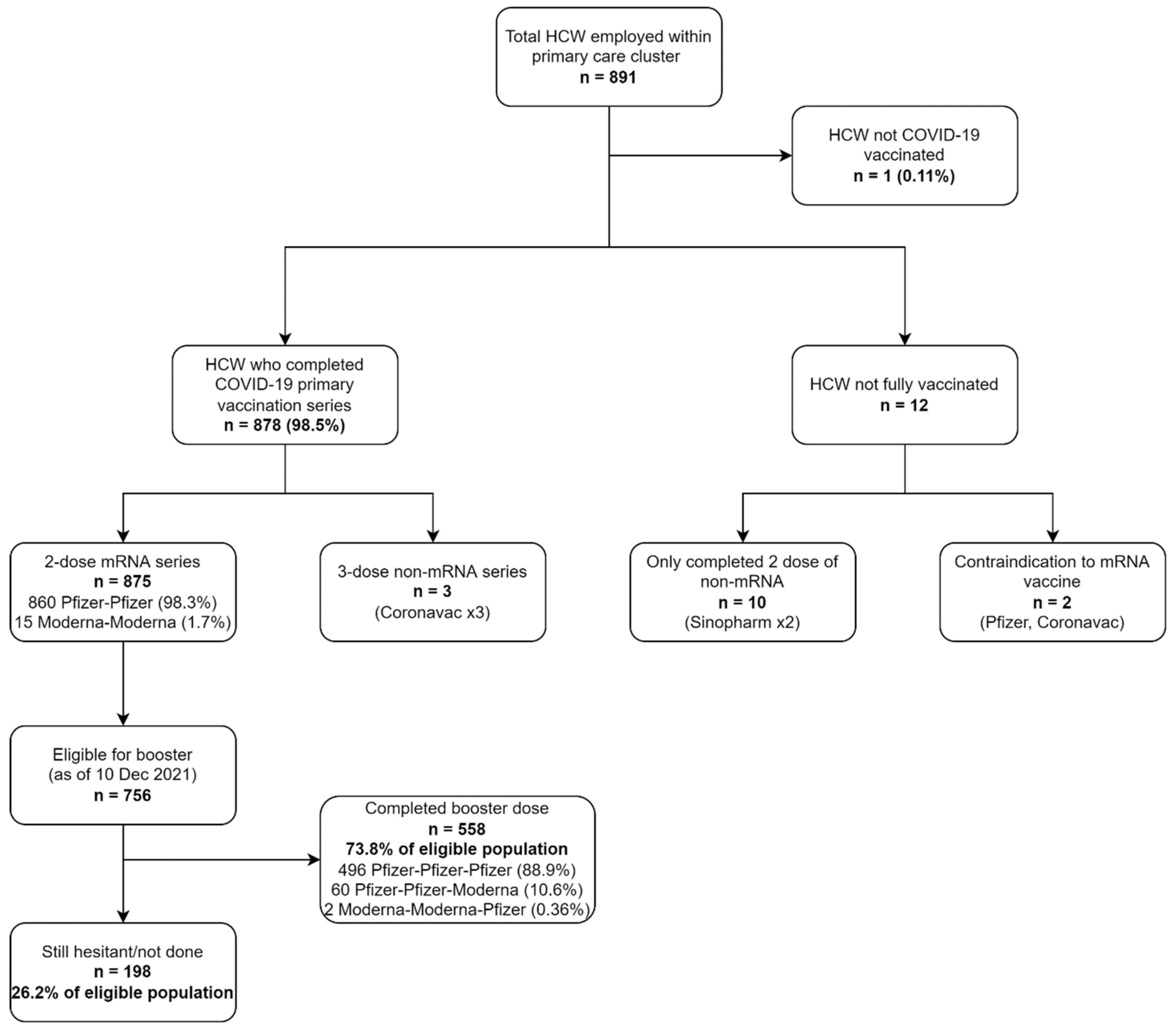
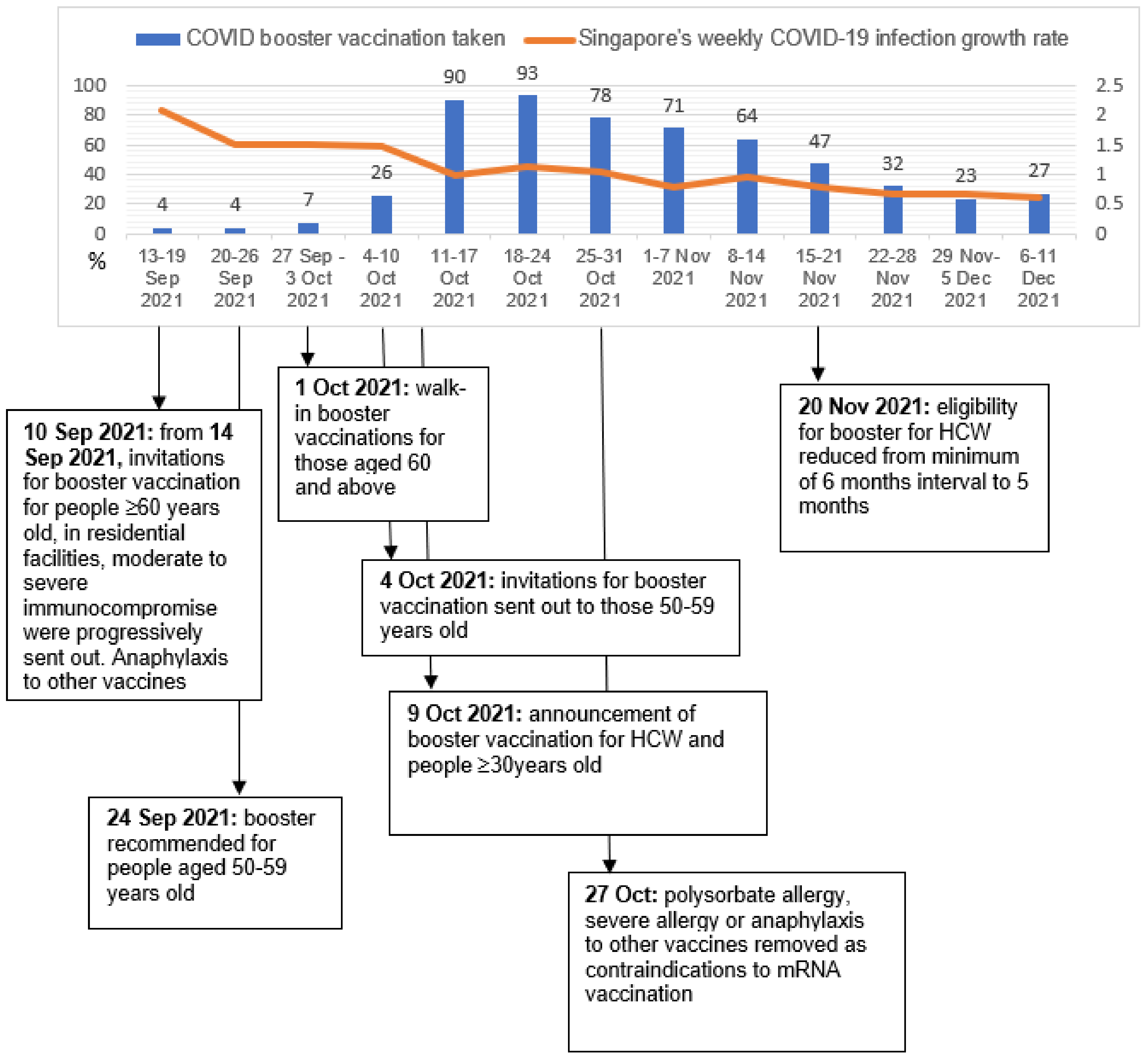
2. Methods
2.1. Study Population and Sampling
2.2. Study Setting
2.3. Study Definitions and Parameters
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
4. Discussion
4.1. Study Strengths
4.2. Study Limitations
4.2.1. Selection Bias
4.2.2. Lack of Age, Other Demographic Factors, and COVID-19 Infection Status in the Database
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID Live—Coronavirus Statistics—Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 13 March 2022).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Moghadas, S.M.; Vilches, T.N.; Zhang, K.; Wells, C.R.; Shoukat, A.; Singer, B.H.; Meyers, L.A.; Neuzil, K.M.; Langley, J.M.; Fitzpatrick, M.C.; et al. The Impact of Vaccination on Coronavirus Disease 2019 (COVID-19) Outbreaks in the United States. Clin. Infect. Dis. 2021, 73, 2257–2264. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.A.; Wu, J.W. Vaccine Confidence in the Time of COVID-19. Eur. J. Epidemiol. 2020, 35, 325–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. The World Health Report. 2006: Working Together for Health; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Infection Prevention and Control for COVID-19 in Healthcare Settings—Second Update, 31 March 2020; Stockholm: ECDC. 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/Infection-prevention-control-for-thecare-of-patients-with-2019-nCoV-healthcare-settings_update-31-March-2020.pdf (accessed on 8 March 2022).
- Katzman, J.G.; Katzman, J.W. Primary Care Clinicians as COVID-19 Vaccine Ambassadors. J. Prim. Care Commun. Health 2021, 12, 21501327211007024. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to Get Vaccinations against COVID-19 in French Healthcare Workers during the First Pandemic Wave: A Cross-Sectional Survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Editor’s Choice: Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef]
- MOH|Vaccination Statistics. Available online: https://www.moh.gov.sg/covid-19/vaccination/statistics (accessed on 1 February 2022).
- Koh, S.W.C.; Liow, Y.; Loh, V.W.K.; Liew, S.J.; Chan, Y.-H.; Young, D. COVID-19 Vaccine Acceptance and Hesitancy among Singaporean Primary Healthcare Workers. Res. Sq. 2021. preprint. [Google Scholar] [CrossRef]
- Tan, L.F.; Huak, C.Y.; Siow, I.; Tan, A.J.; Venugopalan, P.M.; Premkumar, A.; Seetharaman, S.K.; Tan, B.Y.Q. The Road to Achieving Herd Immunity: Factors Associated with Singapore Residents’ Uptake and Hesitancy of the COVID-19 Vaccination. Expert Rev. Vaccines 2022, 1–7. [Google Scholar] [CrossRef]
- Cameroni, E.; Bowen, J.E.; Rosen, L.E.; Saliba, C.; Zepeda, S.K.; Culap, K.; Pinto, D.; VanBlargan, L.A.; De Marco, A.; di Iulio, J.; et al. Broadly Neutralizing Antibodies Overcome SARS-CoV-2 Omicron Antigenic Shift. Nature 2022, 602, 664–670. [Google Scholar] [CrossRef]
- Lu, L.; Mok, B.W.-Y.; Chen, L.-L.; Chan, J.M.-C.; Tsang, O.T.-Y.; Lam, B.H.-S.; Chuang, V.W.-M.; Chu, A.W.-H.; Chan, W.-M.; Ip, J.D.; et al. Neutralization of SARS-CoV-2 Omicron Variant by Sera from BNT162b2 or Coronavac Vaccine Recipients. Clin. Infect Dis. 2021, ciab1041. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; SAGE Working Group on Vaccine Hesitancy. Measuring Vaccine Hesitancy: The Development of a Survey Tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [Green Version]
- Domek, G.J.; O’Leary, S.T.; Bull, S.; Bronsert, M.; Contreras-Roldan, I.L.; Bolaños Ventura, G.A.; Kempe, A.; Asturias, E.J. Measuring Vaccine Hesitancy: Field Testing the WHO SAGE Working Group on Vaccine Hesitancy Survey Tool in Guatemala. Vaccine 2018, 36, 5273–5281. [Google Scholar] [CrossRef]
- Callaway, E. Mix-and-Match COVID Vaccines Trigger Potent Immune Response. Nature 2021, 593, 491. [Google Scholar] [CrossRef]
- Berry, S.D.; Johnson, K.S.; Myles, L.; Herndon, L.; Montoya, A.; Fashaw, S.; Gifford, D. Lessons Learned from Frontline Skilled Nursing Facility Staff Regarding COVID-19 Vaccine Hesitancy. J. Am. Geriatr. Soc. 2021, 69, 1140–1146. [Google Scholar] [CrossRef]
- Klugar, M.; Riad, A.; Mohanan, L.; Pokorná, A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Workers in Czechia: National Cross-Sectional Study. Vaccines 2021, 9, 1437. [Google Scholar] [CrossRef]
- Paul, E.; Fancourt, D. Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Booster Vaccine: An Observational Study of 22,139 Fully Vaccinated Adults in the UK. Lancet Reg. Health—Eur. 2022, 14, 100317. [Google Scholar] [CrossRef]
- Paris, C.; Bénézit, F.; Geslin, M.; Polard, E.; Baldeyrou, M.; Turmel, V.; Tadié, É.; Garlantezec, R.; Tattevin, P. COVID-19 Vaccine Hesitancy among Healthcare Workers. Infect. Dis. Now. 2021, 51, 484–487. [Google Scholar] [CrossRef]
- Qin, C.; Wang, R.; Tao, L.; Liu, M.; Liu, J. Acceptance of a Third Dose of COVID-19 Vaccine and Associated Factors in China Based on Health Belief Model: A National Cross-Sectional Study. Vaccines 2022, 10, 89. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H.; et al. COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among Front-Line Health-Care Workers and the General Community: A Prospective Cohort Study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and Mental Health Impacts of COVID-19 on Healthcare Workers: A Scoping Review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Da Molin, G.; Diella, G.; Montagna, M.T.; Ferracuti, S.; Liguori, G.; Orsi, G.B.; Napoli, C. Acceptance of COVID-19 Vaccination in the Elderly: A Cross-Sectional Study in Southern Italy. Vaccines 2021, 9, 1222. [Google Scholar] [CrossRef]
- Yadete, T.; Batra, K.; Netski, D.M.; Antonio, S.; Patros, M.J.; Bester, J.C. Assessing Acceptability of COVID-19 Vaccine Booster Dose among Adult Americans: A Cross-Sectional Study. Vaccines 2021, 9, 1424. [Google Scholar] [CrossRef] [PubMed]
- Biddle, N.; Sollis, K. Who Wants to Get Boosted? COVID-19 Vaccine Uptake in Australia in January 2022. Available online: https://csrm.cass.anu.edu.au/research/publications/who-wants-get-boosted-covid-19-vaccine-uptake-australia-january-2022 (accessed on 13 March 2022).
- Martin, C.A.; Woolf, K.; Bryant, L.; Carr, S.; Gray, L.J.; Gupta, A.; Guyatt, A.L.; John, C.; Melbourne, C.; McManus, I.C.; et al. Persistent Hesitancy for SARS-CoV-2 Vaccines among Healthcare Workers in the United Kingdom: Analysis of Longitudinal Data from the UK-REACH Cohort Study. Lancet Reg. Health Eur. 2022, 13, 100299. [Google Scholar] [CrossRef] [PubMed]
- Belingheri, M.; Roncalli, M.; Riva, M.A.; Paladino, M.E.; Teruzzi, C.M. COVID-19 Vaccine Hesitancy and Reasons for or against Adherence among Dentists. J. Am. Dent. Assoc. 2021, 152, 740–746. [Google Scholar] [CrossRef] [PubMed]
| Study Variables | COVID-19 Vaccine 1st Dose Delay (Days) | COVID-19 Vaccine Booster Dose Delay (Days) | ||||||
|---|---|---|---|---|---|---|---|---|
| n (%) | Mean (CI) | Median (CI) | p | n (%) | Mean (CI) | Median (CI) | p | |
| 890 (100%) | 69.1 (64.4, 73.8) | 39 (32, 46) | 558 (62.1%) | 28.8 (27.2, 30.4) | 24 (21.3, 26.7) | |||
| Sex | <0.001 | 0.782 | ||||||
| Female | 757 (85.1%) | 72.4 (67.2, 77.6) | 41 (34.5, 47.5) | 466 (83.5%) | 29 (27.2, 30.7) | 26 (23.2, 28.8) | ||
| Male | 133 (14.9%) | 50.1 (39.8, 60.4) | 19 (12.6, 25.4) | 92 (16.5%) | 27.4 (23.4, 31.5) | 19 (13.3, 24.7) | ||
| Clinic | 0.072 | 0.044 | ||||||
| Central Office | 138 (15.5%) | 73.4 (61.8, 85.1) | 45 (38.9, 51.1) | 87 (15.6%) | 31.8 (27.7, 36.0) | 30 (23.1, 36.9) | ||
| Clinic A | 120 (13.5%) | 59.6 (46.2, 73.1) | 20 (10.7, 29.3) | 76 (13.6%) | 29.3 (24.9, 33.7) | 24 (12.3, 35.7) | ||
| Clinic B | 91 (10.2%) | 66.2 (51.4, 81) | 25 (14.9, 35.1) | 62 (11.1%) | 24.7 (20.8, 28.5) | 22 (18.2, 25.8) | ||
| Clinic C | 128 (14.4%) | 62.6 (50.8, 74.5) | 20 (8.17, 31.8) | 80 (14.3%) | 30.9 (26.8, 35.0) | 27 (19.4, 34.6) | ||
| Clinic D | 88 (9.9%) | 72.4 (58.8, 86) | 49 (37.5, 60.5) | 53 (9.5%) | 31.1 (25.6, 36.6) | 30 (18.5, 41.5) | ||
| Clinic E | 148 (16.6%) | 77.7 (65.5, 89.9) | 39 (11, 67) | 94 (16.8%) | 24.9 (21.1, 28.7) | 20 (16.1, 23.9) | ||
| Clinic F | 104 (11.7%) | 55.3 (43.6, 66.9) | 31 (13.5, 48.5) | 74 (13.3%) | 25.9 (21.3, 30.5) | 18 (10.3, 25.7) | ||
| Clinic G | 73 (8.2%) | 89.6 (69.8, 109) | 57 (39.3, 74.7) | 32 (5.73%) | 31.8 (25.1, 38.4) | 19 (1.85, 36.2) | ||
| Profession | 0.019 | 0.028 | ||||||
| Administration * | 122 (13.7%) | 74.1 (61.2, 86.9) | 45 (39, 51) | 71 (12.7%) | 34.6 (30.3, 38.9) | 34 (24.2, 43.8) | ||
| Allied Health + | 42 (4.7%) | 73.3 (48.9, 97.8) | 28 (5.77, 50.2) | 21 (3.76%) | 34.2 (26.6, 41.8) | 33 (20.5, 45.5) | ||
| Ancillary ^ | 331 (37.2%) | 73.9 (66.4, 81.4) | 47 (35.6, 58.4) | 203 (36.3%) | 29.4 (26.7, 32) | 26 (22.2, 29.8) | ||
| Medical # | 165 (18.5%) | 53.3 (43.9, 62.8) | 19 (13.4, 24.6) | 114 (20.4%) | 24.7 (21, 28.4) | 16 (11, 21) | ||
| Nursing | 230 (25.8%) | 70.1 (59.9, 80.3) | 22 (12.6, 31.4) | 149 (26.7%) | 26.9 (23.9, 29.9) | 22 (18.8, 25.2) | ||
| Administration | Allied Health | Ancillary | Medical | Nursing | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Profession | Chi-Square | p | Chi-Square | p | Chi-Square | p | Chi-Square | p | Chi-Square | p |
| Administration | 0.094 | 0.759 | 0.022 | 0.881 | 7.31 | 0.007 | 0.089 | 0.765 | ||
| Allied Health | 0.094 | 0.759 | 0.355 | 0.551 | 2.99 | 0.084 | 0.280 | 0.597 | ||
| Ancillary | 0.022 | 0.881 | 0.355 | 0.551 | 11.7 | <0.001 | 0.005 | 0.946 | ||
| Medical | 7.31 | 0.007 | 2.99 | 0.084 | 11.7 | <0.001 | 5.36 | 0.021 | ||
| Nursing | 0.089 | 0.765 | 0.28 | 0.597 | 0.005 | 0.946 | 5.36 | 0.021 | ||
| Administration | Allied Health | Ancillary | Medical | Nursing | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Profession | Chi-Square | p | Chi-Square | p | Chi-Square | p | Chi-Square | p | Chi-Square | p |
| Administration | 0.109 | 0.742 | 2.53 | 0.111 | 6.17 | 0.013 | 6.81 | 0.009 | ||
| Allied Health | 0.109 | 0.742 | 1.87 | 0.172 | 3.88 | 0.049 | 3.95 | 0.047 | ||
| Ancillary | 2.53 | 0.111 | 1.87 | 0.172 | 2.01 | 0.156 | 1.79 | 0.181 | ||
| Medical | 6.17 | 0.013 | 3.88 | 0.049 | 2.01 | 0.156 | 0.116 | 0.734 | ||
| Nursing | 6.81 | 0.009 | 3.95 | 0.047 | 1.79 | 0.181 | 0.116 | 0.734 | ||
| Study Variables | B | p | HR | 95% CI for HR | |
|---|---|---|---|---|---|
| Coefficient | Lower | Upper | |||
| Sex | |||||
| Female | 1 | ||||
| Male | −0.007 | 0.958 | 0.993 | 0.762 | 1.30 |
| Clinic | |||||
| Clinic A | 1 | ||||
| Central Office | 0.367 | 0.08 | 1.44 | 0.957 | 2.18 |
| Clinic B | 0.278 | 0.108 | 1.32 | 0.941 | 1.85 |
| Clinic C | −0.084 | 0.603 | 0.92 | 0.67 | 1.26 |
| Clinic D | −0.06 | 0.74 | 0.942 | 0.661 | 1.34 |
| Clinic E | 0.258 | 0.098 | 1.29 | 0.954 | 1.76 |
| Clinic F | 0.193 | 0.238 | 1.21 | 0.88 | 1.67 |
| Clinic G | −0.273 | 0.197 | 0.761 | 0.502 | 1.15 |
| Profession | |||||
| Administration | 1 | ||||
| Allied Health | 0.063 | 0.831 | 1.07 | 0.598 | 1.90 |
| Ancillary | 0.427 | 0.035 | 1.53 | 1.03 | 2.28 |
| Medical | 0.588 | 0.006 | 1.8 | 1.18 | 2.74 |
| Nursing | 0.586 | 0.006 | 1.8 | 1.18 | 2.73 |
| Time to dose 1 | −0.003 | 0.003 | 0.997 | 0.994 | 0.999 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koh, S.W.C.; Tan, H.M.; Lee, W.H.; Mathews, J.; Young, D. COVID-19 Vaccine Booster Hesitancy among Healthcare Workers: A Retrospective Observational Study in Singapore. Vaccines 2022, 10, 464. https://doi.org/10.3390/vaccines10030464
Koh SWC, Tan HM, Lee WH, Mathews J, Young D. COVID-19 Vaccine Booster Hesitancy among Healthcare Workers: A Retrospective Observational Study in Singapore. Vaccines. 2022; 10(3):464. https://doi.org/10.3390/vaccines10030464
Chicago/Turabian StyleKoh, Sky Wei Chee, Hwei Ming Tan, Wayne Han Lee, Jancy Mathews, and Doris Young. 2022. "COVID-19 Vaccine Booster Hesitancy among Healthcare Workers: A Retrospective Observational Study in Singapore" Vaccines 10, no. 3: 464. https://doi.org/10.3390/vaccines10030464
APA StyleKoh, S. W. C., Tan, H. M., Lee, W. H., Mathews, J., & Young, D. (2022). COVID-19 Vaccine Booster Hesitancy among Healthcare Workers: A Retrospective Observational Study in Singapore. Vaccines, 10(3), 464. https://doi.org/10.3390/vaccines10030464






