Susceptibility to Vaccine-Preventable Diseases in Four Districts of Xaysomboun Province, Lao People’s Democratic Republic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Serology Testing
2.3. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Hepatitis B Virus (HBV)
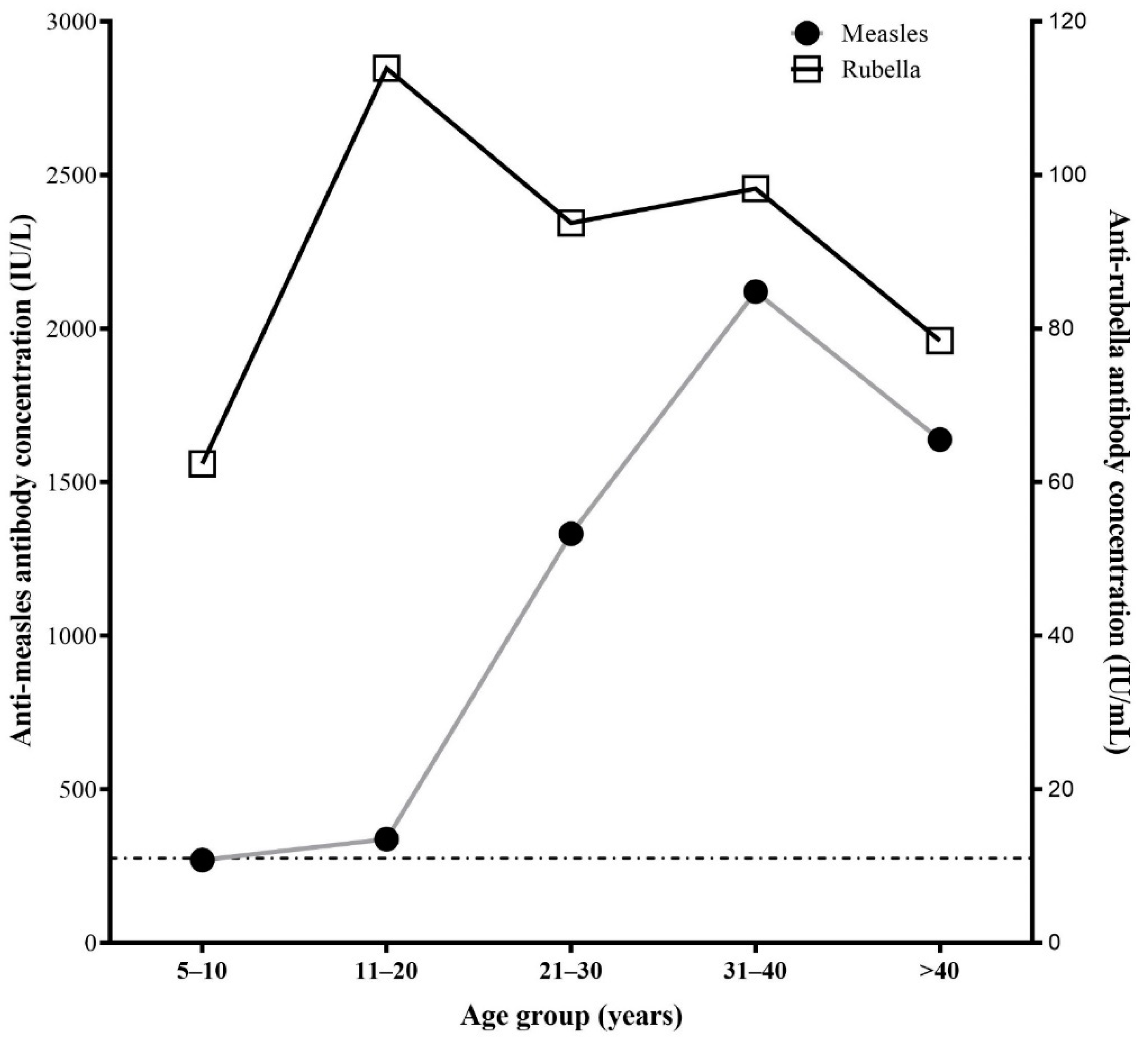
3.3. Measles and Rubella
3.4. Tetanus
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rodrigues, C.M.C.; Plotkin, S.A. Impact of Vaccines; Health, Economic and Social Perspectives. Front. Microbiol. 2020, 11, 1526. [Google Scholar] [CrossRef] [PubMed]
- Cutts, F.T.; Hanson, M. Seroepidemiology: An underused tool for designing and monitoring vaccination programmes in low- and middle-income countries. Trop. Med. Int. Health 2016, 21, 1086–1098. [Google Scholar] [CrossRef] [PubMed]
- Funk, S.; Knapp, J.K.; Lebo, E.; Reef, S.E.; Dabbagh, A.J.; Kretsinger, K.; Jit, M.; Edmunds, W.J.; Strebel, P.M. Combining serological and contact data to derive target immunity levels for achieving and maintaining measles elimination. BMC Med. 2019, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jutavijittum, P.; Andernach, I.E.; Yousukh, A.; Samountry, B.; Samountry, K.; Thammavong, T.; Keokhamphue, J.; Toriyama, K.; Muller, C.P. Occult hepatitis B infections among blood donors in Lao PDR. Vox Sang. 2014, 106, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Black, A.P.; Nouanthong, P.; Nanthavong, N.; Souvannaso, C.; Vilivong, K.; Jutavijittum, P.; Samountry, B.; Lütteke, N.; Hübschen, J.M.; Goossens, S.; et al. Hepatitis B virus in the Lao People’s Democratic Republic: A cross sectional serosurvey in different cohorts. BMC Infect. Dis. 2014, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Black, A.P.; Vilivong, K.; Nouanthong, P.; Souvannaso, C.; Hübschen, J.M.; Muller, C.P. Serosurveillance of vaccine preventable diseases and hepatitis C in healthcare workers from Lao PDR. PLoS ONE 2015, 10, e0123647. [Google Scholar] [CrossRef] [PubMed]
- Xaydalasouk, K.; Strobel, M.; Buisson, Y.; Black, A.P.; Muller, P. Seroprevalence and risk factors of hepatitis B and C virus infections in female workers of Lao garment factories. PLoS ONE 2018, e0199919. [Google Scholar] [CrossRef] [PubMed]
- Edmunds, W.J.; Medley, G.F.; Nokes, D.J.; Hall, A.J.; Whittle, H.C. The influence of age on the development of the hepatitis B carrier state. Proc. R. Soc. B Biol. Sci. 1993, 253, 197–201. [Google Scholar]
- World Cancer Research Fund Liver Cancer Statistics. Available online: www.wcrf.org/dietandcancer/liver-cancer-statistics (accessed on 30 December 2021).
- World Health Organization. WHO Vaccine-Preventable Diseases: Monitoring System. 2020 Global Summary. 2020. Available online: https://apps.who.int/immunization_monitoring/globalsummary (accessed on 30 November 2020).
- Lao Statistics Bureau; UNICEF. Lao Social Indicator Survey II, 2017; Lao Statistics Bureau and UNICEF, Lao PDR. Survey Findings Report. 2017. Available online: https://www.unicef.org/eap/sites/unicef.org.eap/files/2018-06/Summary%20Survey%20Findings%20Report%20an%20statistical%20snapshots%20of%20Lao%20Social%20Indicator%20Survey%20II.pdf. (accessed on 30 December 2021).
- Hefele, L.; Vannachone, S.; Khounvisith, V.; Nouanthong, P.; Sayasone, S.; Kounnavong, S.; Chanthavilay, P.; Muller, C.P.; Black, A.P. Lasting benefit of infant hepatitis B vaccination in adolescents in the Lao People’s Democratic Republic. Int. J. Infect. Dis. 2020, 93, 217–223. [Google Scholar] [CrossRef]
- Nouanthong, P.; Hefele, L.; Keokhamphue, J.; Sorrasin, V.; Khounvisith, V.; Souksakhone, C.; Jutavijittum, P.; Muller, C.P.; Black, A.P.; Hübschen, J.M. Analyses of blood donor samples from eight provinces in Lao PDR suggest considerable variation concerning HBV exposure and carriage. PLoS ONE 2021, 16, e0259814. [Google Scholar] [CrossRef]
- Hachiya, M.; Miyano, S.; Mori, Y.; Vynnycky, E.; Keungsaneth, P.; Vongphrachanh, P.; Xeuatvongsa, A.; Sisouk, T.; Som-Oulay, V.; Khamphaphongphane, B.; et al. Evaluation of nationwide supplementary immunization in Lao People’s Democratic Republic: Population-based seroprevalence survey of anti-measles and anti-rubella IgG in children and adults, mathematical modelling and a stability testing of the vaccine. PLoS ONE 2018, 13, e0194931. [Google Scholar] [CrossRef] [PubMed]
- WHO International Review of the Expanded Programme on Immunization. 2012, pp. 1–19. Available online: www.wpro.who.int/immunization/.../Intl_Review_of_EPI_in_Lao.pdf (accessed on 30 December 2021).
- Ministry of Health and Lao Statistics Bureau 2012. Lao Social Indicator Study (LSIS) 2011–2012. Ministry of Health and Lao Statistics Bureau. Lao Soc. Indic. Study 2012, 12, 1–496. Available online: https://dhsprogram.com/pubs/pdf/FR268/FR268.pdf (accessed on 30 December 2021).
- Sein, C.; Tiwari, T.; Macneil, A.; Wannemuehler, K.; Soulaphy, C.; Souliphone, P.; Reyburn, R.; Ramirez Gonzalez, A.; Watkins, M.; Goodson, J.L. Diphtheria outbreak in Lao People’s Democratic Republic, 2012–2013. Vaccine 2016, 34, 4321–4326. [Google Scholar] [CrossRef] [PubMed]
- Nanthavong, N.; Black, A.P.; Nouanthong, P.; Souvannaso, C.; Vilivong, K.; Muller, C.P.; Goossens, S.; Quet, F.; Buisson, Y. Diphtheria in Lao PDR: Insufficient coverage or ineffective vaccine? PLoS ONE 2015, 10, e0121749. [Google Scholar] [CrossRef] [PubMed]
- Kleine, D.; Billamay, S.; Chanthavilay, P.; Mongkhoune, S.; Keokhamphoui, C.; Souksakhone, C.; Nouanthong, P.; Khamphaphongphane, B.; Muller, C.P.; Black, A.P. Pertussis in Lao PDR: Seroprevalence and disease. Int. J. Infect. Dis. 2020, 95, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Ounnavong, P.; Chanthavilay, P.; Khampanisong, P.; Reinharz, D.; Muller, C.P.; Black, A.P. Seroprevalence of anti-tetanus antibodies in mothers and cord blood and associated factors in health-care settings in Lao People’s Democratic Republic. Vaccine 2020, 38, 1234–1240. [Google Scholar] [CrossRef]
- The Study on the Improvement of Health and Medical Services in the Lao People’s Democratic Republic: Lao Health Master Planning Study; Progress Report 1; Japan International Cooperation Agency: Vientiane, Laos, 2002.
- Lao Statistics Bureau. The 4th Population and Housing Census 2015. 2016. Available online: http://lao.unfpa.org/sites/default/files/pub-pdf/PHC-ENG-FNAL-WEB_0.pdf%0Ahttp://www.lsb.gov.la/lsb/pdf/PHC-ENG-FNAL-WEB.pdf (accessed on 30 December 2021).
- Hefele, L.; Syphan, S.; Xayavong, D.; Homsana, A.; Kleine, D.; Chanthavilay, P.; Nouanthong, P.; Xaydalasouk, K.; Phathammavong, O.; Billamay, S.; et al. Seroprotection at Different Levels of the Healthcare System after Routine Vaccination with Diphtheria-Tetanus-Pertussis whole cell-Hepatitis B-Haemophilus influenzae Type B in Lao People’s Democratic Republic. Clin. Infect. Dis. 2019, 69, 2136–2144. [Google Scholar] [CrossRef]
- Evdokimov, K.; Sayasinh, K.; Nouanthong, P.; Vilivong, K.; Samountry, B.; Phonekeo, D.; Strobel, M.; Haegeman, F.; Heimann, P.; Muller, C.P.; et al. Low and disparate seroprotection after pentavalent childhood vaccination in the Lao People’s Democratic Republic: A cross-sectional study. Clin. Microbiol. Infect. 2017, 23, 197–202. [Google Scholar] [CrossRef][Green Version]
- Van Damme, P.; Van Herck, K. A review of the long-term protection after hepatitis A and B vaccination. Travel Med. Infect. Dis. 2007, 5, 79–84. [Google Scholar] [CrossRef]
- Van Herck, K.; Van Damme, P. Benefits of early hepatitis B immunization programs for newborns and infants. Pediatr. Infect. Dis. J. 2008, 27, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Xaydalasouk, K.; Sayasinh, K.; Hübschen, J.M.; Khounvisith, V.; Keomany, S.; Muller, C.P.; Black, A.P. Age-stratified seroprevalence of vaccine-preventable infectious disease in Saravan, Southern Lao People’s Democratic Republic. Int. J. Infect. Dis. 2021, 107, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Kolwaite, A.R.; Xeuatvongsa, A.; Ramirez-Gonzalez, A.; Wannemuehler, K.; Vongxay, V.; Vilayvone, V.; Hennessey, K.; Patel, M.K. Hepatitis B vaccine stored outside the cold chain setting: A pilot study in rural Lao PDR. Vaccine 2016, 34, 3324–3330. [Google Scholar] [CrossRef] [PubMed]
- Leroi, C.; Adam, P.; Khamduang, W.; Kawilapat, S.; Ngo-Giang-Huong, N.; Ongwandee, S.; Jiamsiri, S.; Jourdain, G. Prevalence of chronic hepatitis B virus infection in Thailand: A systematic review and meta-analysis. Int. J. Infect. Dis. 2016, 51, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Men, P.; Xiao, Y.; Gao, P.; Lv, M.; Yuan, Q.; Chen, W.; Bai, S.; Wu, J. Hepatitis B infection in the general population of China: A systematic review and meta-analysis. BMC Infect. Dis. 2019, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bester, J.C. Measles and measles vaccination a review. JAMA Pediatr. 2016, 170, 1209–1215. [Google Scholar] [CrossRef] [PubMed]
- Nouanthong, P.; Hübschen, J.M.; Billamay, S.; Mongkhoune, S.; Vilivong, K.; Khounvisith, V.; Sinner, R.; Grandadam, M.; Phonekeo, D.; Black, A.P.; et al. Varicella zoster and fever rash surveillance in Lao People’s Democratic Republic. BMC Infect. Dis. 2019, 19, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Vynnycky, E.; Miyano, S.; Komase, K.; Mori, Y.; Takeda, M.; Kitamura, T.; Xeuatvongsa, A.; Hachiya, M. Estimating the immunogenicity of measles-rubella vaccination administered during a mass campaign in Lao People’s Democratic Republic using multi-valent seroprevalence data. Sci. Rep. 2019, 9, 12545. [Google Scholar] [CrossRef]
- Thuy, D.B.; Campbell, J.I.; Thanh, T.T.; Thuy, C.T.; Loan, H.T.; Van Hao, N.; Minh, Y.L.; Van Tan, L.; Boni, M.F.; Thwaites, C.L. Tetanus in Southern Vietnam: Current situation. Am. J. Trop. Med. Hyg. 2017, 96, 93–96. [Google Scholar] [CrossRef]
- Schlumberger, M.; Yvonnet, B.; Que, H.V.T.; Chhem, D.B.; Saliou, P.; Le Tu, T.C.; Glaziou, P. Serological study carried out in Cambodia during a tetanus vaccination in adults. Bull. Soc. Pathol. Exot. 2008, 101, 36–42. [Google Scholar]
- Hanvatananukul, P.; Prasarakee, C.; Sarachai, S.; Aurpibul, L.; Sintupat, K.; Khampan, R.; Saheng, J.; Sudjaritruk, T. Seroprevalence of antibodies against diphtheria, tetanus, and pertussis among healthy Thai adolescents. Int. J. Infect. Dis. 2020, 96, 422–430. [Google Scholar] [CrossRef]
- Kitamura, T.; Komada, K.; Xeuatvongsa, A.; Hachiya, M. Factors affecting childhood immunization in lao people’s democratic republic: A cross-sectional study from nationwide, populationbased, multistage cluster sampling. Biosci. Trends 2013, 7, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Phimmasane, M.; Douangmala, S.; Koffi, P.; Reinharz, D.; Buisson, Y. Factors affecting compliance with measles vaccination in Lao PDR. Vaccine 2010, 28, 6723–6729. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | N (%) | |
|---|---|---|
| Sex | Female | 222 (61.2) |
| Male | 141 (38.8) | |
| Age groups (years) | 5–10 | 72 (19.8) |
| 11–20 | 85 (23.4) | |
| 21–30 | 66 (18.2) | |
| 31–40 | 45 (12.4) | |
| >40 | 95 (26.2) | |
| Ethnicity | Lao-Tai | 141 (38.8) |
| Hmong-Mien | 156 (42.9) | |
| Mone-Khmer | 66 (18.2) | |
| Religion | Animist | 243 (66.9) |
| Buddhist | 120 (33.1) | |
| District | Longxarn | 93 (25.6) |
| Hom | 83 (22.9) | |
| Longchaeng | 82 (22.6) | |
| Thathom | 105 (28.9) | |
| Place of birth | Provincial hospital | 18 (4.9) |
| District hospital | 41 (11.3) | |
| Health center | 19 (5.2) | |
| At home | 285 (78.5) | |
| Marital status | Single | 155 (42.7) |
| Married | 208 (57.3) | |
| Education | None | 118 (32.5) |
| Elementary | 123 (33.9) | |
| Secondary/high school | 107 (29.5) | |
| University | 15 (4.1) | |
| Family monthly income (Kip) * | <1,000,000 | 33 (9.1) |
| 1,000,000–3,000,000 | 301 (82.9) | |
| >3,000,000 | 29 (8.0) | |
| Age Group (years) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anti-HBs | Anti-HBc | HBsAg | 5–10 | 11–20 | 21–30 | 31–40 | >40 | Total | |||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | ||||
| - | - | - | 21/35 (60.0) | 20/37 (54.1) | 11/36 (30.6) | 26/49 (53.1) | 3/25 (12.0) | 9/41 (21.9) | 0/9 (0) | 6/36 (16.7) | 3/36 (8.4) | 10/59 (16.9) | 109/363 (30.1) |
| + | - | - | 10/35 (28.6) | 11/37 (29.7) | 9/36 (25.0) | 6/49 (12.2) | 4/25 (16.0) | 2/41 (4.9) | 0/9 (0) | 0/36 (0) | 6/36 (16.6) | 2/59 (3.4) | 50/363 (13.8) |
| + | + | - | 3/35 (8.6) | 5/37 (13.5) | 8/36 (22.2) | 11/49 (22.4) | 16/25 (64.0) | 18/41(43.9) | 6/9 (66.6) | 18/36 (50.0) | 12/36 (33.4) | 24/59 (40.7) | 121/363 (33.3) |
| - | + | - | 1/35 (2.8) | 0/37 (0) | 2/36 (5.5) | 5/49 (10.2) | 0/25 (0) | 7/41 (17.1) | 0/9 (0) | 6/36 (16.7) | 9/36 (25.0) | 19/59 (32.2) | 49/363 (13.5) |
| - | + | + | 0/35 (0) | 1/37 (2.7) | 6/36 (16.7) | 1/49 (2.1) | 2/25 (8.0) | 5/41 (12.2) | 3/9 (33.4) | 6/36 (16.7) | 6/36 (16.6) | 4/59 (6.8) | 34/363 (9.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Virachith, S.; Lao, M.; Inthepphavong, M.; Inthalath, S.; Hübschen, J.M.; Kounnavong, S.; Sayasone, S.; Black, A.P. Susceptibility to Vaccine-Preventable Diseases in Four Districts of Xaysomboun Province, Lao People’s Democratic Republic. Vaccines 2022, 10, 463. https://doi.org/10.3390/vaccines10030463
Virachith S, Lao M, Inthepphavong M, Inthalath S, Hübschen JM, Kounnavong S, Sayasone S, Black AP. Susceptibility to Vaccine-Preventable Diseases in Four Districts of Xaysomboun Province, Lao People’s Democratic Republic. Vaccines. 2022; 10(3):463. https://doi.org/10.3390/vaccines10030463
Chicago/Turabian StyleVirachith, Siriphone, Mapor Lao, Magnoula Inthepphavong, Saythong Inthalath, Judith M. Hübschen, Sengchanh Kounnavong, Somphou Sayasone, and Antony P. Black. 2022. "Susceptibility to Vaccine-Preventable Diseases in Four Districts of Xaysomboun Province, Lao People’s Democratic Republic" Vaccines 10, no. 3: 463. https://doi.org/10.3390/vaccines10030463
APA StyleVirachith, S., Lao, M., Inthepphavong, M., Inthalath, S., Hübschen, J. M., Kounnavong, S., Sayasone, S., & Black, A. P. (2022). Susceptibility to Vaccine-Preventable Diseases in Four Districts of Xaysomboun Province, Lao People’s Democratic Republic. Vaccines, 10(3), 463. https://doi.org/10.3390/vaccines10030463






