COVID-19 Vaccine Hesitancy and Associated Factors among People with HIV in the United States: Findings from a National Survey
Abstract
:1. Introduction
2. Methods
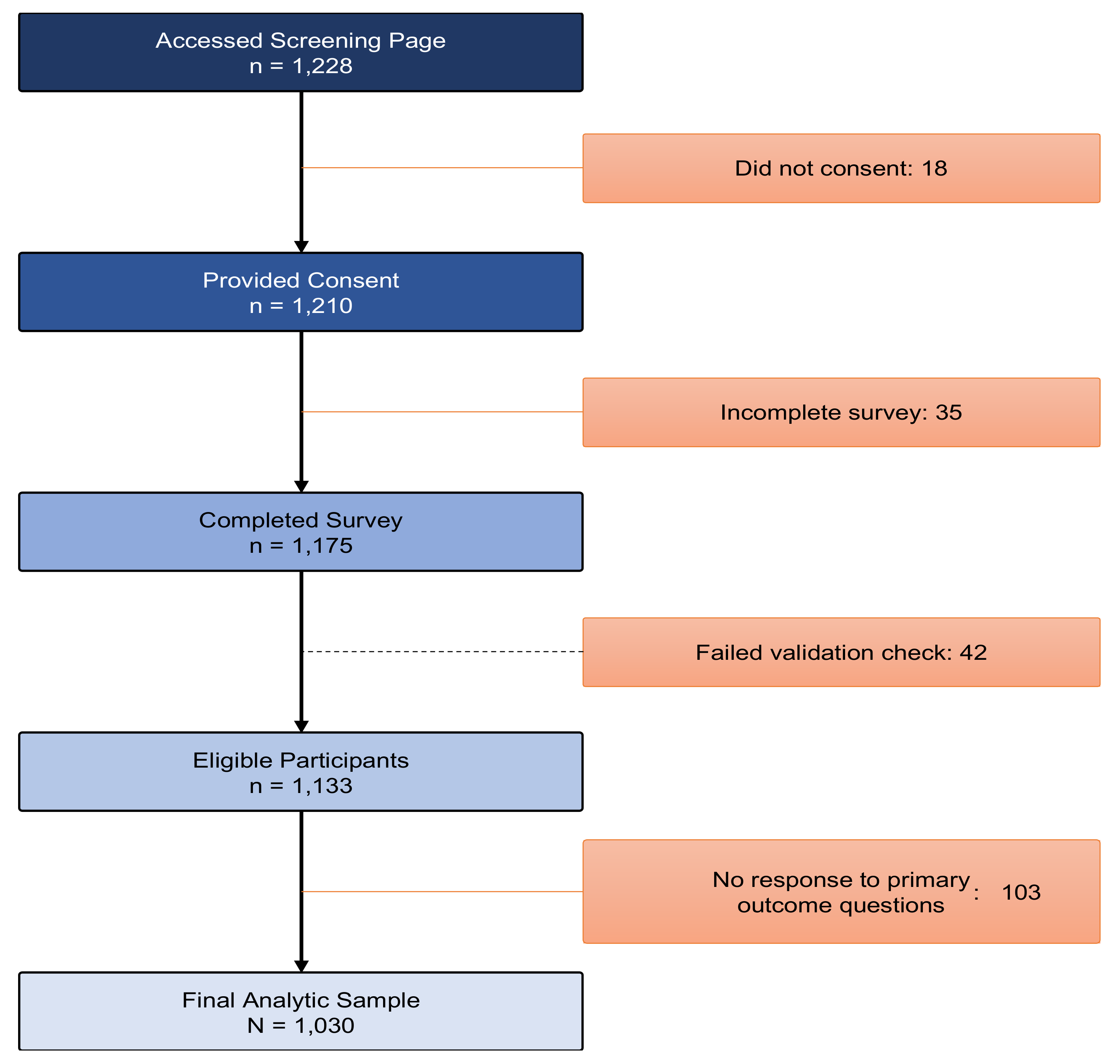
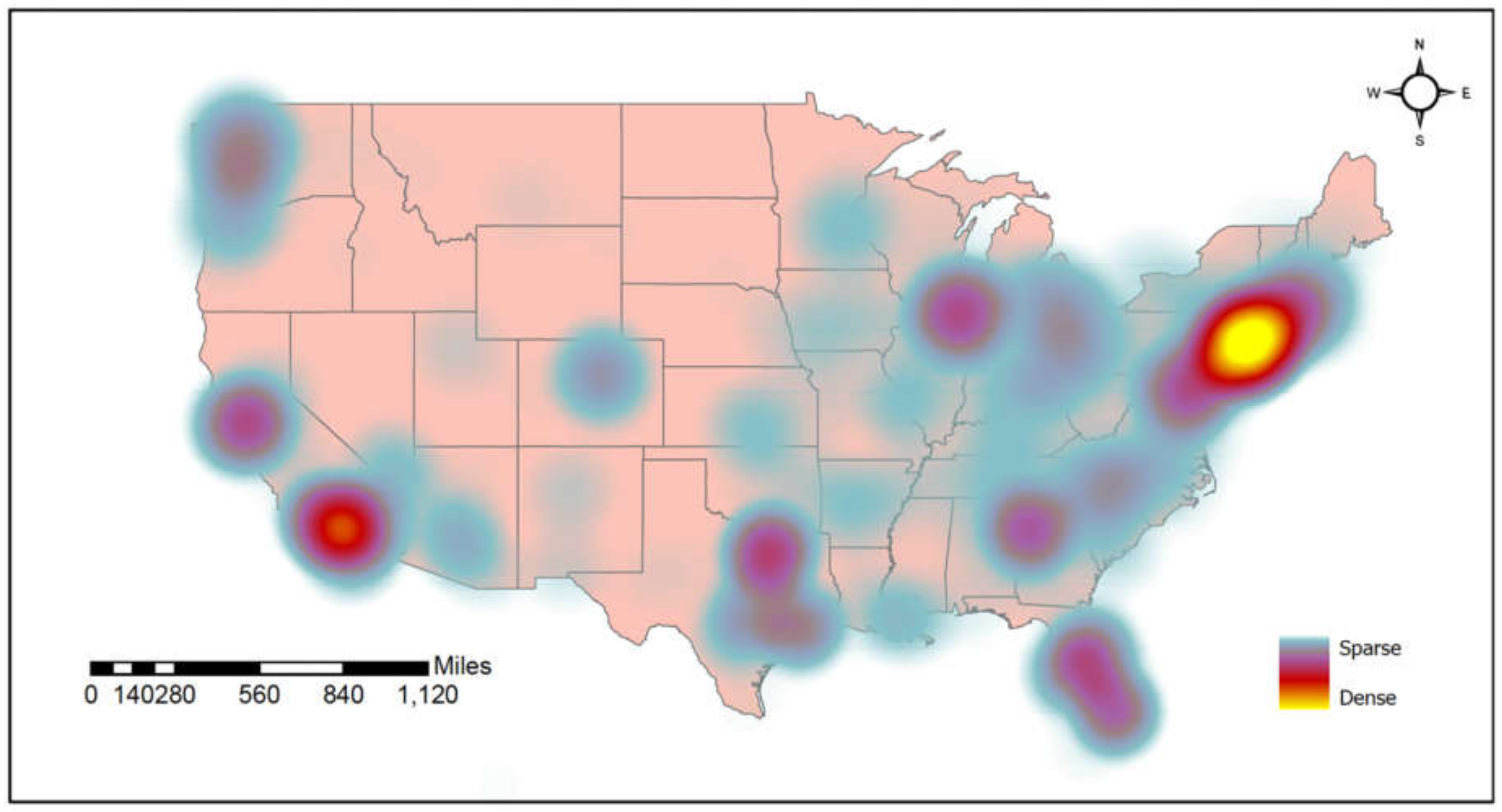
2.1. Study Design and Participants
2.2. Study Procedures
2.3. Study Measures
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- US Food and Drug Administration. COVID-19 Vaccines. 2021. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines (accessed on 5 January 2022).
- Centers for Disease Control and Prevention. Federal Retail Pharmacy Partnership Program for COVID-19 Vaccination Faqs. 2021. Available online: https://www.cdc.gov/vaccines/covid-19/retail-pharmacy-program/index.html (accessed on 6 January 2022).
- World Health Organization. Coronavirus Disease (COVID-19): Herd Immunity, Lockdowns and COVID-19. 2020. Available online: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19 (accessed on 7 March 2021).
- Fisk, R.J. Barriers to vaccination for COVID-19 control—Experience from the United States. Glob. Health J. 2021, 5, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Latkin, A.C.; Dayton, L.; Yi, G.; Konstantopoulos, A.; Boodram, B. Trust in a COVID-19 vaccine in the U.S.: A social-ecological perspective. Soc. Sci. Med. 2021, 270, 113684. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Bogart, L.M.; Ojikutu, B.O.; Tyagi, K.; Klein, D.J.; Mutchler, M.G.; Dong, L.; Lawrence, S.J.; Thomas, D.R.; Kellman, S. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among black Americans living with HIV. JAIDS J. Acquir. Immune Defic. Syndr. 2020, 86, 200–207. [Google Scholar] [CrossRef]
- Becker, G.; Newsom, E. Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am. J. Public Health 2003, 93, 742–748. [Google Scholar] [CrossRef]
- McMaughan, D.J.; Oloruntoba, O.; Smith, M.L. Socioeconomic status and access to healthcare: Interrelated drivers for healthy aging. Front. Public Health 2020, 8, 231. [Google Scholar] [CrossRef]
- Arpey, N.C.; Gaglioti, A.; Rosenbaum, M.E. How socioeconomic status affects patient perceptions of health care: A qualitative study. J. Prim. Care Community Health 2017, 8, 169–175. [Google Scholar] [CrossRef] [Green Version]
- Turan, J.M.; Elafros, M.A.; Logie, C.H.; Banik, S.; Turan, B.; Crockett, K.B.; Pescosolido, B.; Murray, S.M. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019, 17, 7. [Google Scholar] [CrossRef] [Green Version]
- Washington, H.A. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present; Doubleday Books: New York, NY, USA, 2006. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). People at Increased Risk. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html (accessed on 5 January 2022).
- Centers for Disease Control and Prevention. People with Certain Medical Conditions. 12 May 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 12 July 2021).
- Tesoriero, J.M.; Swain, C.-A.E.; Pierce, J.L.; Zamboni, L.; Wu, M.; Holtgrave, D.R.; Gonzalez, C.J.; Udo, T.; Morne, J.E.; Hart-Malloy, R.; et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw. Open 2021, 4, e2037069. [Google Scholar] [CrossRef]
- Sun, J.; Patel, R.C.; Zheng, Q.; Madhira, V.; Olex, A.L.; Islam, J.Y.; French, E.; Chiang, T.P.-Y.; Akselrod, H.; Moffitt, R.; et al. Covid-19 disease severity among people with HIV infection or solid organ transplant in the United States: A nationally-representative, multicenter, observational cohort study. medRxiv 2021. [Google Scholar] [CrossRef]
- Lesko, C.R.; Bengtson, A.M. HIV and COVID-19: Intersecting epidemics with many unknowns. Am. J. Epidemiol. 2020, 190, 10–16. [Google Scholar] [CrossRef]
- Yang, X.; Sun, J.; Patel, R.C.; Zhang, J.; Guo, S.; Zheng, Q.; Olex, A.L.; Olatosi, B.; Weissman, S.B.; Islam, J.Y.; et al. Associations between HIV infection and clinical spectrum of COVID-19: A population level analysis based on US National COVID Cohort Collaborative (N3C) data. Lancet HIV 2021, 8, e690–e700. [Google Scholar] [CrossRef]
- Nomah, K.D.; Reyes-Urueña, J.; Díaz, Y.; Moreno, S.; Aceiton, J.; Bruguera, A.; Vivanco-Hidalgo, R.M.; Llibre, J.M.; Domingo, P.; Falcó, V.; et al. Sociodemographic, clinical, and immunological factors associated with SARS-CoV-2 diagnosis and severe Covid-19 outcomes in people living with HIV: A retrospective cohort study. Lancet HIV 2021, 8, e701–e710. [Google Scholar] [CrossRef]
- Pinto, R.M.; Park, S. COVID-19 pandemic disrupts HIV continuum of care and prevention: Implications for research and practice concerning community-based organizations and frontline providers. AIDS Behav. 2020, 24, 2486–2489. [Google Scholar] [CrossRef]
- Shiau, S.; Krause, K.D.; Valera, P.; Swaminathan, S.; Halkitis, P.N. The burden of COVID-19 in people living with HIV: A syndemic perspective. AIDS Behav. 2020, 24, 2244–2249. [Google Scholar] [CrossRef]
- Brincks, A.M.; Shiu-Yee, K.; Metsch, L.R.; Del Rio, C.; Schwartz, R.P.; Jacobs, P.; Osorio, G.; Sorensen, J.L.; Feaster, D.J. Physician mistrust, medical system mistrust, and perceived discrimination: Associations with HIV care engagement and viral load. AIDS Behav. 2019, 23, 2859–2869. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of web surveys: The checklist for reporting results of internet E-surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Teitcher, E.J.; Bockting, W.O.; Bauermeister, J.A.; Hoefer, C.J.; Miner, M.H.; Klitzman, R.L. Detecting, preventing, and responding to “Fraudsters” in internet research: Ethics and tradeoffs. J. Law Med. Ethics 2015, 43, 116–133. [Google Scholar] [CrossRef] [Green Version]
- Bradley, K.A.; DeBenedetti, A.F.; Volk, R.J.; Williams, E.C.; Frank, D.; Kivlahan, D.R. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol. Clin. Exp. Res. 2007, 31, 1208–1217. [Google Scholar] [CrossRef]
- Gilkey, M.B.; Magnus, B.E.; Reiter, P.L.; McRee, A.-L.; Dempsey, A.F.; Brewer, N.T. The vaccination confidence scale: A brief measure of parents’ vaccination beliefs. Vaccine 2014, 32, 6259–6265. [Google Scholar] [CrossRef] [Green Version]
- Fisher, A.K.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef]
- Ekstrand, M.L.; Heylen, E.; Gandhi, M.; Steward, W.T.; Pereira, M.; Srinivasan, K. COVID-19 vaccine hesitancy among PLWH in South India: Implications for vaccination campaigns. JAIDS J. Acquir. Immune Defic. Syndr. 2021, 88, 421–425. [Google Scholar] [CrossRef]
- Liu, Y.; Han, J.; Li, X.; Chen, D.; Zhao, X.; Qiu, Y.; Zhang, L.; Xiao, J.; Li, B.; Zhao, H. Covid-19 vaccination in people living with HIV (Plwh) in China: A cross sectional study of vaccine hesitancy, safety, and immunogenicity. Vaccines 2021, 9, 1458. [Google Scholar] [CrossRef]
- Vallée, A.; Fourn, E.; Majerholc, C.; Touche, P.; Zucman, D. COVID-19 vaccine hesitancy among French people living with HIV. Vaccines 2021, 9, 302. [Google Scholar] [CrossRef]
- Hochstatter, K.R.; Akhtar, W.Z.; Dietz, S.; Pe-Romashko, K.; Gustafson, D.H.; Shah, D.V.; Krechel, S.; Liebert, C.; Miller, R.; El-Bassel, N.; et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: Experience from a Pilot mHealth Intervention. AIDS Behav. 2020, 25, 354–359. [Google Scholar] [CrossRef]
- Ssentongo, P.; Heilbrunn, E.S.; Ssentongo, A.E.; Advani, S.; Chinchilli, V.M.; Nunez, J.J.; Du, P. Epidemiology and outcomes of COVID-19 in HIV-infected individuals: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 6283. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. eClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- APM Research Lab. COVID-19 Deaths Analyzed by Race and Ethnicity. Available online: https://www.apmresearchlab.org/covid/deaths-by-race (accessed on 5 January 2022).
- Gross, C.P.; Essien, U.R.; Pasha, S.; Gross, J.R.; Wang, S.-Y.; Nunez-Smith, M. Racial and ethnic disparities in population-level COVID-19 mortality. J. Gen. Intern. Med. 2020, 35, 3097–3099. [Google Scholar] [CrossRef] [PubMed]
- Hooper, W.M.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and racial/ethnic disparities. JAMA 2020, 323, 2466–2467. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, T.; Moghtaderi, A.; Lueck, J.A.; Hotez, P.; Strych, U.; Dor, A.; Fowler, E.F.; Motta, M. Correlates and disparities of intention to vaccinate against COVID-19. Soc. Sci. Med. 2021, 272, 113638. [Google Scholar] [CrossRef] [PubMed]
- Ferdinand, C.K.; Nedunchezhian, S.; Reddy, T.K. The COVID-19 and Influenza “Twindemic”: Barriers to influenza vaccination and potential acceptance of SARS-CoV2 vaccination in African Americans. J. Natl. Med. Assoc. 2020, 112, 681–687. [Google Scholar] [CrossRef]
- Quinn, S.C.; Jamison, A.M.; Freimuth, V. Communicating effectively about emergency use authorization and vaccines in the COVID-19 pandemic. Am. J. Public Health 2021, 111, 355–358. [Google Scholar] [CrossRef]
- Shen, A.K.; Iv, R.H.; DeWald, E.; Rosenbaum, S.; Pisani, A.; Orenstein, W. Ensuring equitable access to COVID-19 vaccines in the US: Current System challenges and opportunities. Health Aff. 2021, 40, 62–69. [Google Scholar] [CrossRef]
- Webb, F.J.; Khubchandani, J.; Striley, C.W.; Cottler, L.B. Black-white differences in willingness to participate and perceptions about health research: Results from the population-based HealthStreet study. J. Immigr. Minor. Health 2018, 21, 299–305. [Google Scholar] [CrossRef]
- Jaiswal, J.; Krause, K.D.; Martino, R.J.; D’Avanzo, P.A.; Griffin, M.; Stults, C.B.; Karr, A.G.; Halkitis, P.N. SARS-CoV-2 vaccination hesitancy and behaviors in a national sample of people living with HIV. AIDS Patient Care STDs 2021, 36, 34–44. [Google Scholar] [CrossRef]
- Baumgaertner, B.; Carlisle, J.E.; Justwan, F. The influence of political ideology and trust on willingness to vaccinate. PLoS ONE 2018, 13, e0191728. [Google Scholar] [CrossRef] [Green Version]
- Funk, C.; Kennedy, B.; Johnson, C. Trust in Medical Scientists Has Grown in Us, but Mainly among Democrats. Pew Research Center, 21 May 2020. [Google Scholar]
- Morisi, D.; Jost, J.T.; Singh, V. An asymmetrical “President-in-Power” effect. Am. Political Sci. Rev. 2018, 113, 614–620. [Google Scholar] [CrossRef]
- Van Bavel, J.J. In a Pandemic, Political Polarization Could Kill People. The Washington Post, 22 March 2020. [Google Scholar]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. COVID-19 Vaccines for Children and Teens. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/adolescents.html (accessed on 27 June 2021).
- Wilson, S.L.; Wiysonge, C. Social media and vaccine hesitancy. BMJ Glob. Health 2020, 5, e004206. [Google Scholar] [CrossRef]
- Trethewey, S.P. Strategies to combat medical misinformation on social media. Postgrad. Med. J. 2019, 96, 4–6. [Google Scholar] [CrossRef] [Green Version]
- Ruprecht, M.M.; Wang, X.; Johnson, A.K.; Xu, J.; Felt, D.; Ihenacho, S.; Stonehouse, P.; Curry, C.W.; DeBroux, C.; Costa, D.; et al. Evidence of social and structural COVID-19 disparities by sexual orientation, gender identity, and race/ethnicity in an urban environment. J. Urban Health 2021, 98, 27–40. [Google Scholar] [CrossRef]
- Rief, W. Fear of adverse effects and COVID-19 vaccine hesitancy: Recommendations of the treatment expectation expert group. JAMA Health Forum 2021, 2, e210804. [Google Scholar] [CrossRef]
| Variables | Entire Sample (N = 1030) | |
|---|---|---|
| Frequency | % | |
| Sociodemographic | ||
| Male sex | 924 | 89.7 |
| Race: Black | 116 | 11.3 |
| Race: White | 680 | 66.0 |
| Age (years) | 53.0 (60.0 − 41.0) | |
| Education: bachelor’s degree or higher | 507 | 49.2 |
| Annual income: ≤$19,999 | 252 | 24.5 |
| Sexual orientation: gay | 870 | 84.5 |
| Relationship status: single | 552 | 53.6 |
| Political orientation | ||
| Conservative | 72 | 7.0 |
| Liberal | 679 | 65.9 |
| HIV & health-related attributes | ||
| Has undetectable HIV viral load | 984 | 95.5 |
| CD4 count: >200 cells/mm3 | 804 | 78.1 |
| Time living with HIV (years) | 16.0 (26.0 − 7.0) | |
| Received an annual vaccine for influenza | 867 | 84.2 |
| Alcohol use disorder | 303 | 29.4 |
| Active drug use | 45 | 4.4 |
| COVID-19 history and experiences | ||
| Ever been tested for COVID-19 | 675 | 65.5 |
| Ever tested positive for COVID-19 | 81 | 7.9 |
| Family member tested positive for COVID-19 | 141 | 13.7 |
| Family member died from COVID-19 | 216 | 21.0 |
| COVID-19 vaccine-related concerns | ||
| “I am worried about side effects from the vaccine” | 405 | 39.3 |
| “I am concerned the vaccine will not be safe” | 151 | 14.7 |
| “I don’t trust government to distribute vaccine fairly” | 140 | 13.6 |
| “I don’t want to be experimented on” | 96 | 9.3 |
| “I don’t think the vaccine will be effective” | 55 | 5.3 |
| “I am against vaccines in general” | 8 | 0.8 |
| “I don’t trust medical doctors” | 7 | 0.7 |
| Variables | Univariate | Multivariable | ||||
|---|---|---|---|---|---|---|
| Beta | S.E. | p | Beta | S.E. | p | |
| Sociodemographic | ||||||
| Male sex | −0.320 | 0.057 | <0.001 | −0.121 | 0.063 | 0.053 |
| Race: Black | 0.443 | 0.054 | <0.001 | 0.149 | 0.052 | 0.005 |
| Race: White | −0.300 | 0.036 | <0.001 | −0.093 | 0.035 | 0.008 |
| Age (years) | −0.006 | 0.001 | <0.001 | −0.000 | 0.002 | 0.922 |
| Education: bachelor’s degree or higher | −0.246 | 0.034 | <0.001 | −0.093 | 0.031 | 0.002 |
| Annual income: ≤$19,999 | 0.214 | 0.040 | <0.001 | −0.001 | 0.031 | 0.977 |
| Sexual orientation: gay | −0.267 | 0.048 | <0.001 | 0.005 | 0.053 | 0.919 |
| Relationship status: single | 0.140 | 0.035 | <0.001 | 0.070 | 0.029 | 0.018 |
| Political orientation | ||||||
| Conservative | 0.393 | 0.068 | <0.001 | 0.157 | 0.061 | 0.010 |
| Liberal | −0.325 | 0.036 | <0.001 | -0.131 | 0.033 | <0.001 |
| HIV & health-related attributes | ||||||
| Has undetectable HIV viral load | −0.241 | 0.085 | 0.004 | −0.086 | 0.073 | 0.240 |
| CD4 count: >200 cells/mm3 | −0.190 | 0.052 | <0.001 | −0.082 | 0.041 | 0.048 |
| Time living with HIV (years) | −0.004 | 0.002 | 0.004 | −0.001 | 0.002 | 0.388 |
| Received an annual vaccine for influenza | 0.003 | 0.004 | 0.395 | |||
| Alcohol use disorder | 0.015 | 0.038 | 0.693 | |||
| Active drug use | 0.071 | 0.086 | 0.406 | |||
| COVID-19 history and experiences | ||||||
| Ever been tested for COVID-19 | −0.033 | 0.037 | 0.376 | |||
| Ever tested positive for COVID-19 | 0.080 | 0.065 | 0.221 | |||
| Family member tested positive for COVID-19 | 0.099 | 0.051 | 0.052 | |||
| Family member died from COVID-19 | 0.054 | 0.043 | 0.213 | |||
| COVID-19 vaccine-related concerns | ||||||
| “I am worried about side effects from the vaccine” | 0.446 | 0.033 | <0.001 | 0.226 | 0.032 | <0.001 |
| “I am concerned the vaccine will not be safe” | 0.594 | 0.046 | <0.001 | 0.260 | 0.045 | <0.001 |
| “I don’t trust government to distribute vaccine fairly” | 0.315 | 0.050 | <0.001 | 0.065 | 0.042 | 0.127 |
| “I don’t want to be experimented on” | 0.724 | 0.056 | <0.001 | 0.287 | 0.055 | <0.001 |
| “I don’t think the vaccine will be effective” | 0.524 | 0.076 | <0.001 | 0.169 | 0.063 | 0.008 |
| “I am against vaccines in general” | 2.291 | 0.186 | <0.001 | 1.791 | 0.183 | <0.001 |
| “I don’t trust medical doctors” | 1.161 | 0.210 | <0.001 | 0.038 | 0.184 | 0.838 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shrestha, R.; Meyer, J.P.; Shenoi, S.; Khati, A.; Altice, F.L.; Mistler, C.; Aoun-Barakat, L.; Virata, M.; Olivares, M.; Wickersham, J.A. COVID-19 Vaccine Hesitancy and Associated Factors among People with HIV in the United States: Findings from a National Survey. Vaccines 2022, 10, 424. https://doi.org/10.3390/vaccines10030424
Shrestha R, Meyer JP, Shenoi S, Khati A, Altice FL, Mistler C, Aoun-Barakat L, Virata M, Olivares M, Wickersham JA. COVID-19 Vaccine Hesitancy and Associated Factors among People with HIV in the United States: Findings from a National Survey. Vaccines. 2022; 10(3):424. https://doi.org/10.3390/vaccines10030424
Chicago/Turabian StyleShrestha, Roman, Jaimie P. Meyer, Sheela Shenoi, Antoine Khati, Frederick L. Altice, Colleen Mistler, Lydia Aoun-Barakat, Michael Virata, Miriam Olivares, and Jeffrey A. Wickersham. 2022. "COVID-19 Vaccine Hesitancy and Associated Factors among People with HIV in the United States: Findings from a National Survey" Vaccines 10, no. 3: 424. https://doi.org/10.3390/vaccines10030424
APA StyleShrestha, R., Meyer, J. P., Shenoi, S., Khati, A., Altice, F. L., Mistler, C., Aoun-Barakat, L., Virata, M., Olivares, M., & Wickersham, J. A. (2022). COVID-19 Vaccine Hesitancy and Associated Factors among People with HIV in the United States: Findings from a National Survey. Vaccines, 10(3), 424. https://doi.org/10.3390/vaccines10030424








