Approach of Pregnant Women from Poland and the Ukraine to COVID-19 Vaccination—The Role of Medical Consultation
Abstract
:1. Introduction
Objectives
2. Methodology
2.1. Material and Methods
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Statistical Analysis
3. Results
3.1. Overall Group
3.2. General Characteristics
3.3. Comparison of Selected Indices and Answers for Questions in the Questionnaire According to the Agreement for Inoculation before and after Consultation with a Gynaecologist
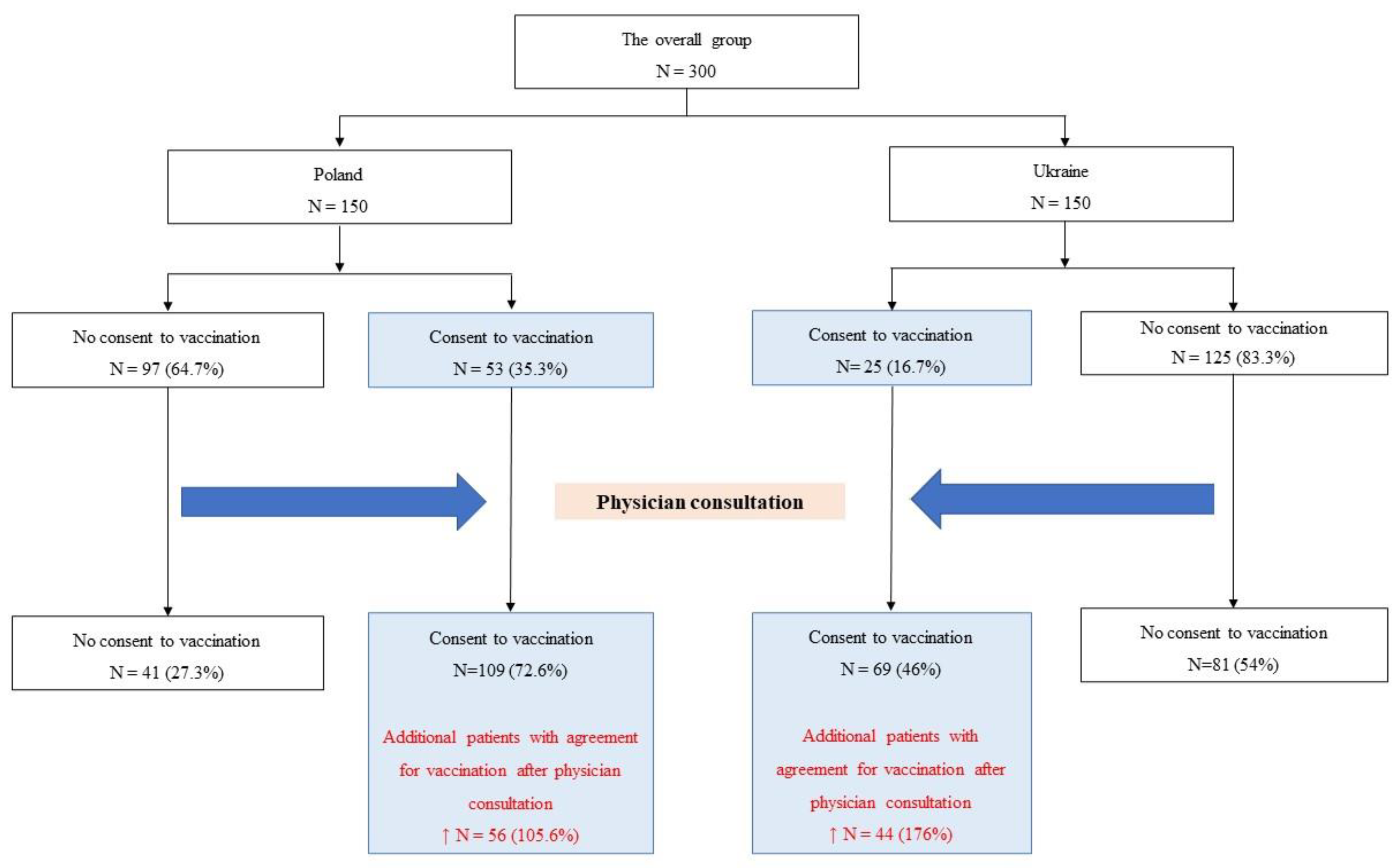
3.4. Relationship between Consultation and Approach to Inoculation against COVID-19
3.5. Predictors of Vaccination against COVID-19–Univariate Analysis
3.6. Predictors of Vaccination against COVID-19–Multivariate Analysis
3.7. Significance of Gynaecological Consultation on Increase in Vaccination Percentage
4. Discussion
4.1. Acceptance of Vaccination—Geographic, Socioeconomic and Medical Aspects
4.2. Modifiable Factors of Vaccination Acceptance
4.3. Gynaecological Counselling
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 vaccine acceptance among pregnant women and mothers of young children: Results of a survey in 16 countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef]
- COVID-19 to Add as Many as 150 Million Extreme Poor by 2021. World Bank. Available online: https://www.worldbank.org/en/news/press-release/2020/10/07/COVID-19-to-add-as-many-as-150-million-extreme-poor-by-2021 (accessed on 8 June 2021).
- The Lancet Infectious Diseases. The intersection of COVID-19 and mental health. Lancet Infect. Dis. 2020, 20, 1217. [CrossRef]
- Gómez-Ochoa, S.A.; Franco, O.H.; Rojas, L.Z.; Raguindin, P.F.; Roa-Díaz, Z.M.; Wyssmann, B.M.; Guevara, S.L.R.; Echeverría, L.E.; Glisic, M.; Muka, T. COVID-19 in Health-Care Workers: A Living Systematic Review and Meta-Analysis of Prevalence, Risk Factors, Clinical Characteristics, and Outcomes. Am. J. Epidemiol. 2021, 190, 161–175. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Ahmed Khan, F.; Napolean Shanmugam, G.N.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Erquicia, J.; Valls, L.; Barja, A.; Gil, S.; Miquel, J.; Leal-Blanquet, J.; Schmidt, C.; Checa, J.; Vega, D. Emotional impact of the COVID-19 pandemic on healthcare workers in one of the most important infection outbreaks in Europe. Med. Clínica Engl. Ed. 2020, 155, 434–440. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob. Health 2020, 5, e003097. [Google Scholar] [CrossRef] [PubMed]
- Ellington, S.; Strid, P.; Tong, V.T.; Woodworth, K.; Galang, R.R.; Zambrano, L.D.; Nahabedian, J.; Anderson, K.; Gilboa, S.M. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, January 22–June 7, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 769–775. [Google Scholar] [CrossRef]
- Collin, J.; Byström, E.; Carnahan, A.; Ahrne, M. Public Health Agency of Sweden’s Brief Report: Pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in Sweden. Acta Obstet. Gynecol. Scand. 2020, 99, 819–822. [Google Scholar] [CrossRef]
- Delahoy, M.J.; Whitaker, M.; O’Halloran, A.; Chai, S.J.; Kirley, P.D.; Alden, N.; Kawasaki, B.; Meek, J.; Yousey-Hindes, K.; Anderson, E.J.; et al. Characteristics and Maternal and Birth Outcomes of Hospitalized Pregnant Women with Laboratory-Confirmed COVID-19—COVID-NET, 13 States, March 1–August 22, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakopoulos, L.; Myers, T.R.; Gee, J.; Lipkind, H.S.; Kharbanda, E.O.; Ryan, D.S.; Williams, J.T.; Naleway, A.L.; Klein, N.P.; Hambidge, S.J.; et al. SARS-CoV-2 Infection Among Hospitalized Pregnant Women: Reasons for Admission and Pregnancy Characteristics—Eight U.S. Health Care Centers, March 1–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1355–1359. [Google Scholar] [CrossRef]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F.; Azziz-Baumgartner, E.; Gilboa, S.M.; et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, January 22–October 3, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef] [PubMed]
- Khoury, R.; Bernstein, P.S.; Debolt, C.; Stone, J.; Sutton, D.M.; Simpson, L.L.; Limaye, M.A.; Roman, A.S.; Fazzari, M.; Penfield, C.A.; et al. Characteristics and Outcomes of 241 Births to Women With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection at Five New York City Medical Centers. Obstet. Gynecol. 2020, 136, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Ferraiolo, A.; Barra, F.; Kratochwila, C.; Paudice, M.; Vellone, V.G.; Godano, E.; Varesano, S.; Noberasco, G.; Ferrero, S.; Arioni, C. Report of Positive Placental Swabs for SARS-CoV-2 in an Asymptomatic Pregnant Woman with COVID-19. Medicina 2020, 56, 306. [Google Scholar] [CrossRef]
- Popescu, D.; Cioca, A.; Muresan, C.; Navolan, D.; Gui, A.; Pop, O.; Marcovici, T.; Ilie, C.; Craina, M.; Boia, M. A Case of COVID-19 Pregnancy Complicated with Hydrops Fetalis and Intrauterine Death. Medicina 2021, 57, 667. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.S.; Mytton, O.T.; Mullins, E.W.S.; Fowler, T.A.; Falconer, C.L.; Murphy, O.B.; Langenberg, C.; Jayatunga, W.J.P.; Eddy, D.H.; Nguyen-Van-Tam, J.S. SARS-CoV-2 (COVID-19): What Do We Know About Children? A Systematic Review. Clin. Infect. Dis. 2020, 71, 2469–2479. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F. Children are unlikely to be the main drivers of the COVID-19 pandemic—A systematic review. Acta Paediatr. 2020, 109, 1525–1530. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Roma, P.; Da Molin, G.; Diella, G.; Montagna, M.T.; Ferracuti, S.; Liguori, G.; Orsi, G.B.; Napoli, C. Acceptance of COVID-19 Vaccination in the Elderly: A Cross-Sectional Study in Southern Italy. Vaccines 2021, 9, 1222. [Google Scholar] [CrossRef] [PubMed]
- Principi, N.; Esposito, S. Is the Immunization of Pregnant Women against COVID-19 Justified? Vaccines 2021, 9, 970. [Google Scholar] [CrossRef]
- Riley, L.E.; Jamieson, D.J. Inclusion of Pregnant and Lactating Persons in COVID-19 Vaccination Efforts. Ann. Intern. Med. 2021, 174, 701–702. [Google Scholar] [CrossRef]
- Theile, R.N.; Wick, M.; Mehta, R.; Weaver, A.L.; Virk, A.; Swift, M. Pregnancy and birth outcomes after SARS-CoV-2 vaccination in pregnancy. Am. J. Obstet. Gynecol. MFM 2021, 3, 100467. [Google Scholar] [CrossRef]
- Mortazavi, F.; Mehrabadi, M.; KiaeeTabar, R. Pregnant women’s well-being and worry during the COVID-19 pandemic: A cross-sectional study. BMC Pregnancy Childbirth 2021, 21, 59. [Google Scholar] [CrossRef]
- Rosso, A.; Massimi, A.; Pitini, E.; Nardi, A.; Baccolini, V.; Marzuillo, C.; De Vito, C.; Villari, P. Factors affecting the vaccination choices of pregnant women for their children: A systematic review of the literature. Hum. Vaccines Immunother. 2020, 16, 1969–1980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danchin, M.H.; Costa-Pinto, J.; Attwell, K.L.; Willaby, H.; Wiley, K.; Hoq, M.; Leask, J.; Perrett, K.; O’Keefe, J.; Giles, M.; et al. Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine 2018, 36, 6473–6479.17. [Google Scholar] [CrossRef] [PubMed]
- Bloom, B.R.; Nowak, G.J.; Orenstein, W. When Will We Have a Vaccine?—Understanding Questions and Answers about COVID-19 Vaccination. N. Engl. J. Med. 2020, 383, 2202–2204. [Google Scholar] [CrossRef] [PubMed]
- Ten Health Issues WHO Will Tackle This Year. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 9 June 2021).
- OSF Preprints | The COVID States Project #9: Will Americans Vaccinate Themselves and Their Children against COVID-19. Available online: https://osf.io/wzgck (accessed on 9 June 2021).
- Stanowisko PTGiP Dotyczące Szczepień Kobiet Ciężarnych Przeciwko COVID19. | PTGiP. Available online: https://www.ptgin.pl/stanowisko-ptgip-dotyczace-szczepien-kobiet-ciezarnych-przeciwko-covid19 (accessed on 20 June 2021).
- Geoghegan, S.; Stephens, L.C.; Feemster, K.A.; Drew, R.J.; Eogan, M.; Butler, K.M. “This choice does not just affect me.” Attitudes of pregnant women toward COVID-19 vaccines: A mixed-methods study. Hum. Vaccines Immunother. 2021, 17, 3371–3376. [Google Scholar] [CrossRef] [PubMed]
- Mohan, S.; Reagu, S.; Lindow, S.; Alabdulla, M. COVID-19 vaccine hesitancy in perinatal women: A cross sectional survey. J. Perinat. Med. 2021, 49, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Mappa, I.; Luviso, M.; Distefano, F.A.; Carbone, L.; Maruotti, G.M.; Rizzo, G. Women perception of SARS-CoV-2 vaccination during pregnancy and subsequent maternal anxiety: A prospective observational study. J. Matern. Fetal Neonatal Med. 2021, 3, 100352. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.P.; Wong, P.F.; AbuBakar, S. Vaccine hesitancy and the resurgence of vaccine preventable diseases: The way forward for Malaysia, a Southeast Asian country. Hum. Vaccines Immunother. 2020, 16, 1511–1520. [Google Scholar] [CrossRef]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 153–155. [Google Scholar] [CrossRef] [Green Version]
- Gencer, H.; Özkan, S.; Vardar, O.; Serçekuş, P. The effects of the COVID 19 pandemic on vaccine decisions in pregnant women. Women Birth 2021. In Press. [Google Scholar] [CrossRef]
- Babicki, M.; Mastalerz-Migas, A. Attitudes toward Vaccination against COVID-19 in Poland. A Longitudinal Study Performed before and Two Months afterV-2 Vaccine Willingness among Pregnant and Breastfeeding Women during the First Pandemic Wave: A Cross-Sectional Study in Switzerland. Vaccines 2021, 9, 503. [Google Scholar] [CrossRef] [PubMed]
- Sowa, P.; Kiszkiel, Ł.; Laskowski, P.P.; Alimowski, M.; Szczerbiński, Ł.; Paniczko, M.; Moniuszko-Malinowska, A.; Kamiński, K. COVID-19 Vaccine Hesitancy in Poland—Multifactorial Impact Trajectories. Vaccines 2021, 9, 876. [Google Scholar] [CrossRef] [PubMed]
- Holt, E. COVID-19 vaccination in Ukraine. Lancet Infect. Dis. 2021, 21, 462. [Google Scholar] [CrossRef]
- Matiashova, L.; Isayeva, G.; Shanker, A.; Tsagkaris, C.; Aborode, A.T.; Essar, M.Y.; Ahmad, S. COVID-19 vaccination in Ukraine: An update on the status of vaccination and the challenges at hand. J. Med. Virol. 2021, 93, 5252–5253. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.; Wang, R.; Han, N.; Liu, J.; Yuan, C.; Deng, L.; Han, C.; Sun, F.; Liu, M.; Liu, J.; et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: A multi-center cross-sectional study based on health belief mode. Hum. Vaccin Immunother. 2021, 17, 2378–2388. [Google Scholar] [CrossRef] [PubMed]
- Levy, A.T.; Singh, S.; Riley, L.E.; Prabhu, M. Acceptance of COVID-19 vaccination in pregnancy: A survey study. Am. J. Obstet. Gynecol. 2021, 3, 100399. [Google Scholar] [CrossRef]
- Samannodi, M. COVID-19 Vaccine Acceptability Among Women Who are Pregnant or Planning for Pregnancy in Saudi Arabia: A Cross-Sectional Study. Patient Prefer. Adherence 2021, 15, 2609–2618. [Google Scholar] [CrossRef]
- Stuckelberger, S.; Favre, G.; Ceulemans, M.; Nordeng, H.; Gerbier, E.; Lambelet, V.; Stojanov, M.; Winterfeld, U.; Baud, D.; Panchaud, A.; et al. SARS-CoV-2 Vaccine Willingness among Pregnant and Breastfeeding Women during the First Pandemic Wave: A Cross-Sectional Study in Switzerland. Viruses 2021, 13, 1199. [Google Scholar] [CrossRef]
- Graham, B.S. Rapid COVID-19 vaccine development. Science 2020, 368, 945–946. [Google Scholar] [CrossRef]
- Baccolini, V.; Rosso, A.; Di Paolo, C.; Isonne, C.; Salerno, C.; Migliara, G.; Prencipe, G.P.; Massimi, A.; Marzuillo, C.; De Vito, C.; et al. What is the Prevalence of Low Health Literacy in European Union Member States? A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 36, 753–761. [Google Scholar] [CrossRef]
- Ceulemans, M.; Foulon, V.; Panchaud, A.; Winterfeld, U.; Pomar, L.; Lambelet, V.; Cleary, B.; O’Shaughnessy, F.; Passier, A.; Richardson, J.; et al. Vaccine Willingness and Impact of the COVID-19 Pandemic on Women’s Perinatal Experiences and Practices—A Multinational, Cross-Sectional Study Covering the First Wave of the Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3367. [Google Scholar] [CrossRef] [PubMed]
- Januszek, S.M.; Faryniak-Zuzak, A.; Barnaś, E.; Łoziński, T.; Góra, T.; Siwiec, N.; Szczerba, P.; Januszek, R.; Kluz, T. The Approach of Pregnant Women to Vaccination Based on a COVID-19 Systematic Review. Medicina 2021, 57, 977. [Google Scholar] [CrossRef] [PubMed]
- Prematunge, C.; Corace, K.; McCarthy, A.; Nair, R.C.; Pugsley, R.; Garber, G. Factors influencing pandemic influenza vaccination of healthcare workers—A systematic review. Vaccine 2012, 30, 4733–4743. [Google Scholar] [CrossRef] [PubMed]
- Professionally Responsible Advocacy for Women and Children First during the COVID-19 Pandemic: Guidance from World Association of Perinatal Medicine and International Academy of Perinatal Medicine. Available online: https://www.degruyter.com/document/doi/10.1515/jpm-2020-0329/html (accessed on 11 July 2021).
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Cavaliere, A.F.; Zaami, S.; Pallottini, M.; Perelli, F.; Vidiri, A.; Marinelli, E.; Straface, G.; Signore, F.; Scambia, G.; Marchi, L. Flu and Tdap Maternal Immunization Hesitancy in Times of COVID-19: An Italian Survey on Multiethnic Sample. Vaccines 2021, 9, 1107. [Google Scholar] [CrossRef] [PubMed]
| Before Gynaecological Consultation Odds Ratio (95% Confidence Interval, p-Value) | After Gynaecological Consultation Odds Ratio (95% Confidence Interval, p-Value) | |
|---|---|---|
| Are you planning to vaccinate your children against COVID-19? (no vs. yes) | 0.277 (0.150–0.477, <0.001) | |
| Do you think the complications after receiving the COVID-19 vaccine are: (rare/very rare vs. common/very common) | 0.406 (0.242–0.642, <0.001) | |
| Have you been vaccinated against COVID-19?—Reason for negative approach: | ||
| Fear of damage to the foetus (yes vs. no) | 0.073 (0.023–0.197, <0.001) | 0.024 (0.009–0.057, <0.001) |
| Fear of post-vaccination complications/adverse reactions (yes vs. no) | 0.119 (0.039–0.324, <0.001) | 0.040 (0.009–0.057, <0.001) |
| I have not had such an opportunity yet due to the limitations in the vaccination programme (yes vs. no) | 0.026 (0.001–0.20, <0.001) | |
| Before Medical Visit | ||||
|---|---|---|---|---|
| Yes (1–6) | No (7) | Total | ||
| After medicalvisit | Yes (1–6) Count (%) | 58 (19.4) | 52 (17.4) | 110 (36.8) |
| No (7) Count (%) | 7 (2.34) | 182 (60.9) | 189 (63.2) | |
| Total (%) | 65 (21.7) | 234 (78.3) | 299 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Januszek, S.; Siwiec, N.; Januszek, R.; Kluz, M.; Lebed, R.; Toś, P.; Góra, T.; Plens, K.; Dąbrowski, K.; Sidorowicz, M.; et al. Approach of Pregnant Women from Poland and the Ukraine to COVID-19 Vaccination—The Role of Medical Consultation. Vaccines 2022, 10, 255. https://doi.org/10.3390/vaccines10020255
Januszek S, Siwiec N, Januszek R, Kluz M, Lebed R, Toś P, Góra T, Plens K, Dąbrowski K, Sidorowicz M, et al. Approach of Pregnant Women from Poland and the Ukraine to COVID-19 Vaccination—The Role of Medical Consultation. Vaccines. 2022; 10(2):255. https://doi.org/10.3390/vaccines10020255
Chicago/Turabian StyleJanuszek, Sławomir, Natalia Siwiec, Rafał Januszek, Marta Kluz, Roman Lebed, Paweł Toś, Tomasz Góra, Krzysztof Plens, Krzysztof Dąbrowski, Marcin Sidorowicz, and et al. 2022. "Approach of Pregnant Women from Poland and the Ukraine to COVID-19 Vaccination—The Role of Medical Consultation" Vaccines 10, no. 2: 255. https://doi.org/10.3390/vaccines10020255
APA StyleJanuszek, S., Siwiec, N., Januszek, R., Kluz, M., Lebed, R., Toś, P., Góra, T., Plens, K., Dąbrowski, K., Sidorowicz, M., Szcześniewska, A., Barnaś, E., Kalandyk-Osinko, K., Darmochwal-Kolarz, D., & Kluz, T. (2022). Approach of Pregnant Women from Poland and the Ukraine to COVID-19 Vaccination—The Role of Medical Consultation. Vaccines, 10(2), 255. https://doi.org/10.3390/vaccines10020255







