Leishmaniac Quest for Developing a Novel Vaccine Platform. Is a Roadmap for Its Advances Provided by the Mad Dash to Produce Vaccines for COVID-19?
Abstract
| Table of Content | ||||
| Page | ||||
| 1. Introduction | 3 | |||
| 2. Information/database search | 3–4 | |||
| 3. Results (SARS-CoV-2/COVID-19 versus Leishmania/leishmaniasis) | ||||
| 3.1. Causative agents | ||||
| 3.1.1. Molecular genetics | 4 | |||
| 3.1.2. Primary and secondary infection of host cell | 5–6 | |||
| 3.1.3. Species and variants | 6–7 | |||
| 3.2. Signs, symptoms and sequelae of the disease | ||||
| 3.2.1. The major clinical symptoms | 7 | |||
| 3.2.2. Associated clinical consequences | 7–8 | |||
| 3.3. Epidemiology | ||||
| 3.3.1. Transmission | 8 | |||
| 3.3.2. Distribution | 8–9 | |||
| 3.3.3. Incidence | 9 | |||
| 3.3.4. Risk factors | 9 | |||
| 3.4. Surveillance, treatment and control | ||||
| 3.4.1. Diagnosis | 9–10 | |||
| 3.4.2. Clinical managements | ||||
| A. Chemotherapy | 10 | |||
| B. Alternative therapy | 10 | |||
| C. Immunotherapy | 10–11 | |||
| 3.4.3. Preventive measures | 11 | |||
| 3.4.4. Control programs | 11–12 | |||
| 3.5. Vaccine | ||||
| 3.5.1. Development, production and application | ||||
| A1-A6 vaccine platforms for COVID-19 | 12–14 | |||
| B1-B4 vaccine platforms for human leishmaniasis | 13–15 | |||
| 3.5.2. Clinical trials | 15 | |||
| 3.5.3. Human challenge trials | 15–16 | |||
| 3.5.4. Vaccine rollout | 16 | |||
| 3.5.5. Socio-economic impacts on vaccination rate & herd immunity | 16 | |||
| 3.5.6. Human immune response to vaccination | 17 | |||
| 3.5.7. Rare, but serious side-effect of live adenovirus vaccines? | 17 | |||
| 3.6. Leishmania platform for safe and effective delivery of vaccines | ||||
| 3.6.1. Leishmania as an effective vaccine platform | 17–18 | |||
| 3.6.2. Leishmania as a safe vaccine platform by installation of a dual | ||||
| suicidal mechanism for singlet oxygen-initiated inactivation | 18–20 | |||
| 3.6.3. Leishmania delivery of vaccines for T-cell immunity against | ||||
| infectious & malignant diseases | 20–22 | |||
| 4. Discussion | ||||
| 4.1. Prospect of disease control from the perspective of COVID-19 pandemic | 22–23 | |||
| 4.2. The success of anti-Covid vaccines stimulates new approaches | 23 | |||
| 4.3. Leishmania vs adenovirus as a vaccine platform | 23 | |||
| 4.4. Leishmania delivery of vaccines against multiple diseases | 24 | |||
| 4.5. Leishmania platform for anti-Covid vaccines | 24 | |||
| 4.6. Assessing human immune response to pathogens/vaccines | 25–26 | |||
| 5. Conclusion | 26 | |||
| 6. References | 27–30 | |||
1. Introduction
2. Information/Database Search
3. Results (SARS-CoV-2/COVID-19 vs. Leishmania/Leishmaniasis)
3.1. Causative Agents
3.1.1. Molecular Genetics
3.1.2. Primary and Secondary Infection of Host Cells
3.1.3. Species and Variants
3.2. Signs, Symptoms, and Sequelae of the Disease
3.2.1. The Major Clinical Symptoms
3.2.2. Associated Clinical Consequences
3.3. Epidemiology
3.3.1. Transmission
3.3.2. Distribution
3.3.3. Incidence
3.3.4. Risk Factors
3.4. Surveillance, Treatment, and Control
3.4.1. Diagnosis
3.4.2. Clinical Managements
A. Chemotherapy
B. Alternative Therapy
C. Immunotherapy
3.4.3. Preventive Measures
3.4.4. Control Programs
3.5. Vaccine
3.5.1. Development, Production, and Application
3.5.2. Clinical Trials
3.5.3. Human Challenge Trials
3.5.4. Vaccine Rollout
3.5.5. Socio-Economic Impacts on Vaccination Rate and Herd Immunity
3.5.6. Human Immune Response to Vaccination
3.5.7. Rare but Serious Side-Effect of Live Adenovirus Vaccines?
3.6. Leishmania Platform for Safe and Effective Delivery of Vaccines
3.6.1. Leishmania as an Effective Vaccine Platform
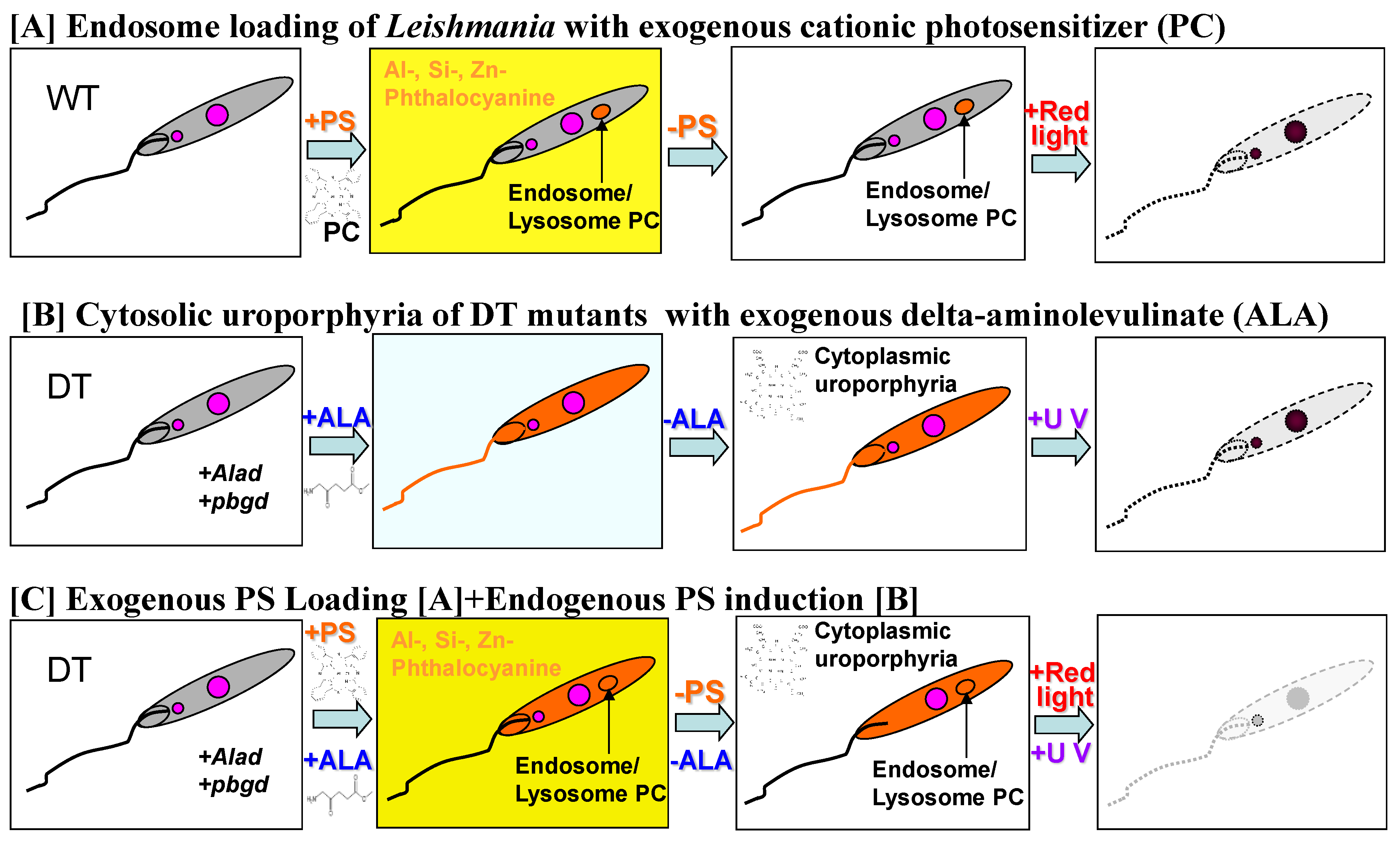
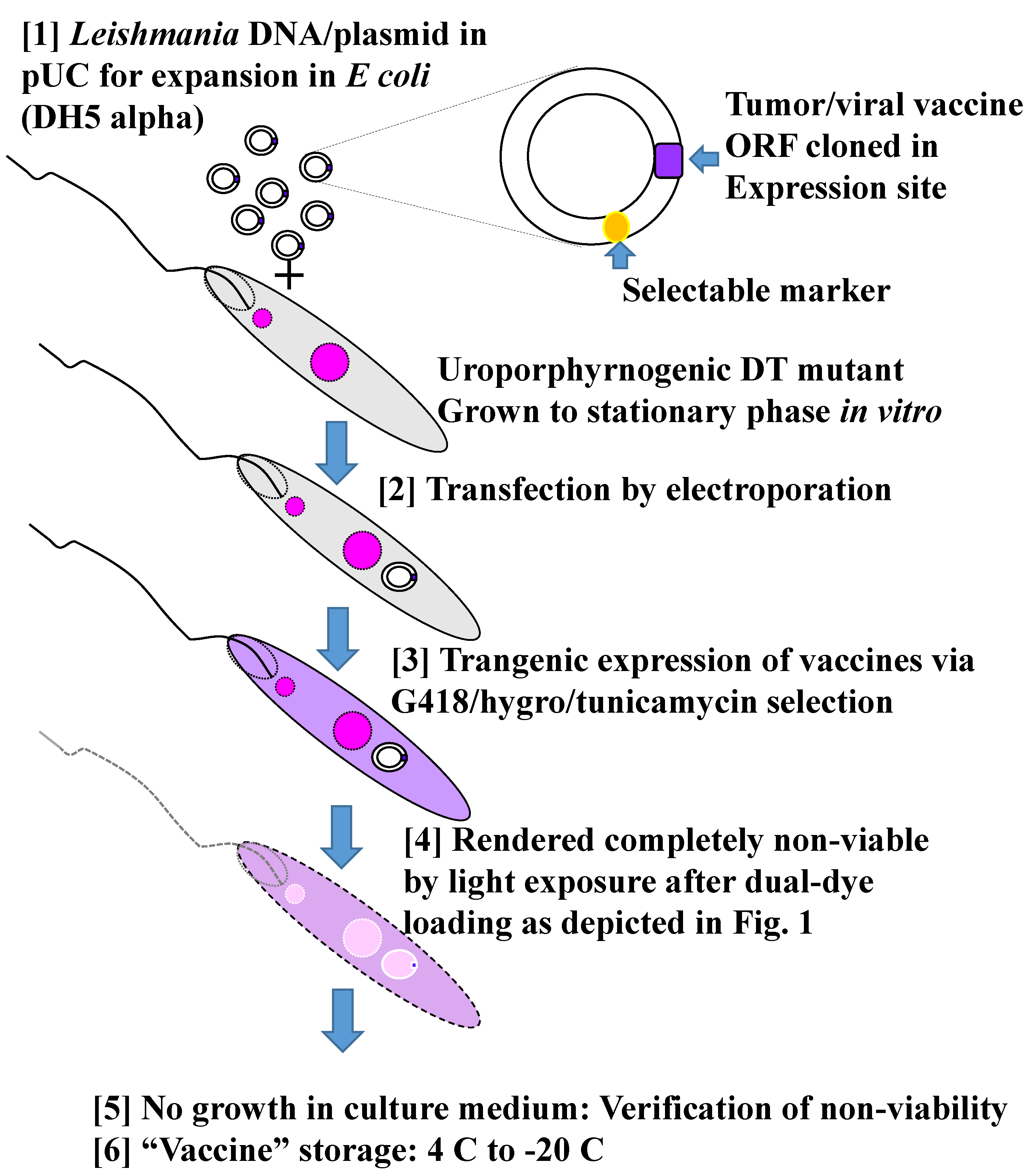
3.6.2. Leishmania are Made Safe as a Vaccine Platform by Installation of a Dual Suicidal Mechanism for Singlet Oxygen-Initiated Inactivation
3.6.3. Safe and Effective Delivery of Vaccines by 1O2-Inactivated Leishmania for T-Cell Mediated Immunity Against Infectious and Malignant Diseases
4. Discussion
4.1. Prospect of Disease Control from the Perspective of COVID-19 Pandemic by Vaccination and Beyond
4.2. The Success of Anti-Covid Vaccines Provides Impetus to the Development of New Approaches in Vaccinology
4.3. The Successful Deployment of Adenoviruses as a Platform for Anti-Covid Vaccines Makes the Use of Leishmania for Vaccine Delivery all the More Conceivable
4.4. The 1O2-Inactivated Leishmania are Potentially Deployable as a Platform to Deliver Multiple Vaccines from a Single or Multiple Pathogens Simultaneously Against Different Diseases
4.5. Complementary to the Current Mono-Specific Anti-Covid Vaccines Is Perhaps the Use of Leishmania Transfectants Expressing Spike Protein Together with One or More Additional SARS-CoV-2 Antigens
4.6. COVID-19 Pandemic Has Brought Several Important Areas of Vaccine-Related Research into Focus for Attention
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, K.P. Overview of Leishmaniasis with Special Emphasis on Kala-Azar in South Asia. In Neglected Tropical Diseases; Sunit, K., Ed.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 1–63. [Google Scholar]
- Chang, K.P. Leishmaniases. In Encyclopedia of Life Sciences, Item 1954 4rd ed.; Wiley & Son: Hoboken, NJ, USA, 2021. [Google Scholar]
- V’kovski, P.; Kratzel, A.; Steiner, S.; Stalder, H.; Thiel, V. Coronavirus Biology and Replication: Implications for SARS-CoV-2. Nat. Rev. Microbiol. 2021, 19, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Hartenian, E.; Nandakumar, D.; Lari, A.; Ly, M.; Tucker, J.M.; Glaunsinger, B.A. The molecular virology of coronaviruses. J. Biol. Chem. 2020, 295, 12910–12934. [Google Scholar] [CrossRef] [PubMed]
- Bar-On, Y.M.; Flamholz, A.; Phillips, R.; Milo, R. SARS-CoV-2 (COVID-19) by the numbers. Elife 2020, 9, e57309. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.J.; Lim, S.G.; Hong, W. Regulation of cell death during infection by the severe acute respiratory syndrome coronavirus and other coronaviruses. Cell Microbiol. 2007, 9, 2552–2561. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.P.; Chaudhuri, G.; Fong, D. Molecular determinants of Leishmania virulence. Annu. Rev. Microbiol. 1990, 44, 499–529. [Google Scholar] [CrossRef]
- Verma, J.K.; Rastogi, A.; Mukhopadhyay, A. Leishmania donovani resides in modified early endosomes by upregulating Rab5a expression via the downregulation of miR-494. PLoS Pathog. 2017, 13, e1006459. [Google Scholar] [CrossRef]
- Payne, S. Family Coronaviridae. In Viruses; Academic Press: New York, NY, USA, 2017; pp. 149–158. [Google Scholar] [CrossRef]
- Aucott, J.N.; Rebman, A.W. Long-haul COVID: Heed the lessons from other infection-triggered illnesses. Lancet 2021, 397, 967–968. [Google Scholar] [CrossRef]
- Abrams, J.Y.; Oster, M.E.; Godfred-Cato, S.E.; Bryant, B.; Datta, S.D.; Campbell, A.P.; Leung, J.W.; Tsang, C.A.; Pierce, T.J.; Kennedy, J.L. Factors linked to severe outcomes in multisystem inflammatory syndrome in children (MIS-C) in the USA: A retrospective surveillance study. Lancet Child Adolesc. Health. 2021, 5, 323–331. [Google Scholar] [CrossRef]
- Consiglio, C.R.; Cotugno, N.; Sardh, F.; Pou, C.; Amodio, D.; Rodriguez, L.; Tan, Z.; Zicari, S.; Ruggiero, A.; Pascucci, G.R.; et al. The Immunology of Multisystem Inflammatory Syndrome in Children with COVID-19. Cell 2020, 183, 968–981.e7. [Google Scholar] [CrossRef]
- Ramaswamy, A.; Brodsky, N.N.; Sumida, T.S.; Comi, M.; Asashima, H.; Hoehn, K.B.; Li, N.; Liu, Y.; Shah, A.; Ravindra, N.G. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity 2021, 54, 1083–1095. [Google Scholar] [CrossRef]
- García-Fernández, L.; Romero-Ferreiro, V.; Padilla, S.; López-Roldán, P.D.; Monzó-García, M.; Rodriguez-Jimenez, R. The impact on mental health patients of COVID-19 outbreak in Spain. J. Psychiatr. Res. 2021, 136, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Yanik, M.; Gurel, M.S.; Simsek, Z.; Kati, M. The psychological impact of cutaneous leishmaniasis. Clin. Exp. Dermatol. 2004, 29, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Wu, C.; Li, X.; Song, Y.; Yao, X.; Wu, X.; Duan, Y.; Zhang, H.; Wang, Y.; Qian, Z. On the origin and continuing evolution of SARS-CoV-2. Natl. Sci. Rev. 2020, 7, 1012–1023. [Google Scholar] [CrossRef] [PubMed]
- Peacock, T.P.; Penrice-Randal, R.; Hiscox, J.A.; Barclay, W.S. SARS-CoV-2 one year on: Evidence for ongoing viral adaptation. J. Gen. Virol. 2021, 102, 001584. [Google Scholar] [CrossRef] [PubMed]
- Temmam, S.; Vongphayloth, K.; Salazar, E.B.; Munier, S.; Bonomi, M.; Régnault, B.; Douangboubpha, B.; Karam, Y.; Chretien, D.; Sanamxay, D.; et al. Coronaviruses with a SARS-CoV-2-Like Receptor-Binding Domain Allowing ACE2-Mediated Entry into Human Cells Isolated from Bats of Indochinese Peninsula. Johns Hopkins University School of Public Health Research Square. 2021, pp. 1–24. Available online: https://www.researchsquare.com/article/rs-871965/v1 (accessed on 17 September 2021). [CrossRef]
- Mallapaty, S. The search for animals harbouring coronavirus—and why it matters. Nature 2021, 591, 26–28. [Google Scholar] [CrossRef]
- Fenollar, F.; Mediannikov, O.; Maurin, M.; Devaux, C.; Colson, P.; Levasseur, A.; Fournier, P.E.; Raoult, D. Mink, SARS-CoV-2, and the Human-Animal Interface. Front Microbiol. 2021, 12, 663815. [Google Scholar] [CrossRef]
- Wolff, D.; Nee, S.; Hickey, N.S.; Marschollek, M. Risk factors for Covid-19 severity and fatality: A structured literature review. Infection 2021, 49, 15–28. [Google Scholar] [CrossRef]
- Dolgin, E. The race for antiviral drugs to beat COVID—and the next pandemic. Nature 2021, 592, 340–343. [Google Scholar] [CrossRef]
- Drayman, N.; DeMarco, J.K.; Jones, K.A.; Azizi, S.A.; Froggatt, H.M.; Tan, K.; Maltseva, N.I.; Chen, S.; Nicolaescu, V.; Dvorkin, S.; et al. Masitinib is a broad coronavirus 3CL inhibitor that blocks replication of SARS-CoV-2. Science 2021, 373, 931–936. [Google Scholar] [CrossRef]
- Zhao, J.; Guo, S.; Yi, D.; Li, Q.; Ma, L.; Zhang, Y.; Wang, J.; Li, X.; Guo, F.; Lin, R.; et al. A cell-based assay to discover inhibitors of SARS-CoV-2 RNA dependent RNA polymerase. Antiviral Res. 2021, 190, 105078. [Google Scholar] [CrossRef]
- Si, L.; Bai, H.; Rodas, M.; Cao, W.; Oh, C.Y.; Jiang, A.; Moller, R.; Hoagland, D.; Oishi, K.; Horiuchi, S.; et al. A human-airway-on-a-chip for the rapid identification of candidate antiviral therapeutics and prophylactics. Nat. Biomed Eng. 2021, 5, 815–829. [Google Scholar] [CrossRef]
- Casadevall, A.; Pirofski, L.A. The convalescent sera option for containing COVID-19. J. Clin. Investig. 2020, 130, 1545–1548. [Google Scholar] [CrossRef]
- Lee, W.T.; Girardin, R.C.; Dupuis, A.P.; Kulas, K.E.; Payne, A.F.; Wong, S.J.; Arinsburg, S.; Nguyen, F.T.; Mendu, D.R.; Firpo-Betancourt, A. Neutralizing Antibody Responses in COVID-19 Convalescent Sera. J. Infect. Dis. 2021, 223, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Tregoning, J.S.; Brown, E.S.; Cheeseman, H.M.; Flight, K.E.; Higham, S.L.; Lemm, N.M.; Pierce, B.F.; Stirling, D.C.; Wang, Z.; Pollock, K.M. Vaccines for COVID-19. Clin. Exp. Immunol. 2020, 202, 162–192. [Google Scholar] [CrossRef] [PubMed]
- Karikó, K. In vitro-Transcribed mRNA Therapeutics: Out of the Shadows and Into the Spotlight. Mol. Ther. 2019, 27, 691–692. [Google Scholar] [CrossRef] [PubMed]
- Marshall, E. Gene therapy death prompts review of adenovirus vector. Science 1999, 286, 2244–2245. [Google Scholar] [CrossRef]
- Baraniuk, C. Covid-19: What do we know about Sputnik V and other Russian vaccines? BMJ 2021, 372, n743. [Google Scholar] [CrossRef]
- Yoichi, F. Return of inactivated whole-virus vaccine for superior efficacy. August 2011. Immunol. Cell Biol. 2019, 90, 571–578. [Google Scholar] [CrossRef]
- Gao, Q.; Bao, L.; Mao, H.; Wang, L.; Xu, K.; Yang, M.; Li, Y.; Zhu, L.; Wang, N.; Lv, Z.; et al. Development of an inactivated vaccine candidate for SARS-CoV-2. Science 2020, 369, 77–81. [Google Scholar] [CrossRef]
- Pollet, J.; Chen, W.-H.; Versteeg, L.; Keegan, B.; Zhan, B.; Wei, J.; Liu, Z.; Lee, J.; Kundu, R.; Adhikari, R.; et al. SARS-CoV-2 RBD219-N1C1: A yeast-expressed SARS-CoV-2 recombinant receptor-binding domain candidate vaccine stimulates virus neutralizing antibodies and T-cell immunity in mice. Hum. Vaccines Immunother. 2021, 17, 2356–2366. [Google Scholar] [CrossRef]
- Sun, W.; Leist, S.R.; McCroskery, S.; Liu, Y.; Slamanig, S.; Oliva, J.; Amanat, F.; Schäfer, A.; Dinnon, K.H.; García-Sastre, A.; et al. Newcastle disease virus (NDV) expressing the spike protein of SARS-CoV-2 as a live virus vaccine candidate. EBioMedicine 2020, 62, 103132. [Google Scholar] [CrossRef]
- Mukhamedova, M.; Wrapp, D.; Shen, C.-H.; Gilman, M.S.; Ruckwardt, T.J.; Schramm, C.A.; Ault, L.; Chang, L.; Derrien-Colemyn, A.; Lucas, S.A.; et al. Vaccination with prefusion-stabilized respiratory syncytial virus fusion protein induces genetically and antigenically diverse antibody responses. Immunity 2021, 54, 769–780.e6. [Google Scholar] [CrossRef] [PubMed]
- Weingarten-Gabbay, S.; Klaeger, S.; Sarkizova, S.; Pearlman, L.R.; Chen, D.-Y.; Gallagher, K.M.; Bauer, M.R.; Taylor, H.B.; Dunn, W.A.; Tarr, C.; et al. Profiling SARS-CoV-2 HLA-I peptidome reveals T cell epitopes from out-of-frame ORFs. Cell 2021, 184, 3962–3980. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.H.; Peters, N.C.; Maruyama, S.R.; de Brito, E.C., Jr.; de Miranda Santos, I.K.F. Working group on research priorities for development of leishmaniasis Vaccines. PLoS Negl. Trop. Dis. 2011, 5, e943. [Google Scholar] [CrossRef]
- Coler, R.N.; Reed, S.G. Second-generation vaccines against leishmaniasis. Trends Parasitol. 2005, 21, 244–249. [Google Scholar] [CrossRef]
- De Oliveira, C.I.; Nascimento, I.P.; Barral, A.; Soto, M.; Barral-Netto, M. Challenges and perspectives in vaccination against leishmaniasis. Parasitol. Int. 2009, 58, 319–324. [Google Scholar] [CrossRef]
- Duthie, M.S.; Raman, V.S.; Piazza, F.M.; Reed, S.G. The development and clinical evaluation of second-generation leishmaniasis vaccines. Vaccine 2012, 30, 134–141. [Google Scholar] [CrossRef]
- Kumar, R.; Engwerda, C. Vaccines to prevent leishmaniasis. Clin Transl Immunol. 2014, 3, e13. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, P.M.; Beaumier, C.M.; Strych, U.; Hayward, T.; Hotez, P.J.; Bottazzi, M.E. Status of vaccine research and development of vaccines for leishmaniasis. Vaccine 2016, 34, 2992–2995. [Google Scholar] [CrossRef]
- Hofmeyer, K.A.; Duthie, M.S.; Laurance, J.D.; Favila, M.A.; Van Hoeven, N.; Coler, R.N.; Reed, S.G. Optimizing immunization strategies for the induction of antigen-specific CD4 and CD8 T cell responses for protection against intracellular parasites. Clin. Vaccine Immunol. 2016, 23, 785–794. [Google Scholar] [CrossRef]
- Reed, S.G.; Coler, R.N.; Mondal, D.; Kamhawi, S.; Valenzuela, J.G. Leishmania vaccine development: Exploiting the host-vector-parasite interface. Expert Rev. Vaccines 2016, 15, 81–90. [Google Scholar] [CrossRef]
- Mo, A.X.; Pesce, J.; Hall, B.F. Visceral leishmaniasis control and elimination: Is there a role for vaccines in achieving regional and global goals? Am. J. Trop. Med. Hyg. 2016, 16, 184. [Google Scholar] [CrossRef][Green Version]
- Seyed, N.; Taheri, T.; Rafati, S. Post-Genomics and Vaccine Improvement for Leishmania. Front. Microbiol. 2016, 7, 467. [Google Scholar] [CrossRef]
- Srivastava, S.; Shankar, P.; Mishra, J.; Singh, S. Possibilities and challenges for developing a successful vaccine for leishmaniasis. Parasites Vectors 2016, 9, 277. [Google Scholar] [CrossRef] [PubMed]
- Moafi, M.; Rezvan, H.; Sherkat, R.; Taleban, R. Leishmania Vaccines Entered in Clinical Trials: A Review of Literature. Int. J. Prev. Med. 2019, 10, 95. [Google Scholar] [CrossRef]
- Coutinho, D.O.B.; Duthie, M.S.; Alves Pereira, V.R. Vaccines for leishmaniasis and the implications of their development for American tegumentary leishmaniasis. Hum. Vaccines Immunother. 2020, 16, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Mohebali, M.; Nadim, A.; Khamesipour, A. An overview of leishmanization experience: A successful control measure and a tool to evaluate candidate vaccines. Acta Trop. 2019, 200, 105173. [Google Scholar] [CrossRef] [PubMed]
- Dey, R.; Dagur, P.K.; Selvapandiyan, A.; McCoy, J.P.; Salotra, P.; Duncan, R.; Nakhasi, H.L. Live AttenuatedLeishmania donovanip27 Gene Knockout Parasites Are Nonpathogenic and Elicit Long-Term Protective Immunity in BALB/c Mice. J. Immunol. 2013, 190, 2138–2149. [Google Scholar] [CrossRef]
- Zhang, W.-W.; Karmakar, S.; Gannavaram, S.; Dey, R.; Lypaczewski, P.; Ismail, N.; Siddiqui, A.; Simonyan, V.; Oliveira, F.; Coutinho-Abreu, I.V.; et al. A second generation leishmanization vaccine with a markerless attenuated Leishmania major strain using CRISPR gene editing. Nat. Commun. 2020, 11, 1–14. [Google Scholar] [CrossRef]
- Kamil, A.A.; Khalil, E.A.; Musa, A.M.; Modabber, F.; Mukhtar, M.M.; Ibrahim, M.E.; Zijlstra, E.E.; Sacks, D.; Smith, P.G.; Zicker, F.; et al. Alum-precipitated autoclaved Leishmania major plus Bacille Calmette-Guérrin, a candidate vaccine for visceral leishmaniasis: Safety, skin-delayed type hypersensitivity response and dose finding in healthy volunteers. Trans. R Soc. Trop. Med. Hyg. 2003, 97, 365–368. [Google Scholar] [CrossRef]
- Chakravarty, J.; Kumar, S.; Trivedi, S.; Rai, V.K.; Singh, A.; Ashman, J.A.; Laughlin, E.M.; Coler, R.N.; Kahn, S.J.; Beckmann, A.M.; et al. A clinical trial to evaluate the safety and immunogenicity of the LEISH-F1+MPL-SE vaccine for use in the prevention of visceral leishmaniasis. Vaccine 2011, 29, 3531–3537. [Google Scholar] [CrossRef] [PubMed]
- Llanos-Cuentas, A.; Calderón, W.; Cruz, M.; Ashman, J.A.; Alves, F.P.; Coler, R.N.; Bogatzki, L.Y.; Bertholet, S.; Laughlin, E.M.; Kahn, S.J.; et al. A clinical trial to evaluate the safety and immunogenicity of the LEISH-F1+MPL-SE vaccine when used in combination with sodium stibogluconate for the treatment of mucosal leishmaniasis. Vaccine 2010, 28, 7427–7435. [Google Scholar] [CrossRef] [PubMed]
- Younis, B.M.; Osman, M.; Khalil, E.A.G.; Santoro, F.; Furini, S.; Wiggins, R.; Keding, A.; Carraro, M.; Musa, A.E.A.; Abdarahaman, M.A.A.; et al. Safety and immunogenicity of ChAd63-KH vaccine in post-kala-azar dermal leishmaniasis patients in Sudan. Mol. Ther. 2021, 29, 2366–2377. [Google Scholar] [CrossRef] [PubMed]
- Gradoni, L. Canine Leishmania vaccines: Still a long way to go. Vet. Parasitol. 2015, 208, 94–100. [Google Scholar] [CrossRef]
- Velez, R.; Gállego, M. Commercially approved vaccines for canine leishmaniosis: A review of available data on their safety and efficacy. Trop. Med. Int. Health 2020, 25, 540–557. [Google Scholar] [CrossRef]
- Goto, Y.; Bhatia, A.; Raman, V.S.; Liang, H.; Mohamath, R.; Picone, A.F.; Vidal, S.E.Z.; Vedvick, T.S.; Howard, R.F.; Reed, S.G. KSAC, the First Defined Polyprotein Vaccine Candidate for Visceral Leishmaniasis. Clin. Vaccine Immunol. 2011, 18, 1118–1124. [Google Scholar] [CrossRef]
- Cecílio, P.; Oristian, J.; Meneses, C.; Serafim, T.D.; Valenzuela, J.G.; Da Silva, A.C.; Oliveira, F. Engineering a vector-based pan-Leishmania vaccine for humans: Proof of principle. Sci. Rep. 2020, 10, 1–20. [Google Scholar] [CrossRef]
- Ashwin, H.; Sadlova, J.; Vojtkova, B.; Becvar, T.; Lypaczewski, P.; Schwartz, E.; Greensted, E.; Van Bocxlaer, K.; Pasin, M.; Lipinski, K.S.; et al. Characterization of a new Leishmania major strain for use in a controlled human infection model. Nat. Commun. 2021, 12, 215. [Google Scholar] [CrossRef]
- Aschwanden, C. Five reasons why COVID herd immunity is probably impossible. Nature 2021, 591, 520–522. [Google Scholar] [CrossRef]
- Sahin, U.; Muik, A.; Derhovanessian, E.; Vogler, I.; Kranz, L.M.; Vormehr, M.; Baum, A.; Pascal, K.; Quandt, J.; Maurus, D.; et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature 2020, 586, 594–599. [Google Scholar] [CrossRef]
- Angyal, A.; Longet, S.; Moore, S.C.; Payne, R.P.; Harding, A.; Tipton, T.; Rongkard, P.; Ali, M.; Hering, L.M.; Meardon, N.; et al. T-cell and antibody responses to first BNT162b2 vaccine dose in previously infected and SARS-CoV-2-naive UK health-care workers: A multicentre prospective cohort study. Lancet Microbe. 2022, 3, e21–e31. [Google Scholar] [CrossRef]
- Breton, G.; Mendoza, P.; Hägglöf, T.; Oliveira, T.Y.; Schaefer-Babajew, D.; Gaebler, C.; Turroja, M.; Hurley, A.; Caskey, M.; Nussenzweig, M.C. Persistent cellular immunity to SARS-CoV-2 infection. J. Exp. Med. 2021, 218, e20202515. [Google Scholar] [CrossRef] [PubMed]
- Gaebler, C.; Wang, Z.; Lorenzi, J.C.C.; Muecksch, F.; Finkin, S.; Tokuyama, M.; Cho, A.; Jankovic, M.; Schaefer-Babajew, D.; Oliveira, T.Y.; et al. Evolution of antibody immunity to SARS-CoV-2. Nature 2021, 591, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.S.; O’halloran, J.A.; Kalaidina, E.; Kim, W.; Schmitz, A.J.; Zhou, J.Q.; Lei, T.; Thapa, M.; Chen, R.E.; Case, J.B.; et al. SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Nature 2021, 596, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Grifoni, A.; Sidney, J.; Vita, R.; Peters, B.; Crotty, S.; Weiskopf, D.; Sette, A. SARS-CoV-2 human T cell epitopes: Adaptive immune response against COVID-19. Cell Host Microbe 2021, 29, 1076–1092. [Google Scholar] [CrossRef]
- Hacisuleyman, E.; Hale, C.; Saito, Y.; Blachere, N.E.; Bergh, M.; Conlon, E.G.; Schaefer-Babajew, D.J.; DaSilva, J.; Muecksch, F.; Gaebler, C.; et al. Vaccine Breakthrough Infections with SARS-CoV-2 Variants. N. Engl. J. Med. 2021, 384, 2212–2218. [Google Scholar] [CrossRef]
- Starr, T.N.; Greaney, A.J.; Addetia, A.; Hannon, W.W.; Choudhary, M.C.; Dingens, A.S.; Li, J.Z.; Bloom, J.D. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science 2021, 371, 850–854. [Google Scholar] [CrossRef]
- Zhou, H.; Dcosta, B.M.; Samanovic, M.I.; Mulligan, M.J.; Landau, N.R.; Tada, T.B. 1.526 SARS-CoV-2 Variants Identified in New York City are Neutralized by Vaccine-Elicited and Therapeutic Monoclonal Antibodies. mBio 2021, 12, e0138621. [Google Scholar] [CrossRef]
- Edara, V.V.; Norwood, C.; Floyd, K.; Lai, L.; Davis-Gardner, M.E.; Hudson, W.H.; Mantus, G.; Nyhoff, L.E.; Adelman, M.W.; Fineman, R.; et al. Infection- and vaccine-induced antibody binding and neutralization of the B.1.351 SARS-CoV-2 variant. Cell Host Microbe 2021, 29, 516–521.e3. [Google Scholar] [CrossRef]
- Li, R.; Ma, X.; Deng, J.; Chen, Q.; Liu, W.; Peng, Z.; Qiao, Y.; Lin, Y.; He, X.; Zhang, H. Differential efficiencies to neutralize the novel mutants B.1.1.7 and 501Y.V2 by collected sera from convalescent COVID-19 patients and RBD nanoparticle-vaccinated rhesus macaques. Cell. Mol. Immunol. 2021, 18, 1058–1060. [Google Scholar] [CrossRef]
- Scully, M.; Singh, D.; Lown, R.; Poles, A.; Solomon, T.; Levi, M.; Goldblatt, D.; Kotoucek, P.; Thomas, W.; Lester, W. Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19 Vaccination. N. Engl. J. Med. 2021, 384, 2202–2211. [Google Scholar] [CrossRef] [PubMed]
- Kaushal, H.; Bras-Gonçalves, R.; Negi, N.S.; Lemesre, J.L.; Papierok, G.; Salotra, P. Role of CD8(+) T cells in protection against Leishmania donovani infection in healed Visceral Leishmaniasis individuals. BMC Infect. Dis. 2014, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hamrouni, S.; Bras-Gonçalves, R.; Kidar, A.; Aoun, K.; Chamakh-Ayari, R.; Petitdidier, E.; Messaoudi, Y.; Pagniez, J.; Lemesre, J.L.; Meddeb-Garnaoui, A. Design of multi-epitope peptides containing HLA class-I and class-II-restricted epitopes derived from immunogenic Leishmania proteins, and evaluation of CD4+ and CD8+ T cell responses induced in cured cutaneous leishmaniasis subjects. PLoS Negl. Trop. Dis. 2020, 14, e0008093. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S. Extra Life: A Short History of Living Longer; Riverhead Books; Penguin Publishing Group: Riverhead, NY, USA, 2021; p. 320. ISBN 9780525538851. [Google Scholar]
- Cordsmeier, A.; Wagner, N.; Lührmann, A.; Berens, C. Defying Death—How Coxiella burnetii Copes with Intentional Host Cell Suicide. Yale J. Biol. Med. 2019, 92, 619–628. [Google Scholar]
- Eldin, C.; Mélenotte, C.; Mediannikov, O.; Ghigo, E.; Million, M.; Edouard, S.; Mege, J.L.; Maurin, M.; Raoult, D. From Q Fever to Coxiella burnetii Infection: A Paradigm Change. Clin. Microbiol. Rev. 2017, 30, 115–190. [Google Scholar] [CrossRef]
- Chang, K.P.; Kolli, B.K.; The New Light Group. New “light” for one-world approach toward safe and effective control of animal diseases and insect vectors from leishmaniac perspectives. Parasites Vectors 2016, 9, 1–13. [Google Scholar] [CrossRef]
- Sah, J.F.; Ito, H.; Kolli, B.K.; Peterson, D.A.; Sassa, S.; Chang, K.P. Genetic rescue of Leishmania deficiency in porphyrin biosynthesis creates mutants suitable for analysis of cellular events in uroporphyria and for photodynamic therapy. J. Biol. Chem. 2002, 277, 14902–14909. [Google Scholar] [CrossRef]
- Dutta, S.; Sassa, S.; Chang, K.P. Leishmania spp.: Delta-aminolevulinate-inducible porphyria by genetic complementation of incomplete heme biosynthesis. Exp. Parasitol. 2008, 118, 629–636. [Google Scholar] [CrossRef]
- Sharma, R.; Viana, S.M.; Ng, D.K.P.; Kolli, B.K.; Chang, K.P.; de Oliveira, C.I. Photodynamic inactivation of Leishmania braziliensis doubly sensitized with uroporphyrin and diamino-phthalocyanine activates effector functions of macrophages in vitro. Sci. Rep. 2020, 10, 17065. [Google Scholar] [CrossRef]
- Dutta, S.; Ongarora, B.G.; Li, H.; Vicente, M.G.H.; Kolli, B.K.; Chang, K.P. Intracellular targeting specificity of novel phthalocyanines assessed in a host-parasite model for developing potential photomedicine. PLoS ONE 2011, 6, e20786. [Google Scholar] [CrossRef]
- Al-Qahtani, A.; Alkahtani, S.; Kolli, B.; Tripathi, P.; Dutta, S.; Al-Kahtane, A.A.; Jiang, X.J.; Ng, D.K.; Chang, K.P. Aminophthalocyanine-Mediated Photodynamic Inactivation of Leishmania tropica. Antimicrob. Agents Chemother. 2016, 60, 2003–2011. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Kolli, B.K.; Tang, A.; Sassa, S.; Chang, K.P. Transgenic Leishmania model for delta-aminolevulinate-inducible monospecific uroporphyria: Cytolytic phototoxicity initiated by singlet oxygen-mediated inactivation of functional proteins and its ablation by evacuation of cytosolic uroporphyrin. Eukaryot. Cell 2008, 7, 1146–1157. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Waki, K.; Chang, K.P. Combinational sensitization of Leishmania with uroporphyrin and aluminum phthalocyanine synergistically enhances their photodynamic inactivation in vitro and in vivo. Photochem Photobiol. 2012, 88, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Chang, C.; Kolli, B.K.; Sassa, S.; Yousef Showe, M.; Showe, L.; Chang, K.P. Delta-aminolevulinate-induced host-parasite porphyric disparity for selective photolysis of transgenic Leishmania in the phagolysosomes of mononuclear phagocytes: A potential novel platform for vaccine delivery. Euk. Cell 2012, 11, 430–441. [Google Scholar] [CrossRef][Green Version]
- Kumari, S.; Samant, M.; Khare, P.; Misra, P.; Dutta, S.; Kolli, B.K.; Sharma, S.; Chang, K.P.; Dube, A. Photodynamic vaccination of hamsters with inducible suicidal mutants of Leishmania amazonensis elicits immunity against visceral leishmaniasis. Eur. J. Immunol. 2009, 39, 178–191. [Google Scholar] [CrossRef]
- Viana, S.M.; Celes, F.S.; Ramirez, L.; Kolli, B.; Ng, D.K.P.; Chang, K.P.; De Oliveira, C.I. Photodynamic Vaccination of BALB/c Mice for Prophylaxis of Cutaneous Leishmaniasis Caused by Leishmania amazonensis. Front Microbiol. 2018, 9, 165. [Google Scholar] [CrossRef]
- Chang, K.P.; Kolli, B.K.; Fan, C.K.; Ng, D.K.P.; Wong, C.T.T.; Manna, L.; Corso, R.; Shih, N.Y.; Elliott, R.L.; Jiang, X.P.; et al. Progress toward development of photodynamic vaccination against infectious/malignant diseases and photodynamic mosquitocides. In Proceedings of the SPIE 10479, Light-Based Diagnosis and Treatment of Infectious Diseases, San Francisco, CA, USA, 8 February 2018. [Google Scholar] [CrossRef]
- Chang, K.P.; Ng, D.K.P.; Fan, C.K.; Batchu, R.B.; Kolli, B.K. Effective Delivery of Cancer Vaccines with Oxidatively Photo-Inactivated Transgenic Leishmania for Tumor Immunotherapy in Mouse Models. OBM Genet. Mol. Cancer Ther. 2020, 4. [Google Scholar] [CrossRef]
- Thomas, M.B. Epidemics on the move: Climate change and infectious disease. PLoS Biol. 2020, 18, e3001013. [Google Scholar] [CrossRef]
- Chang, K.P. Vaccination for Disease Prevention and Control: The Necessity of Renewed Emphasis and New Approaches. J. Immunol. Immunotech. 2014, 1, 10.17653/2374-9105.SSe0001. [Google Scholar] [CrossRef]
- Tatsis, N. Ertl HC. Adenoviruses as vaccine vectors. Mol. Ther. 2004, 10, 616–629. [Google Scholar] [CrossRef]
- Martinez, D.R.; Schäfer, A.; Leist, S.R.; De la Cruz, G.; West, A.; Atochina-Vasserman, E.N.; Lindesmith, L.C.; Pardi, N.; Parks, R.; Barr, M.; et al. Chimeric spike mRNA vaccines protect against Sarbecovirus challenge in mice. Science 2021, 373, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.S.; Sullivan, N.J. Emerging viral diseases from a vaccinology perspective: Preparing for the next pandemic. Nat. Immunol. 2018, 19, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Planas, D.; Veyer, D.; Baidaliuk, A.; Staropoli, I.; Guivel-Benhassine, F.; Rajah, M.M.; Planchais, C.; Porrot, F.; Robillard, N.; Puech, J.; et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature 2021, 596, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Jason, N.; Xiaoyu, L.; Matthew, M.; Guorui, X.; Victoria, M.; Warner, G.C.; Sulggi, A.; Lee, N.; Roan, R. mRNA vaccine-induced T cells respond identically to SARS-CoV-2 variants of concern but differ in longevity and homing properties depending on prior infection status. Elife 2021, 10, e72619. [Google Scholar] [CrossRef]
- Chang, K.P.; Reed, S.G.; McGwire, B.S.; Soong, L. Leishmania model for microbial virulence: The relevance of parasite multiplication and pathoantigenicity. Acta Trop. 2003, 85, 375–390. [Google Scholar] [CrossRef]
- Chang, K.P.; McGwire, B.S. Molecular determinants and regulation of Leishmania virulence. Kinetoplastid Biol. Dis. 2002, 1, 1. [Google Scholar] [CrossRef]
- Langenberg, M.C.C.; Dekkers, O.M.; Roestenberg, M. Are placebo controls necessary in controlled human infection trials for vaccines? Lancet Infect Dis. 2020, 20, e69–e74. [Google Scholar] [CrossRef]
- Nurk, S.; Koren, S.; Rhie, A.; Rautiainen, M.; Bzikadze, A.V.; Mikheenko, A.; Vollger, M.R.; Altemose, N.; Uralsky, L.; Gershman, A.; et al. The complete sequence of a human genome. bioRxiv 2021, 1–32. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, K.P.; Reynolds, J.M.; Liu, Y.; He, J.J. Leishmaniac Quest for Developing a Novel Vaccine Platform. Is a Roadmap for Its Advances Provided by the Mad Dash to Produce Vaccines for COVID-19? Vaccines 2022, 10, 248. https://doi.org/10.3390/vaccines10020248
Chang KP, Reynolds JM, Liu Y, He JJ. Leishmaniac Quest for Developing a Novel Vaccine Platform. Is a Roadmap for Its Advances Provided by the Mad Dash to Produce Vaccines for COVID-19? Vaccines. 2022; 10(2):248. https://doi.org/10.3390/vaccines10020248
Chicago/Turabian StyleChang, Kwang Poo, Joseph M. Reynolds, Ying Liu, and Johnny J. He. 2022. "Leishmaniac Quest for Developing a Novel Vaccine Platform. Is a Roadmap for Its Advances Provided by the Mad Dash to Produce Vaccines for COVID-19?" Vaccines 10, no. 2: 248. https://doi.org/10.3390/vaccines10020248
APA StyleChang, K. P., Reynolds, J. M., Liu, Y., & He, J. J. (2022). Leishmaniac Quest for Developing a Novel Vaccine Platform. Is a Roadmap for Its Advances Provided by the Mad Dash to Produce Vaccines for COVID-19? Vaccines, 10(2), 248. https://doi.org/10.3390/vaccines10020248





