The Relationship between Health Literacy and COVID-19 Vaccination Prevalence during a Rapidly Evolving Pandemic and Infodemic
Abstract
1. Introduction
- Is there a difference among county areas (North Fulton, South Fulton, Atlanta) in vaccination prevalence and in demographic factors that might predict vaccination prevalence?
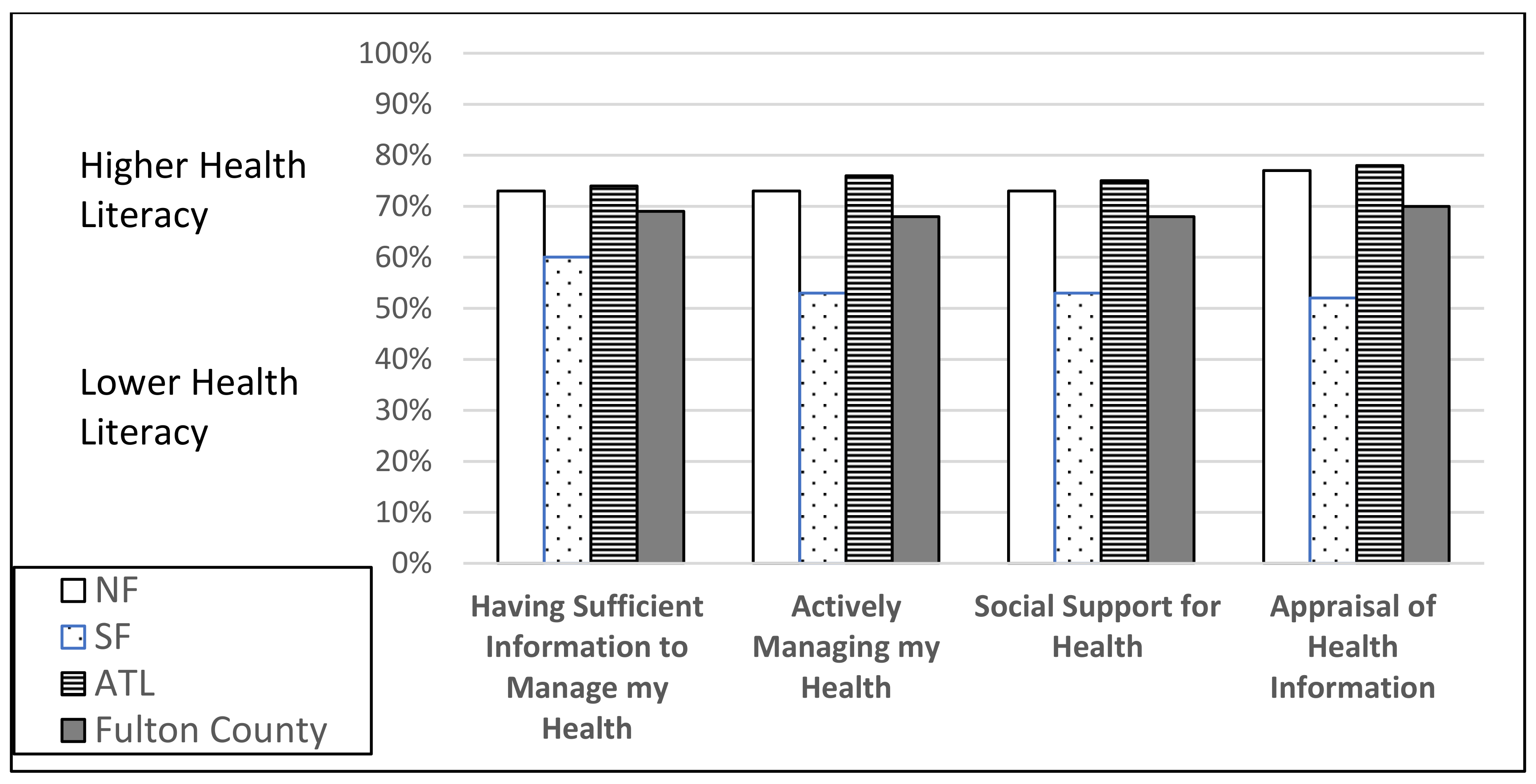
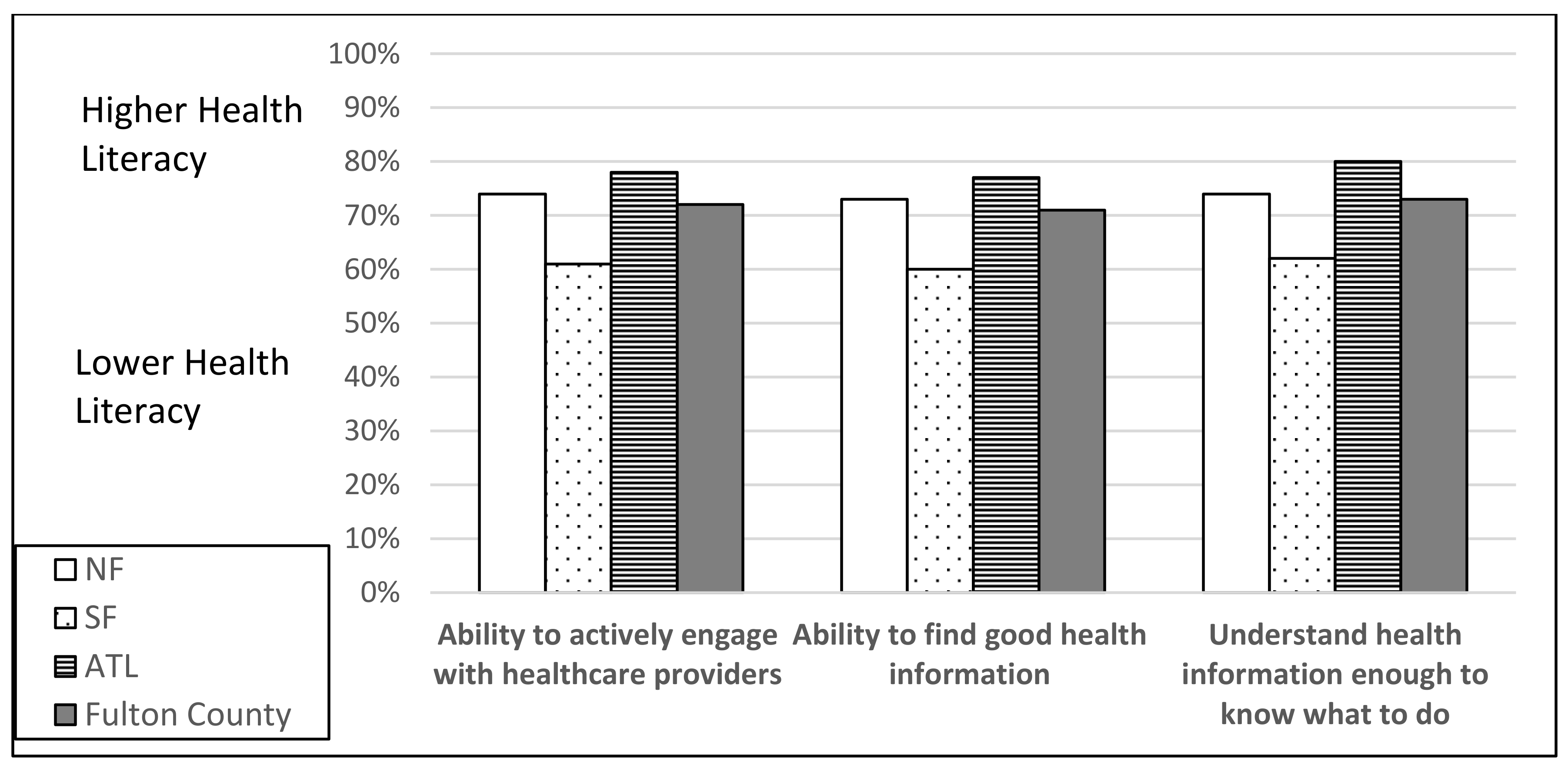
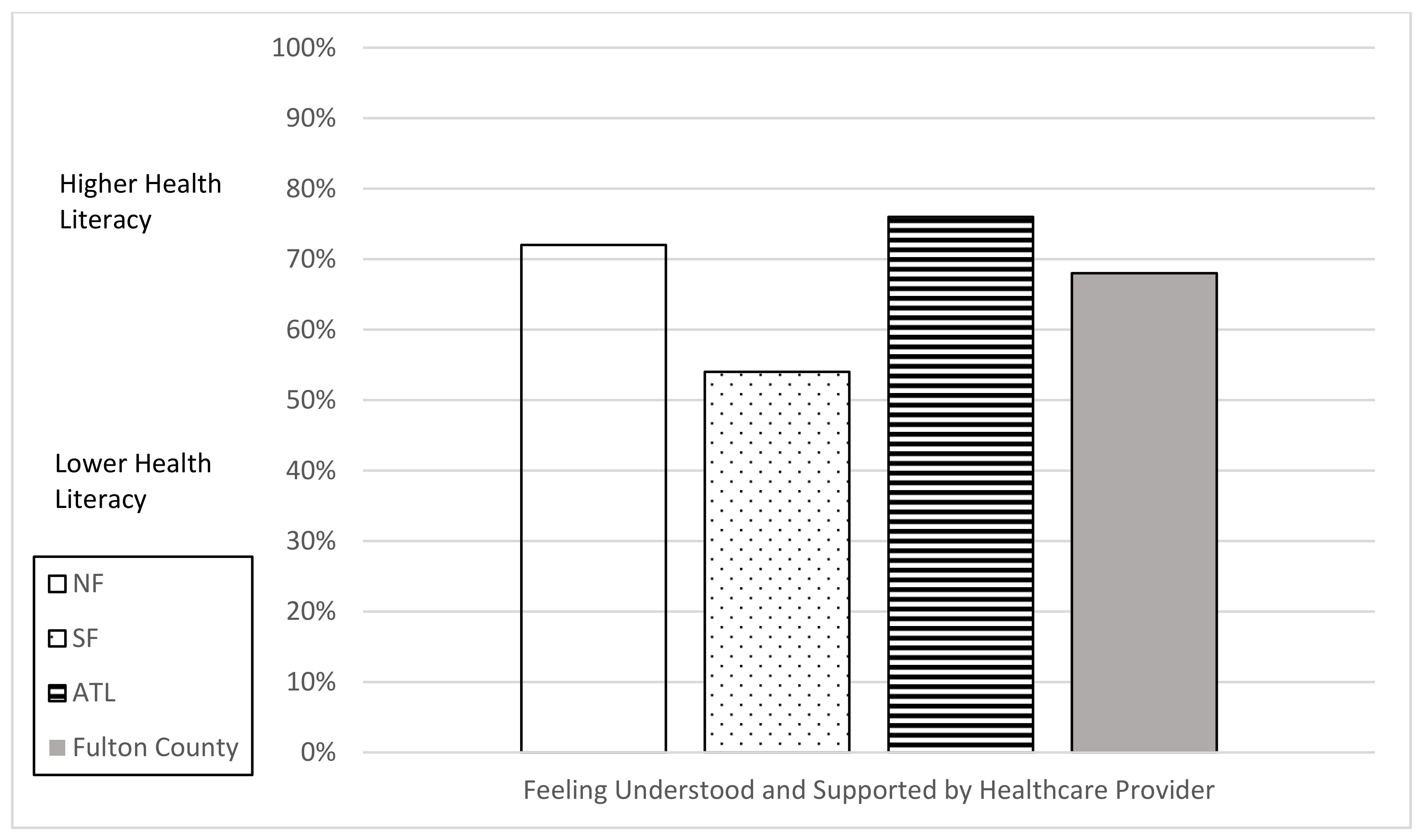
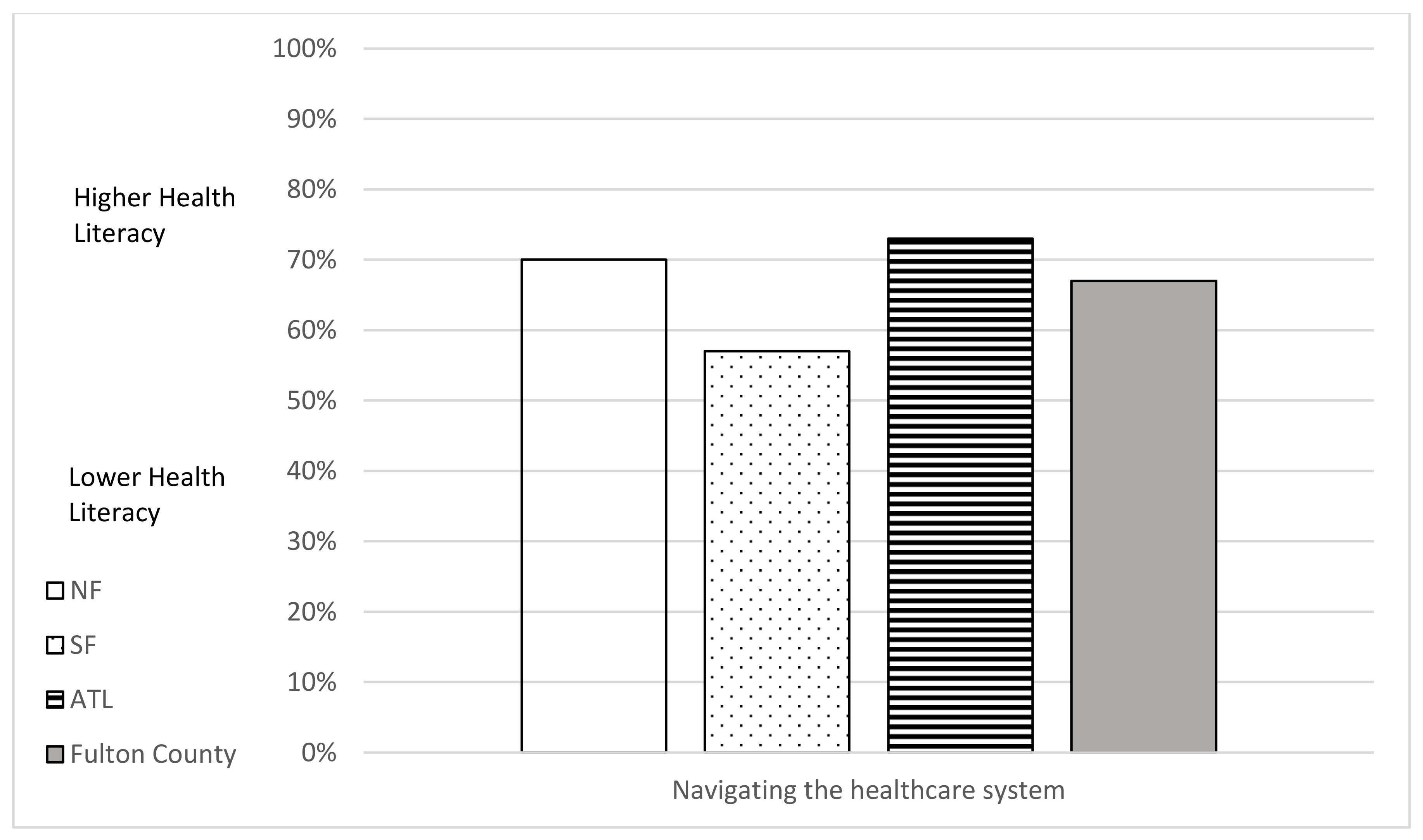
- How do individual and organizational health literacy scores for Fulton County residents vary by county area (North Fulton, South Fulton, Atlanta)?
- Is functional, interactive, and critical health literacy associated with vaccination prevalence by county area?
2. Methods
2.1. Sample
2.2. Measures
3. Results
4. Discussion
Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okan, O.; Messer, M.; Levin-Zamir, D.; Paakkari, L.; Sørensen, K. Health literacy as a social vaccine in the COVID-19 pandemic. Health Promot. Int. 2022, daab197. [Google Scholar] [CrossRef] [PubMed]
- Hange, N.; Agoli, A.M.; Pormento, M.K.L.; Sharma, A.; Somagutta, M.R.; Paikkattil, N.; Jadhav, A.; Bethineedi, D.; Pisude, P. Impact of COVID-19 response on public health literacy and communication. Health Promot. Perspect. 2022, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Swire-Thompson, B.; Lazer, D. Public Health and Online Misinformation: Challenges and Recommendations. Annu. Rev. Public Health 2020, 41, 433–451. [Google Scholar] [CrossRef] [PubMed]
- Baccolini, V.; Renzi, E.; Isonne, C.; Migliara, G.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. COVID-19 Vaccine Hesitancy among Italian University Students: A Cross-Sectional Survey during the First Months of the Vaccination Campaign. Vaccines 2021, 9, 1292. [Google Scholar] [CrossRef] [PubMed]
- Laurencin, C.T.; McClinton, A. The COVID-19 Pandemic: A Call to Action to Identify and Address Racial and Ethnic Disparities. J. Racial Ethn. Health Disparities 2020, 7, 398–402. [Google Scholar] [CrossRef]
- Lockyer, B.; Islam, S.; Rahman, A.; Dickerson, J.; Pickett, K.; Sheldon, T.; Wright, J.; McEachan, R.; Sheard, L.; the Bradford Institute for Health Research COVID-19 Scientific Advisory Group. Understanding COVID-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021, 24, 1158–1167. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; (HLS-EU) Consortium Health Literacy Project European. Health Literacy and Public Health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. Health Literacy Tool Shed. Available online: https://healthliteracy.bu.edu/ (accessed on 28 October 2022).
- Hawkins, M.; Gill, S.D.; Batterham, R.; Elsworth, G.R.; Osborne, R.H. The Health Literacy Questionnaire (HLQ) at the patient-clinician interface: A qualitative study of what patients and clinicians mean by their HLQ scores. BMC Health Serv. Res. 2017, 17, 309. [Google Scholar] [CrossRef]
- Sentell, T.; Vamos, S.; Okan, O. Interdisciplinary Perspectives on Health Literacy Research Around the World: More Important Than Ever in a Time of COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3010. [Google Scholar] [CrossRef]
- Damian, A.J.; Gallo, J.J. Promoting Health Literacy during the COVID-19 Pandemic: A Call to Action for Healthcare Professionals: HKS Misinformation Review. Available online: https://misinforeview.hks.harvard.edu/article/promoting-health-literacy-during-the-covid-19-pandemic-a-call-to-action-for-healthcare-professionals/ (accessed on 28 October 2022).
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef]
- Weldring, T.; Smith, S.M.S. Article Commentary: Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv. Insights 2013, 6, HSI.S11093. [Google Scholar] [CrossRef]
- Hawkins, M.; Elsworth, G.R.; Osborne, R.H. Application of validity theory and methodology to patient-reported outcome measures (Proms): Building an argument for validity. Qual. Life Res. 2018, 27, 1695–1710. [Google Scholar] [CrossRef]
- Jessup, R.L.; Osborne, R.H.; Beauchamp, A.; Bourne, A.; Buchbinder, R. Health literacy of recently hospitalised patients: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Health Serv. Res. 2017, 17, 52. [Google Scholar] [CrossRef]
- Simpson, R.M.; Knowles, E.; O’Cathain, A. Health Literacy Levels of British adults: A cross-sectional survey using two domains of the Health Literacy Questionnaire (HLQ). BMC Public Health 2020, 20, 1819. [Google Scholar] [CrossRef]
- Georgia COVID-19 Vaccinations by Census Tract and Demographics Arcgis.com. Available online: https://www.arcgis.com/home/item.html?id=17a8a4af79e5453a9132aaa29fb4ad22 (accessed on 17 July 2022).
- HUD-USPS ZIP Code Crosswalk Files. Available online: https://www.huduser.gov/portal/datasets/usps_crosswalk.html (accessed on 30 June 2022).
- Berg, S.H.; O’Hara, J.K.; Shortt, M.T.; Thune, H.; Brønnick, K.K.; Lungu, D.A.; Røislien, J.; Wiig, S. Health authorities’ health risk communication with the public during pandemics: A rapid scoping review. BMC Public Health 2021, 21, 1401. [Google Scholar] [CrossRef]
- Turhan, Z.; Dilcen, H.Y.; Dolu, İ. The mediating role of Health Literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr. Psychol. 2021, 41, 8147–8156. [Google Scholar] [CrossRef]
- Montagni, I.; Ouazzani-Touhami, K.; Mebarki, A.; Texier, N.; Schück, S.; Tzourio, C.; the CONFINS Group. Acceptance of a COVID-19 vaccine is associated with ability to detect fake news and health literacy. J. Public Health 2021, 43, 695–702. [Google Scholar] [CrossRef]
- Cadeddu, C.; Regazzi, L.; Bonaccorsi, G.; Rosano, A.; Unim, B.; Griebler, R.; Link, T.; De Castro, P.; D’Elia, R.; Mastrilli, V.; et al. The determinants of vaccine literacy in the Italian population: Results from the Health Literacy Survey 2019. Int. J. Environ. Res. Public Health 2022, 19, 4429. [Google Scholar] [CrossRef]
- Hu, S.; Xiong, C.; Li, Q.; Wang, Z.; Jiang, Y. COVID-19 vaccine hesitancy cannot fully explain disparities in vaccination coverage across the contiguous United States. Vaccines 2022, 40, 5471–5482. [Google Scholar] [CrossRef]
- Gharpure, R.; Guo, A.; Bishnoi, C.K.; Patel, U.; Gifford, D.; Tippins, A.; Jaffe, A.; Shulman, E.; Stone, N.; Mungai, E.; et al. Early COVID-19 First-Dose Vaccination Coverage Among Residents and Staff Members of Skilled Nursing Facilities Participating in the Pharmacy Partnership for Long-Term Care Program—United States, December 2020–January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Karmakar, M.; Lantz, P.M.; Tipirneni, R. Association of Social and Demographic Factors with COVID-19 Incidence and Death Rates in the US. JAMA Netw. Open 2021, 4, e2036462. [Google Scholar] [CrossRef] [PubMed]
- Roozenbeek, J.; Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; van der Bles, A.M.; van der Linden, S. Susceptibility to misinformation about COVID-19 around the world. R. Soc. Open Sci. 2020, 7, 201199. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Lima, G.; Cha, M.; Cha, C.; Kulshrestha, J.; Ahn, Y.-Y.; Varol, O. Misinformation, believability, and vaccine acceptance over 40 countries: Takeaways from the initial phase of the COVID-19 infodemic. PLoS ONE 2022, 17, e0263381. [Google Scholar] [CrossRef]
- Sheridan, S.L.; Halpern, D.J.; Viera, A.J.; Berkman, N.D.; Donahue, K.E.; Crotty, K. Interventions for Individuals with Low Health Literacy: A Systematic Review. J. Health Commun. 2011, 16 (Suppl. 3), 30–54. [Google Scholar] [CrossRef]
- Sudore, R.; Schillinger, D. Interventions to Improve Care for Patients with Limited Health Literacy. J. Clin. Outcomes Manag. 2009, 16, 20–29. [Google Scholar]
- Kripalani, S.; Weiss, B.D. Teaching about health literacy and clear communication. J. Gen. Intern. Med. 2006, 21, 888–890. [Google Scholar] [CrossRef]
- Adult Literacy in the United States. Available online: https://nces.ed.gov/pubs2019/2019179/index.asp (accessed on 30 July 2022).
- Federal Plain Language Guidelines. 2011. Available online: https://www.plainlanguage.gov/guidelines/ (accessed on 30 July 2022).
- National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care. Available online: https://thinkculturalhealth.hhs.gov/assets/pdfs/EnhancedNationalCLASStandards.pdf (accessed on 30 July 2022).
| North Fulton (21.2%) | South Fulton (44.2%) | Atlanta (34.6%) | Total Fulton County | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean (Sd) | n | % | Mean (Sd) | n | % | Mean (Sd) | n | % | Mean (Sd) | |
| Age | 90 | 36.7 (12.9) | 188 | 44.7 (14.3) | 147 | 40.1 (13.4) | 425 | 40.8 (13.9) | ||||
| Female | 60 | 66.7% | 144 | 76.6% | 101 | 68.7% | 305 | 71.8% | ||||
| High School Diploma or Less | 15 | 16.7% | 28 | 14.9% | 17 | 11.6% | 60 | 14.1% | ||||
| No Health Insurance | 16 | 17.8% | 25 | 13.3% | 24 | 16.3% | 65 | 15.3% | ||||
| African American or Black | 76 | 84.4% | 166 | 88.3% | 129 | 87.8% | 371 | 87.3% | ||||
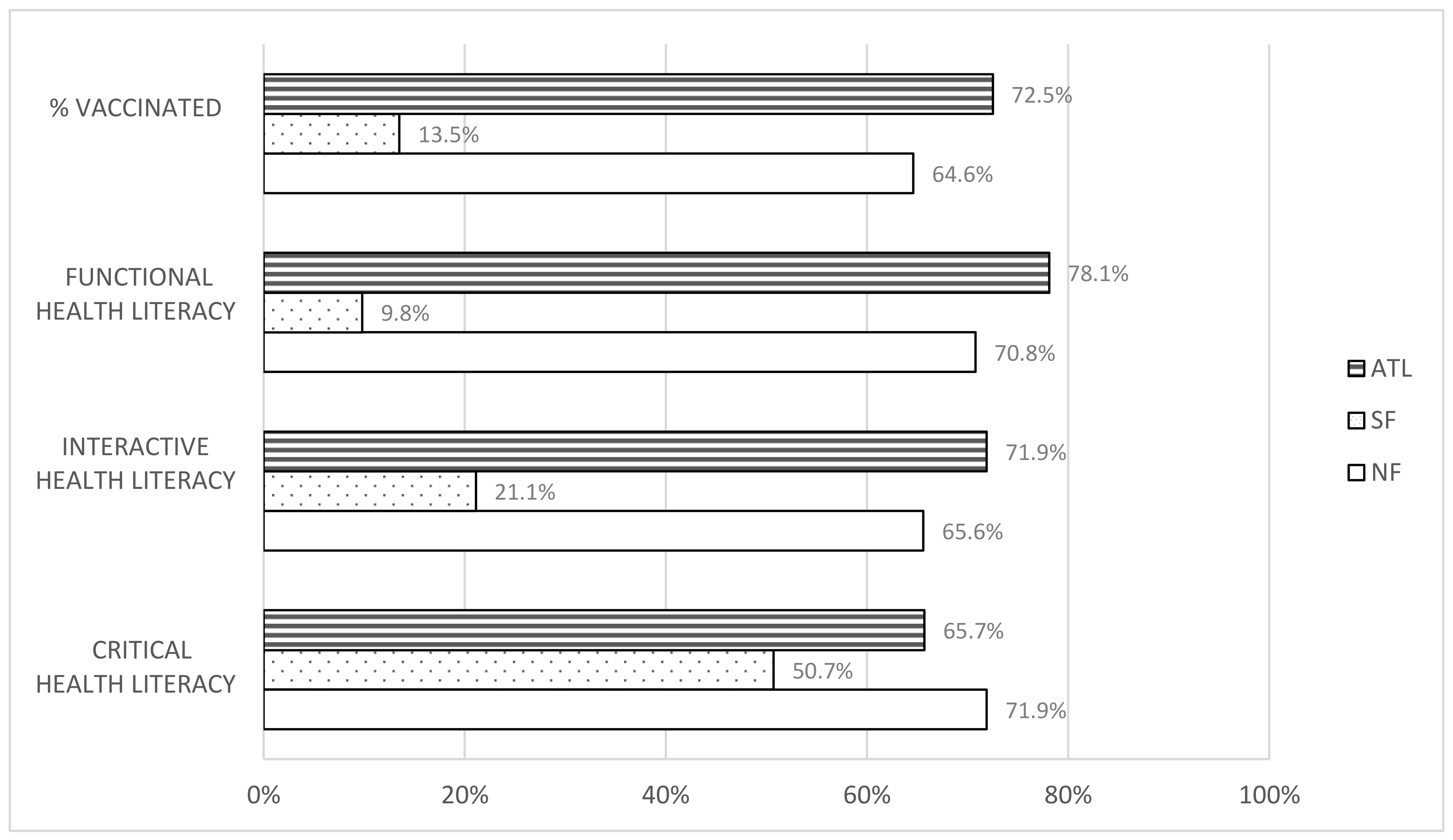
| Complete Vaccination Prevalence * | 71.9% | 50.7% | 65.7% | 62.4% | ||||||||
| Variable | B | SE B | Beta | t | p |
|---|---|---|---|---|---|
| Gender | 0.61 | 0.863 | 0.035 | 0.707 | 0.48 |
| Age | −0.125 | 0.029 | −0.21 | −4.265 | 0.00 * |
| Health Insurance Status | 0.276 | 1.132 | 0.012 | 0.243 | 0.808 |
| Education | 0.502 | 1.16 | 0.021 | 0.433 | 0.665 |
| Complete Vaccination | B | 95% CI for B | SE B | β | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Model | 0.450 | 0.445 | |||||
| Constant | 67.257 | 65.410 | 69.104 | 0.940 | 0.450 | ||
| Age | −0.119 | −0.162 | −0.076 | 0.022 | −0.200 ** | ||
| FHL * | −1.211 | −1.830 | −0.591 | 0.315 | −0.395 ** | ||
| IHL * | 0.718 | 0.268 | 1.168 | 0.229 | 0.449 ** | ||
| CHL * | 1.600 | 1.080 | 2.119 | 0.264 | 0.533 ** | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feinberg, I.; Scott, J.Y.; Holland, D.P.; Lyn, R.; Scott, L.C.; Maloney, K.M.; Rothenberg, R. The Relationship between Health Literacy and COVID-19 Vaccination Prevalence during a Rapidly Evolving Pandemic and Infodemic. Vaccines 2022, 10, 1989. https://doi.org/10.3390/vaccines10121989
Feinberg I, Scott JY, Holland DP, Lyn R, Scott LC, Maloney KM, Rothenberg R. The Relationship between Health Literacy and COVID-19 Vaccination Prevalence during a Rapidly Evolving Pandemic and Infodemic. Vaccines. 2022; 10(12):1989. https://doi.org/10.3390/vaccines10121989
Chicago/Turabian StyleFeinberg, Iris, Jane Yoon Scott, David P. Holland, Rodney Lyn, Lia C. Scott, Kevin M. Maloney, and Richard Rothenberg. 2022. "The Relationship between Health Literacy and COVID-19 Vaccination Prevalence during a Rapidly Evolving Pandemic and Infodemic" Vaccines 10, no. 12: 1989. https://doi.org/10.3390/vaccines10121989
APA StyleFeinberg, I., Scott, J. Y., Holland, D. P., Lyn, R., Scott, L. C., Maloney, K. M., & Rothenberg, R. (2022). The Relationship between Health Literacy and COVID-19 Vaccination Prevalence during a Rapidly Evolving Pandemic and Infodemic. Vaccines, 10(12), 1989. https://doi.org/10.3390/vaccines10121989








