Understanding Influenza and SARS-CoV-2 Vaccine Hesitancy in Racial and Ethnic Minority Caregivers
Abstract
1. Introduction
2. Materials and Methods
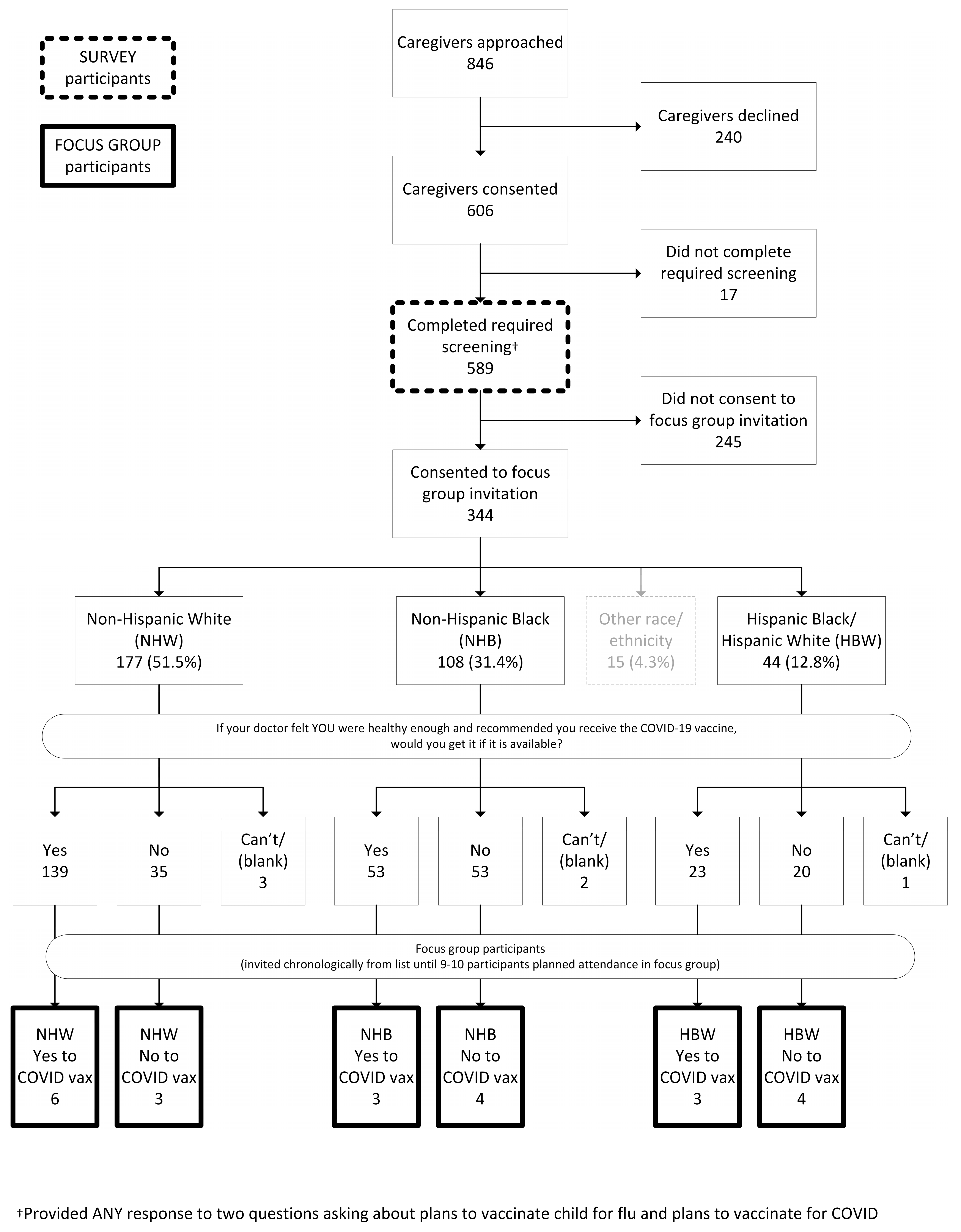
2.1. Part 1: Survey Population and Recruitment
2.1.1. Survey Data Collection Form Development and Validation
2.1.2. Survey Analysis
2.2. Part 2: Focus Group Population and Recruitment
2.2.1. Focus Group Guide Development, Validation, and Facilitation
2.2.2. Focus Group Thematic Content Analysis
3. Results
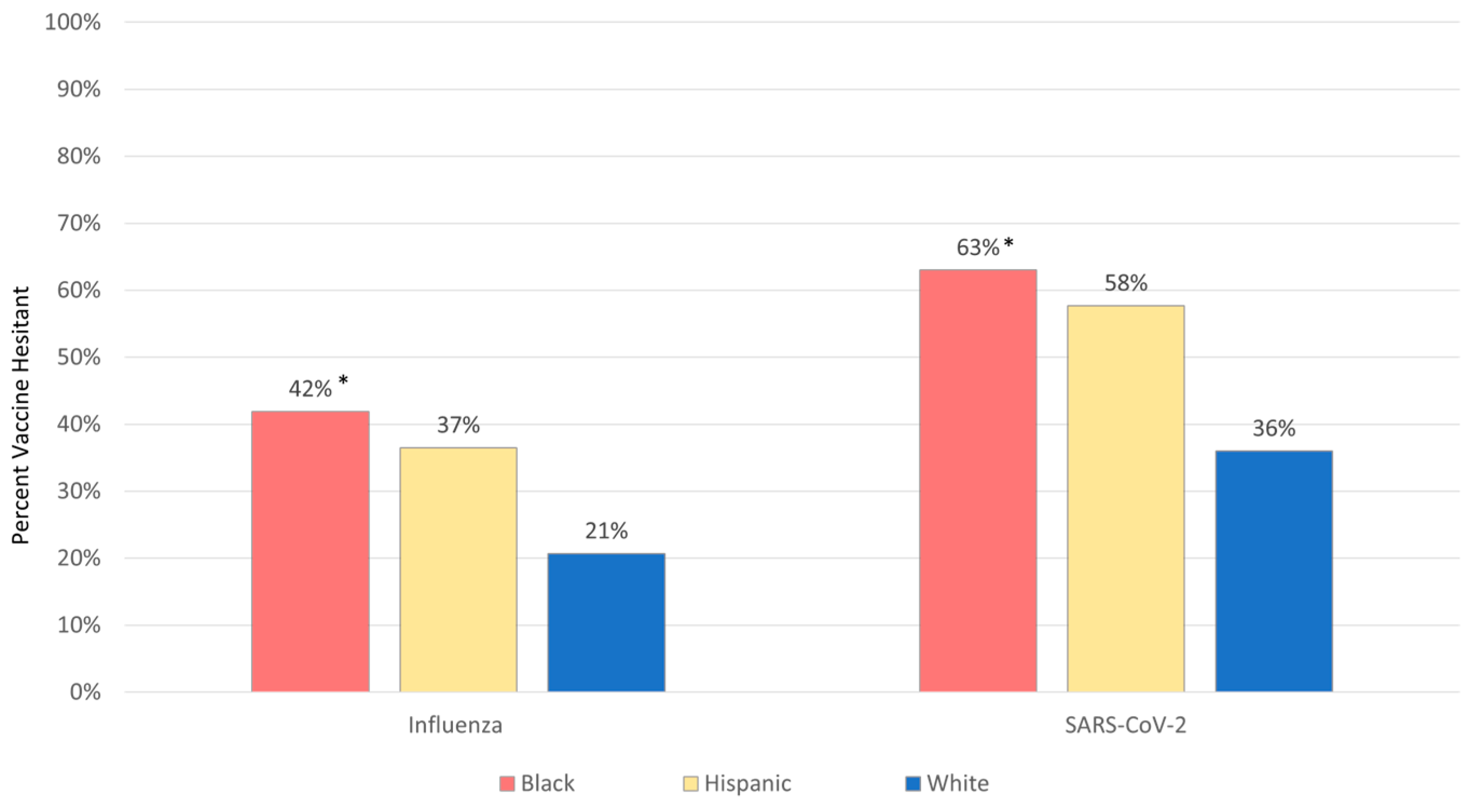
3.1. Survey
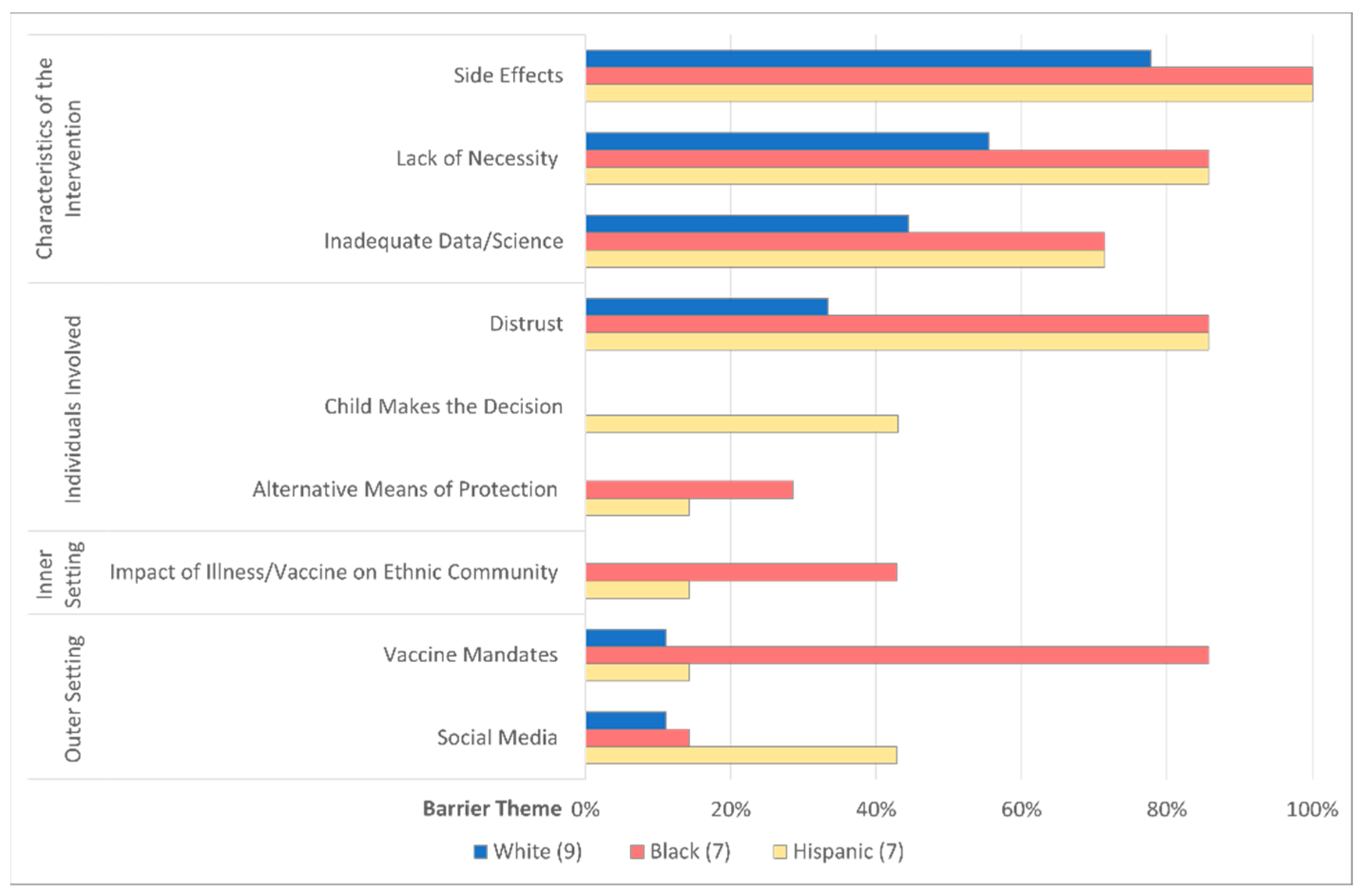
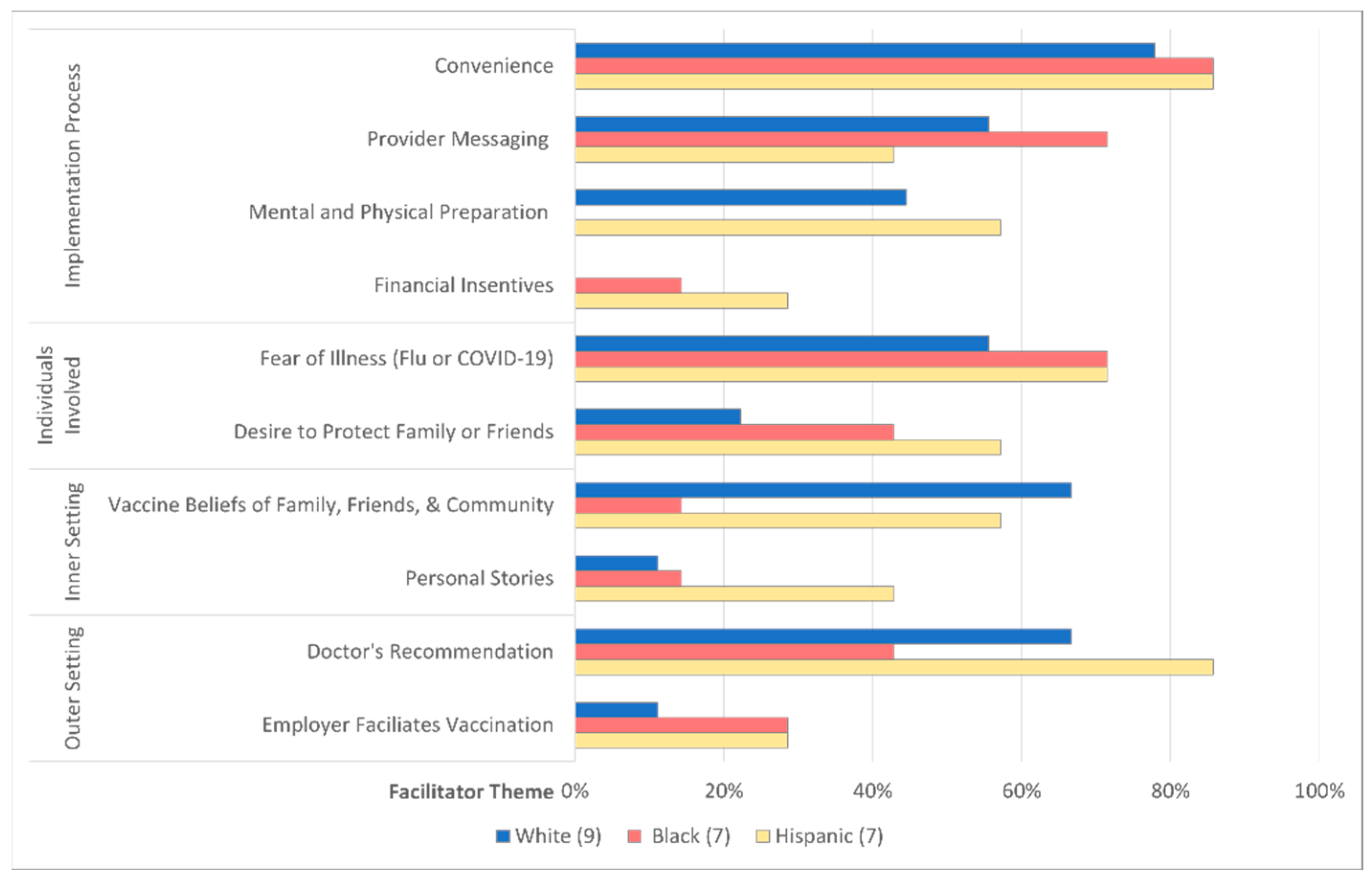
3.2. Focus Group
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Effect | Estimate | 95% Confidence Limits | p-Value | |
|---|---|---|---|---|
| Race | 0.0566 | |||
| Hispanic Black or White vs. Non-Hispanic White | 0.649 | 0.329 | 1.280 | 0.2125 |
| More than one race, regardless of Ethnicity vs. Non-Hispanic White | 0.319 | 0.132 | 0.771 | 0.0111 |
| Non-Hispanic Black vs. Non-Hispanic White | 0.547 | 0.332 | 0.902 | 0.0181 |
| Other race vs. Non-Hispanic White | 0.647 | 0.223 | 1.880 | 0.4240 |
| Insurance | 0.0024 | |||
| No insurance or Unsure vs. Private or Commercial Insurance | 0.509 | 0.106 | 2.444 | 0.3986 |
| Public Insurance (CHIP, Badger care, Medicaid, Medicare) vs. Private or Commercial Insurance | 0.446 | 0.283 | 0.704 | 0.0005 |
| Effect | Odds Ratio | 95% Confidence Limits | p-Value | |
|---|---|---|---|---|
| Race | 0.0529 | |||
| Hispanic Black or White vs. Non-Hispanic White | 0.633 | 0.307 | 1.304 | 0.2150 |
| More than one race, regardless of Ethnicity vs. Non-Hispanic White | 0.833 | 0.294 | 2.355 | 0.7302 |
| Non-Hispanic Black vs. Non-Hispanic White | 0.513 | 0.301 | 0.874 | 0.0141 |
| Other race vs. Non-Hispanic White | 2.049 | 0.652 | 6.442 | 0.2195 |
| Age | 0.0002 | |||
| 18–25 vs. 46+ | 0.219 | 0.089 | 0.543 | 0.0010 |
| 26–35 vs. 46+ | 0.240 | 0.120 | 0.481 | <0.0001 |
| 36–45 vs. 46+ | 0.452 | 0.228 | 0.894 | 0.0226 |
| Insurance | 0.0176 | |||
| No insurance or Unsure vs. Private or Commercial Insurance | 0.255 | 0.035 | 1.864 | 0.1782 |
| Public Insurance (CHIP, Badger care, Medicaid, Medicare) vs. Private or Commercial Insurance | 0.511 | 0.313 | 0.833 | 0.0071 |
| COVID Risk | 1.697 | 1.468 | 1.962 | <0.0001 |
| Focus Group | Parent ID | Race/ Ethnicity | Parent Intent to Receive COVID-19 | Prior Parent Influenza | Intent to Vaccinate Child for Flu | Intent to Vaccinate Child for COVID-19 | Gender | Age | Education | Insurance |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | Non-Hispanic White | Definitely Yes | Yes | Definitely Yes | Definitely Yes | Female | 46–55 | Graduate/ Professional degree | Private/ Commercial |
| 2 | 36–45 | |||||||||
| 3 | Some college/ College degree | |||||||||
| 4 | Probably Yes | Male | 55+ | |||||||
| 5 | Probably Yes | Probably Yes | 26–35 | |||||||
| 6 | No | Definitely no | Female | 36–45 | ||||||
| 2 | 7 | Non-Hispanic White | Definitely no | Yes | Probably yes | Definitely no | Female | 36–45 | Some college/ College degree | Public |
| 8 | No | 26–35 | Private/ Commercial | |||||||
| 9 | Yes | Male | ||||||||
| 3 | 10 | Non-Hispanic Black | Definitely yes | Yes | Probably yes | Unsure | Female | 36–45 | Some college/ College degree | Private/Commercial |
| 11 | Probably yes | Definitely yes | Definitely yes | 26–35 | Some high school | Public | ||||
| 12 | Probably no | Probably no | Some college/ College degree | Private/Commercial | ||||||
| 4 | 13 | Non-Hispanic Black | Unsure | Yes | Probably yes | Unsure | Female | 26–35 | No high school | Public |
| 14 | Definitely no | No | Definitely no | 18–25 | Some college/ College degree | |||||
| 15 | Definitely no | 36–45 | ||||||||
| 16 | 26–35 | Some high school | ||||||||
| 5 | 17 | Hispanic White | Definitely yes | Yes | Definitely yes | Definitely yes | Female | 18–25 | Some high school | Public |
| 18 | No | Probably no | Probably yes | 36–45 | Graduate/ Professional degree | Private/Commercial | ||||
| 19 | Hispanic White/Black | Not answered | Yes | Probably yes | Probably no | 26–35 | Some college/ College degree | Public | ||
| 6 | 20 | Hispanic Black | Unsure | No | Unsure | Probably no | Female | 26–35 | Some high school | Public |
| 21 | Hispanic White | Definitely no | Probably no | Definitely no | Some college/ College degree | |||||
| 22 | Definitely yes | Probably yes | Definitely yes | 36–45 | Some high school | Private/Commercial | ||||
| 23 | Unsure | Yes | Unsure | Unsure | 26–35 | Some college/ College degree | Public |
| CFIR Domain/Theme | Description of Facilitator | Supporting Quote | Distribution of Themes |
|---|---|---|---|
| Characteristics of the Intervention | |||
| Side Effects | Concern about prior vaccine tolerance including short-term and long-term side effects of vaccines was expressed. | “I find it really concerning…the amount of adverse reactions that are reported in VAERS are like disproportionate to flu vaccine… there’s enough young men that have had heart issues related to it, seems like a very real concern for me to have a couple of young boys. I don’t know how it’s going to affect them. It’s very unproven technology.” (W, anti) | 6FG, (2W, 2B, 2H) |
| Lack of Necessity | A perception that the vaccine is unnecessary due to a lack of vaccine effectiveness at preventing illness, a low perceived severity of influenza or COVID-19 illness, or a low risk for illness due to low risk past medical history, occupation, or home/school environment. | “I don’t think it’s important…to get the children vaccinated with the COVID vaccine right now… Maybe if we had more evidence that children are getting COVID like adults were getting COVID, but adults were dropping dead from COVID, children are not. (B, pro) | 6 FG, (2W, 2B, 2H) |
| Inadequate Data/ Science | The lack of available information regarding the facts behind vaccine development including length of time and number of people in whom vaccines have been tested. Vaccine novelty, rushed development process, and a lack of adequate follow-up time to assess for side effects were also included in this theme. | “I’m not getting my kids vaccinated because this vaccination shot came about so fast. It almost takes about 10 years to make an actual vaccination shot, so how did they make one in nine months? You’re not giving us enough information, y’all just want us to get this shot and be okay with that.” (B, anti) | 6 FG, (2W, 2B, 2H) |
| Individuals Involved in the Intervention | |||
| Distrust | Caregiver distrust that vaccines have been developed in a safe and efficacious manner. Specifically, concerns were raised that children should not be treated as “test subjects”, the science used to develop the vaccine was not sound, the provider recommending the vaccine was withholding information or lacks sufficient knowledge of vaccine, or that CDC and US government were promoting vaccines for personal gain or other nefarious reasons. | “I don’t know what goes into the vaccine, but…I’ve looked into it and it’s a bunch of words I can’t pronounce. …I’ll be honest…I don’t really necessarily trust that, and you know, right now pharmaceutical companies (don’t) have the people’s best interests at heart…I feel like it’s more of a money thing than keeping the public safe.” (H, anti) | 5 FG, (1W, 2B, 2H) |
| Child Makes the Decision | Most notably in Hispanics, parent deferred to the child to decide whether to obtain the vaccine. | “I really leave it up to my 16, almost 17yo. I left it up to her whether she wanted to take it, and she refused and she didn’t want to because she was scared of the things that she’s seen on the news.” (H, anti) | 2 FG (2H) |
| Alternative Means of Protection | Some families utilized social distancing, masking, and hand hygiene to protect against illness and believed vaccines were not necessary. | “I’m still on the fence about it because…I feel healthy. I practice, you know, the safe guidelines of masking up when it’s required and necessary. So I’m still not convinced that I should, or that I even want to [get the shot].” (H, anti) | 4 FG (2B, 2H) |
| Inner Setting | |||
| Impact of Illness/ Vaccine on Ethnic Community | Most notably in Blacks and Hispanics, the effects of influenza or COVID-19 illness or vaccinations on their specific communities, as well as concerns about how their community has historically been treated or impacted by the medical community. | “We’re the community that’s being affected the most by COVID. The people are dying the most by COVID. We’re not the ones trying to jump in the forefront and be those people that could potentially end up getting killed by this vaccine.” (B, pro) | 3 FG (2B, 1H) |
| Outer Setting | |||
| Vaccine Mandates | Requirements to obtain vaccine for school, employment, or other reasons as well as the right of the parent to choose if child should be vaccinated. Most parents believe parent should have the right to determine if child got vaccinated, but many reported they would only get the vaccine if mandated. | “If people have a choice, they’re more comfortable with choosing your own, versus being forced. I think that’s why a lot of people haven’t got the COVID vaccine ‘cause they’re not comfortable because they feel like, oh they want to force me or change me or make me do something I don’t want to do.” (B, pro) | 4 FG (1W, 2B, 1H) |
| Social media | Social media and news portrayal of vaccines. | “You hear all these horrific stories about people that have had the vaccine and they end up dying right after the vaccine. And all the news doesn’t help the situation, you know, persuade people that are trying to get vaccinated. It’s all about the media, too…it scares people.” (H, anti) | 4 FG (1W, 1B, 2H) |
| CFIR Domain/Theme | Description of Facilitator | Supporting Quote | Distribution of Theme |
|---|---|---|---|
| Implementation Process | |||
| Convenience | Ease of obtaining a vaccine, via providing vaccines at common locations, a variety of flexible appointment times around school and work schedules and facilitating dose 2 scheduling for SARS-CoV-2. | “I think when they rolled out, for COVID vaccine, they made it so convenient for people to get vaccinated. I didn’t find it hard to get vaccinated for COVID at all as an adult. Maybe if…the time [comes] and it’s acceptable for children to get it, at the doctor’s office, make it as easy for us to get our kids vaccinated as you did adults.” (B, pro) | 6 FG, (2W, 2B, 2H) |
| Provider Messaging | How and what providers communicate to families to promote vaccines. Parents prefer a neutral tone, that is sensitive to the parent/child’s culture and avoids pro-vaccine bias. Parents desire transparent messaging with data on the benefits, side effects, and long-term risks of vaccines. | “If they can explain to me more about, like, what’s in these shots. Like, what’s the medicine, what’s the outcome of the medicine. …And not just the good, I [want to] hear the bad too.” (B, anti) | 5 FG, (2W, 2B, 1H) |
| Mental and Physical Preparation | The process of preparing for vaccination, this includes mentally reviewing vaccine information, making a decision prior to being offered, and emotionally preparing the child for vaccination. Physically, parents prepared supplies (acetaminophen and electrolyte fluids) to address side effects and scheduled time off from work. | “Now we mentally prepare and we’re like, “Okay, we’re going to the pediatrician, we’re getting these shots. Let’s all take a deep breath. Like let’s get takeout for dinner, right? Like we plan to take care of ourselves. And one of our kiddos is prone to getting like a spiking of fever. So, we…know that now and we’re ready with the medicines.”(W, pro) | 5FG, (2W, 1B, 2H) |
| Financial Incentives | Offering stipends or gift cards to receive vaccine or making vaccines free of charge. | “I feel like if they were to get, like, 10% off Target gift card if they got their flu shot at CVS pharmacy or whatnot, like, I feel like that would kind of…help persuade people.” (H, anti) | 2 FG (1B, 1H) |
| Individuals Involved in the Intervention | |||
| Fear of Illness (Flu or COVID-19) | A concern about becoming ill from virus as well as a desire to be protected from illness. | “…It’s just been a really, really crazy high number of deaths with it. So that scares all of us and…that puts perspective that you might have a better chance of life with the vaccine.” (H, pro) | 6 FG, (2W, 2B, 2H) |
| Desire to Protect Family, Friends, & Community | Desire to obtain vaccine to prevent illness transmission to high-risk family members, friends, or other community members. | “I got it [vaccine] for myself because my parents are older, and they were completely terrified. We spent the past year and a half away from them. …They would not let us in the house, and we were a very close family, so that was extremely hard. So, I kind of balanced it out—like, let me take this risk for them. They got the vaccine. I’ll take the vaccine for them.” (W, anti) | 6FG, (2W, 2B, 2H) |
| Inner Setting | |||
| Vaccine Beliefs of Family, Friends, & Community | The impact of family, friends, or the local community’s vaccination status & vaccine beliefs on the caregiver’s decision to vaccinate. | “Everybody in my extended family is vaccinated. My sister …she’s a social worker in a dialysis clinic…And so she was like the first in line to get vaccinated along with other healthcare workers. So yeah, we’re all vaccinated. I would definitely plan to vaccinate the kiddos once they’re able to be.” (W, pro) | 5FG, (2W, 1B, 2H) |
| Personal Stories | Personal experiences of self or others with illness or vaccine that affected caregiver decision-making around vaccines. | “When my nephew was born, he was a month old and he had Influenza B, and…we almost lost him. So, I’m very pro getting the flu shot.” (H, anti) | 4 FG (1W, 1B, 2H) |
| Outer Setting | |||
| Doctor’s Recommendation | A positive recommendation for vaccination from the child’s primary physician. | “We always trust our doctor’s suggestions. So even like, you know, with the COVID vaccine for myself and my two older kids who are eligible…if my doctor recommends it versus if she doesn’t, that’s our big decision maker.” (W, pro) | 5FG, (2W, 1B, 2H) |
| Employer Facilitates Vaccination | Employers provides caregivers time off or compensation for getting their child vaccinated. | “Jobs provide time for parents to take off to go get their children vaccinated and you pay them for it.” B, pro) | 4FG (1W, 1B, 2H) |
References
- Goyal, M.K.; Simpson, J.N.; Boyle, M.D.; Badolato, G.M.; Delaney, M.; McCarter, R.; Cora-Bramble, D. Racial and/or Ethnic and Socioeconomic Disparities of SARS-CoV-2 Infection among Children. Pediatrics 2020, 146, 2020009951. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.H.; Kepler, K.L.; Geevarughese, A.; Paneth-Pollak, R.; Dorsinville, M.S.; Ngai, S.; Reilly, K.H. Race/Ethnicity among Children with COVID-19-Associated Multisystem Inflammatory Syndrome. JAMA Netw. Open 2020, 3, e2030280. [Google Scholar] [CrossRef] [PubMed]
- Disparities in COVID-19 Associated Hospitalizations. Online Centers for Disease Control and Prevention Updated 30 December 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-hospitalization.html (accessed on 14 January 2022).
- O’Halloran, A.C.; Holstein, R.; Cummings, C.; Kirley, P.D.; Alden, N.B.; Yousey-Hindes, K.; Anderson, E.J.; Ryan, P.; Kim, S.; Lynfield, R.; et al. Rates of Influenza-Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death by Race and Ethnicity in the United States from 2009 to 2019. JAMA Netw. Open 2021, 4, e2121880. [Google Scholar] [CrossRef] [PubMed]
- Flu Vaccination Coverage, United States, 2020–2021 Influenza Season. FluVax. 2021. Available online: https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm (accessed on 9 June 2022).
- Alfieri, N.L.; Kusma, J.D.; Heard-Garris, N.; Davis, M.M.; Golbeck, E.; Barrera, L.; Macy, M.L. Parental COVID-19 Vaccine Hesitancy for Children: Vulnerability in an Urban Hotspot. BMC Public Health 2021, 21, 1662. [Google Scholar] [CrossRef]
- Szilagyi, P.G.; Shah, M.D.; Delgado, J.R.; Thomas, K.; Vizueta, N.; Cui, Y.; Vangala, S.; Shetgiri, R.; Kapteyn, A. Parents’ Intentions and Perceptions about COVID-19 Vaccination for Their Children: Results from a National Survey. Pediatrics 2021, 148, e2021052335. [Google Scholar] [CrossRef]
- Ten Threats to Global Health 2019. World Health Organization. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 24 April 2020).
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 Vaccine Accetance in the US. Lancet 2020, 26, 100495. [Google Scholar] [CrossRef]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L.; et al. Caregiver Willingness to Vaccinate their Children against COVID-19: Cross Sectional Survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Lin, J.S.; Hoffman, L.; Bean, S.I.; O’Connor, E.A.; Martin, A.M.; Iacocca, M.O.; Bacon, O.P.; Davies, M.C. Addressing Racism in Preventive Services: Methods Report to Support the US Preventive Services Task Force. JAMA 2021, 326, 2412–2420. [Google Scholar] [CrossRef]
- Bhat-Schelbert, K.; Lin, C.J.; Matambanadzo, A.; Hannibal, K.; Nowalk, M.P.; Zimmerman, R.K. Barriers to and Facilitators of Child Influenza Vaccine—Perspectives from Parents, Teens, Marketing and Healthcare professionals. Vaccine 2012, 30, 2448–2452. [Google Scholar] [CrossRef] [PubMed]
- Escoffery, C.; Riehman, K.; Watson, L.; Priess, A.S.; Borne, M.F.; Halpin, S.N.; Rhiness, C.; Wiggins, E.; Kegler, M.C. Facilitators and Barriers to the Implementation of the HPV VACs (Vaccinate Adolescents against Cancers) Program: A Consolidated Framework for Implementation Research Analysis. Prev. Chronic Dis. 2019, 16, E85. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering Implementation of Health Services Research Findings into Practice: A Consolidated Framework for Advancing Implementation Science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Krupik, D.; Ali, S.; Mater, A.; Hall, J.E.; Bone, J.N.; Thompson, G.C.; Yen, K.; Griffiths, M.A.; Klein, A.; et al. Caregiver Willingness to Vaccinate Their Children against COVID-19 after Adult Vaccine Approval. Int. J. Environ. Res. Public Health 2021, 18, 10224. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Kaitelidou, D. Willingness, Refusal and Influential Factors of Parents to Vaccinate their Children against the COVID-19: A Systematic Review and Meta-analysis. Prev. Med. 2022, 157, 106994. [Google Scholar] [CrossRef]
- Hamel, L.; Lopes, L.; Kearney, A.; Stokes, M.; Kirzinger, A.; Sparks, G.; Brodie, M. KFF COVID-19 Vaccine Monitor: Winter 2021 Update on Parent’s Views of Vaccine for Kids 2021. KFF COVID-19 Vaccine Monitor. Available online: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-winter-2021-update-on-parents-views-of-vaccines/ (accessed on 9 December 2021).
- Gagneur, A. Motivational Interviewing: A Powerful Tool to Address Vaccine Hesitancy. Can. Commun. Dis. Rep. 2020, 46, 93–97. [Google Scholar] [CrossRef]
- Waisbord, S.L.; Larson, H. Why Invest in Communication for Immunization: Evidence and Lessons Learned. 2005. Available online: https://www.semanticscholar.org/paper/Why-invest-in-communication-for-immunization-and-Waisbord-Hj/e81435a2eb842a4a8cd36793674a0f162db20d99 (accessed on 9 December 2021).
- Chin, J.; Zhou, Y.; Chen, C.L.; Lomiguen, C.M.; McClelland, S.; Lee-Wong, M. Influenza Vaccination Quality Improvement as a Model for COVID-19 Prophylaxis. Cureus 2021, 13, e12549. [Google Scholar] [CrossRef]
- Oku, A.; Oyo-Ita, A.; Glenton, C.; Fretheim, A.; Ames, H.; Muloliwa, A.; Kaufman, J.; Hill, S.; Cliff, J.; Cartier, Y.; et al. Perceptions and Experiences of Childhood Vaccination Communication Strategies among Caregivers and Health Workers in Nigeria: A qualitative study. PLoS ONE 2017, 12, e0186733. [Google Scholar] [CrossRef]
- Khubchandani, J.; Macias, Y. COVID-19 Vaccination Hesitancy in Hispanics and African-Americans: A Review and Recommendations for Practice. Brain Behav. Immun. Health 2021, 15, 100277. [Google Scholar] [CrossRef]
- Baumer-Mouradian, S.H.; Servi, A.; Kleinschmidt, A.; Nimmer, M.; Lazarevic, K.; Hanson, T.; Jastrow, J.; Jaworski, B.; Kopetsky, M.; Drendel, A.L. Vaccinating in the Emergency Department, a Model to Overcome Influenza Vaccine Hesitancy. Pediatr. Qual. Saf. 2021, 6, e430. [Google Scholar] [CrossRef]
- Baumer-Mouradian, S.H.; Kleinschmidt, A.; Servi, A.; Jaworski, B.; Lazarevic, K.; Kopetsky, M.; Nimmer, M.; Hanson, T.; Gray, M.P.; Drendel, A.L. Vaccinating in the Emergency Department, a Novel Approach to Improve Influenza Vaccination Rates via a Quality Improvement Initiative. Pediatr. Qual. Saf. 2020, 5, e322. [Google Scholar] [CrossRef] [PubMed]
- Hart, R.J.; Paul, R.I.; Levine, A.; Sikes, K.; Bryant, K.; Stevenson, M.D. Parent Intent and Willingness to Immunize Children Against Influenza in the Pediatric Emergency Department. Pediatr. Emerg. Care 2019, 35, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Crain, E.F. The Role of the Emergency Department in Primary Care. Pediatr. Emerg. Care 1992, 8, 98–104. [Google Scholar] [CrossRef]
- Hetherington, E.; Edwards, S.A.; MacDonald, S.E.; Racine, N.; Madigan, S.; McDonald, S.; Tough, S. SARS-CoV-2 Vaccination Intentions among Mothers of Children aged 9 to 12 years: A Survey of the All Our Families Cohort. CMAJ Open 2021, 9, e548–e555. [Google Scholar] [CrossRef] [PubMed]
- Kempe, A.; Saville, A.W.; Albertin, C.; Zimet, G.; Breck, A.; Helmkamp, L.; Vangala, S.; Dickinson, L.M.; Rand, C.; Humiston, S.; et al. Parental Hesitancy about Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics 2020, 146, e20193852. [Google Scholar] [CrossRef]
- Suran, M. Why Parents Still Hesitate to Vaccinate Their Children against COVID-19. JAMA 2022, 327, 23–25. [Google Scholar] [CrossRef]
- Peng, J.; Marquez, C.; Rubio, L.; Chamie, G.; Jones, D.; Jacobo, J.; Rojas, S.; Rojas, S.; Tulier-Laiwa, V.; Black, D.; et al. High Likelihood of Accepting COVID-19 Vaccine in a Latinx Community at High SARS-CoV-2 Risk in San Francisco. Open Forum Infect. Dis. 2021, 8, ofab202. [Google Scholar] [CrossRef]
- Kricorian, K.; Turner, K. COVID-19 Vaccine Acceptance and Beliefs among Black and Hispanic Americans. PLoS ONE 2021, 16, e0256122. [Google Scholar] [CrossRef]
- Baumer-Mouradian, S.H.; Hart, R.J.; Bone, J.N.; Seiler, M.; Olson, P.; Keitel, K.; Manzano, S.; Gualco, G.; Krupik, D.; Schroter, S.; et al. Should COVID-19 Vaccines be Mandated in Schools?—An International Caregiver Perspective. Vaccine 2022, 40, 5384–5390. [Google Scholar] [CrossRef]
| Variables | Total n = 589 (col %) |
|---|---|
| Parent Gender | |
| Male | 101 (17.1) |
| Female | 468 (79.5) |
| Other | 2 (0.3) |
| Missing | 18 (3.1) |
| Parent Age | |
| 18–25 | 60 (10.2) |
| 26–35 | 209 (35.5) |
| 36–45 | 222 (37.7) |
| 46+ | 81 (13.8) |
| Missing | 17 (2.8) |
| Parent Education | |
| No high school | 15 (2.6) |
| Some high school/High school diploma/GED | 138 (23.4) |
| Some college/College degree | 277 (47.0) |
| Graduate/Professional degree | 141 (23.9) |
| Missing | 18 (3.1) |
| Parent Race and Ethnicity | |
| Non-Hispanic White | 277 (47.0) |
| Non-Hispanic Black | 148 (25.1) |
| Hispanic Black or Hispanic White | 52 (8.8) |
| More than one race, regardless of Ethnicity | 26 (4.4) |
| Other race | 18 (3.1) |
| Missing | 68 (11.6) |
| Parent Insurance | |
| Private or Commercial Insurance | 293 (49.8) |
| Public Insurance (CHIP, Badger care, Medicaid, Medicare) | 268 (45.5) |
| No insurance or Unsure | 9 (1.5) |
| Missing | 19 (3.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baumer-Mouradian, S.H.; Hart, R.J.; Visotcky, A.; Fraser, R.; Prasad, S.; Levas, M.; Nimmer, M.; Brousseau, D.C. Understanding Influenza and SARS-CoV-2 Vaccine Hesitancy in Racial and Ethnic Minority Caregivers. Vaccines 2022, 10, 1968. https://doi.org/10.3390/vaccines10111968
Baumer-Mouradian SH, Hart RJ, Visotcky A, Fraser R, Prasad S, Levas M, Nimmer M, Brousseau DC. Understanding Influenza and SARS-CoV-2 Vaccine Hesitancy in Racial and Ethnic Minority Caregivers. Vaccines. 2022; 10(11):1968. https://doi.org/10.3390/vaccines10111968
Chicago/Turabian StyleBaumer-Mouradian, Shannon H., Rebecca J. Hart, Alexis Visotcky, Raphael Fraser, Swathi Prasad, Michael Levas, Mark Nimmer, and David C. Brousseau. 2022. "Understanding Influenza and SARS-CoV-2 Vaccine Hesitancy in Racial and Ethnic Minority Caregivers" Vaccines 10, no. 11: 1968. https://doi.org/10.3390/vaccines10111968
APA StyleBaumer-Mouradian, S. H., Hart, R. J., Visotcky, A., Fraser, R., Prasad, S., Levas, M., Nimmer, M., & Brousseau, D. C. (2022). Understanding Influenza and SARS-CoV-2 Vaccine Hesitancy in Racial and Ethnic Minority Caregivers. Vaccines, 10(11), 1968. https://doi.org/10.3390/vaccines10111968





