Seroprevalence of Varicella-Zoster Virus and Measles among Healthcare Workers in a Tertiary Medical Center in Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Changes in New Employee Medical Checkups
2.3. Evaluation of the Serostatus
2.4. Statistical Analysis
3. Results
3.1. Study Population
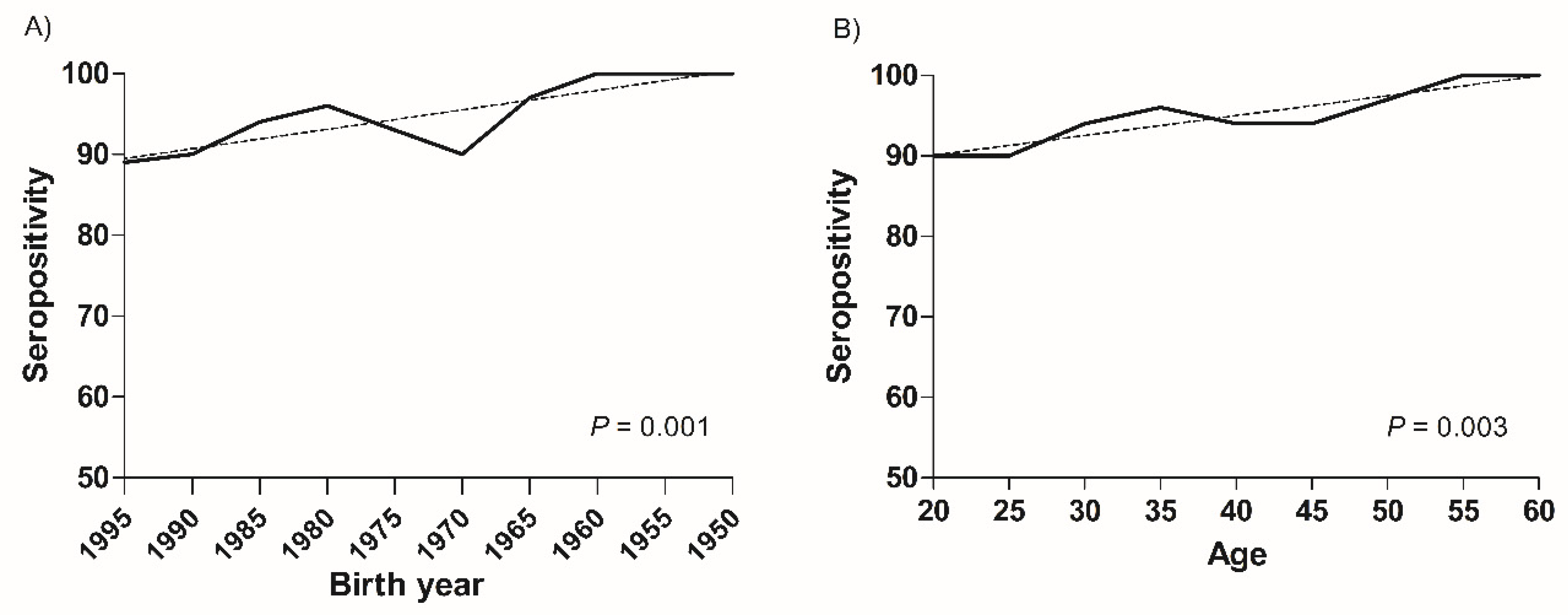
3.2. Seroprevalence of VZV
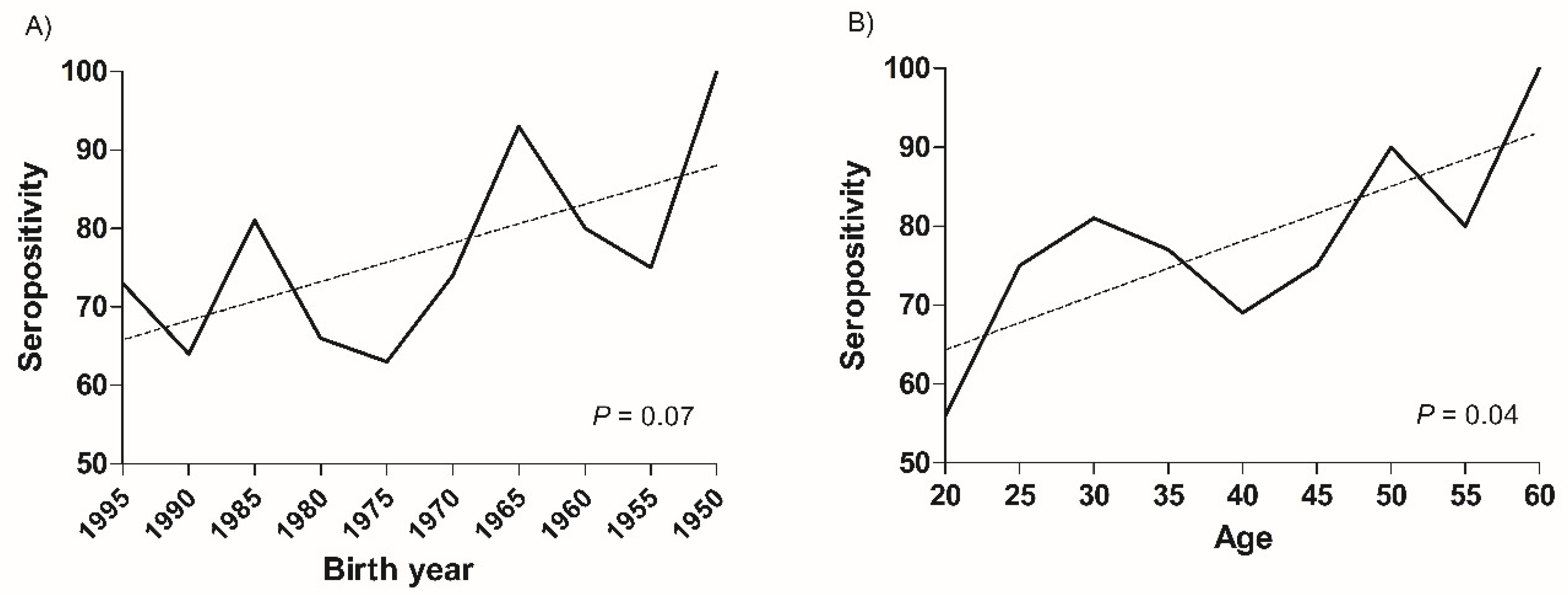
3.3. Seroprevalence of Measles
3.4. Seroprevalence of Measles and VZV According to Occupational Group
3.5. Trends of Seroprevalence of Varicella-Zoster and Measles
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Lo Presti, C.; Curti, C.; Montana, M.; Bornet, C.; Vanelle, P. Chickenpox: An update. Med. Mal. Infect. 2019, 49, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hübschen, J.M.; Gouandjika-Vasilache, I.; Dina, J. Measles. Lancet 2022, 399, 678–690. [Google Scholar] [CrossRef]
- Guerra, F.M.; Bolotin, S.; Lim, G.; Heffernan, J.; Deeks, S.L.; Li, Y.; Crowcroft, N.S. The basic reproduction number (R0) of measles: A systematic review. Lancet Infect. Dis. 2017, 17, e420–e428. [Google Scholar] [CrossRef]
- Marangi, L.; Mirinaviciute, G.; Flem, E.; Scalia Tomba, G.; Guzzetta, G.; Freiesleben de Blasio, B.; Manfredi, P. The natural history of varicella zoster virus infection in Norway: Further insights on exogenous boosting and progressive immunity to herpes zoster. PLoS ONE 2017, 12, e0176845. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.; Ray, P.; Tran, T.N.; Black, S.; Shinefield, H.R.; Coplan, P.M.; Lewis, E.; Fireman, B.; Saddier, P. Long-term effectiveness of varicella vaccine: A 14-Year, prospective cohort study. Pediatrics 2013, 131, e1389–e1396. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.K.; Goodson, J.L.; Alexander, J.P., Jr.; Kretsinger, K.; Sodha, S.V.; Steulet, C.; Gacic-Dobo, M.; Rota, P.A.; McFarland, J.; Menning, L.; et al. Progress toward regional measles elimination—Worldwide, 2000–2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1700–1705. [Google Scholar] [CrossRef]
- Hayman, D.T.S. Measles vaccination in an increasingly immunized and developed world. Hum. Vaccin. Immunother. 2019, 15, 28–33. [Google Scholar] [CrossRef]
- Varela, F.H.; Pinto, L.A.; Scotta, M.C. Global impact of varicella vaccination programs. Hum. Vaccin. Immunother. 2019, 15, 645–657. [Google Scholar] [CrossRef]
- Grose, C. Varicella vaccination of children in the United States: Assessment after the first decade 1995–2005. J. Clin. Virol. 2005, 33, 89–95; discussion 96–98. [Google Scholar] [CrossRef]
- Porter, A.; Goldfarb, J. Measles: A dangerous vaccine-preventable disease returns. Cleve. Clin. J. Med. 2019, 86, 393–398. [Google Scholar] [CrossRef]
- Kim, E.Y.; Jeong, S.Y.; Lee, G.H.; Song, J.; Lee, D.H. Characteristics of varicella outbreaks in Korea, 2018–2202. Public Health Wkly. Rep. 2021, 14, 652–663. [Google Scholar]
- Choi, S.; Cho, E.H. Analysis of the occurrence of measles in Korea, 2019. Public Health Wkly. Rep. 2020, 13, 2445–2458. [Google Scholar]
- Kang, H.J.; Han, Y.W.; Kim, S.J.; Kim, Y.J.; Kim, A.R.; Kim, J.A.; Jung, H.D.; Eom, H.E.; Park, O.; Kim, S.S. An increasing, potentially measles-susceptible population over time after vaccination in Korea. Vaccine 2017, 35, 4126–4132. [Google Scholar] [CrossRef] [PubMed]
- Han, S.B.; Park, S.H.; Yi, Y.; Ji, S.K.; Jang, S.H.; Park, M.H.; Lee, J.E.; Jeong, H.S.; Shin, S. Measles seroprevalence among healthcare workers in South Korea during the post-elimination period. Hum. Vaccin. Immunother. 2021, 17, 2517–2521. [Google Scholar] [CrossRef]
- Yoo, Y.; Park, W.J.; Cho, S.; Lim, D.Y.; Kim, S.; Kang, W.; Kim, H.; Moon, J.D. Seroprevalence of measles, mumps, rubella, and varicella-zoster antibodies in new female nurses in the Republic of Korea. Ann. Occup. Env. Med. 2021, 33, e19. [Google Scholar] [CrossRef]
- Jung, J.; Kim, S.K.; Kwak, S.H.; Hong, M.J.; Kim, S.H. Seroprevalence of Measles in Healthcare Workers in South Korea. Infect. Chemother. 2019, 51, 58–61. [Google Scholar] [CrossRef]
- Chang, H.H.; Kim, S.W.; Kwon, K.T.; Kim, H.I.; Kim, M.J.; Ryu, S.Y.; Kim, H.A.; Hur, J.; Kwon, H.H.; Hong, H.L. Preliminary report of seroprevalence of anti-measles immunoglobulin G among healthcare workers of 6 teaching hospitals of Daegu, Korea in 2019. Infect. Chemother. 2019, 51, 54–57. [Google Scholar] [CrossRef]
- Kwak, Y.G.; Song, J.E.; Oh, G.B.; Jeong, I.H.; Cho, C.R.; Kim, N.; Yoo, H.M.; Yoo, G.M.; Lee, M.J.; Kim, B.N. Comparison of the seroprevalence of measles antibodies among healthcare workers in two Korean hospitals in 2019. Infect. Chemother. 2020, 52, 93–97. [Google Scholar] [CrossRef]
- Song, K.; Lee, J.M.; Lee, E.J.; Lee, B.R.; Choi, J.Y.; Yun, J.; Lee, S.N.; Jang, M.Y.; Kim, H.W.; Kim, H.S.; et al. Control of a nosocomial measles outbreak among previously vaccinated adults in a population with high vaccine coverage: Korea, 2019. Eur. J. Clin. Microbiol. Infect. Dis. 2022, 41, 455–466. [Google Scholar] [CrossRef]
- Choe, Y.J.; Park, Y.J.; Kim, J.W.; Eom, H.E.; Park, O.; Oh, M.D.; Lee, J.K. An outbreak of measles in a university in Korea, 2014. J. Korean Med. Sci. 2017, 32, 1876–1878. [Google Scholar] [CrossRef]
- Lee, H.; Cho, H.K.; Kim, K.H. Seroepidemiology of varicella-zoster virus in Korea. J. Korean Med. Sci. 2013, 28, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.S.; Noh, J.Y.; Huh, J.Y.; Jo, Y.M.; Lee, J.; Song, J.Y.; Kim, W.J.; Cheong, H.J. Seroprevalence of varicella-zoster virus in Korea. J. Med. Virol. 2010, 82, 2123–2126. [Google Scholar] [CrossRef] [PubMed]
- Chris Maple, P.A.; Gunn, A.; Sellwood, J.; Brown, D.W.; Gray, J.J. Comparison of fifteen commercial assays for detecting Varicella Zoster virus IgG with reference to a time resolved fluorescence immunoassay (TRFIA) and the performance of two commercial assays for screening sera from immunocompromised individuals. J. Virol. Methods 2009, 155, 143–149. [Google Scholar] [CrossRef] [PubMed]
- de Ory, F.; Minguito, T.; Balfagon, P.; Sanz, J.C. Comparison of chemiluminescent immunoassay and ELISA for measles IgG and IgM. APMIS 2015, 123, 648–651. [Google Scholar] [CrossRef] [PubMed]
- Botelho-Nevers, E.; Gautret, P.; Biellik, R.; Brouqui, P. Nosocomial transmission of measles: An updated review. Vaccine 2012, 30, 3996–4001. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G. 2000~2001 result and lesson of the measles campaign for measles epidemic elimination. Korean J. Pediatr. Infect. Dis. 2001, 8, 280–284. [Google Scholar] [CrossRef]
- Infectious Diseases Homepage. Available online: https://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaView.do?pblctDtaSeAt=8&pblctDtaSn=2039 (accessed on 20 October 2022).
- Choi, J.K.; Park, S.H.; Park, S.; Choi, S.M.; Kim, S.H.; Lee, D.G.; Yoo, J.H.; Choi, J.H.; Kang, J.H. Trends in varicella and herpes zoster epidemiology before and after the implementation of universal one-dose varicella vaccination over one decade in South Korea, 2003–2015. Hum. Vaccin. Immunother. 2019, 15, 2554–2560. [Google Scholar] [CrossRef]
- Lee, Y.H.; Choe, Y.J.; Cho, S.I.; Bang, J.H.; Oh, M.D.; Lee, J.K. Increasing varicella incidence rates among children in the Republic of Korea: An age-period-cohort analysis. Epidemiol. Infect. 2019, 147, e245. [Google Scholar] [CrossRef]
- Infectious Diseases Homepage. Available online: https://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaView.do?pblctDtaSeAt=1&pblctDtaSn=2682 (accessed on 20 October 2022).
- Suzuki, A.; Nishiura, H. Transmission dynamics of varicella before, during and after the COVID-19 pandemic in Japan: A modelling study. Math. Biosci. Eng. 2022, 19, 5998–6012. [Google Scholar] [CrossRef]
- Thakur, M.; Zhou, R.; Mohan, M.; Marathe, A.; Chen, J.; Hoops, S.; Machi, D.; Lewis, B.; Vullikanti, A. COVID’s collateral damage: Likelihood of measles resurgence in the United States. BMC Infect. Dis. 2022, 22, 743. [Google Scholar] [CrossRef]
- Kang, J.H.; Park, Y.S.; Park, S.Y.; Kim, S.B.; Ko, K.P.; Seo, Y.H. Varicella seroprevalence among health care workers in Korea: Validity of self-reported history and cost-effectiveness of prevaccination screening. Am. J. Infect. Control 2014, 42, 885–887. [Google Scholar] [CrossRef] [PubMed]
- Fatha, N.; Ang, L.W.; Goh, K.T. Changing seroprevalence of varicella zoster virus infection in a tropical city state, Singapore. Int. J. Infect. Dis. 2014, 22, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Kumakura, S.; Shibata, H.; Onoda, K.; Nishimura, N.; Matsuda, C.; Hirose, M. Seroprevalence survey on measles, mumps, rubella and varicella antibodies in healthcare workers in Japan: Sex, age, occupational-related differences and vaccine efficacy. Epidemiol. Infect. 2014, 142, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Koivisto, K.; Puhakka, L.; Lappalainen, M.; Blomqvist, S.; Saxen, H.; Nieminen, T. Immunity against vaccine-preventable diseases in Finnish pediatric healthcare workers in 2015. Vaccine 2017, 35, 1608–1614. [Google Scholar] [CrossRef] [PubMed]
- von Linstow, M.L.; Yde Nielsen, A.; Kirkby, N.; Eltvedt, A.; Nordmann Winther, T.; Bybeck Nielsen, A.; Bang, D.; Poulsen, A. Immunity to vaccine-preventable diseases among paediatric healthcare workers in Denmark, 2019. Eurosurveillance 2021, 26, 2001167. [Google Scholar] [CrossRef]
- Plans-Rubio, P. Evaluation of the establishment of herd immunity in the population by means of serological surveys and vaccination coverage. Hum. Vaccin. Immunother. 2012, 8, 184–188. [Google Scholar] [CrossRef]
- Kim, Y.; Hwang, J.Y.; Lee, K.M.; Lee, E.; Park, H. Cross-sectional study of varicella zoster virus immunity in healthy Korean children assessed by glycoprotein enzyme-linked immunosorbent assay and fluorescent antibody to membrane antigen test. Vaccines 2021, 9, 492. [Google Scholar] [CrossRef]
- Huang, W.C.; Huang, L.M.; Chang, I.S.; Tsai, F.Y.; Chang, L.Y. Varicella breakthrough infection and vaccine effectiveness in Taiwan. Vaccine 2011, 29, 2756–2760. [Google Scholar] [CrossRef]
- Pan, X.; Shu, M.; Ma, R.; Fang, T.; Dong, H.; Sun, Y.; Xu, G. Varicella breakthrough infection and effectiveness of 2-dose varicella vaccine in China. Vaccine 2018, 36, 5665–5670. [Google Scholar] [CrossRef]
- Bianchi, F.P.; Stefanizzi, P.; Trerotoli, P.; Tafuri, S. Sex and age as determinants of the seroprevalence of anti-measles IgG among European healthcare workers: A systematic review and meta-analysis. Vaccine 2022, 40, 3127–3141. [Google Scholar] [CrossRef]
- Kaaijk, P.; Nicolaie, M.A.; van Rooijen, D.; van Houten, M.A.; van der Klis, F.R.; Buisman, A.M.; van Binnendijk, R.S. Dynamics of the Antibody Response After a Third Dose of Measles-Mumps-Rubella Vaccine Indicate a Slower Decline Compared With a Second Dose. Open Forum Infect. Dis. 2020, 7, ofaa505. [Google Scholar] [CrossRef] [PubMed]
- Quach, H.Q.; Chen, J.; Monroe, J.M.; Ratishvili, T.; Warner, N.D.; Grill, D.E.; Haralambieva, I.H.; Ovsyannikova, I.G.; Poland, G.A.; Kennedy, R.B. The influence of sex, BMI, and age on cellular and humoral immune responses against measles after a 3rd dose of MMR vaccine. J. Infect. Dis. 2022, jiac351. [Google Scholar] [CrossRef] [PubMed]
- Kaaijk, P.; Wijmenga-Monsuur, A.J.; Ten Hulscher, H.I.; Kerkhof, J.; Smits, G.; Nicolaie, M.A.; van Houten, M.A.; van Binnendijk, R.S. Antibody levels at 3-years follow-up of a third dose of measles-mumps-rubella vaccine in young adults. Vaccines 2022, 10, 132. [Google Scholar] [CrossRef] [PubMed]
- Gorny, A.W.; Mittal, C.; Saw, S.; Venkatachalam, I.; Fisher, D.A.; Tambyah, P.A. Varicella seroprevalence in healthcare workers in a tertiary hospital: An audit of cross-sectional data. BMC Res. Notes 2015, 8, 664. [Google Scholar] [CrossRef] [PubMed]
| Total | Positive | Indeterminate | Negative | |
|---|---|---|---|---|
| Birth year | ||||
| 1950–1954 | 1 | 1 (100) | 0 | 0 |
| 1955–1959 | 4 | 4 (100) | 0 | 0 |
| 1960–1964 | 15 | 15 (100) | 0 | 0 |
| 1965–1969 | 29 | 28 (97) | 1 (3) | 0 |
| 1970–1974 | 20 | 18 (90) | 2 (10) | 0 |
| 1975–1979 | 28 | 26 (93) | 2 (7) | 0 |
| 1980–1984 | 140 | 135 (96) | 1 (1) | 4 (3) |
| 1985–1989 | 350 | 329 (94) | 10 (3) | 11 (3) |
| 1990–1994 | 908 | 816 (90) | 49 (5) | 43 (5) |
| 1995–1999 | 575 | 512 (89) | 34 (6) | 29 (5) |
| Age | ||||
| >60 | 4 | 4 (100) | 0 | 0 |
| 55–59 | 15 | 15 (100) | 0 | 0 |
| 50–54 | 29 | 28 (97) | 1 (3) | 0 |
| 45–49 | 17 | 16 (94) | 1 (6) | 0 |
| 40–44 | 17 | 16 (94) | 1 (6) | 0 |
| 35–39 | 113 | 108 (96) | 3 (3) | 2 (2) |
| 30–34 | 309 | 291 (94) | 8 (3) | 10 (3) |
| 25–29 | 867 | 780 (90) | 47 (5) | 40 (5) |
| 20–24 | 699 | 626 (90) | 38 (5) | 35 (5) |
| Total | 2070 | 1884 (91) | 99 (5) | 87 (4) |
| Total | Positive | Indeterminate | Negative | |
|---|---|---|---|---|
| Birth year | ||||
| 1950–1954 | 1 | 1 (100) | 0 | 0 |
| 1955–1959 | 4 | 3 (75) | 1 (25) | 0 |
| 1960–1964 | 15 | 12 (80) | 3 (20) | 0 |
| 1965–1969 | 29 | 27 (93) | 2 (7) | 0 |
| 1970–1974 | 19 | 14 (74) | 3 (16) | 2 (11) |
| 1975–1979 | 27 | 17 (63) | 7 (26) | 3 (11) |
| 1980–1984 | 134 | 89 (66) | 25 (19) | 20 (5) |
| 1985–1989 | 330 | 268 (81) | 46 (14) | 16 (5) |
| 1990–1994 | 836 | 537 (64) | 135 (16) | 164 (20) |
| 1995–1999 | 432 | 316 (73) | 25 (6) | 91 (21) |
| Age | ||||
| >60 | 4 | 4 (100) | 0 | 0 |
| 55–59 | 15 | 12 (80) | 3 (20) | 0 |
| 50–54 | 29 | 26 (90) | 3 (10) | 0 |
| 45–49 | 16 | 12 (75) | 2 (13) | 2 (13) |
| 40–44 | 16 | 11 (69) | 3 (19) | 2 (13) |
| 35–39 | 106 | 82 (77) | 16 (15) | 8 (8) |
| 30–34 | 288 | 234 (81) | 35 (12) | 19 (7) |
| 25–29 | 780 | 583 (75) | 91 (12) | 106 (14) |
| 20–24 | 573 | 320 (56) | 94 (16) | 159 (28) |
| Total | 1827 | 1284 (70) | 247 (14) | 296 (16) |
| Seroprevalence of Varicella-Zoster Virus | p Value | Seroprevalence of Measles | p Value | |
|---|---|---|---|---|
| Occupational group | <0.001 | <0.001 | ||
| Doctors | 449/473 (95) a,b | 318/417 (76) a,b | ||
| Nurses | 1013/1118 (91) a | 641/943 (68) a,c | ||
| Nursing assistants | 39/39 (100) | 35/38 (92) c,d | ||
| Other HCWs | 383/440 (87) b | 290/429 (68) b,d |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yun, J.H.; Lee, E.; Choi, J.H.; Ki, H.K.; Park, J. Seroprevalence of Varicella-Zoster Virus and Measles among Healthcare Workers in a Tertiary Medical Center in Korea. Vaccines 2022, 10, 1956. https://doi.org/10.3390/vaccines10111956
Yun JH, Lee E, Choi JH, Ki HK, Park J. Seroprevalence of Varicella-Zoster Virus and Measles among Healthcare Workers in a Tertiary Medical Center in Korea. Vaccines. 2022; 10(11):1956. https://doi.org/10.3390/vaccines10111956
Chicago/Turabian StyleYun, Ji Hyun, Eunsol Lee, Jeong Hwa Choi, Hyun Kyun Ki, and Jiho Park. 2022. "Seroprevalence of Varicella-Zoster Virus and Measles among Healthcare Workers in a Tertiary Medical Center in Korea" Vaccines 10, no. 11: 1956. https://doi.org/10.3390/vaccines10111956
APA StyleYun, J. H., Lee, E., Choi, J. H., Ki, H. K., & Park, J. (2022). Seroprevalence of Varicella-Zoster Virus and Measles among Healthcare Workers in a Tertiary Medical Center in Korea. Vaccines, 10(11), 1956. https://doi.org/10.3390/vaccines10111956





