Determining the SARS-CoV-2 Anti-Spike Cutoff Level Denoting Neutralizing Activity Using Two Commercial Kits
Abstract
1. Introduction
2. Methods
2.1. Study Setting and Sample Size Determination
2.2. Data Collection Methods and Tools
2.3. Statistical Analysis
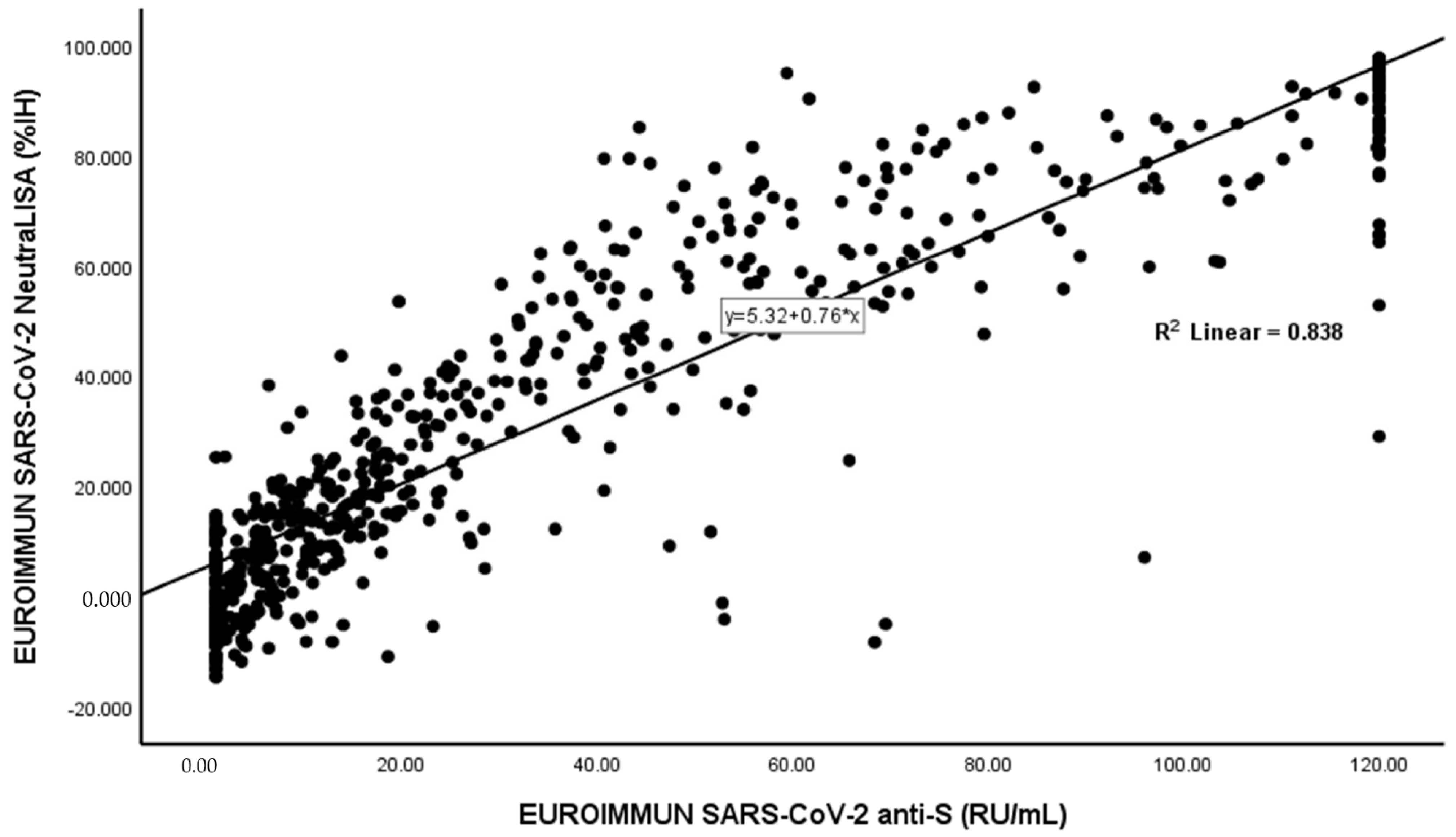
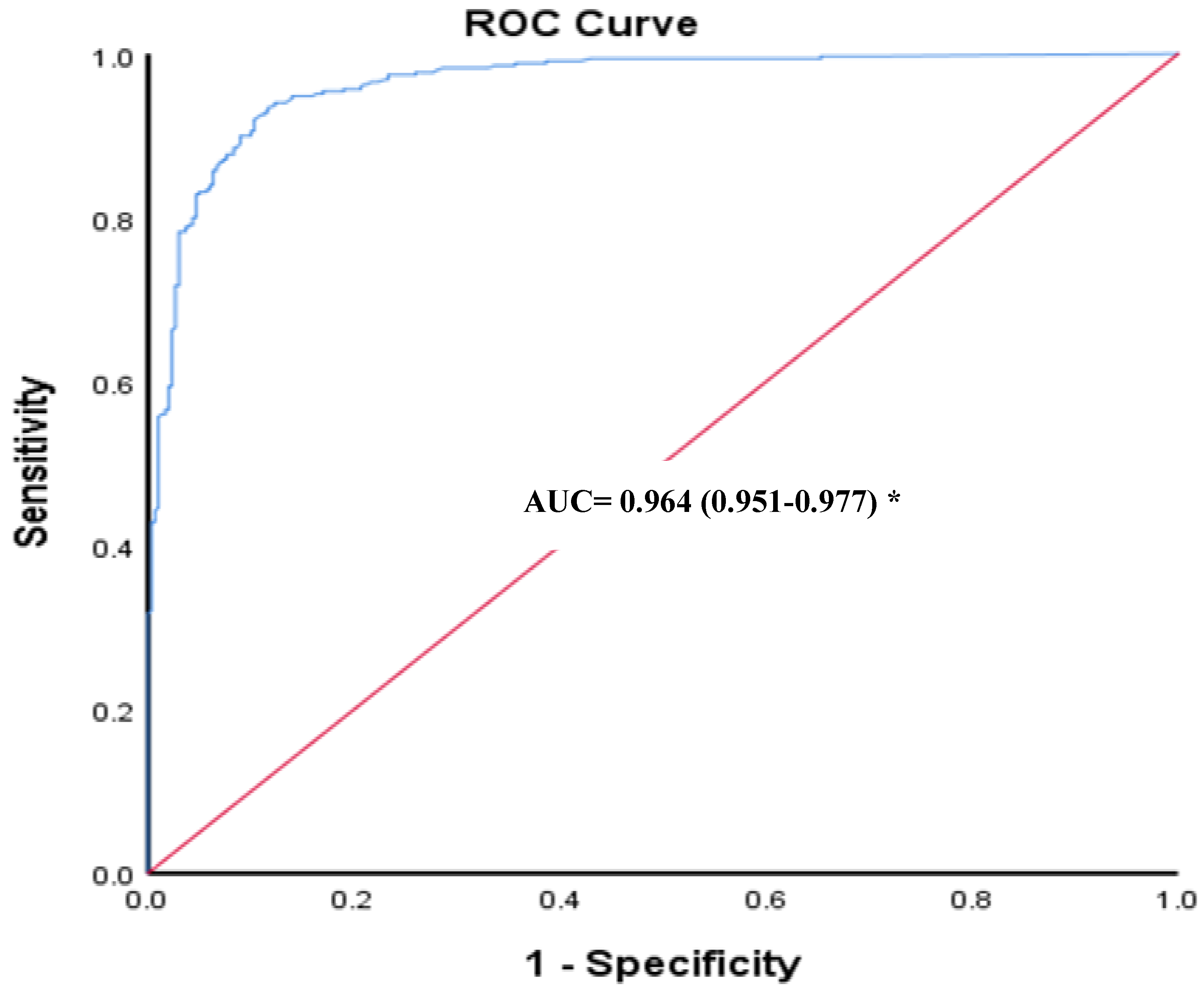
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020, 181, 271–280.e278. [Google Scholar] [CrossRef] [PubMed]
- Yan, R.; Zhang, Y.; Li, Y.; Xia, L.; Guo, Y.; Zhou, Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 2020, 367, 1444–1448. [Google Scholar] [CrossRef] [PubMed]
- Plotkin, S.A. Correlates of protection induced by vaccination. Clin. Vaccine Immunol. 2010, 17, 1055–1065. [Google Scholar] [CrossRef] [PubMed]
- Dolscheid-Pommerich, R.; Bartok, E.; Renn, M.; Kümmerer, B.M.; Schulte, B.; Schmithausen, R.M.; Stoffel-Wagner, B.; Streeck, H.; Saschenbrecker, S.; Steinhagen, K. Correlation between a quantitative anti-SARS-CoV-2 IgG ELISA and neutralization activity. J. Med. Virol. 2022, 94, 388–392. [Google Scholar] [CrossRef]
- US Food and Drug Adminsitration (FDA). Recommendations for Investigational COVID-19 Convalescent Plasma. 2020. Available online: https://www.fda.gov/vaccines-blood-biologics/investigational-new-drug-applications-inds-cber-regulated-products/recommendations-investigational-covid-19-convalescent-plasma (accessed on 9 August 2021).
- Gomaa, M.R.; Kandeil, A.; Mostafa, A.; Roshdy, W.H.; Kayed, A.E.; Shehata, M.; Kutkat, O.; Moatasim, Y.; El Taweel, A.; Mahmoud, S.H.; et al. Prevalence of Severe Acute Respiratory Syndrome Coronavirus 2 Neutralizing Antibodies in Egyptian Convalescent Plasma Donors. Front. Microbiol. 2020, 11, 596851. [Google Scholar] [CrossRef]
- Ward, H.; Cooke, G.S.; Atchison, C.; Whitaker, M.; Elliott, J.; Moshe, M.; Brown, J.C.; Flower, B.; Daunt, A.; Ainslie, K. Prevalence of antibody positivity to SARS-CoV-2 following the first peak of infection in England: Serial cross-sectional studies of 365,000 adults. Lancet Reg. Health-Eur. 2021, 4, 100098. [Google Scholar] [CrossRef]
- Xiaojie, S.; Yu, L.; Guang, Y.; Min, Q. Neutralizing antibodies targeting SARS-CoV-2 spike protein. Stem Cell Res. 2021, 50, 102125. [Google Scholar] [CrossRef]
- Khoury, D.S.; Cromer, D.; Reynaldi, A.; Schlub, T.E.; Wheatley, A.K.; Juno, J.A.; Subbarao, K.; Kent, S.J.; Triccas, J.A.; Davenport, M.P. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 2021, 27, 1205–1211. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, L.; Sang, L.; Ye, F.; Ruan, S.; Zhong, B.; Song, T.; Alshukairi, A.N.; Chen, R.; Zhang, Z. Kinetics of viral load and antibody response in relation to COVID-19 severity. J. Clin. Investig. 2020, 130, 5235–5244. [Google Scholar] [CrossRef]
- Ni, L.; Ye, F.; Cheng, M.-L.; Feng, Y.; Deng, Y.-Q.; Zhao, H.; Wei, P.; Ge, J.; Gou, M.; Li, X. Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. Immunity 2020, 52, 971–977.e973. [Google Scholar] [CrossRef]
- Kohmer, N.; Rühl, C.; Ciesek, S.; Rabenau, H.F. Utility of different surrogate enzyme-linked immunosorbent assays (sELISAs) for detection of SARS-CoV-2 neutralizing antibodies. J. Clin. Med. 2021, 10, 2128. [Google Scholar] [CrossRef] [PubMed]
- Bal, A.; Pozzetto, B.; Trabaud, M.-A.; Escuret, V.; Rabilloud, M.; Langlois-Jacques, C.; Paul, A.; Guibert, N.; D’Aubarède-Frieh, C.; Massardier-Pilonchery, A. Evaluation of high-throughput SARS-CoV-2 serological assays in a longitudinal cohort of patients with mild COVID-19: Clinical sensitivity, specificity, and association with virus neutralization test. Clin. Chem. 2021, 67, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Bonelli, F.; Sarasini, A.; Zierold, C.; Calleri, M.; Bonetti, A.; Vismara, C.; Blocki, F.A.; Pallavicini, L.; Chinali, A.; Campisi, D. Clinical and analytical performance of an automated serological test that identifies S1/S2-neutralizing IgG in COVID-19 patients semiquantitatively. J. Clin. Microbiol. 2020, 58, e01224-20. [Google Scholar] [CrossRef] [PubMed]
- Therrien, C.; Serhir, B.; Bélanger-Collard, M.; Skrzypczak, J.; Shank, D.; Renaud, C.; Girouard, J.; Loungnarath, V.; Carrier, M.; Brochu, G. Multicenter evaluation of the clinical performance and the neutralizing antibody activity prediction properties of 10 high-throughput serological assays used in clinical laboratories. J. Clin. Microbiol. 2021, 59, e02511–e02520. [Google Scholar] [CrossRef] [PubMed]
- El-Ghitany, E.M.; Farag, S.; Farghaly, A.G.; Hashish, M.H.; Hassaan, M.A.; Omran, E.A. A pre-vaccine exploratory survey of SARS-CoV-2 humoral immunity among Egyptian general population. Trop. Med. Health 2022, 50, 53. [Google Scholar] [CrossRef] [PubMed]
- Gaber, Y.; Alem, S.A.; Musa, S.; Amer, K.; Elnagdy, T.; Hassan, W.A.; Abdelrahman, R.Z.; Gad, A.; Ali, M.A.; Badary, H.A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) immunoglobulins using chemiluminescence immunoassay and its correlation with neutralizing antibodies. Virus Res. 2022, 319, 198852. [Google Scholar] [CrossRef]
- EUROIMMUN. SARS-CoV-2 Neutralisation Test in ELISA Format. Available online: https://www.coronavirus-diagnostics.com/documents/Indications/Infections/Coronavirus/EI_2606_I_UK_C.pdf (accessed on 10 August 2021).
- Gosink, J. Investigation of SARS-CoV-2- Specific Immune Reponses. Available online: https://www.euroimmun.de/fileadmin/user_upload/News/Professional-articles/CLI_June_2021_SARS-CoV-2_immune_responses.pdf. (accessed on 12 August 2021).
- Kristiansen, P.A.; Page, M.; Bernasconi, V.; Mattiuzzo, G.; Dull, P.; Makar, K.; Plotkin, S.; Knezevic, I. WHO International Standard for anti-SARS-CoV-2 immunoglobulin. Lancet 2021, 397, 1347–1348. [Google Scholar] [CrossRef]
- Cecconi, M.; Piovani, D.; Brunetta, E.; Aghemo, A.; Greco, M.; Ciccarelli, M.; Angelini, C.; Voza, A.; Omodei, P.; Vespa, E. Early predictors of clinical deterioration in a cohort of 239 patients hospitalized for Covid-19 infection in Lombardy, Italy. J. Clin. Med. 2020, 9, 1548. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. (Zagreb) 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Lucas, C.; Klein, J.; Sundaram, M.E.; Liu, F.; Wong, P.; Silva, J.; Mao, T.; Oh, J.E.; Mohanty, S.; Huang, J.; et al. Delayed production of neutralizing antibodies correlates with fatal COVID-19. Nat. Med. 2021, 27, 1178–1186. [Google Scholar] [CrossRef]
- Cromer, D.; Juno, J.A.; Khoury, D.; Reynaldi, A.; Wheatley, A.K.; Kent, S.J.; Davenport, M.P. Prospects for durable immune control of SARS-CoV-2 and prevention of reinfection. Nat. Rev. Immunol. 2021, 21, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Knezevic, I.; Mattiuzzo, G.; Page, M.; Minor, P.; Griffiths, E.; Nuebling, M.; Moorthy, V. WHO International Standard for evaluation of the antibody response to COVID-19 vaccines: Call for urgent action by the scientific community. Lancet Microbe 2021, 3, E235–E240. [Google Scholar] [CrossRef]
- Pieri, M.; Infantino, M.; Manfredi, M.; Nuccetelli, M.; Grossi, V.; Lari, B.; Tomassetti, F.; Sarubbi, S.; Russo, E.; Amedei, A.; et al. Performance evaluation of four surrogate Virus Neutralization Tests (sVNTs) in comparison to the in vivo gold standard test. FBL 2022, 27, 74. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.W.; Chia, W.N.; Qin, X.; Liu, P.; Chen, M.I.C.; Tiu, C.; Hu, Z.; Chen, V.C.-W.; Young, B.E.; Sia, W.R.; et al. A SARS-CoV-2 surrogate virus neutralization test based on antibody-mediated blockage of ACE2–spike protein–protein interaction. Nat. Biotechnol. 2020, 38, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- Montesinos, I.; Dahma, H.; Wolff, F.; Dauby, N.; Delaunoy, S.; Wuyts, M.; Detemmerman, C.; Duterme, C.; Vandenberg, O.; Martin, C. Neutralizing antibody responses following natural SARS-CoV-2 infection: Dynamics and correlation with commercial serologic tests. J. Clin. Virol. 2021, 144, 104988. [Google Scholar] [CrossRef] [PubMed]
- Chi, X.; Yan, R.; Zhang, J.; Zhang, G.; Zhang, Y.; Hao, M.; Zhang, Z.; Fan, P.; Dong, Y.; Yang, Y. A neutralizing human antibody binds to the N-terminal domain of the Spike protein of SARS-CoV-2. Science 2020, 369, 650–655. [Google Scholar] [CrossRef]
- Salazar, E.; Kuchipudi, S.V.; Christensen, P.A.; Eagar, T.; Yi, X.; Zhao, P.; Jin, Z.; Long, S.W.; Olsen, R.J.; Chen, J. Convalescent plasma anti–SARS-CoV-2 spike protein ectodomain and receptor-binding domain IgG correlate with virus neutralization. J. Clin. Investig. 2020, 130, 6728–6738. [Google Scholar] [CrossRef]
- Weisblum, Y.; Schmidt, F.; Zhang, F.; DaSilva, J.; Poston, D.; Lorenzi, J.C.C.; Muecksch, F.; Rutkowska, M.; Hoffmann, H.-H.; Michailidis, E.; et al. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. eLife 2020, 9, e61312. [Google Scholar] [CrossRef]
- Dinç, H.Ö.; Demirci, M.; Özdemir, Y.E.; Sirekbasan, S.; Aktaş, A.N.; Karaali, R.; Tok, Y.T.; Özbey, D.; Akçin, R.; Gareayaghi, N. Anti-SARS-CoV-2 IgG and neutralizing antibody levels in patients with past COVID-19 infection: A longitudinal study. Balk. Med. J. 2022, 39, 172. [Google Scholar] [CrossRef]
- Valdivia, A.; Torres, I.; Latorre, V.; Francés-Gómez, C.; Albert, E.; Gozalbo-Rovira, R.; Alcaraz, M.J.; Buesa, J.; Rodríguez-Díaz, J.; Geller, R. Inference of SARS-CoV-2 spike-binding neutralizing antibody titers in sera from hospitalized COVID-19 patients by using commercial enzyme and chemiluminescent immunoassays. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 485–494. [Google Scholar] [CrossRef]
- Xue, J.-H.; Wang, Y.-J.; Li, W.; Li, Q.-L.; Xu, Q.-Y.; Niu, J.-J.; Liu, L.-L. Anti–Receptor-Binding Domain Immunoglobulin G Antibody as a Predictor of Seropositivity for Anti–SARS-CoV-2 Neutralizing Antibody. Arch. Pathol. Lab. Med. 2022, 146, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Omran, E.A.; Habashy, R.E.; Ezz Elarab, L.A.; Hashish, M.H.; El-Barrawy, M.A.; Abdelwahab, I.A.; Fekry, M.M. Anti-Spike and Neutralizing Antibodies after Two Doses of COVID-19 Sinopharm/BIBP Vaccine. Vaccines 2022, 10, 1340. Available online: https://www.mdpi.com/2076-393X/10/8/1340 (accessed on 10 July 2021). [CrossRef] [PubMed]
- Adams, E.R.; Ainsworth, M.; Anand, R.; Andersson, M.I.; Auckland, K.; Baillie, J.K.; Barnes, E.; Beer, S.; Bell, J.I.; Berry, T. Antibody testing for COVID-19: A report from the National COVID Scientific Advisory Panel. Wellcome Open Res. 2020, 5, 139. [Google Scholar] [CrossRef] [PubMed]
- Marot, S.; Malet, I.; Leducq, V.; Zafilaza, K.; Sterlin, D.; Planas, D.; Gothland, A.; Jary, A.; Dorgham, K.; Bruel, T. Rapid decline of neutralizing antibodies against SARS-CoV-2 among infected healthcare workers. Nat. Commun. 2021, 12, 844. [Google Scholar] [CrossRef]
- Roshdy, W.H.; Kandeil, A.; El-Shesheny, R.; Khalifa, M.K.; Al-Karmalawy, A.A.; Showky, S.; Naguib, A.; Elguindy, N.; Fahim, M.; Abu Elsood, H.; et al. Insight into Genetic Characteristics of Identified SARS-CoV-2 Variants in Egypt from March 2020 to May 2021. Pathogens 2022, 11, 834. Available online: https://www.mdpi.com/2076-0817/11/8/834 (accessed on 10 July 2021). [CrossRef]
- Service, S.I. Tageddin: Delta Variant Has not Appeared in Egypt so Far. 2021. Available online: https://www.sis.gov.eg/Story/158646?lang=en-us (accessed on 30 August 2021).
- Guérin, P.; Yahi, N.; Azzaz, F.; Chahinian, H.; Sabatier, J.-M.; Fantini, J. Structural dynamics of the SARS-CoV-2 spike protein: A 2-year retrospective analysis of SARS-CoV-2 variants (from alpha to omicron) reveals an early divergence between conserved and variable epitopes. Molecules 2022, 27, 3851. [Google Scholar] [CrossRef]
- Ai, J.; Zhang, H.; Zhang, Y.; Lin, K.; Zhang, Y.; Wu, J.; Wan, Y.; Huang, Y.; Song, J.; Fu, Z. Omicron variant showed lower neutralizing sensitivity than other SARS-CoV-2 variants to immune sera elicited by vaccines after boost. Emerg. Microbes Infect. 2022, 11, 337–343. [Google Scholar] [CrossRef]
| No. | % | Median: Titer (anti-S)/IH%(nAbs) | IQR | ||
|---|---|---|---|---|---|
| SARS-CoV-2 anti-S IgG | Negative | 202 | 31.1 | 1.65 | 4.10 |
| Positive | 448 | 68.9 | 44.00 | 77.48 | |
| Total | 650 | 100.0 | 20.40 | 60.53 | |
| SARS-CoV-2 nAbs | Negative | 300 | 46.2 | 4.82 | 15.46 |
| Positive | 350 | 53.8 | 62.18 | 46.29 | |
| Total | 650 | 100.0 | 24.81 | 59.18 |
| EUROIMMUN SARS-CoV-2 NeutraLISA | Total | |||
|---|---|---|---|---|
| Negative (n = 300) | Positive (n = 350) | |||
| EUROIMMUN SARS-CoV-2 anti-S | Negative | 197 (97.5%) | 5 (2.5%) | 202 |
| Positive | 103 (23.0%) | 345 (77.0%) | 448 | |
| Cohen’s kappa coefficient (κ) = 0.658 (0.602–0.714), SE = 0.029, p-value < 0.01 Overall percent agreement = 83.38% | ||||
| Sensitivity = 98.57% (96.69–99.53%) | ||||
| Specificity = 65.66% (59.99–71.02%) | ||||
| * NPV = 97.52% (94.26–98.95%) | ||||
| ** PPV = 77.00% (74.11–79.67%) | ||||
| *** Positive LR = 2.87 (2.45–3.35) | ||||
| **** Negative LR = 0.02 (0.00–0.05) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Ghitany, E.M.; Hashish, M.H.; Farghaly, A.G.; Omran, E.A. Determining the SARS-CoV-2 Anti-Spike Cutoff Level Denoting Neutralizing Activity Using Two Commercial Kits. Vaccines 2022, 10, 1952. https://doi.org/10.3390/vaccines10111952
El-Ghitany EM, Hashish MH, Farghaly AG, Omran EA. Determining the SARS-CoV-2 Anti-Spike Cutoff Level Denoting Neutralizing Activity Using Two Commercial Kits. Vaccines. 2022; 10(11):1952. https://doi.org/10.3390/vaccines10111952
Chicago/Turabian StyleEl-Ghitany, Engy Mohamed, Mona H. Hashish, Azza Galal Farghaly, and Eman A. Omran. 2022. "Determining the SARS-CoV-2 Anti-Spike Cutoff Level Denoting Neutralizing Activity Using Two Commercial Kits" Vaccines 10, no. 11: 1952. https://doi.org/10.3390/vaccines10111952
APA StyleEl-Ghitany, E. M., Hashish, M. H., Farghaly, A. G., & Omran, E. A. (2022). Determining the SARS-CoV-2 Anti-Spike Cutoff Level Denoting Neutralizing Activity Using Two Commercial Kits. Vaccines, 10(11), 1952. https://doi.org/10.3390/vaccines10111952






