Does the COVID-19 Vaccination Rate Change According to the Education and Income: A Study on Vaccination Rates in Cities of Turkey between 2021-September and 2022-February
Abstract
1. Introduction
2. Materials and Methods
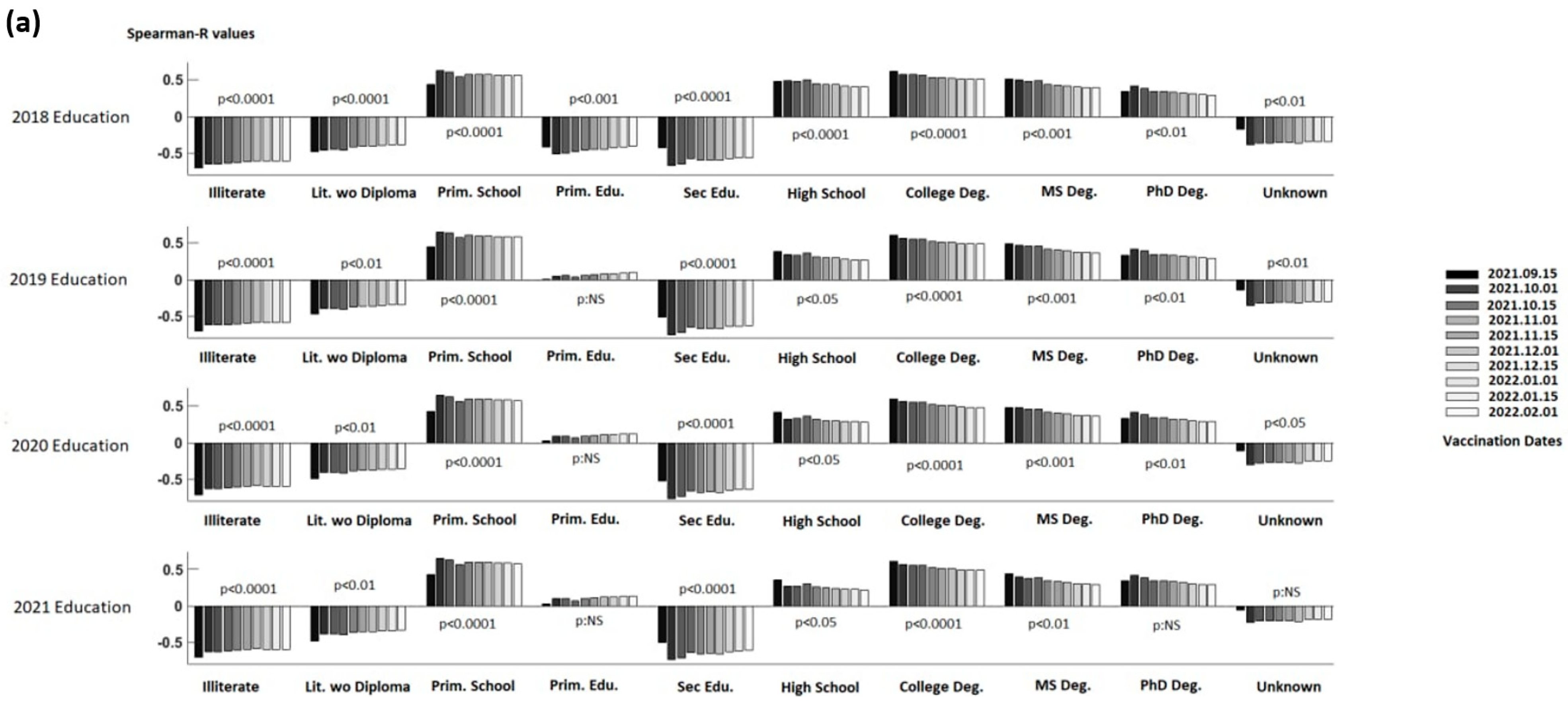
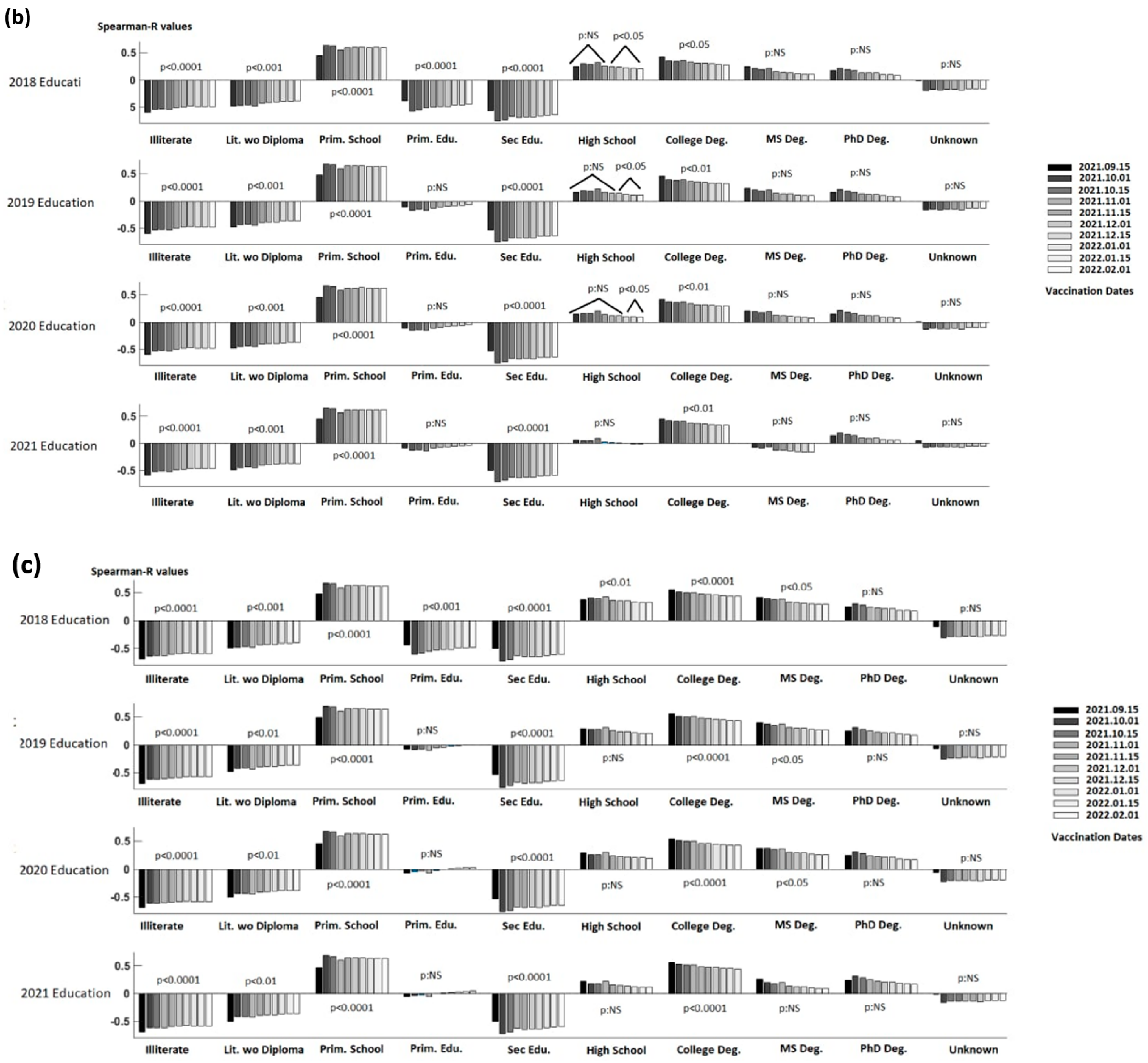
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19)—Overview. Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 15 September 2021).
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 15 September 2021).
- World Health Organization. Numbers at a Glance. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjw08aYBhDlARIsAA_gb0dMdb1bliPkaPx-ogleaqoVr_idM0fQ6ZAlg240DoqgPoClurrO2EAaApjMEALw_wcB (accessed on 15 August 2022).
- World Health Organization. Novel Coronavirus (COVID-19) Cases. Available online: https://github.com/CSSEGISandData/COVID-19 (accessed on 15 August 2022).
- Centers for Disease Control and Prevention. Benefits of Getting a COVID-19 Vaccine. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html#:~:text=COVID%2D19%20vaccination%20helps%20protect,illness%20or%20post%2DCOVID%20conditions (accessed on 15 January 2022).
- Mayoclinic. COVID-19 Drugs: Are There Any That Work? Available online: https://www.mayoclinic.org/diseases-conditions/coronavirus/expert-answers/coronavirus-drugs/faq-20485627 (accessed on 7 April 2022).
- World Health Organization. Coronavirus Disease (COVID-19): Vaccines. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-(covid-19)-vaccines?adgroupsurvey={adgroupsurvey}&gclid=CjwKCAjwvNaYBhA3EiwACgndghhyvDvXXVDN0_ODg3Qv3s-fk57DSBzEPFS5ZhFLY4FcsIS7ABoCCRoC9rUQAvD_BwE (accessed on 2 September 2022).
- WHO COVID-19 Vaccine Tracker and Landscape. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 5 September 2022).
- Palacios, R.; Batista, A.P.; Albuquerque, C.S.N.; Patiño, E.G.; Santos, J.D.P.; Tilli Reis Pessoa Conde, M.; Piorelli, R.D.O.; Pereira Júnior, L.C.; Raboni, S.M.; Ramos, F.; et al. Efficacy and Safety of a COVID-19 Inactivated Vaccine in Healthcare Professionals in Brazil: The PROFISCOV Study. SSRN Electron. J. 2021. [Google Scholar] [CrossRef]
- Tanriover, M.D.; Doğanay, H.L.; Akova, M.; Güner, H.R.; Azap, A.; Akhan, S.; Köse, Ş.; Erdinç, F.Ş.; Akalın, E.H.; Tabak, .F.; et al. Efficacy and Safety of an Inactivated Whole-Virion SARS-CoV-2 Vaccine (CoronaVac): Interim Results of a Double-Blind, Randomised, Placebo-Controlled, Phase 3 Trial in Turkey. Lancet 2021, 398, 213–222. [Google Scholar] [CrossRef]
- Ministry of Health. The First Coronavirus Vaccine Was Given to Minister of Health Fahrettin Koca (In Turkish). Available online: https://www.saglik.gov.tr/TR,78148/ilk-koronavirus-asisi-saglik-bakani-fahrettin-kocaya-yapildi.html (accessed on 20 October 2021).
- Anadolu Agency. Ministry of Health: 5 Million Doses of Sinovac Vaccine Reached Turkey Today (In Turkish). Available online: https://www.aa.com.tr/tr/koronavirus/saglik-bakanligi-5-milyon-doz-sinovac-asisi-bugun-turkiyeye-ulasti/2279453 (accessed on 6 August 2021).
- Ministry of Health COVID-19 Vaccine Information Platform (In Turkish). Available online: https://covid19asi.saglik.gov.tr/TR-77706/covid-19-asisi-ulusal-uygulama-stratejisi.html (accessed on 18 October 2021).
- Hurriyet. It Started to Be Used for the First Time Today (In Turkish). Available online: https://www.hurriyet.com.tr/gundem/pfizer-biontech-asisi-hakkinda-merak-edilenler-41778462 (accessed on 18 September 2021).
- Centers for Disease Control and Prevention. Overview of COVID-19 Vaccines. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/overview-COVID-19-vaccines.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fvaccines%2Fdifferent-vaccines%2FPfizer-BioNTech.html (accessed on 2 September 2022).
- Thomas, S.J.; Moreira, E.D., Jr.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Polack, F.P.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine through 6 Months. N. Engl. J. Med. 2021, 385, 1761–1773. [Google Scholar] [CrossRef] [PubMed]
- Anadolu Agency. Turkey OKs Emergency Use of Sputnik-V Vaccine. Available online: https://www.aa.com.tr/en/latest-on-coronavirus-outbreak/turkey-oks-emergency-use-of-sputnik-v-vaccine/2225824 (accessed on 17 April 2022).
- Diken Newspaper. Russian Vaccine Turned into Riddle: Ministry Is Still Silent, It Is Not Clear Why It Is Not Used (In Turkish). Available online: https://www.diken.com.tr/sputnik-v-bilmecesi-saglik-bakanligi-hala-sessiz-ttb-acikladi/ (accessed on 26 October 2021).
- BBC. Turkovac: Emergency Use Approved for Domestic COVID Vaccine. Available online: https://www.bbc.com/turkce/haberler-dunya-59754868 (accessed on 20 July 2021).
- Turkish Republic Ministry of Health COVID-19 Vaccine Information Platform (In Turkish). Available online: https://covid19asi.saglik.gov.tr (accessed on 1 February 2022).
- Our World in Data. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus#coronavirus-country-profiles (accessed on 25 August 2022).
- World Health Organization. Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 14 October 2022).
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, L. COVID-19 Vaccine Hesitancy in a Representative Working-Age Population in France: A Survey Experiment Based on Vaccine Characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Nguyen, K.; Corlin, L.; Allen, J.D.; Chung, M. Changes in COVID-19 Vaccination Receipt and Intention to Vaccinate by Socioeconomic Characteristics and Geographic Area, United States, January 6–March 29, 2021. Ann. Med. 2021, 53, 1419–1428. [Google Scholar] [CrossRef] [PubMed]
- Brownstein, N.C.; Reddy, H.; Whiting, J.; Kasting, M.L.; Head, K.J.; Vadaparampil, S.T.; Giuliano, A.R.; Gwede, C.K.; Meade, C.D.; Christy, S.M. COVID-19 Vaccine Behaviors and Intentions among a National Sample of United States Adults Ages 18–45. Prev. Med. 2022, 160, 107038. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, Q.; Tarimo, C.S.; Wang, M.; Gu, J.; Wei, W.; Ma, M.; Zhao, L.; Mu, Z.; Miao, Y. COVID-19 Vaccine Hesitancy Among Chinese Population: A Large-Scale National Study. Front. Immunol. 2021, 12, 781161. [Google Scholar] [CrossRef] [PubMed]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 Vaccine Hesitancy and Resistance: Correlates in a Nationally Representative Longitudinal Survey of the Australian Population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Abdullah, M.; Shahait, A.D.; Qaisieh, R.; Al-Ramahi, M.; Bader, G.; AbuRajab, M.O.; Haddad, T.A.; Al-Omari, A.Y.; Issa, M.S.B.; Bader, T.; et al. Perspectives on COVID-19 Vaccines and Its Hesitancy Among Jordanian Population. Cureus 2022, 14, e26337. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.L.; Wileden, L.; Shanks, T.R.; Goold, S.D.; Morenoff, J.D.; Gorin, S.N.S. Mediators of Racial Differences in COVID-19 Vaccine Acceptance and Uptake: A Cohort Study in Detroit, MI. Vaccines 2021, 10, 36. [Google Scholar] [CrossRef]
- Khairat, S.; Zou, B.; Adler-Milstein, J. Factors and Reasons Associated with Low COVID-19 Vaccine Uptake among Highly Hesitant Communities in the US. Am. J. Infect. Control 2022, 50, 262–267. [Google Scholar] [CrossRef]
- Latkin, C.; Dayton, L.; Miller, J.; Yi, G.; Balaban, A.; Boodram, B.; Uzzi, M.; Falade-Nwulia, O. A Longitudinal Study of Vaccine Hesitancy Attitudes and Social Influence as Predictors of COVID-19 Vaccine Uptake in the US. Hum. Vaccines Immunother. 2022, 18, 2043102. [Google Scholar] [CrossRef] [PubMed]
- Sonmezer, M.C.; Sahin, T.K.; Erul, E.; Ceylan, F.S.; Hamurcu, M.Y.; Morova, N.; Al, I.R.; Unal, S. Knowledge, Attitudes, and Perception towards COVID-19 Vaccination among the Adult Population: A Cross-Sectional Study in Turkey. Vaccines 2022, 10, 278. [Google Scholar] [CrossRef] [PubMed]
- Muhajarine, N.; Adeyinka, D.A.; McCutcheon, J.; Green, K.L.; Fahlman, M.; Kallio, N. COVID-19 Vaccine Hesitancy and Refusal and Associated Factors in an Adult Population in Saskatchewan, Canada: Evidence from Predictive Modelling”. Editör Anat Gesser-Edelsburg. PLoS ONE 2021, 16, e0259513. [Google Scholar] [CrossRef] [PubMed]
- The Turkish Statistical Institute Database. Available online: https://data.tuik.gov.tr/Search/Search?text=e%C4%9Fitim&dil=1 (accessed on 1 September 2021).
- The Turkish Statistical Institute Database. Available online: https://data.tuik.gov.tr/Bulten/Index?p=Il-Bazinda-Gayrisafi-Yurt-Ici-Hasila-2020-37188 (accessed on 1 September 2021).
- Randolph, H.E.; Barreiro, L.B. Herd Immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Smallpox. Available online: https://www.who.int/health-topics/smallpox#tab=tab_1 (accessed on 15 September 2021).
- World Health Organization. Poliomyelitis. Available online: https://www.who.int/news-room/fact-sheets/detail/poliomyelitis (accessed on 15 September 2021).
- Dube, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; The SAGE Working Group on Vaccine Hesitancy. Strategies for Addressing Vaccine Hesitancy—A Systematic Review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cengiz, B.; Sayılır, M.Ü.; Zengin, N.Y.; Küçük, Ö.N.; Soylu, A.R. Does the COVID-19 Vaccination Rate Change According to the Education and Income: A Study on Vaccination Rates in Cities of Turkey between 2021-September and 2022-February. Vaccines 2022, 10, 1933. https://doi.org/10.3390/vaccines10111933
Cengiz B, Sayılır MÜ, Zengin NY, Küçük ÖN, Soylu AR. Does the COVID-19 Vaccination Rate Change According to the Education and Income: A Study on Vaccination Rates in Cities of Turkey between 2021-September and 2022-February. Vaccines. 2022; 10(11):1933. https://doi.org/10.3390/vaccines10111933
Chicago/Turabian StyleCengiz, Beyza, Mustafa Ünal Sayılır, Nur Yıldız Zengin, Öykü Nehir Küçük, and Abdullah Ruhi Soylu. 2022. "Does the COVID-19 Vaccination Rate Change According to the Education and Income: A Study on Vaccination Rates in Cities of Turkey between 2021-September and 2022-February" Vaccines 10, no. 11: 1933. https://doi.org/10.3390/vaccines10111933
APA StyleCengiz, B., Sayılır, M. Ü., Zengin, N. Y., Küçük, Ö. N., & Soylu, A. R. (2022). Does the COVID-19 Vaccination Rate Change According to the Education and Income: A Study on Vaccination Rates in Cities of Turkey between 2021-September and 2022-February. Vaccines, 10(11), 1933. https://doi.org/10.3390/vaccines10111933





