Caregiver Willingness to Vaccinate Children with Pneumococcal Vaccines and to Pay in a Low-Resource Setting in China: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Statistical Analysis
2.3. Ethical Approval
3. Results
3.1. Demographic Characteristics of Participants
3.2. Behavioral and Social Factors Related to Vaccination
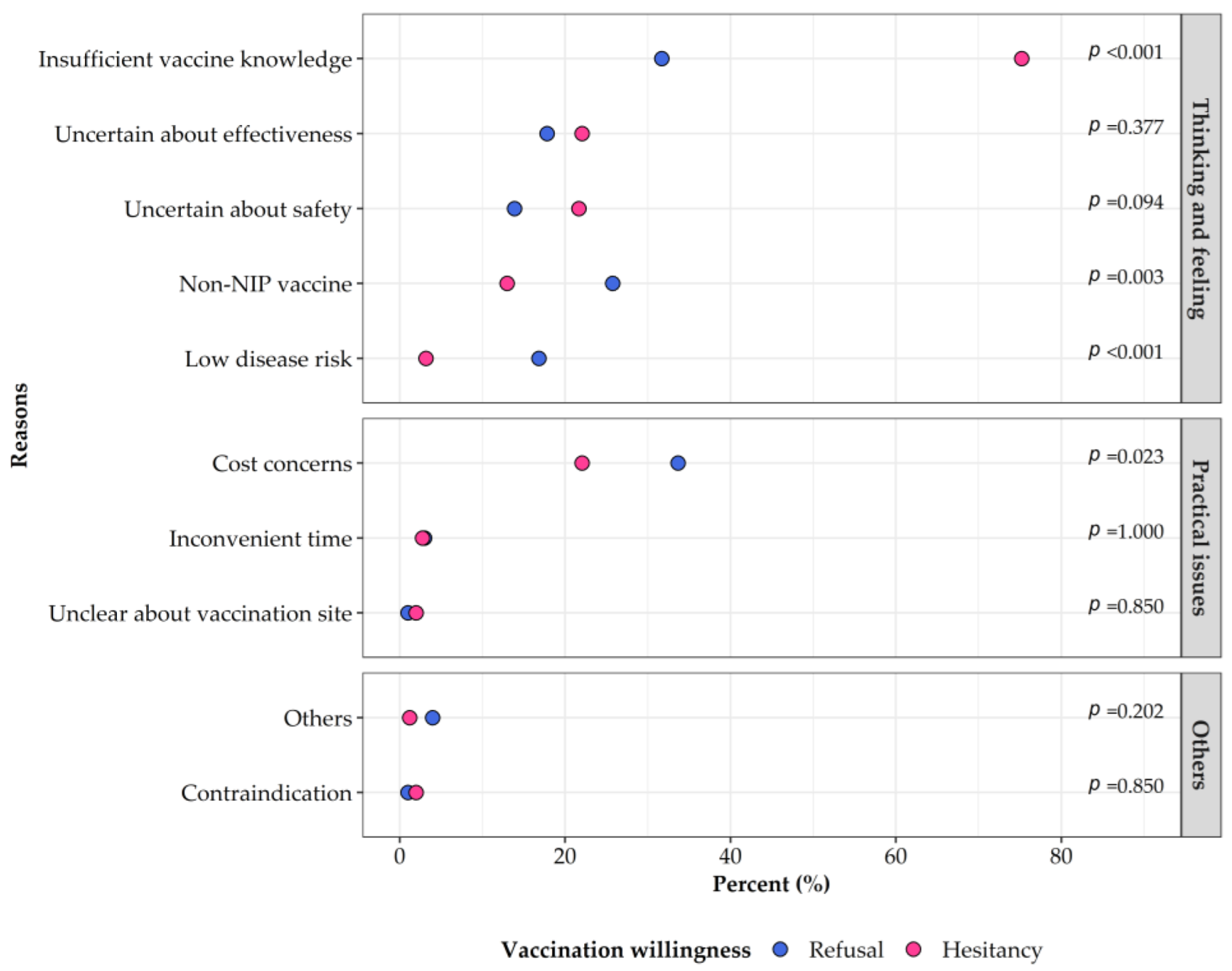
3.3. Willingness to Accept PCV13 Vaccination and Associated Factors
3.4. Willingness to Pay for PCV13 Vaccination and Associated Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- World Health Organization. Organisation mondiale de la S. pneumococcal conjugate vaccines in infants and children under 5 years of age: Who position paper—February 2019—Vaccins antipneumococciques conjugués chez les nourrissons et les enfants de moins de 5 ans: Note de synthèse de l’oms—Février 2019. Wkly. Epidemiol. Rec. 2019, 94, 85–103. [Google Scholar]
- Hanada, S.; Pirzadeh, M.; Carver, K.Y.; Deng, J.C. Respiratory viral infection-induced microbiome alterations and secondary bacterial pneumonia. Front. Immunol. 2018, 9, 2640. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Meeting of the immunization strategic advisory group of experts, November 2007—Conclusions and recommendations. Wkly. Epidemiol. Rec. 2008, 83, 1–15. [Google Scholar]
- Loughlin, A.M.; Hsu, K.; Silverio, A.L.; Marchant, C.D.; Pelton, S.I. Direct and indirect effects of PCV13 on nasopharyngeal carriage of PCV13 unique pneumococcal serotypes in Massachusetts’ children. Pediatr. Inf. Dis. J. 2014, 33, 504–510. [Google Scholar] [CrossRef]
- Troeger, C.E.; Khalil, I.A.; Blacker, B.F.; Biehl, M.H.; Albertson, S.B.; Zimsen, S.R.M.; Rao, P.C.; Abate, D.; Admasie, A.; Ahmadi, A.; et al. Quantifying risks and interventions that have affected the burden of lower respiratory infections among children younger than 5 years: An analysis for the global burden of disease study 2017. Lancet Inf. Dis. 2020, 20, 60–79. [Google Scholar] [CrossRef]
- Immunization Coverage [Updated 14 July 2022]. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 14 August 2022).
- Lai, X.; Wahl, B.; Yu, W.; Xu, T.; Zhang, H.; Garcia, C.; Qin, Y.; Guo, Y.; Yin, Z.; Knoll, M.D.; et al. National, regional, and provincial disease burden attributed to Streptococcus pneumoniae and Haemophilus influenzae type B in children in China: Modelled estimates for 2010–17. Lancet Reg. Health—West. Pac. 2022, 22, 100430. [Google Scholar] [CrossRef]
- Wang, J.; Wu, Q.S.; Lu, J.; Ni, Y.H.; Zhou, F. Low vaccination coverage of pneumococcal conjugate vaccines (PCVs) in Shanghai, China: A database analysis based on birth cohorts from 2012 to 2020. Vaccine 2021, 39, 6189–6194. [Google Scholar] [CrossRef]
- Oduwole, E.O.; Pienaar, E.D.; Mahomed, H.; Wiysonge, C.S. Overview of tools and measures investigating vaccine hesitancy in a ten year period: A scoping review. Vaccines 2022, 10, 1198. [Google Scholar] [CrossRef]
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- WHO. Report of the Sage Working Group on Vaccine Hesitancy. Available online: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf (accessed on 14 August 2022).
- WHO. Understanding the behavioural and social drivers of vaccine uptake WHO position paper—May 2022. Wkly. Epidemiol. Rec. 2022, 97, 209–224. [Google Scholar]
- Chu, H.; Liu, S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Educ. Couns. 2021, 104, 1878–1886. [Google Scholar] [CrossRef] [PubMed]
- Nachega, J.B.; A Sam-Agudu, N.; Masekela, R.; van der Zalm, M.M.; Nsanzimana, S.; Condo, J.; Ntoumi, F.; Rabie, H.; Kruger, M.; Wiysonge, C.S.; et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob. Health 2021, 9, e746–e748. [Google Scholar] [CrossRef]
- Li, Z.; Li, Z.; Mykhailov, A.; Shi, W.; Yang, Z.; Xia, S. Evaluation and analysis of socio-economic development level and management in Guangxi province of China. Stud. Appl. Econ. 2021, 39, 5. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, T.; Wang, Y.; Ma, L.; Xie, S.; Zhou, J.; Qi, W.; Wang, Q.; Dai, P.; Du, Y.; et al. Willingness of caregivers to have their children vaccinated with pneumococcal vaccines in the context of an innovative immunization strategy—Weifang City, Shandong province, 2021. China CDC Wkly. 2022, 4, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Prince, R. Using surveys to value public goods: The contingent valuation method. Nat. Res. J. 1989, 29, 900–902. [Google Scholar]
- McDonald, J.F.; Moffitt, R.A. The uses of tobit analysis. Rev. Econ. Stat. 1980, 62, 318–321. [Google Scholar] [CrossRef]
- Wang, C.; Su, L.; Mu, Q.; Gu, X.; Guo, X.; Wang, X. Cost-effectiveness analysis of domestic 13-valent pneumococcal conjugate vaccine for children under 5 years of age in Mainland China. Hum. Vaccines Immunother. 2021, 17, 2241–2248. [Google Scholar] [CrossRef]
- Hou, Z.; Jie, C.; Yue, D.; Fang, H.; Meng, Q.; Zhang, Y. Determinants of willingness to pay for self-paid vaccines in China. Vaccine 2014, 32, 4471–4477. [Google Scholar] [CrossRef]
- Yu, M.; Yao, X.; Liu, G.; Wu, J.; Lv, M.; Pang, Y.; Xie, Z.; Huang, Y. Barriers and facilitators to uptake and promotion of influenza vaccination among health care workers in the community in Beijing, China: A qualitative study. Vaccine 2022, 40, 2202–2208. [Google Scholar] [CrossRef]
- Klett-Tammen, C.J.; Krause, G.; Seefeld, L.; Ott, J.J. Determinants of tetanus, pneumococcal and influenza vaccination in the elderly: A representative cross-sectional study on knowledge, attitude and practice (Kap). BMC Pub. Health 2016, 16, 121. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhu, H.; Lai, X.; Zhang, H.; Huang, Y.; Feng, H.; Lyu, Y.; Jing, R.; Guo, J.; Fang, H. From COVID-19 vaccination intention to actual vaccine uptake: A longitudinal study among Chinese adults after six months of a national vaccination campaign. Exp. Rev. Vaccines 2022, 21, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Wang, Q.; Yue, N.; Zheng, M.; Wang, D.; Duan, C.; Yu, X.; Zhang, X.; Bao, C.; Jin, H. Influenza vaccination coverage of population and the factors influencing influenza vaccination in Mainland China: A meta-analysis. Vaccine 2018, 36, 7262–7269. [Google Scholar] [CrossRef] [PubMed]
- Pavia, M.; Rita Foresta, M.; Carbone, V.; Angelillo, I.F. Influenza and pneumococcal immunization in the elderly: Knowledge, attitudes, and practices among general practitioners in Italy. Pub. Health 2003, 117, 202–207. [Google Scholar] [CrossRef]
- Trucchi, C.; Restivo, V.; Amicizia, D.; Fortunato, F.; Manca, A.; Martinelli, D.; Montecucco, A.; Piazza, M.F.; Prato, R.; Tisa, V.; et al. Italian health care workers’ knowledge, attitudes, and practices regarding human papillomavirus infection and prevention. Int. J. Environ. Res. Pub. Health 2020, 17, 5278. [Google Scholar] [CrossRef]
- Anastasi, D.; Di Giuseppe, G.; Marinelli, P.; Angelillo, I.F. Paediatricians knowledge, attitudes, and practices regarding immunizations for infants in Italy. BMC Pub. Health 2009, 9, 463. [Google Scholar] [CrossRef]
- Corben, P.; Leask, J. Vaccination hesitancy in the antenatal period: A cross-sectional survey. BMC Pub. Health 2018, 18, 566. [Google Scholar] [CrossRef]
- Lai, X.; Li, M.; Hou, Z.; Guo, J.; Zhang, H.; Wang, J.; Fang, H. Factors associated with caregivers’ hesitancy to vaccinate children against influenza: A cross-sectional survey in China. Vaccine 2022, 40, 3975–3983. [Google Scholar] [CrossRef]
- Sato, R.; Takasaki, Y. Peer effects on vaccination behavior: Experimental evidence from rural Nigeria. Econ. Dev. Cult. Chang. 2019, 68, 93–129. [Google Scholar] [CrossRef]
- Liu, F.; Zheng, C.; Wang, L.; Geng, M.; Chen, H.; Zhou, S.; Ran, L.; Li, Z.; Zhang, Y.; Feng, Z.; et al. Interpretation of the protocol for prevention and control of COVID-19 in China (Edition 8). China CDC Wkly. 2021, 3, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Ji, M.; Huang, Z.; Ren, J.; Wagner, A.L. Vaccine hesitancy and receipt of mandatory and optional pediatric vaccines in Shanghai, China. Hum. Vaccines Immunother. 2022, 18, 2043025. [Google Scholar] [CrossRef]
- National Bureau of Statistics. Statistical Communique of the People’s Republic of China on the 2021 National Economic and Social Development [Updated 28 February 2022]. Available online: http://www.stats.gov.cn/english/PressRelease/202202/t20220227_1827963.html (accessed on 31 August 2022).
- Guilin Bureau of Statistics. Statistical Communique of the Guilin City on the 2021 National Economic and Social Development [Updated 24 April 2022]. Available online: http://tjj.guilin.gov.cn/tjsj/tjgb/202204/t20220427_2261233.html (accessed on 31 August 2022).
- Ceyhan, M.; Ozsurekci, Y.; Aykac, K.; Hacibedel, B.; Ozbilgili, E. Economic burden of pneumococcal infections in children under 5 years of age. Hum. Vaccines Immunother. 2018, 14, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Amicizia, D.; Astengo, M.; Paganino, C.; Piazza, M.F.; Sticchi, C.; Orsi, A.; Varlese, F.; Hu, T.; Petigara, T.; Senese, F.; et al. Economic burden of pneumococcal disease in children in Liguria, Italy. Hum. Vaccines Immunother. 2022, 18, 2082205. [Google Scholar] [CrossRef] [PubMed]
- Shiri, T.; Khan, K.; Keaney, K.; Mukherjee, G.; McCarthy, N.D.; Petrou, S. Pneumococcal disease: A systematic review of health utilities, resource use, costs, and economic evaluations of interventions. Value Health 2019, 22, 1329–1344. [Google Scholar] [CrossRef]
- Maurer, K.A.; Chen, H.-F.; Wagner, A.L.; Hegde, S.T.; Patel, T.; Boulton, M.L.; Hutton, D.W. Cost-effectiveness analysis of pneumococcal vaccination for infants in China. Vaccine 2016, 34, 6343–6349. [Google Scholar] [CrossRef]

| Total | Intention to Get the Child Vaccinated with 13-Valent Pneumococcal Conjugate Vaccines | p | |||
|---|---|---|---|---|---|
| Acceptance | Hesitancy | Refusal | |||
| n (%) | 1254 (100.00) | 899 (71.69) | 254 (20.26) | 101 (8.05) | |
| Caregivers’ characteristics | |||||
| Age (years), median (Q1-Q3) | 32.00 (29.00–35.00) | 32.00 (29.00–35.00) | 32.50 (29.00–36.00) | 33.00 (30.00–35.00) | 0.158 |
| Age group (years), n (%) | 0.066 | ||||
| ≤29 | 344 (27.43) | 255 (28.36) | 66 (25.98) | 23 (22.77) | |
| 30–34 | 492 (39.23) | 352 (39.15) | 99 (38.98) | 41 (40.59) | |
| 35–39 | 290 (23.13) | 214 (23.80) | 50 (19.69) | 26 (25.74) | |
| ≥40 | 128 (10.21) | 78 (8.68) | 39 (15.35) | 11 (10.89) | |
| Sex, n (%) | 0.005 * | ||||
| Male | 288 (22.97) | 200 (22.25) | 74 (29.13) | 14 (13.86) | |
| Female | 966 (77.03) | 699 (77.75) | 180 (70.87) | 87 (86.14) | |
| Educational attainment, n (%) | <0.001 * | ||||
| High school and below | 488 (38.92) | 314 (34.93) | 127 (50.00) | 47 (46.53) | |
| Bachelor’s degree and above | 766 (61.08) | 585 (65.07) | 127 (50.00) | 54 (53.47) | |
| Relationship to the child, n (%) | 0.004 * | ||||
| Mother | 950 (75.76) | 691 (76.86) | 174 (68.50) | 85 (84.16) | |
| Father | 284 (22.65) | 198 (22.02) | 72 (28.35) | 14 (13.86) | |
| Grandparent | 20 (1.59) | 10 (1.11) | 8 (3.15) | 2 (1.98) | |
| Annual household income (CNY 10,000), n (%) | 0.055 | ||||
| <5 | 378 (30.14) | 249 (27.70) | 93 (36.61) | 36 (35.64) | |
| 5–15 | 597 (47.61) | 433 (48.16) | 116 (45.67) | 48 (47.52) | |
| 15–25 | 195 (15.55) | 149 (16.57) | 33 (12.99) | 13 (12.87) | |
| ≥25 | 84 (6.70) | 68 (7.56) | 12 (4.72) | 4 (3.96) | |
| Children’s characteristics | |||||
| Sex, n (%) | 0.351 | ||||
| Male | 628 (50.12) | 441 (49.11) | 130 (51.18) | 57 (56.44) | |
| Female | 625 (49.88) | 457 (50.89) | 124 (48.82) | 44 (43.56) | |
| Age (months), median (Q1-Q3) | 9.00 (4.00–19.00) | 9.00 (4.00–18.00) | 9.00 (5.00–21.00) | 11.00 (5.00–22.00) | 0.123 |
| Age group (months), n (%) | 0.121 | ||||
| <6 | 393 (31.34) | 292 (32.48) | 70 (27.56) | 31 (30.69) | |
| 6–11 | 362 (28.87) | 265 (29.48) | 76 (29.92) | 21 (20.79) | |
| 12–23 | 271 (21.61) | 193 (21.47) | 51 (20.08) | 27 (26.73) | |
| 24–59 | 228 (18.18) | 149 (16.57) | 57 (22.44) | 22 (21.78) | |
| An only child, n (%) | 612 (48.80) | 473 (52.61) | 107 (42.13) | 32 (31.68) | <0.001 * |
| Refusal or Hesitancy versus Acceptance | Hesitancy versus Acceptance | Refusal versus Acceptance | |
|---|---|---|---|
| Demographics | |||
| Only-child family (Ref = “No”) | 0.48 (0.36–0.65) | 0.57 (0.41–0.79) | 0.30 (0.19–0.50) |
| Social and psychological context | |||
| Baseline vaccine hesitancy | |||
| Perceived high effectiveness (Ref = “No”) | 0.61 (0.44–0.84) | 0.63 (0.44–0.90) | 0.57 (0.35–0.94) |
| Willing to vaccinate their child with self-paid vaccines (Ref = “No”) | 0.41 (0.26–0.64) | 0.51 (0.31–0.83) | 0.24 (0.13–0.44) |
| Vaccine preference (Ref = “No preference”) | |||
| Domestic | 1.09 (0.81–1.48) | - | - |
| Imported | 0.50 (0.28–0.89) | - | - |
| Cues to action | |||
| The child has a history of pneumonia (Ref = “No”) | 0.63 (0.41–0.96) | - | - |
| Subjective norm | |||
| The child’s siblings have been vaccinated with PCV13 (Ref = “No or unclear”) | 0.13 (0.06–0.27) | 0.11 (0.04–0.30) | 0.15 (0.05–0.46) |
| Have been recommended PCV13 by health workers (Ref = “No”) | - | 0.40 (0.19–0.82) | - |
| Trust health workers’ vaccination recommendation (Ref = “No”) | 0.49 (0.34–0.70) | 0.49 (0.33–0.73) | 0.52 (0.30–0.90) |
| Risk perception of pneumonia | |||
| Perceived high severity of pneumonia (Ref = “No”) | 0.55 (0.33–0.92) | 0.80 (0.45–1.43) | 0.25 (0.13–0.48) |
| Attitudes and beliefs about PCV13 | |||
| Know that PCV13 is not the vaccine for COVID-19 (Ref = “No”) | - | - | 2.37 (1.29–4.36) |
| Know PCV13 (Ref = “No”) | 0.57 (0.41–0.78) | 0.43 (0.25–0.73) | - |
| PCV13 should be introduced to NIP (Ref = “No or unclear”) | 0.13 (0.09–0.20) | 0.14 (0.09–0.22) | 0.12 (0.07–0.22) |
| Number of Participants, n (%) | WTP (CNY), Median (Q1-Q3) | Estimate | p | |
|---|---|---|---|---|
| Total | 1138 (100.0) | 2260.00 (674.00–2588.00) | - | - |
| Demographics | ||||
| Only-child family | ||||
| Yes | 575 (50.53) | 2588.00 (968.00–2588.00) | 634.16 | <0.001 |
| No | 563 (49.47) | 1542.00 (593.00–2588.00) | Ref | |
| Social and psychological context | ||||
| Baseline vaccine hesitancy | ||||
| Perceived high vaccine effectiveness | ||||
| Yes | 832 (73.11) | 2588.00 (903.50–2588.00) | 500.86 | <0.001 |
| No | 306 (26.89) | 1138.50 (508.00–2588.00) | Ref | |
| Willing to vaccinate their child with self-paid vaccines | ||||
| No | 92 (8.08) | 383.00 (88.00–1022.00) | −1199.73 | <0.001 |
| Yes | 1046 (91.92) | 2588.00 (867.00–2588.00) | Ref | |
| Vaccine preference | ||||
| Domestic | 523 (45.96) | 1736.00 (613.00–2588.00) | −222.83 | 0.044 |
| Imported | 137 (12.04) | 2588.00 (1058.00–2588.00) | 285.89 | 0.107 |
| No preference | 478 (42.00) | 2588.00 (886.00–2588.00) | Ref | |
| Subject norm | ||||
| The child’s siblings have been vaccinated with PCV13 | ||||
| Yes | 131 (11.51) | 2588.00 (1060.00–2588.00) | 590.06 | 0.001 |
| No or unclear | 1007 (88.49) | 2005.00 (660.00–2588.00) | Ref | |
| Family members have a medical education background | ||||
| Yes | 263 (23.11) | 2588.00 (907.00–2588.00) | 282.11 | 0.026 |
| No | 875 (76.89) | 1853.00 (663.00–2588.00) | Ref | |
| Attitudes and beliefs about PCV13 | ||||
| Know that PCV13 is not the vaccine for COVID-19 | ||||
| No | 406 (35.68) | 2057.00 (613.00–2588.00) | 264.18 | 0.042 |
| Yes | 732 (64.32) | 2588.00 (842.00–2588.00) | Ref | |
| Know PCV13 | ||||
| No | 693 (60.90) | 1640.00 (593.00–2588.00) | −434.90 | 0.001 |
| Yes | 445 (39.10) | 2588.00 (1114.00–2588.00) | Ref | |
| Motivation for vaccination | ||||
| Intention to get the child vaccinated with PCV13 | ||||
| Hesitancy | 242 (21.27) | 903.50 (346.00–2588.00) | −674.59 | <0.001 |
| Acceptance | 896 (78.73) | 2588.00 (971.00–2588.00) | Ref | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.; Ma, Y.; Li, W.; Tang, G.; Jiang, Y.; Li, H.; Jiang, S.; Zhou, Y.; Yang, Y.; Zhang, T.; et al. Caregiver Willingness to Vaccinate Children with Pneumococcal Vaccines and to Pay in a Low-Resource Setting in China: A Cross-Sectional Study. Vaccines 2022, 10, 1897. https://doi.org/10.3390/vaccines10111897
Li L, Ma Y, Li W, Tang G, Jiang Y, Li H, Jiang S, Zhou Y, Yang Y, Zhang T, et al. Caregiver Willingness to Vaccinate Children with Pneumococcal Vaccines and to Pay in a Low-Resource Setting in China: A Cross-Sectional Study. Vaccines. 2022; 10(11):1897. https://doi.org/10.3390/vaccines10111897
Chicago/Turabian StyleLi, Linqiao, Yuan Ma, Wei Li, Guorong Tang, Yan Jiang, Huangcui Li, Shuxiang Jiang, Yun Zhou, Yuan Yang, Ting Zhang, and et al. 2022. "Caregiver Willingness to Vaccinate Children with Pneumococcal Vaccines and to Pay in a Low-Resource Setting in China: A Cross-Sectional Study" Vaccines 10, no. 11: 1897. https://doi.org/10.3390/vaccines10111897
APA StyleLi, L., Ma, Y., Li, W., Tang, G., Jiang, Y., Li, H., Jiang, S., Zhou, Y., Yang, Y., Zhang, T., Yang, W., Ma, L., & Feng, L. (2022). Caregiver Willingness to Vaccinate Children with Pneumococcal Vaccines and to Pay in a Low-Resource Setting in China: A Cross-Sectional Study. Vaccines, 10(11), 1897. https://doi.org/10.3390/vaccines10111897







