The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
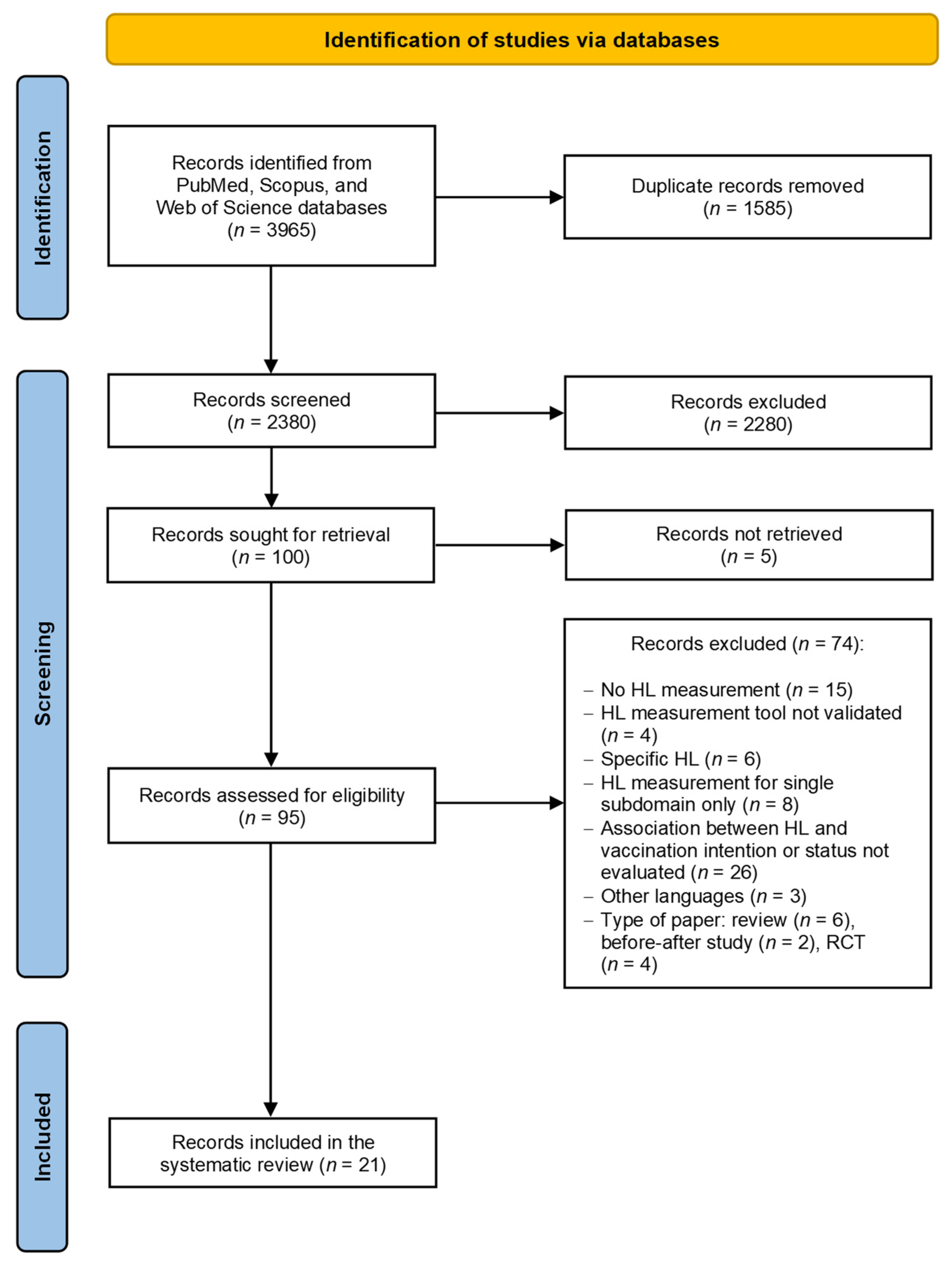
2.1. Search Strategy and Study Selection
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Quality Assessment
3. Results
3.1. Characteristics of the Studies Included
3.1.1. Intention to Vaccinate
3.1.2. Vaccination Status
3.2. Association between HL and Vaccination Behavior
3.2.1. Intention to Vaccinate
3.2.2. Vaccination Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Renzi, E.; Baccolini, V.; Migliara, G.; Bellotta, C.; Ceparano, M.; Donia, P.; Marzuillo, C.; De Vito, C.; Villari, P.; Massimi, A. Mapping the Prevalence of COVID-19 Vaccine Acceptance at the Global and Regional Level: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 1488. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Vaccine Action Plan: Monitoring, Evaluation and Accountability: Secretariat Annual Report 2020; World Health Organization (WHO): Geneva, Switzerland, 2020; ISBN 9789240014329. [Google Scholar]
- Amanna, I.J.; Slika, M.K. Successful Vaccines. Curr. Top. Microbiol. Immunol. 2020, 428, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Galles, N.C.; Liu, P.Y.; Updike, R.L.; Fullman, N.; Nguyen, J.; Rolfe, S.; Sbarra, A.N.; Schipp, M.F.; Marks, A.; Abady, G.G.; et al. Measuring routine childhood vaccination coverage in 204 countries and territories, 1980–2019: A systematic analysis for the Global Burden of Disease Study 2020, Release 1. Lancet 2021, 398, 503–521. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Monthly Measles and Rubella Monitoring Report; Period covered: 1 March 2019–9 February 2020; Stock. ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- Baker, P.; Kelly, D.; Medeiros, R.; Morrissey, M.; Price, R. Eliminating HPV-caused cancers in Europe: Achieving the possible. J. Cancer Policy 2021, 28, 100280. [Google Scholar] [CrossRef]
- Lindstrand, A.; Cherian, T.; Chang-Blanc, D.; Feikin, D.; O’brien, K.L. The World of Immunization: Achievements, Challenges, and Strategic Vision for the Next Decade. J. Infect. Dis. 2021, 224, S452–S467. [Google Scholar] [CrossRef]
- World Health Organization. Immunization Agenda 2030—A Global Strategy to Leave no One Behind; WHO: Geneva, Switzerland, 2021; pp. 1–58. [Google Scholar]
- Rosso, A.; Massimi, A.; Pitini, E.; Nardi, A.; Baccolini, V.; Marzuillo, C.; De Vito, C.; Villari, P. Factors affecting the vaccination choices of pregnant women for their children: A systematic review of the literature. Hum. Vaccines Immunother. 2020, 16, 1969–1980. [Google Scholar] [CrossRef]
- Shet, A.; Carr, K.; Danovaro-Holliday, M.C.; Sodha, S.V.; Prosperi, C.; Wunderlich, J.; Wonodi, C.; Reynolds, H.W.; Mirza, I.; Gacic-Dobo, M.; et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: Evidence of disruption and recovery from 170 countries and territories. Lancet Glob. Health 2022, 10, e186–e194. [Google Scholar] [CrossRef]
- Causey, K.; Fullman, N.; Sorensen, R.J.D.; Galles, N.C.; Zheng, P.; Aravkin, A.; Danovaro-Holliday, M.C.; Martinez-Piedra, R.; Sodha, S.V.; Velandia-González, M.P.; et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: A modelling study. Lancet 2021, 398, 522–534. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlôt, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef]
- Reno, C.; Maietti, E.; Fantini, M.P.; Savoia, E.; Manzoli, L.; Montalti, M.; Gori, D. Enhancing COVID-19 vaccines acceptance: Results from a survey on vaccine hesitancy in northern Italy. Vaccines 2021, 9, 378. [Google Scholar] [CrossRef]
- Rosso, A.; Massimi, A.; De Vito, C.; Adamo, G.; Baccolini, V.; Marzuillo, C.; Vacchio, M.R.; Villari, P. Knowledge and attitudes on pediatric vaccinations and intention to vaccinate in a sample of pregnant women from the City of Rome. Vaccine 2019, 37, 1954–1963. [Google Scholar] [CrossRef] [PubMed]
- Pitini, E.; Baccolini, V.; Rosso, A.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. How public health professionals view mandatory vaccination in italy—A cross-sectional survey. Vaccines 2021, 9, 580. [Google Scholar] [CrossRef] [PubMed]
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Tsouros, A.D. Health Literacy: The Solid Facts; World Health Organization: Copenhagen, Denmark, 2013. [Google Scholar]
- Baccolini, V.; Rosso, A.; Di Paolo, C.; Isonne, C.; Salerno, C.; Migliara, G.; Prencipe, G.; Massimi, A.; Marzuillo, C.; De Vito, C.; et al. What is the Prevalence of Low Health Literacy in European Union Member States? A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 36, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Stormacq, C.; Van Den Broucke, S.; Wosinski, J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot. Int. 2019, 34, e1–e17. [Google Scholar] [CrossRef]
- Santana, S.; Brach, C.; Harris, L.; Ochiai, E.; Blakey, C.; Bevington, F.; Kleinman, D.; Pronk, N. Updating Health Literacy for Healthy People 2030: Defining Its Importance for a New Decade in Public Health. J. Public Health Manag. Pract. 2021, 27, S258–S264. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC) What Is Health Literacy? Available online: https://www.cdc.gov/healthliteracy/learn/index.html# (accessed on 14 July 2022).
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Baccolini, V.; Isonne, C.; Salerno, C.; Giffi, M.; Migliara, G.; Mazzalai, E.; Turatto, F.; Sinopoli, A.; Rosso, A.; De Vito, C.; et al. The association between adherence to cancer screening programs and health literacy: A systematic review and meta-analysis. Prev. Med. 2022, 155, 106927. [Google Scholar] [CrossRef]
- Lorini, C.; Santomauro, F.; Donzellini, M.; Capecchi, L.; Bechini, A.; Boccalini, S.; Bonanni, P.; Bonaccorsi, G. Health literacy and vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 478–488. [Google Scholar] [CrossRef]
- Rowlands, G. Health literacy: Ways to maximise the impact and effectiveness of vaccination information. Hum. Vaccines Immunother. 2014, 10, 2130–2135. [Google Scholar] [CrossRef]
- Mccormack, L.; Haun, J.; Sørensen, K.; Valerio, M. Recommendations for advancing health literacy measurement. J. Health Commun. 2013, 18, 9–14. [Google Scholar] [CrossRef]
- Kiechle, E.S.; Bailey, S.C.; Hedlund, L.A.; Viera, A.J.; Sheridan, S.L. Different Measures, Different Outcomes? A Systematic Review of Performance-Based versus Self-Reported Measures of Health Literacy and Numeracy. J. Gen. Intern. Med. 2015, 30, 1538–1546. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021); Cochrane: Chichester, UK, 2021. [Google Scholar]
- Sørensen, K.; Van Den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 6 May 2022).
- Aslantekin-özçoban, F.; Uluşen, M.; Yalnız-dilcen, H.; Çilesiz, E. Are midwifery students ready for the COVID-19 vaccine? The decision to vaccinate and affecting factors. Hum. Vaccin. Immunother. 2021, 17, 4896–4903. [Google Scholar] [CrossRef] [PubMed]
- Arvanitis, M.; Opsasnick, L.; Conor, R.O.; Curtis, L.M.; Vuyyuru, C.; Yoshino, J.; Bailey, S.C.; Jean-jacques, M.; Wolf, M.S. Factors associated with COVID-19 vaccine trust and hesitancy among adults with chronic conditions. Prev. Med. Rep. 2021, 24, 101484. [Google Scholar] [CrossRef]
- Fukuda, Y.; Ando, S.; Fukuda, K. Knowledge and preventive actions toward COVID-19, vaccination intent, and health literacy among educators in Japan: An online survey. PLoS ONE 2021, 16, e0257552. [Google Scholar] [CrossRef]
- Longchamps, C.; Ducarroz, S.; Crouzet, L.; Vignier, N.; Pourtau, L.; Allaire, C.; Colleville, A.C. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine 2021, 39, 3315–3318. [Google Scholar] [CrossRef]
- Montagni, I.; Mebarki, A.; Texier, N.; Schück, S.; Tzourio, C. Acceptance of a COVID-19 vaccine is associated with ability to detect fake news and health literacy. J. Public Health 2021, 43, 695–702. [Google Scholar] [CrossRef]
- Patil, U.; Kostareva, U.; Hadley, M.; Manganello, J.A.; Okan, O.; Dadaczynski, K.; Massey, P.M.; Agner, J.; Sentell, T. Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U. S. College Students: Implications for Interventions. Int. J. Environ. Res. Public Health 2021, 18, 3301. [Google Scholar] [CrossRef]
- Scott, T.L.; Gazmararian, J.A.; Williams, M.V.; Baker, D.W. Health literacy and preventive health care use among medicare enrollees in a managed care organization. Med. Care 2002, 40, 395–404. [Google Scholar] [CrossRef]
- Howard, D.H.; Sentell, T.; Gazmararian, J.A.; Florida, S. Impact of Health Literacy on Socioeconomic and Racial Differences in Health in an Elderly Population. J. Gen. Intern. Med. 2006, 21, 857–861. [Google Scholar] [CrossRef] [PubMed]
- O’Conor, R.; Muellers, K.; Arvanitis, M.; Vicencio, D.P.; Wolf, M.S.; Wisnivesky, J.P.; Federman, A.D. Effects of health literacy and cognitive abilities on COPD self-management behaviors: A prospective cohort study. Respir. Med. 2019, 160, 105630. [Google Scholar] [CrossRef] [PubMed]
- Omar, R.; Said, M.A.; Mohammadi, N.A. Factors Associated with Influenza Vaccination Uptake among Healthcare Worker in Tertiary Hospitals in Perak, Malaysia. ASM Sci. J. 2020, 13, 130–141. [Google Scholar] [CrossRef]
- Rafferty, A.P.; Winterbauer, N.L.; Luo, H.; Bell, R.A.; Little, N.R.G. Diabetes Self-Care and Clinical Care Among Adults With Low Health Literacy. J. Public Health Manag. Pract. 2019, 27, 144–153. [Google Scholar] [CrossRef]
- Pati, S.; Huang, J.; Wong, A.; Baba, Z.; Ostapenko, S.; Fiks, A.G.; Cnaan, A. Do changes in socio-demographic characteristics impact up-to-date immunization status between 3 and 24 months of age? A prospective study among an inner-city birth cohort in the United States. Hum. Vaccin. Immunother. 2017, 13, 1141–1148. [Google Scholar] [CrossRef]
- White, S.; Chen, J.; Atchison, R. Relationship of Preventive Health Practices and Health Literacy: A National Study. Am. J. Health Behav. 2008, 32, 227–242. [Google Scholar] [CrossRef]
- Bennett, I.M. The Contribution of Health Literacy to Disparities in Self-Rated Health Status and Preventive Health Behaviors in Older Adults. Ann. Fam. Med. 2009, 7, 204–211. [Google Scholar] [CrossRef]
- Pati, S.; Feemster, K.A.; Mohamad, Z. Maternal Health Literacy and Late Initiation of Immunizations among an Inner-City Birth Cohort. Matern. Child Health J. 2010, 15, 386–394. [Google Scholar] [CrossRef]
- Amit, A.; Nehama, H.; Rishpon, S.; Baron-epel, O. Patient Education and Counseling Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Educ. Couns. 2017, 100, 768–775. [Google Scholar] [CrossRef]
- Moran, M.B.; Chatterjee, S.J.; Frank, L.B.; Murphy, S.T.; Zhao, N.; Chen, N.; Ball-Rokeach, S. Individual, Cultural and Structural Predictors of Vaccine Safety Confidence and Influenza Vaccination Among Hispanic Female Subgroups. J. Immigr. Minority Health 2017, 19, 790–800. [Google Scholar] [CrossRef]
- Widdice, L.E.; Hoagland, R.; Callahan, S.T.; Kahn, J.A.; Harrison, C.J.; Pahud, B.A.; Frey, S.E.; Berry, A.A.; Kotloff, K.L.; Edwards, K.M.; et al. Caregiver and adolescent factors associated with delayed completion of the three-dose human papillomavirus vaccination series. Vaccine 2018, 36, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Castro-sánchez, E.; Vila-candel, R.; Soriano-vidal, F.J.; Navarro-illana, E.; Díez-domingo, J. Influence of health literacy on acceptance of influenza and pertussis vaccinations: A cross-sectional study among Spanish pregnant women. BMJ Open 2018, 8, e022132. [Google Scholar] [CrossRef] [PubMed]
- Song, I.G.; Lee, H.; Yi, J.; Kim, M.S.; Kawachi, I.; Park, M. Health literacy and use of preventive health services among North Korean defectors in the Republic of Korea. PLoS ONE 2018, 13, e0195964. [Google Scholar] [CrossRef]
- Lorini, C.; Collini, F.; Gasparini, F.; Paolini, D.; Grazzini, M.; Ierardi, F.; Galletti, G.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines 2020, 8, 154. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control Facilitating COVID-19 Vaccination Acceptance and Uptake in the EU/EEA; Stock. ECDC: Stockholm, Sweden, 2021.
- Baker, D.W.; Gazmararian, J.A.; Williams, M.V.; Scott, T.; Parker, R.M.; Green, D.; Ren, J.; Peel, J. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am. J. Public Health 2002, 92, 1278–1283. [Google Scholar] [CrossRef] [PubMed]
- Bostock, S.; Steptoe, A. Association between low functional health literacy and mortality in older adults: Longitudinal cohort study. BMJ 2012, 344, e1602. [Google Scholar] [CrossRef]
- Sentell, T.; Braun, K.L.; Davis, J.; Davis, T. Health literacy and meeting breast and cervical cancer screening guidelines among Asians and whites in California. Springerplus 2015, 4, 432. [Google Scholar] [CrossRef]
- Dai, H.; Saccardo, S.; Han, M.A.; Roh, L.; Raja, N.; Vangala, S.; Modi, H.; Pandya, S.; Sloyan, M.; Croymans, D.M. Behavioural nudges increase COVID-19 vaccinations. Nature 2021, 597, 404–409. [Google Scholar] [CrossRef]
- Sheeran, P. Intention—Behavior Relations: A Conceptual and Empirical Review European Review of Social Psychology. Eur. Rev. Soc. Psychol. 2011, 12, 1–36. [Google Scholar] [CrossRef]
- Osborne, R.H.; Cheng, C.C.; Nolte, S.; Elmer, S.; Besancon, S.; Budhathoki, S.S.; Debussche, X.; Dias, S.; Kolar, P.; Loureiro, M.I.; et al. Health literacy measurement: Embracing based approach diversity in a strengths- to promote health and equity, and avoid epistemic injustice. BMJ Glob. Health 2022, 7, e009623. [Google Scholar] [CrossRef]
- Altin, S.V.; Finke, I.; Kautz-Freimuth, S.; Stock, S. The evolution of health literacy assessment tools: A systematic review. BMC Public Health 2014, 14, 1207. [Google Scholar] [CrossRef] [PubMed]
- Ndwandwe, D.; Wiysonge, C.S. COVID-19 vaccines. Curr. Opin. Immunol. 2021, 71, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Thornton, J. COVID-19: Trust in government and other people linked with lower infection rate and higher vaccination uptake. BMJ 2022, 376, o292. [Google Scholar] [CrossRef] [PubMed]
- Penţa, M.A.; Băban, A. Message Framing in Vaccine Communication: A Systematic Review of Published Literature. Health Commun. 2018, 33, 299–314. [Google Scholar] [CrossRef]
- Olson, O.; Berry, C.; Kumar, N. Addressing parental vaccine hesitancy towards childhood vaccines in the united states: A systematic literature review of communication interventions and strategies. Vaccines 2020, 8, 590. [Google Scholar] [CrossRef]
- Mcgee, L.U. Communication Strategies to Address Vaccine Hesitancy in Healthcare Settings and on Social Media Communication Strategies to Address Vaccine Hesitancy in Healthcare Settings. J. Appl. Res. Child. 2019, 10, 7. [Google Scholar]
- Marlow, L.A.V.; Waller, J.; Evans, R.E.C.; Wardle, J. Predictors of interest in HPV vaccination: A study of British adolescents. Vaccine 2009, 27, 2483–2488. [Google Scholar] [CrossRef]
- Danis, K.; Georgakopoulou, T.; Stavrou, T.; Laggas, D.; Panagiotopoulos, T. Predictors of Childhood Vaccination Uptake: A Cross-sectional Study in Greece. Procedia Vaccinol. 2010, 2, 86–91. [Google Scholar] [CrossRef][Green Version]
- Nasreen, S.; Gebretekle, G.B.; Lynch, M.; Kurdina, A.; Thomas, M.; Fadel, S.; Houle, S.K.D.; Waite, N.M.; Crowcroft, N.S.; Allin, S. Understanding predictors of pneumococcal vaccine uptake in older adults aged 65 years and older in high-income countries across the globe: A scoping review. Vaccine 2022, 40, 4380–4393. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention—National Center for Immunization and Respiratory Diseases (NCIRD) Influenza Vaccination: A Summary for Clinicians. Available online: http://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm (accessed on 22 July 2022).
- Smetana, J.; Chlibek, R.; Shaw, J. In fl uenza vaccination in the elderly. Hum. Vaccin Immunother. 2018, 14, 540–549. [Google Scholar] [CrossRef]
- Baccolini, V.; Sindoni, A.; Adamo, G.; Rosso, A.; Massimi, A.; Bella, A.; Filia, A.; Magurano, F.; Marzuillo, C.; Villari, P.; et al. Measles among healthcare workers in Italy: Is it time to act? Hum. Vaccines Immunother. 2020, 16, 2618–2627. [Google Scholar] [CrossRef] [PubMed]
- Sindoni, A.; Baccolini, V.; Adamo, G.; Massimi, A.; Migliara, G.; De Vito, C.; Marzuillo, C.; Villari, P. Effect of the mandatory vaccination law on measles and rubella incidence and vaccination coverage in Italy (2013–2019). Hum. Vaccines Immunother. 2022, 18, 1950505. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Rizzo, C.; Rosselli, R.; Battista, T.; Conforto, A.; Cimino, L.; Poscia, A.; Fiacchini, D. Ten Actions to Counteract Vaccine Hesitancy Suggested by the Italian Society of Hygiene, Preventive Medicine, and Public Health. Vaccines 2022, 10, 1030. [Google Scholar] [CrossRef] [PubMed]
- Bechini, A.; Bonanni, P.; Lauri, S.; Tiscione, E.; Levi, M.; Prato, R.; Fortunato, F.; Martinelli, D.; Gasparini, R.; Panatto, D.; et al. Strategies and actions of multi-purpose health communication on vaccine preventable infectious diseases in order to increase vaccination coverage in the population: The ESCULAPIO project. Hum. Vaccines Immunother. 2017, 13, 369–375. [Google Scholar] [CrossRef] [PubMed][Green Version]
| First Author, Year | Country | Study Design | Target Population | Vaccination | Study Quality |
|---|---|---|---|---|---|
| Aslantekin-Özçoban, 2021 | Turkey | CS | Midwifery students (N = 1891) | SARS-CoV-2 | 8 |
| Arvanitis, 2021 | USA | CS | Older adults with one or more chronic diseases recruited from a community of academic clinics (N = 601) | SARS-CoV-2 | 8 |
| Fukuda, 2021 | Japan | CS | School, college and university educators aged 20–60 years (N = 1000) | SARS-CoV-2 | 9 |
| Longchamps, 2021 | France | CS | Homeless people aged ≥18 years recruited from short and long-term homeless shelters (N = 235) | SARS-CoV-2 | 7 |
| Montagni, 2021 | France | CS | Adults >18 years from the general population enrolled from PBS (N = 1647) | SARS-CoV-2 | 6 |
| Patil, 2021 | USA | CS | College students (N = 256) | SARS-CoV-2 | 8 |
| First Author, Year | Country | Study Design | Target Population | Vaccination | Study Quality |
|---|---|---|---|---|---|
| Scott, 2002 | US | Cross-sectional | Community-dwelling Medicare aged ≥65 years enrolled in a national managed care organization (N = 2722) | Influenza, pneumococcal | 8 |
| Howard, 2006 | US | Retrospective cohort | Community-dwelling Medicare aged ≥65 years enrolled in a national managed care organization (N = 3260) | Influenza, pneumococcal | 8 |
| White, 2008 | US | Cross-sectional | Individuals aged ≥16 years enrolled from PBS (N = 18,100) | Influenza, pneumococcal | 8 |
| Bennett, 2009 | US | Cross-sectional | Individuals aged ≥65 years enrolled from PBS (N = 2668) | Influenza | 9 |
| Pati, 2010 | US | Prospective cohort | Medicaid-eligible mothers recruited in urban hospital (N = 506) | Hexavalent | 9 |
| Amit Aharon, 2017 | Israel | Case-control | Parents recruited from a health registry (N = 731) | DTPa + HBV + MMR | 7 |
| Moran, 2017 | US | Cross-sectional | Hispanic women aged between 21 and 50 years recruited in clinics and community sites (N = 1565) | Influenza | 7 |
| Pati, 2017 | US | Prospective cohort | Medicaid-eligible mothers recruited in urban hospital (N = 693) | Hexavalent + MMR + pneumococcal | 8 |
| Widdice, 2018 | US | Cross-sectional | Caregivers enrolled at time of the third dose vaccination recruited in pediatric adolescent and family medicine practices (N = 422) | HPV | 8 |
| Castro-Sánchez, 2018 | Spain | Cross-sectional | Pregnant women recruited in maternity wards (N = 119) | Influenza, pertussis | 9 |
| Song, 2018 | South Korea | Cross-sectional | Adult North Korean defectors (N = 399) | Influenza | 6 |
| O’Conor, 2019 | US | Prospective cohort | Adults with COPD recruited in a community clinic (N = 388) | Influenza, pneumococcal | 8 |
| Rafferty, 2019 | US | Cross-sectional | Adult diabetic patients (N = 4397) | Influenza | 8 |
| Omar, 2020 | Malaysia | Cross-sectional | Healthcare workers (N = 775) | Influenza | 10 |
| Lorini, 2020 a | Italy | Cross-sectional | Healthcare workers (N = 711) | Influenza | 6 |
| Author, Year | HL | Vaccination Intention | Statistical Analysis | Main Findings | Adjustment Factors | ||
|---|---|---|---|---|---|---|---|
| Measurement α | Coding | Measurement | Coding | ||||
| Aslantekin-Özçoban, 2021 | HLS-EU-Q25 | Continuous | Nine questions investigating trust, perceived effectiveness, and benefits of the COVID-19 vaccination | Vaccination attitude scale (score: 0–5): - low score: negative attitude - high score: positive attitude | Multivariable linear regression | Non-significant association between HL and vaccination attitude (aβ = 0.027, p = 0.188) | Attitudes towards COVID-19 vaccine; perception of COVID-19 causes |
| Arvanitis, 2021 | NVS | Three categories: - low - marginal - adequate | Two questions: - “I trust that any future coronavirus vaccine will be safe and effective” - “I will be vaccinated for the coronavirus as soon as a vaccine becomes available” | Vaccination agreement scale (score: 0–10): - low score: no agreement - high score: total agreement | ANOVA | Non-significant association between HL and vaccination agreement (p = 0.06) | / |
| Fukuda, 2021 | HLS-EU-Q47 | Continuous | One question relating to the timing of vaccination intention after inoculation availability | Vaccination intention scale (score: 1–5): - low score: will not inoculate - high score: immediately | Multivariable linear regression | Significant association between higher HL and vaccination intention (aβ = 0.021, p < 0.001) | Gender; age; academic background; being under care of physician |
| Longchamps, 2021 | HLQ | Two categories: - low - intermediate or high | One question: “If a vaccine existed, would you be willing to get vaccinated?” | Two categories of vaccination intention: - yes: not hesitant - no or I don’t know: vaccine hesitant | Multivariable logistic regression | Significant association between intermediate/high HL and vaccine hesitancy (aOR = 0.38, 95% CI: 0.21–0.68) | Gender; family composition; administrative status |
| Montagni, 2021 | 5-item scale developed by the French Public Health Agency | Two categories: - bad - good | One question: “Would you be willing to get vaccinated against coronavirus even if the vaccine has not yet been fully proven effective?” | Three categories of vaccination intention: - yes: pro-vaccination - I don’t know: vaccine hesitant - no: anti-vaccination | Multinomial logistic regression | - Significant association between poor HL and being vaccine hesitant vs. pro-vaccination (aRRR = 1.44, 95% CI: 1.04–2.00) - Non-significant association between poor HL and being anti-vaccination vs. pro-vaccination (aRRR = 1.25, 95% CI: 0.96–1.63) | Gender; being regularly vaccinated against the flu; having an up-to-date vaccination; studying or working in the health domain, capacity to detect fake news |
| Patil, 2021 | SILS | Two categories: - low - adequate | One question: “How likely would you be to get a COVID-19 vaccine, if available?” | Two categories of vaccination intention: - very likely: willing to undergo vaccination - somewhat or not likely: vaccine hesitant | Multivariable logistic regression | Non-significant association between low HL and likelihood to vaccinate (aOR = 0.88, 95% CI: 0.50–1.56) | Social network size; gender; race/ethnicity; disability; first generation university student status; political affiliation |
| Author, Year | HL | Vaccination Status | Statistical Analysis | Main Findings | Adjustment Factors β | ||
|---|---|---|---|---|---|---|---|
| Measurement α | Coding | Measurement | Coding | ||||
| Influenza | |||||||
| Scott, 2002 | S-TOFHLA | Three categories: - inadequate - marginal - adequate | One SR question: having ever received the vaccination | Two categories of vaccination status: - yes - no | Multivariable logistic regression | - Significant association between inadequate HL and no vaccination uptake (aOR = 1.4, 95% CI: 1.1–1.9) - Non-significant association between marginal HL and no vaccination uptake (aOR = 1.0, 95% CI: 0.7–1.4) | AGR, education, income, physician visit (last 3 months), MMSE, chronic condition, IADL limitation |
| Howard, 2006 | S-TOHFLA | Three categories: - inadequate - marginal - adequate | One SR question: having ever received the vaccination | Two categories of vaccination status: - yes - no | Multivariable logistic regression | - Significant association between inadequate HL and vaccination uptake (aOR = 0.76, p = 0.020) - Non-significant association between marginal HL and vaccination uptake (aOR = 1.06, p = 0.707) | AGR, education, income, tobacco consumption, chronic conditions, area of residence |
| White, 2008 | NAAL | Continuous | One SR question: having received the vaccination in the previous year | Two categories of vaccination status: - yes - no | Marginal maximum likelihood probit regression | - Adults aged <40 years: significant association between higher HL and vaccination uptake (aβ = −0.07, p < 0.05) - Adults aged 40–64 years: non-significant association between higher HL and vaccination uptake (aβ = 0.01, p > 0.05) - Adults aged >65 years: significant association between higher HL and vaccination uptake (aβ = 0.17, p < 0.05) | AGR, health status, poverty level, insurance coverage, oral reading fluency |
| Bennett, 2009 | NAAL | Continuous | One SR question: having ever received the vaccination | Two categories of vaccination status: - yes - no | Marginal maximum likelihood probit regression | Significant association between higher HL and vaccination uptake (aβ = 0.14, p < 0.05) | AGR, education, income, US born |
| Moran, 2017 | SBSQ | Two categories: - inadequate - adequate | One SR question: frequency of vaccination against influenza | Two categories of frequency of vaccination: - almost always or always: regularly receiving vaccination - never, rarely, or sometimes: not regularly receiving vaccination | Multivariable logistic regression | Non-significant association between adequate HL and regularly receiving influenza vaccination (aOR = 1.12, 95% CI: 0.88–1.43) | Country of birth, educational level, annual income, age, health insurance, health state, fatalism, acculturation, years lived in the US, religiosity, confidence in the vaccine safety |
| Castro-Sánchez, 2018 | SAHLSA-50 | Continuous | Immunization status extracted from the vaccination registry | Two categories of vaccination status: - received the vaccination during pregnancy - did not receive the vaccination during pregnancy | Mann–Whitney U test | Significant association between higher HL and vaccination uptake (p = 0.019) | / |
| NVS | Continuous | Mann–Whitney U test | Non-significant association between higher HL and vaccination uptake (p = 0.320) | ||||
| SILS | Continuous | Mann–Whitney U test | Non-significant association between higher HL and vaccination uptake (p = 0.942) | ||||
| Song, 2018 | S-KHLS | Three categories: - low - intermediate - high | One SR question: having received the vaccination in the previous two years | Two categories of vaccination status: - yes - no | Multivariable logistic regression | - Significant association between intermediate HL and vaccination uptake (aOR = 2.44, 95% CI: 1.19–5.00) - Significant association between high HL and vaccination uptake (aOR = 2.10, 95% CI: 1.02–4.35) | Age, gender, marital status, duration of stay in other countries before entry, duration of stay in the Republic of Korea |
| O’Conor, 2019 | S-TOFHLA | Two categories: - limited - adequate | One SR question: having received the vaccination in the previous year | Two categories of vaccination status: - yes - no | GEE model for repeated measurements | Non-significant association between adequate HL and vaccination uptake (aOR =0.85, 95% CI: 0.62–1.18) | AGR, income, number of comorbidities, severity of COPD |
| Rafferty, 2019 | BRFSS | Two categories: - not low- low | One SR question: having received the vaccination in the previous year | Two categories of vaccination status: - yes - no | Multivariable logistic regression | Non-significant association between low HL and vaccination uptake (aOR = 0.98, 95% CI: 0.74–1.29) | AGR, education, household income, health status |
| Omar, 2020 | FCCHL | Continuous | One SR question: “Did you have an influenza vaccination between November 2016 and October 2017?” | Two categories of vaccination status: - yes - no | Multivariable logistic regression | Non-significant association between higher HL and vaccination uptake: - functional HL: aOR = 1.04, 95% CI: 0.79–1.37 - critical HL: aOR = 1.08, 95% CI: 0.76–1.53 - communicative HL: aOR = 0.98, 95% CI: 0.65–1.45 | AGR, religion, education, job category, department, income, chronic disease, marital status, smoking status, and living with person at high risk of getting influenza complications, knowledge, behavioral, HL variables |
| Lorini, 2020 | IMETER | Continuous | Three SR questions: having received the vaccination in 2016–2017, in 2017–2018, and intention to vaccinate in 2018–2019 | Three categories of vaccination behavior: - always get vaccinated - vaccinated at least once in the previous years or intended to vaccinate (sometimes) - never vaccinated and did not intend to vaccinate (never) | Multinomial logistic regression | - Non-significant association between higher HL and vaccination behavior (sometimes vs. never: aRRR = 0.99, 95% CI: 0.97-1-01) - Non-significant association between higher HL and vaccination behavior (always vs. never: aRRR = 0.98, 95% CI: 0.95–1.01) | Gender, age, mother language |
| Pneumococcal | |||||||
| Scott, 2002 | S-TOFHLA | Three categories: - inadequate - marginal - adequate | One SR question: having ever received the vaccination | Two categories of vaccination status: - yes - no | Multivariable logistic regression | - Significant association between inadequate HL and no vaccination uptake (aOR = 1.3, 95% CI: 1.1–1.7) - Non-significant association between marginal HL and no vaccination uptake (aOR = 1.2, 95% CI: 0.9–1.7) | AGR, education, income, physician visit (last 3 months), MMSE, chronic condition, IADL limitation |
| Howard, 2006 | S-TOFHLA | Three categories: - inadequate - marginal - adequate | One SR question: having ever received the vaccination | Two categories of vaccination status: - yes - no | Multivariable logistic regression | - Non-significant association between inadequate HL and vaccination uptake (aOR = 0.85, p = 0.114) - Non-significant association between marginal HL and vaccination uptake (aOR = 0.91, p = 0.445) | AGR, education, income, tobacco consumption, chronic conditions, area of residence |
| White, 2008 | NAAL | Continuous | One SR question: having received the vaccination in the previous year | Two categories of vaccination status: - yes - no | Marginal maximum likelihood probit regression | Non-significant association between higher HL and vaccination uptake (aβ = −0.01, p > 0.05) | AGR, health status, poverty level, insurance coverage, oral reading fluency |
| O’Conor, 2019 | S-TOFHLA | Two categories: - limited - adequate | One SR question: having ever received the vaccination | Two categories of vaccination status: - yes - no | GEE models for repeated measurements | Non-significant association between adequate HL and vaccination uptake (aOR = 1.01, 95% CI: 0.64–1.60) | AGR, income, number of comorbidities, severity of COPD |
| HPV | |||||||
| Widdice, 2018 | REALM | Three categories of HL grade equivalent: - 6th grade or below (very low) - 7th to 8th grade (low) - high school | One SR question: time to completion of three doses (days between the first and third dose) | Four categories of time to completion of vaccination cycle: - not delayed (≤12 months) - delayed (12–24 months) - delayed (24–36 months) - delayed (>36 months) | Multinomial logistic regression | - Non-significant association between very low HL and delayed completion of vaccination cycle - Non-significant association between low HL and delayed completion of vaccination cycle | Race, caregiver education, adolescent insurance, gap in adolescent insurance since HPV dose, number of parents in household, parents’ marital status, adolescent health visits in the previous year, appointment availability, caregiver ability to obtain timely appointments for adolescent’s medical care, ability to get through on the telephone |
| Hexavalent | |||||||
| Pati, 2010 | S-TOFHLA | Two categories: - inadequate or marginal - adequate | Immunization status extracted from vaccination registry | Two categories for up-to-date vaccination status at 3 and 7 months: - yes - no | Multivariable logistic regression | Non-significant association between higher maternal HL and child’s up-to-date immunization status: - 3 months (aOR = 1.08, 95% CI: 0.67–1.76) - 7 months (aOR = 0.92, 95% CI: 0.57–1.48) | Maternal race/ethnicity, age, education, receiving antenatal care, participation in WIC program, marital status, location of the infant’s health care facility, vaccination status at the age of 3 months (for 7 months model only) |
| Hexavalent + MMR + Pneumococcal | |||||||
| Pati, 2017 | S-TOFHLA | Two categories: - inadequate or marginal - adequate | Immunization status extracted from vaccination registry | Two categories for up-to-date vaccination status at 24 months: - yes - no | Chi-square test | Non-significant association between maternal HL and child’s up-to-date immunization status at 24 months | / |
| DTPa + MMR + HBV | |||||||
| Amit Aharon, 2017 | VHLS | Continuous | Immunization status extracted from vaccination registry | Completion of vaccination protocol at 2 years: - yes - no | Path analysis | - Significant association between higher communicative HL and completion of vaccination protocol at 2 years (β = 0.06, p < 0.05) - Functional HL and critical HL had an indirect effect, mediated through other variables, on completion of the vaccination protocol at 2 years | NA |
| Pertussis | |||||||
| Castro-Sánchez, 2018 | SAHLSA-50 | Continuous | Immunization status extracted from vaccination registry | Two categories of vaccination status: - received the vaccination during pregnancy - did not receive the vaccination during pregnancy | Mann–Whitney U test | Significant association between higher HL and vaccination uptake (p < 0.05) | / |
| NVS | Continuous | Mann–Whitney U test | Non-significant association between higher HL and vaccination uptake (p > 0.05) | ||||
| SILS | Continuous | Mann–Whitney U test | Non-significant association between higher HL and vaccination uptake (p > 0.05) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siena, L.M.; Isonne, C.; Sciurti, A.; De Blasiis, M.R.; Migliara, G.; Marzuillo, C.; De Vito, C.; Villari, P.; Baccolini, V. The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review. Vaccines 2022, 10, 1832. https://doi.org/10.3390/vaccines10111832
Siena LM, Isonne C, Sciurti A, De Blasiis MR, Migliara G, Marzuillo C, De Vito C, Villari P, Baccolini V. The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review. Vaccines. 2022; 10(11):1832. https://doi.org/10.3390/vaccines10111832
Chicago/Turabian StyleSiena, Leonardo Maria, Claudia Isonne, Antonio Sciurti, Maria Roberta De Blasiis, Giuseppe Migliara, Carolina Marzuillo, Corrado De Vito, Paolo Villari, and Valentina Baccolini. 2022. "The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review" Vaccines 10, no. 11: 1832. https://doi.org/10.3390/vaccines10111832
APA StyleSiena, L. M., Isonne, C., Sciurti, A., De Blasiis, M. R., Migliara, G., Marzuillo, C., De Vito, C., Villari, P., & Baccolini, V. (2022). The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review. Vaccines, 10(11), 1832. https://doi.org/10.3390/vaccines10111832






