Abstract
Influenza vaccination rates among Chinese middle school students are low. This study aims to explore the influencing factors of vaccination among middle school students and promote vaccination. We conducted a mixed-methods study, integrating a questionnaire survey among 9145 middle school students in four cities in China and semi-structured interviews with 35 middle school students to understand their attitudes and perceptions toward vaccination based on the Health Belief Model. We found the overall vaccination rate was 38.2% (3493/9145), with students in Beijing, boarding at school, or senior high school showing higher values than their counterparts (p < 0.05). Multiple logistic regression results showed that non-boarding (OR = 0.46, 95%CI: 0.42–0.51) and perceived barriers (OR = 0.97, 95%CI: 0.96–0.98) were unfavorable factors for influenza vaccination, whereas perceived susceptibility (OR = 1.07, 95%CI: 1.05–1.08), perceived benefits (OR = 1.02, 95%CI: 1.01–1.04), cues to action (OR = 1.08, 95%CI: 1.05–1.11), and self-efficacy (OR = 1.04, 95%CI: 1.02–1.07) were facilitators. Qualitative results indicated that positive health beliefs, school, and the home environment contribute to vaccination. In conclusion, the influenza vaccination rate among middle school students remains low. The concerns about the safety and potential side effects of vaccines are the main barriers to vaccination, underscoring the need for strengthening communication, education, and information among students and their teachers/parents.
1. Introduction
Influenza (flu) is a global health threat [1], causing almost 4 million infections and 650 thousand deaths worldwide each year [2,3]. According to statistics on influenza prevalence among 13,329 unvaccinated persons in 32 randomized controlled trials of influenza vaccination worldwide, symptomatic influenza prevalence was 12.7% in children, 4.4% in adults, and 7.2% in elderly [4], indicating that children are at a higher risk of getting influenza. Poor air ventilation in classrooms and close contact between students make schools a high-risk site for influenza outbreaks [5,6,7]. More than 90% of the influenza outbreaks reported each year in China occur in schools and childcare institutions [8]. School-age children have the highest rate of influenza infection compared to other populations [9]. School-age children play an important role in bridging influenza spread in schools, families, and communities. Influenza epidemics can cause large numbers of school-age children to be absent from school, and parents to be absent from work [10].
Vaccination is the most effective strategy to prevent the spread of influenza [11]. During the 2017–2018 flu season, influenza vaccinations prevented 7.1 million illnesses and 41% of the expected hospitalizations of young children in the United States [12]. Large-scale centralized influenza vaccination can greatly reduce the risk of an influenza outbreak when the vaccine strain matches the circulating strain [13]. Additionally, even when the strain of influenza in the vaccine does not exactly match the one that is circulating, it can still effectively lower the risk [14]. In recent years, to increase the uptake of the influenza vaccine in adolescent populations, many programs have been launched. The school-located influenza vaccination (SLIV) program in the United States offers the best option for achieving high-immunization coverage in a short period of time [7]. The seasonal influenza program in England recommends children aged between 2 and 16 to be vaccinated with a live attenuated influenza vaccine (LAIV) [15]. However, many countries have reported low influenza vaccination coverage [16,17,18], which is considerably below the target of more than 75% suggested by the World Health Organization (WHO) [19].
The Health Belief Model (HBM), developed by social psychologists in the 1850s, is one of the most widely used models to study the relationship between health behaviors and health service utilization [20]. This model explains health behaviors in the following ways: perceived susceptibility to disease, perceived severity of disease, perceived benefits of an intervention, perceived barriers to an intervention, cues to action, and self-efficacy [21]. Research has shown that education and health beliefs influence adolescent vaccination decisions [22]. Moreover, previous studies have identified HBM’s components as important predictors of influenza vaccination [23,24,25], and its constructs provide a theoretical framework of the interview outline as well [26,27]. In order to inform health policy development to improve influenza vaccination rates and protect middle school students from severe outcomes of influenza infection, we explored the influencing factors of influenza vaccination among middle school students through a mixed-methods study based on HBM.
2. Materials and Methods
2.1. Study Design, Population, and Settings
We conducted a cross-sectional survey among middle school students in four Chinese cities (Beijing, Xi’an in Shaanxi province, Shenzhen in Guangdong province, and Anqing in Anhui province) in December 2020 by using convenient cluster sampling. We used the Wenjuanxing® (Changsha Ranxing Information Technology Co., Ltd., Changsha, China) online survey tool (similar to SurveyMonkey®, San Mateo, CA, USA) to collect relevant information. We distributed 9463 questionnaires with informed consent. After excluding blank questionnaires (refusal to participate) and invalid questionnaires (incomplete responses), a total of 9145 questionnaires were analyzed (96.6%). Only Chinese schoolchildren were eligible, and only if they agreed to attend the survey, could read and comprehend the survey content, and were studying in ordinary middle schools rather than vocational schools.
Qualitative interviews were conducted from March to April 2021. A total of 35 middle school students from 4 schools in Dongcheng District, Beijing, were selected, using the purposive sampling method for semi-structured interviews, to investigate the influence of health belief factors on their vaccination decisions. Among them, 17 (48.6%) were boys, 18 (51.4%) were junior high school students, and 14 (40.0%) were boarding students. This study was approved by the Ethics Committee of Capital Medical University (Z2020SY116), and all participants signed the informed consent.
2.2. Questionnaire
The questionnaire consists of two parts. The first part contains demographic information, such as sex, grade, accommodation, region, and “whether to vaccinate against influenza this year (2020)”. The second part is a 20-item scale designed based on the HBM, using the Likert 5-level scoring method (Supplementary Material), including questions such as ”influenza vaccine will help me avoid missing class because of illness”, “I refused to get vaccinated because I was afraid of needles’ prick”, “TV news, WeChat subscriptions and other mass media say that the influenza vaccine is good for me and I should be vaccinated”, and “when I openly discuss vaccination with others, they may positively influence me”.
The Kaiser–Meyer–Olkin (KMO) value of the questionnaire was 0.853, and Bartlett’s Test of Sphericity’s p-value was <0.05, which is suitable for factor analysis. Exploratory factor analysis (EFA) with principal component analysis method using SAS 9.4 identified five dimensions: (1) perceived susceptibility, including three items, such as “I belong to a susceptible group” and “influenza vaccination is very important” (Cronbach’s alpha = 0.705); (2) perceived benefits, including four items, such as “influenza vaccine will help us avoid influenza” and “influenza vaccine will help save my parents’ time to care for me” (Cronbach’s alpha = 0.871); (3) perceived barriers, including seven items, such as “I am worried about adverse reactions after the influenza vaccination” and ” my classmates would observe me and I would feel embarrassed” (Cronbach’s alpha = 0.813); (4) cues to action, including three items, such as “according to the centers for disease control and prevention (CDC) public service announcement that getting the influenza vaccine is good for me and I should be vaccinated” and “The medical staff told me that the influenza vaccine is good for me and I should be vaccinated” (Cronbach’s alpha = 0.915); and (5) self-efficacy, including three items, such as “when I openly discuss vaccination with others, I will have a positive impact on the beliefs of others” and “I tend to listen to my parents about vaccinating or not” (Cronbach’s alpha = 0.713). The questionnaire has good reliability and the cumulative contribution rate of the five factors is 64%.
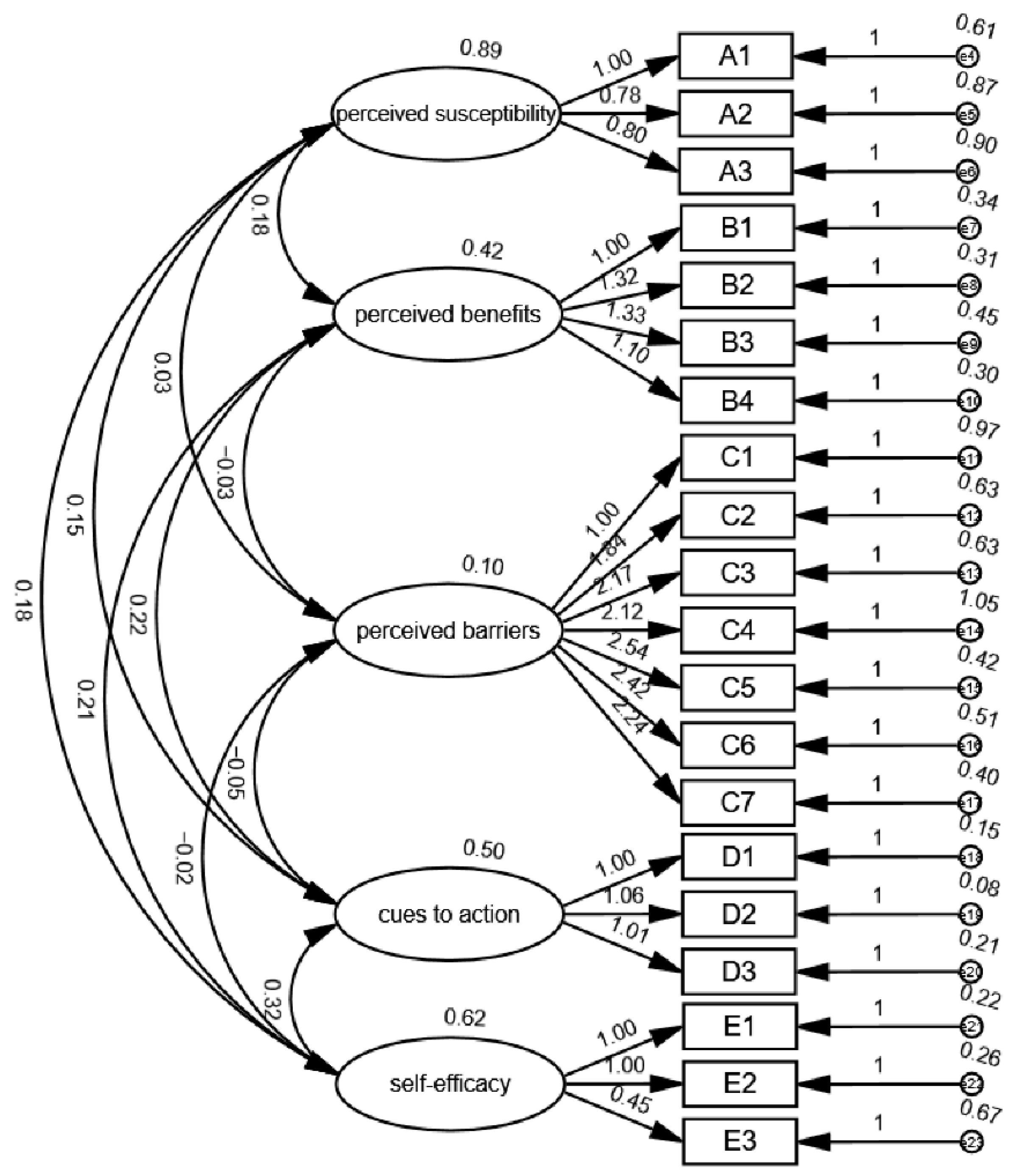
Confirmatory factor analysis (CFA) was performed using Amos 24. The results showed the goodness of fit index (GFI) = 0.955, adjusted goodness of fit index (AGFI) = 0.941, normed fit index (NFI) = 0.950, comparative fit index (CFI) = 0.952, incremental fit the index (IFI) = 0.952, and the root mean square error of approximation (RMSEA) = 0.051, indicating that the model fits well and has good construct validity (Figure 1).
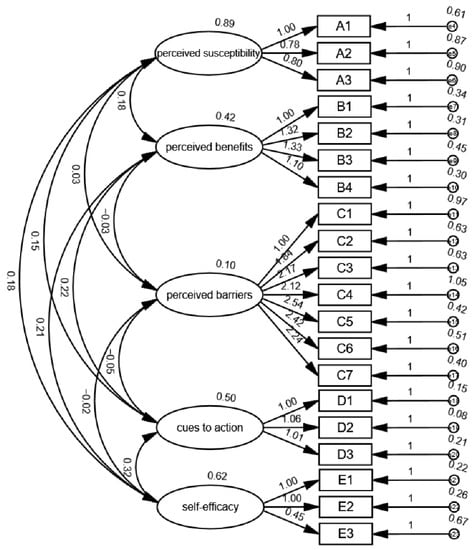
Figure 1.
Confirmatory factor analysis structural equation plot.
2.3. Qualitative Interview
The qualitative interview adopted a self-designed interview outline based on HBM, including questions such as “Did you receive the influenza vaccine last year (2020)?”, “When the school organizes influenza vaccination, will you ask the peers around you whether they are going to be vaccinated?”, and “Do your parents support your influenza vaccination?”. Before we issued the formal survey, we solicitated opinions and comments from experts and middle school teachers on the rationality of the interview questions, the commonality of language descriptions, and the explanatory power. Further, we conducted pre-interviewing among two middle school students to form the final interview outline. The interviewers obtained information through face-to-face interviews, using group interviews, with 4 to 8 students in each group; a total of 7 groups were interviewed. Each interview lasted about 15–20 min.
2.4. Quality Control
The questionnaire was designed based on the literature on HBM and had been revised several times for good reliability and validity. The questionnaire was self-administrated by the middle school students themselves, who were able to fully understand the relevant questions and make choices based on their personal judgement. The online survey is conducted through Wenjuanxing®, a SurveyMonkey®-like online survey tool in China, avoiding the efforts such as training of field staff for information collection and therefore reducing measurement errors. The closed-ended online questionnaire allows for coding of answers in a patched process, avoiding errors in manual data entry and ensuring the accuracy and authenticity of the data during data merging and analysis.
The interview outline was optimized and revised several times based on HBM and the research objectives. With the consent of the interviewees, we made recordings and transcribed these verbatim, verified with the interview transcripts. The interview process was conducted in a quiet and undisturbed environment.
2.5. Statistical Analysis
Data were compiled in Microsoft Excel and exported to Statistical Analysis System software (V.9.4, SAS Institute Inc., Cary, NC, USA) for cleaning and analysis. Descriptive analysis was performed. Frequency tables with percentages were generated for demographic categorical variables, while the mean and standard deviation (SD) were calculated for scores of each dimension in the HBM. A Chi-square test was applied to determine the association between the different demographic variables and influenza vaccination, whereas an independent t-test was conducted to analyze whether the dimensions of the HBM had differences between the groups receiving an influenza vaccine or not. A multiple logistic regression was performed to identify the associated factors of influenza vaccination, where the scores of each dimension of HBM were considered as independent variables and whether or not to receive an influenza vaccine was the dependent variable, with sex and accommodation used as adjustment factors in the model. A two-tailed p < 0.05 was considered statistically significant.
The analysis of the interview data moved from initial coding to focused coding, through to theoretical coding, resulting in the production of core concepts and categories using NVivo 11 qualitative analysis software, which was completed in line with the process set out within constructivist grounded theory [28].
3. Results
3.1. Demographic Characteristics of the Participants
Among the 9145 participants, 3493 (38.2%) received the influenza vaccine. There was no difference between boys and girls in influenza vaccination rate (p > 0.05). There were differences in vaccination rates between stage of schooling, region, and accommodation, where vaccination rates among students in senior high school, living in Beijing, and boarding at school were higher than those of their counterparts (p < 0.05) (Table 1).

Table 1.
Comparison of the influenza vaccination rates among middle school students with different demographic characteristics.
3.2. Univariate Analysis of Influenza Vaccination and Scores of Each Dimension of the HBM
The dimensions of the HBM presented differences between the groups receiving an influenza vaccine or not (p < 0.001). Students who received the vaccine were more likely to perceive influenza susceptibility, perceive the benefits of the vaccine, perceive the cues to action, and have higher self-efficacy. Students who did not receive the vaccine during the survey year (2020) were more likely to perceive the barriers of vaccination (Table 2).

Table 2.
Comparison of influenza vaccination among middle school students with different HBM dimensions scores (n = 9145).
3.3. Multiple Logistic Regression Analysis of Influencing Factors on Influenza Vaccination
The results showed that non-boarding (OR = 0.46, 95%CI: 0.42–0.51) and perceived barriers (OR = 0.97, 95%CI: 0.96–0.98) were unfavorable factors for influenza vaccination among middle school students, whereas perceived susceptibility (OR = 1.07, 95%CI: 1.05–1.08), perceived benefits (OR = 1.02, 95%CI: 1.01–1.04), cues to action (OR = 1.08, 95%CI: 1.05–1.11), and self-efficacy (OR = 1.04, 95%CI: 1.02–1.07) were facilitators of influenza vaccination (Table 3).

Table 3.
Multiple logistic regression analysis of the influencing factors on influenza vaccination among middle school students (n = 9145).
3.4. Qualitative Interview Analysis
This study analyzed the original interview data and extracted a total of 31 primary codes, such as “I don’t want to get sick”, “no one around has the flu”, “feeling troublesome”, and “afraid of prick or pain”. Based on those 31 primary codes, 10 categories were summarized, including “self-efficacy” and “perceived susceptibility”. Based on 10 categories, three main categories, namely, “health beliefs”, “school factors”, and “family factors”, were summarized.
3.4.1. Health Beliefs
Perceived susceptibility: Results showed that many middle school students were aware of their susceptibility to influenza, and had the willingness to receive a vaccine: “I should get a flu vaccine this year because I took a two-week break due to a recent common cold”, “I am vulnerable to catch a cold, it’s very uncomfortable”, and “parents says if I get cold frequently, I will grow less than others”. However, some students did not realize their susceptibility to influenza, so they relaxed their vigilance: “I have never been sick”, and “No one at our school got the flu”. It can be seen that a lack of perceived susceptibility to influenza is a barrier for middle school students taking the influenza vaccination.
Perceived benefits: According to student reports, benefits included improved immunity, avoidance of absenteeism, and no need for physical education classes: “If I’ve had it before, I would have gained some immunity”, “Annual vaccination for so many years is very useful to avoid absentness in class”, “The last time you got flu shot, you said that you can skip gym class”, and “I don’t think it worth a risk for a long time of sore throat or even cough for a long time and I would rather take a shot”. It can be seen that the perceived benefits of vaccination can help drive more students to be vaccinated.
Perceived barriers: There were students who expressed their concerns about vaccine: “I was vaccinated when I was in elementary school, and I always had a fever, so I stopped getting vaccinated after then”, “I was vaccinated in my first year of junior high school, I was allergic, and the symptoms were obvious, so I won’t take the vaccine again”, “It’s useless”, “I heard people were pricked but they still caught a cold and had a fever”, and “I may be allergic over the special ingredients of the vaccine and parents told me”. Concerns about the side effects and efficacy of the influenza vaccine seem to be an important reason for preventing vaccination of middle school students.
Cues to action: In term of access to influenza vaccine information, most students reported “biology class”, and some others mentioned “hospital doctor”, “school doctor”, “parents”, “local public service announcements, anywhere in the traffic”. The more ways students know about access to the influenza vaccine, the more likely they are to get vaccinated.
Self-efficacy: When asked, “Do your parents listen to your opinion or do you abide with your parents’ opinion when it comes to influenza vaccination?”, some participants said that their parents would respect their own opinions: “Whether to get flu shot or not should depend on my current physical condition”, “Parents respect my opinion more”, and “It’s up to me to decide whether to get the flu vaccine or not”. Some students said that they listened to their parents’ decision: “Even if I want to listen to myself, I can’t get vaccinated unless they sign the informed consent”, and “I think parents should be informed about the benefits of this vaccine, because it is up to parents’ decision whether we will receive the vaccine or not.” It suggests that high self-efficacy drive influenza vaccination.
Attitudes towards vaccine: Students indicated mainly three different attitudes, namely, support, neutral, and resistance towards vaccines: “I have always got vaccinated every year”, “I don’t care”, and “I will not vaccinate”. A positive attitude can help with influenza vaccination.
3.4.2. School Factors
During the interview, when asked, “When the school organizes influenza vaccination, will you ask the students around you if they are going to be vaccinated?”, most students answered “no” and “ask casually”. However, some students, especially boys, said that they “follow the crowd and do what others do”, “depend on the situation”, and “if more than half of the class were vaccinated, then I will vaccinate”. Furthermore, some students also used the WeChat group to discuss this tendency: “I can know who has been vaccinated and who did not via the parent WeChat group”, and “If more people get vaccinated, I will vaccinate”. In term of class teacher’s attitude towards the influenza vaccine, most students described it as “no interest” and “neutral”. Some students said that class teachers did not care about informed consent: “Just tell us not to forget to sign it”. However, due to the students’ admiration for their teacher, if the class teacher suggested everyone getting vaccinated, many students said, “as long as our class teacher recommends or supports, I will take a jab”.
It can be seen that the class/school atmosphere and class teacher’s cognition and attitude towards the influenza vaccine can directly or indirectly affect the students’ decision. A favorable atmosphere can drive more students to consider vaccination, thereby increasing the overall vaccination rate of the class.
3.4.3. Family factors
Parents also showed three different attitudes, namely, support, neutral, and resistance towards vaccines: “definitely support, who would want their children to get sick”, “my parents said that I can get vaccinated or not”, “my mother didn’t let me vaccinate, and she never let me vaccinate since my childhood”, “mother would ask me how much proportion of students take shot and follow the majority and it is not a big deal”, and “mother would consult the my teachers and other parents but mostly she will support me vaccinating”. It can be seen that parents, as the guardians of the students, can directly influence and decide whether or not the students are vaccinated.
4. Discussion
Our study investigated the factors influencing influenza vaccination among middle school students in four cities through a mixed-methods study. The results showed that the self-reported influenza vaccination rate of middle school students in China was 38.2%, which is lower than the WHO’s proposed vaccination target of 75% [19] and that reported by another Chinese study (51%) [14]. Likewise, the vaccination rate is lower than the United States’ vaccination rate (58.6%) among children aged 6 months to 17 years in 2020–2021 [18] and vaccination rate (43.6%) among secondary school-aged children in the United Kingdom [29]. Nevertheless, it is encouraging that the vaccination rate in this study is higher than the vaccination rate of primary and middle school students (32.2%) in Beijing from 2016 to 2017 [30]. Studies have shown that concerns about vaccine side effects are an important reason for not receiving vaccine [31,32]. There are differences in susceptibility to adverse events, which varied by age; for instance, some adverse events, such as fever and the associated febrile seizures, are more common in children than adults [33]. According to the data of adverse events following immunization (AEFI) of seasonal influenza vaccines (InfV) administrated in China, during the 2015–2018 influenza season, the most frequently reported adverse reaction among all inactivated influenza vaccine (IIV) was fever, with a slightly higher incidence of hyperthermia (4.274/100,000 doses) in the children’s vaccine than the adults’ one (4.47 vs. 4.17/100,000 doses) [34]. We speculate that the low vaccination rate among middle school students is also due to concerns about adverse effects since there was a significant proportion of students in both the questionnaire survey and qualitative interviews who reported concerns about adverse reactions to influenza vaccination. It may be related to China’s scandals related to vaccine misconduct, leading to a loss of public confidence in vaccination [35].
The vaccination rate was significantly higher in Beijing than other three cities, which may be attributed to the provision of free vaccination services for primary and middle school students and the elderly since 2007 [36]. Furthermore, the influenza vaccination rate of boarding students was significantly higher than that of non-boarding students in this study. It may be related to the fact that boarding students spend more time living in schools and receive uniform education and life guidance, they may be less influenced by their parents, as parental influence is thought to be a factor causing hesitation about vaccines [37]. A study found that influenza vaccination rates increased with educational attainment in Japan, knowledge dissemination through education department have the potential to increase vaccine coverage [38], which could explain the higher vaccination rate among senior high school students in this study.
Our study found that students who received a vaccine this year showed greater levels of perceived susceptibility, benefits, cues to action, and self-efficacy in comparison to those who did not receive a vaccine this year. The findings of our study corroborate the results of a study on vaccination intentions in Hong Kong [39]. On the other hand, students who did not vaccinate this year reported a higher level of perceived barriers.
The results of this study are similar to findings on seasonal influenza vaccine uptake in China, both suggesting that high levels of perceived susceptibility and/or perceived vaccination benefits could drive influenza vaccination [40]. Summaries of the HBM-based theoretical framework found that the perceived barrier was significant in all studies in preventive health behavior studies [41]. Our study also showed that the perceived barrier was an unfavorable factor for influenza vaccination. Self-efficacy was a facilitator of healthy behaviors, consistent with many other studies [42,43]. Similar to the results of another HBM-based vaccine acceptance survey in Hong Kong [44], we found that cues to action was the strongest driver of vaccination promotion based on HBM.
Qualitative results suggested that HBM-based semi-structured interviews are effective in exploring the influencing factors of influenza vaccination. Results suggested that parents, as guardians of their children, often play a decisive role in getting their children vaccinated. This is consistent with other studies showing that parental influence was a significant hesitant factor contributing to low vaccination rates [45,46,47]. It suggests that, to overcome hesitancy, the safety of vaccines be enhanced, and effective health education be provided to both middle school students and their parents to address their concerns about the occurrence of adverse reactions. Another reason for low vaccination rates may be that the time of the interviews was in the middle or post-COVID-19 pandemic, where most people were vaccinated several times already; indeed, research suggested that influenza vaccination rates in the post-COVID-19 vaccine era be lower due to the perceived “vaccine saturation” phenomenon [48]. During the interviews, we found there were problems such as concerns about side effects of the vaccine, lack of perceived susceptibility and benefits, and low self-efficacy, which are consistent with the results of previous studies [49]. Hence, more research is needed to explore the factors that influence middle school students’ health beliefs about vaccination. The interview also revealed that class teachers, especially those who are affirmed and trusted by their students, play a favorable role in influencing their decision to vaccinate against influenza. We recommend that, in order to achieve a higher vaccination rate, schools should put more effort into mobilizing class teachers to advocate influenza vaccination.
The strengths of our study lie in the use of a combination of qualitative and quantitative research methods based on HBM. This mixed-methods study yielded more comprehensive and informative results through comprehensive data analysis. We also acknowledge several limitations of our study. First, this cross-sectional survey covered only four cities and may not represent the students of China entirely. Nevertheless, the four cities are located in eastern, southern, central, and northwestern China; hence, the characteristics of the students are well reflected. Second, the questionnaire did not cover the “perceived severity” of the dimension of HBM, since studies have shown it is not strongly associated with preventive health behaviors [41]. Third, whether the middle school students received the influenza vaccination was self-reported and recall bias is unavoidable; however, it is rare for middle school students to forget an event of receiving a jab within one year.
5. Conclusions
This study investigated the factors influencing influenza vaccination among middle school students through a mixed-methods approach based on the theory of HBM. We found that the influenza vaccination rate of middle school students was mainly affected by school stage, region, accommodation, perceived susceptibility, perceived benefits, perceived barriers, self-efficacy, and cues to action. Our findings could inform policy makers and public service announcements to address concerns about vaccine safety and build a favorable school atmosphere, so as to increase the vaccination rate of middle school students.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10111802/s1, The items based on HBM.
Author Contributions
Y.H. conceptualized and designed the research; H.X., N.A. and M.G. conducted the survey; Y.A., M.L. and M.S. drafted the manuscript; Y.A. performed data analysis; H.X. and N.A. verified the data analysis process; Y.H. and B.T. edited and modified the original manuscript. All authors had final approval of the submitted and published versions and agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (Yifei Hu, Grant No. 72061137007).
Institutional Review Board Statement
The study involved humans was conducted in accordance with the Declaration of Helsinki, and was approved by Ethics Committee of Capital Medical University.
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The data that support the findings of this study are not publicly available but are available from the corresponding author on reasonable request.
Acknowledgments
We express our sincere thanks to the middle school students who participated in the survey and the interview.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Clayville, L.R. Influenza update: A review of currently available vaccines. Pharm. Ther. 2011, 36, 659–684. [Google Scholar]
- Loiacono, M.M.; Mitsakakis, N.; Kwong, J.C.; Gomez, G.B.; Chit, A.; Grootendorst, P. Development and Validation of a Clinical Prediction Tool for Seasonal Influenza Vaccination in England. JAMA Netw. Open 2020, 3, e207743. [Google Scholar] [CrossRef] [PubMed]
- Somes, M.P.; Turner, R.M.; Dwyer, L.J.; Newall, A.T. Estimating the annual attack rate of seasonal influenza among unvaccinated individuals: A systematic review and meta-analysis. Vaccine 2018, 36, 3199–3207. [Google Scholar] [CrossRef]
- Uscher-Pines, L.; Schwartz, H.L.; Ahmed, F.; Zheteyeva, Y.; Tamargo Leschitz, J.; Pillemer, F.; Faherty, L.; Uzicanin, A. Feasibility of Social Distancing Practices in US Schools to Reduce Influenza Transmission During a Pandemic. J. Public Health Manag. Pract. 2020, 26, 357–370. [Google Scholar] [CrossRef]
- Finnie, T.J.; Copley, V.R.; Hall, I.M.; Leach, S. An analysis of influenza outbreaks in institutions and enclosed societies. Epidemiol. Infect. 2014, 142, 107–113. [Google Scholar] [CrossRef]
- Gaglani, M.J. Editorial commentary: School-located influenza vaccination: Why worth the effort? Clin. Infect. Dis. 2014, 59, 333–335. [Google Scholar] [CrossRef]
- TWG; Influenza Vaccination; National Immunization Advisory Committee; Technical Working Group. Technical guidelines for seasonal influenza vaccination in China (2021–2022). Zhonghua Liu Xing Bing Xue Za Zhi 2021, 42, 1722–1749. [Google Scholar]
- Fiore, A.E.; Epperson, S.; Perrotta, D.; Bernstein, H.; Neuzil, K. Expanding the recommendations for annual influenza vaccination to school-age children in the United States. Pediatrics 2012, 129 (Suppl. S2), S54–S62. [Google Scholar] [CrossRef]
- Neuzil, K.M.; Hohlbein, C.; Zhu, Y. Illness among schoolchildren during influenza season: Effect on school absenteeism, parental absenteeism from work, and secondary illness in families. Arch. Pediatr. Adolesc. Med. 2002, 156, 986–991. [Google Scholar] [CrossRef]
- Eisenstein, M. Towards a universal flu vaccine. Nature 2019, 573, S50–S52. [Google Scholar] [CrossRef] [PubMed]
- de St Maurice, A.; Edwards, K. Rethinking Flu Vaccine Messaging. Pediatrics 2020, 146, e20201770. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Wang, Q.; Yang, P.; Zhang, L.; Wu, S.; Zhang, Y.; Sun, Y.; Duan, W.; Ma, C.; Zhang, M.; et al. Influenza vaccination in preventing outbreaks in schools: A long-term ecological overview. Vaccine 2017, 35, 7133–7138. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Yang, P.; Wang, Q.; Zhang, L.; Duan, W.; Pan, Y.; Wu, S.; Wang, H. Influenza Vaccination and Non-Pharmaceutical Measure Effectiveness for Preventing Influenza Outbreaks in Schools: A Surveillance-Based Evaluation in Beijing. Vaccines 2020, 8, 714. [Google Scholar] [CrossRef]
- MacDonald, P. Extension of influenza immunization program to children in England—Future plans. Hum. Vaccines Immunother. 2016, 12, 2707–2708. [Google Scholar] [CrossRef]
- Alauzet, P.; Morand, A.; Mazenq, J.; Gaudart, J.; Bosdure, E.; Dubus, J.C. Key role of pediatricians and disease for influenza vaccination in children with high-risk chronic diseases. Eur. J. Pediatr. 2021, 180, 303–306. [Google Scholar] [CrossRef]
- Blyth, C.C.; Macartney, K.K.; McRae, J.; Clark, J.E.; Marshall, H.S.; Buttery, J.; Francis, J.R.; Kotsimbos, T.; Kelly, P.M.; Cheng, A.C. Influenza Epidemiology, Vaccine Coverage and Vaccine Effectiveness in Children Admitted to Sentinel Australian Hospitals in 2017: Results from the PAEDS-FluCAN Collaboration. Clin. Infect. Dis. 2019, 68, 940–948. [Google Scholar] [CrossRef]
- Flu Vaccination Coverage, United States, 2020–2021 Influenza Season. Available online: https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm (accessed on 20 September 2022).
- Influenza vaccines. Wkly. Epidemiol. Rec. 2005, 80, 279–287.
- Rosenstock, I.M. Why people use health services. Milbank Mem. Fund Q. 1966, 44, S94–S127. [Google Scholar] [CrossRef]
- Trent, M.J.; Salmon, D.A.; MacIntyre, C.R. Using the health belief model to identify barriers to seasonal influenza vaccination among Australian adults in 2019. Influenza Other Respir. Viruses 2021, 15, 678–687. [Google Scholar] [CrossRef]
- Shon, E.J.; Ki, Y.; Lee, L. Effects of Health Beliefs on Flu Vaccination and Physical Health among Under/Graduate Students in the U.S.: Racial Differences (Whites, African Americans, Hispanics, and Asians). Soc. Work Public Health 2021, 36, 377–391. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Shahrabani, S.; Benzion, U. Workplace vaccination and other factors impacting influenza vaccination decision among employees in Israel. Int. J. Environ. Res. Public Health 2010, 7, 853–869. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.F.; Ng, C.S.M.; Wu, A.M.S.; Ma, Y.L.; Lau, M.M.C. Low coverage of influenza vaccination among Chinese children aged 12-23 months: Prevalence and associated factors. PLoS ONE 2018, 13, e0205561. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.; DeJonckheere, M.; Oliverio, A.L.; Brown, K.S.; Van Sparrentak, M.; Wu, J.P. A theoretical model of contraceptive decision-making and behaviour in diabetes: A qualitative application of the Health Belief Model. Diabet. Med. 2021, 38, e14434. [Google Scholar] [CrossRef]
- Hawkins, M.M.; Lopez, A.A.; Schmitt, M.E.; Tamkin, V.L.; Dressel, A.E.; Kako, P.; Mkandawire-Valhmu, L.; Weinhardt, L.S. A qualitative analysis of perceptions of and reactions to COVID-19. Public Health Nurs. 2022, 39, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Glaser, B.; Strauss, A.L. The Discovery of Grounded Theory: Strategy for Qualitative Research. Nurs. Res. 1968, 17, 377–380. [Google Scholar] [CrossRef]
- Seasonal Influenza Vaccine Uptake in Children of School Age: Winter Season 2021 to 2022. Available online: https://www.gov.uk/government/statistics/seasonal-influenza-vaccine-uptake-in-children-of-school-age-winter-season-2021-to-2022 (accessed on 17 October 2022).
- Zhang, L.; van der Hoek, W.; Krafft, T.; Pilot, E.; Asten, L.V.; Lin, G.; Wu, S.; Duan, W.; Yang, P.; Wang, Q. Influenza vaccine effectiveness estimates against influenza A(H3N2) and A(H1N1) pdm09 among children during school-based outbreaks in the 2016-2017 season in Beijing, China. Hum. Vaccines Immunother. 2020, 16, 816–822. [Google Scholar] [CrossRef]
- Zhang, J.; While, A.E.; Norman, I.J. Nurses’ knowledge and risk perception towards seasonal influenza and vaccination and their vaccination behaviours: A cross-sectional survey. Int. J. Nurs. Stud. 2011, 48, 1281–1289. [Google Scholar] [CrossRef]
- Yan, S.; Wang, Y.; Zhu, W.; Zhang, L.; Gu, H.; Liu, D.; Zhu, A.; Xu, H.; Hao, L.; Ye, C. Barriers to influenza vaccination among different populations in Shanghai. Hum. Vaccines Immunother. 2021, 17, 1403–1411. [Google Scholar] [CrossRef]
- Halsey, N.A.; Talaat, K.R.; Greenbaum, A.; Mensah, E.; Dudley, M.Z.; Proveaux, T.; Salmon, D.A. The safety of influenza vaccines in children: An Institute for Vaccine Safety white paper. Vaccine 2015, 33 (Suppl. S5), F1–F67. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.D.; Li, K.L.; Xu, D.S.; Ye, J.K.; Xiao, Q.Y.; Wang, H.Q. Study on surveillance data of adverse events following immunization of seasonal influenza vaccine in China during 2015–2018 influenza season. Zhonghua Yu Fang Yi Xue Za Zhi 2019, 53, 987–992. [Google Scholar] [PubMed]
- Han, B.; Wang, S.; Wan, Y.; Liu, J.; Zhao, T.; Cui, J.; Zhuang, H.; Cui, F. Has the public lost confidence in vaccines because of a vaccine scandal in China. Vaccine 2019, 37, 5270–5275. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Muscatello, D.J.; Wang, Q.; Yang, P.; Wu, J.; MacIntyre, C.R. Overview of influenza vaccination policy in Beijing, China: Current status and future prospects. J. Public Health Policy 2017, 38, 366–379. [Google Scholar] [CrossRef]
- Olusanya, O.A.; Bednarczyk, R.A.; Davis, R.L.; Shaban-Nejad, A. Addressing Parental Vaccine Hesitancy and Other Barriers to Childhood/Adolescent Vaccination Uptake During the Coronavirus (COVID-19) Pandemic. Front. Immunol. 2021, 12, 663074. [Google Scholar] [CrossRef]
- Chinzorig, T.; Sugiyama, K.; Aida, J.; Tsuboya, T.; Osaka, K. Are social inequalities in influenza vaccination coverage in Japan reduced by health policy? Prev. Med. Rep. 2019, 16, 100959. [Google Scholar] [CrossRef]
- Yan, E.; Lai, D.W.L.; Lee, V.W.P. Predictors of Intention to Vaccinate against COVID-19 in the General Public in Hong Kong: Findings from a Population-Based, Cross-Sectional Survey. Vaccines 2021, 9, 696. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, Y.; Liang, H.; Chen, Y. Seasonal Influenza Vaccine Acceptance among Pregnant Women in Zhejiang Province, China: Evidence Based on Health Belief Model. Int. J. Environ. Res. Public Health 2017, 14, 1551. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef]
- Fathian-Dastgerdi, Z.; Khoshgoftar, M.; Tavakoli, B.; Jaleh, M. Factors associated with preventive behaviors of COVID-19 among adolescents: Applying the health belief model. Res. Soc. Adm. Pharm. 2021, 17, 1786–1790. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Bukhsh, A.; Rehman, H.; Mallhi, T.H.; Ata, H.; Rehman, I.U.; Lee, L.H.; Goh, B.H.; Khan, T.M. Parents’ attitude, awareness and behaviour towards influenza vaccination in Pakistan. Hum. Vaccines Immunother. 2018, 14, 952–957. [Google Scholar] [CrossRef] [PubMed]
- Alolayan, A.; Almotairi, B.; Alshammari, S.; Alhearri, M.; Alsuhaibani, M. Seasonal Influenza Vaccination among Saudi Children: Parental Barriers and Willingness to Vaccinate Their Children. Int. J. Environ. Res. Public Health 2019, 16, 4226. [Google Scholar] [CrossRef]
- Ramprasad, C.; Zachariah, R.; Steinhoff, M.; Simon, A. Parental attitudes towards influenza vaccination for children in South India. World J. Pediatr. 2017, 13, 84–90. [Google Scholar] [CrossRef]
- Nitzan, I.; Akavian, I.; Adar, O.; Rittblat, M.; Tomer, G.; Shmueli, O.; Friedensohn, L.; Talmy, T. Acceptance of Seasonal Influenza Vaccine Following COVID-19 Vaccination: A Survey among Israel Defense Forces Soldiers. Behav. Med. 2022, 1–8. [Google Scholar] [CrossRef]
- Long, E.; Ponder, M.; Bernard, S. Knowledge, attitudes, and beliefs related to hypertension and hyperlipidemia self-management among African-American men living in the southeastern United States. Patient Educ. Couns. 2017, 100, 1000–1006. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).