What Contributes to COVID-19 Vaccine Hesitancy? A Systematic Review of the Psychological Factors Associated with COVID-19 Vaccine Hesitancy
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Selection Process and Data Extraction
2.4. Quality Assessment and Evidence Synthesis
3. Results
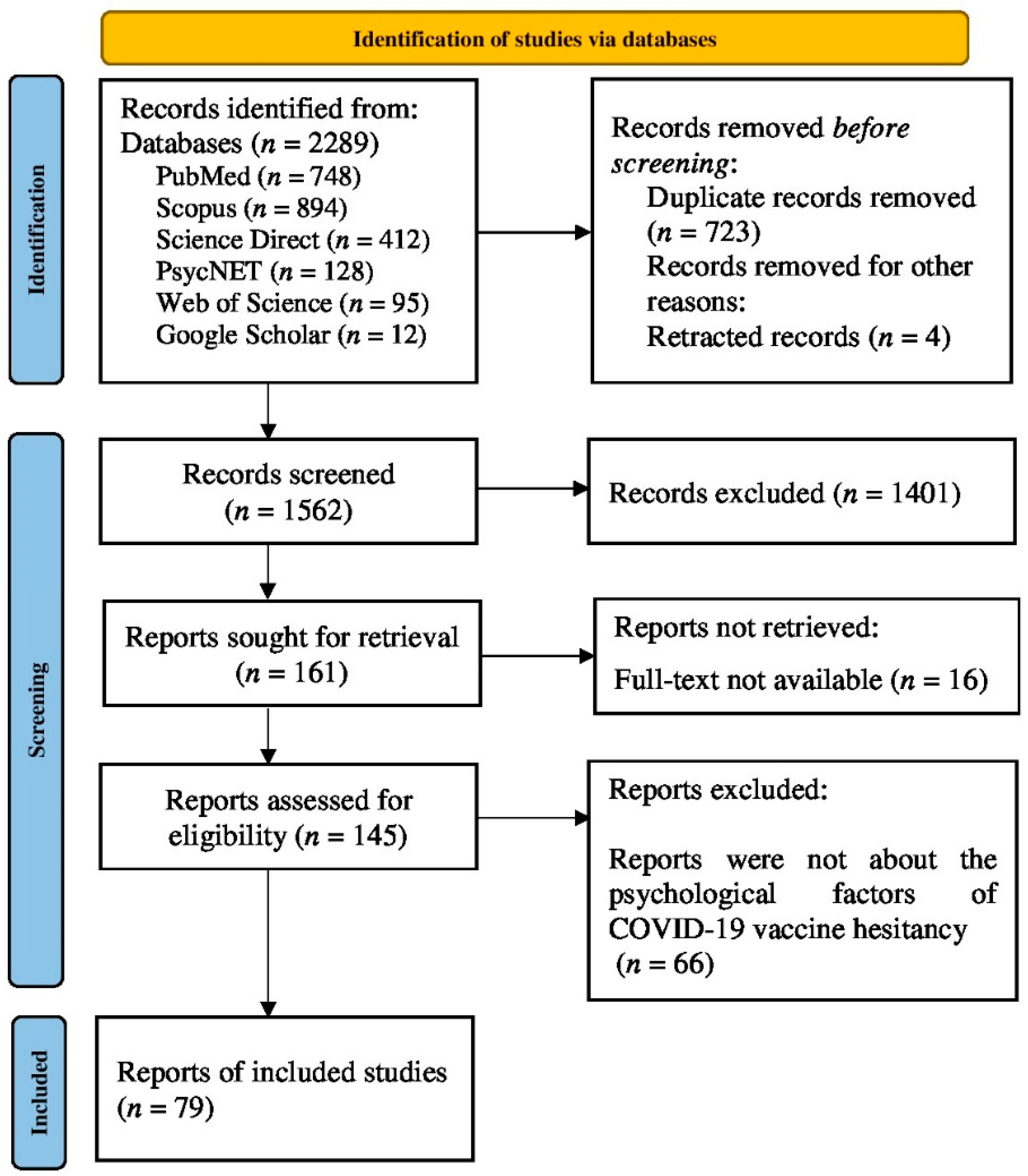
3.1. Identification of Studies
3.2. Study Characteristics
3.3. Quality Assessment
3.4. Psychological Factors Associated with Vaccine Hesitancy
3.4.1. Appraisal of COVID-19 Pandemic
3.4.2. Vaccine Safety and Side Effects
3.4.3. Vaccine Confidence/Trust
3.4.4. Trust in Government and Healthcare Professionals
3.4.5. Scepticism around Vaccine Production
3.4.6. Conspiracy Beliefs
3.4.7. Emotions
3.4.8. Information and Knowledge about Vaccines
4. Discussion
5. Implications, Limitations, and Future Recommendations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mesch, G.S.; Schwirian, K.P. Vaccination hesitancy: Fear, trust, and exposure expectancy of an Ebola outbreak. Heliyon 2019, 5, e02016. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Thangaraju, P.; Venkatesan, S. WHO Ten threats to global health in 2019: Antimicrobial resistance. Med. J. 2019, 44, 1150–1151. [Google Scholar] [CrossRef]
- Pang, J.; Wang, M.X.; Ang, I.Y.H.; Tan, S.H.X.; Lewis, R.F.; Chen, J.I.-P.; Gutierrez, R.A.; Gwee, S.X.W.; Chua, P.E.Y.; Yang, Q.; et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel Coronavirus (2019-nCoV): A Systematic Review. J. Clin. Med. 2020, 9, 623. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dubé, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; The SAGE Working Group on Vaccine Hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef]
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Ren, J.; Huang, Z.; Contreras-Roldan, I.L.; Gebremeskel, B.; et al. Comparisons of Vaccine Hesitancy across Five Low- and Middle-Income Countries. Vaccines 2019, 7, 155. [Google Scholar] [CrossRef]
- Wolfe, R.M.; Sharp, L.K. Anti-vaccinationists past and present. BMJ 2002, 325, 430–432. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Karafillakis, E.; Larson, H.J. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine 2017, 35, 4840–4850. [Google Scholar] [CrossRef]
- Pelčić, G.; Karačić, S.; Mikirtichan, G.L.; Kubar, O.I.; Leavitt, F.J.; Cheng-tek Tai, M.; Morishita, N.; Vuletić, S.; Tomašević, L. Religious exception for vaccination or religious excuses for avoiding vaccination. Croat. Med. J. 2016, 57, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014, 112, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Garcia, R.; Arinezfernandez, M.C.; Garciacarballo, M.; Hernandezbarrera, V.; de Miguel, A.G.; Carrascogarrido, P. Influenza vaccination coverage and related factors among Spanish patients with chronic obstructive pulmonary disease. Vaccine 2005, 23, 3679–3686. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Cho, S.-I. Influenza Vaccination Coverage among Adults in Korea: 2008–2009 to 2011–2012 Seasons. Int. J. Environ. Res. Public Health 2014, 11, 12162–12173. [Google Scholar] [CrossRef]
- Wada, K.; Smith, D.R. Influenza Vaccination Uptake among the Working Age Population of Japan: Results from a National Cross-Sectional Survey. PLoS ONE 2013, 8, e59272. [Google Scholar] [CrossRef]
- Chiatti, C.; Barbadoro, P.; Lamura, G.; Pennacchietti, L.; Di Stanislao, F.; D’Errico, M.M.; Prospero, E. Influenza vaccine uptake among community-dwelling Italian elderly: Results from a large cross-sectional study. BMC Public Health 2011, 11, 207. [Google Scholar] [CrossRef]
- Pulcini, C.; Massin, S.; Launay, O.; Verger, P. Factors associated with vaccination for hepatitis B, pertussis, seasonal and pandemic influenza among French general practitioners: A 2010 survey. Vaccine 2013, 31, 3943–3949. [Google Scholar] [CrossRef]
- Takayama, M.; Wetmore, C.M.; Mokdad, A.H. Characteristics associated with the uptake of influenza vaccination among adults in the United States. Prev. Med. 2012, 54, 358–362. [Google Scholar] [CrossRef]
- Damiani, G.; Federico, B.; Visca, M.; Agostini, F.; Ricciardi, W. The impact of socioeconomic level on influenza vaccination among Italian adults and elderly: A cross-sectional study. Prev. Med. 2007, 45, 373–379. [Google Scholar] [CrossRef]
- Schmitz, H.; Wübker, A. What determines influenza vaccination take-up of elderly Europeans? Health Econ. 2011, 20, 1281–1297. [Google Scholar] [CrossRef]
- Jamison, A.M.; Quinn, S.C.; Freimuth, V.S. “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc. Sci. Med. 2018, 221, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Nihlén Fahlquist, J. Vaccine hesitancy and trust. Ethical aspects of risk communication. Scand. J. Public Health 2017, 46, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Mesch, G.S.; Schwirian, K.P. Confidence in government and vaccination willingness in the USA. Health Promot. Int. 2014, 30, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Suk, J.E.; Lopalco, P.; Celentano, L. Hesitancy, Trust and Individualism in Vaccination Decision-Making. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef]
- Wake, A.D. The Willingness to Receive COVID-19 Vaccine and Its Associated Factors: “Vaccination Refusal Could Prolong the War of This Pandemic”—A Systematic Review. Risk Manag. Health Policy 2021, 14, 2609–2623. [Google Scholar] [CrossRef]
- Karlsson, L.C.; Soveri, A.; Lewandowsky, S.; Karlsson, L.; Karlsson, H.; Nolvi, S.; Karukivi, M.; Lindfelt, M.; Antfolk, J. Fearing the disease or the vaccine: The case of COVID-19. Pers. Individ. Differ. 2021, 172, 110590. [Google Scholar] [CrossRef]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef]
- Olagoke, A.A.; Olagoke, O.O.; Hughes, A.M. Intention to Vaccinate Against the Novel 2019 Coronavirus Disease: The Role of Health Locus of Control and Religiosity. J. Relig. Health 2020, 60, 65–80. [Google Scholar] [CrossRef]
- Siddiqui, M.; Salmon, D.A.; Omer, S.B. Epidemiology of vaccine hesitancy in the United States. Hum. Vaccines Immunother. 2013, 9, 2643–2648. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Marti, M.; de Cola, M.; Macdonald, N.E.; Dumolard, L.; Duclos, P. Assessments of global drivers of vaccine hesitancy in 2014—Looking beyond safety concerns. PLoS ONE 2017, 12, e0172310. [Google Scholar] [CrossRef] [PubMed]
- Hornsey, M.J.; Harris, E.A.; Fielding, K.S. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018, 37, 307–315. [Google Scholar] [CrossRef]
- de Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s Approach. Int. J. Evid. Based Health 2015, 13, 163–169. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef]
- Alqudeimat, Y.; Alenezi, D.; AlHajri, B.; Alfouzan, H.; Almokhaizeem, Z.; Altamimi, S.; Almansouri, W.; Alzalzalah, S.; Ziyab, A.H. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Med Princ. Pract. 2021, 30, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cordina, M.; Lauri, M.A.; Lauri, J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm. Pract. 2021, 19, 2317. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Dobalian, A.; Ward, K.D. COVID-19 Vaccine Hesitancy and Its Determinants Among Adults with a History of Tobacco or Marijuana Use. J. Community Health 2021, 46, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- Nazlı, Ş.B.; Yığman, F.; Sevindik, M.; Deniz Özturan, D. Psychological factors affecting COVID-19 vaccine hesitancy. Ir. J. Med. Sci. 2021, 191, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Schernhammer, E.; Weitzer, J.; Laubichler, M.D.; Birmann, B.M.; Bertau, M.; Zenk, L.; Caniglia, G.; Jäger, C.C.; Steiner, G. Correlates of COVID-19 vaccine hesitancy in Austria: Trust and the government. J. Public Health 2021, 44, e106. [Google Scholar] [CrossRef] [PubMed]
- Altulahi, N.; AlNujaim, S.; Alabdulqader, A.; Alkharashi, A.; AlMalki, A.; AlSiari, F.; Bashawri, Y.; Alsubaie, S.; AlShahrani, D.; AlGoraini, Y. Willingness, beliefs, and barriers regarding the COVID-19 vaccine in Saudi Arabia: A multiregional cross-sectional study. BMC Fam. Pract. 2021, 22, 247. [Google Scholar] [CrossRef]
- Aloweidi, A.; Bsisu, I.; Suleiman, A.; Abu-Halaweh, S.; Almustafa, M.; Aqel, M.; Amro, A.; Radwan, N.; Assaf, D.; Abdullah, M.Z.; et al. Hesitancy towards COVID-19 Vaccines: An Analytical Cross–Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 5111. [Google Scholar] [CrossRef]
- Benham, J.L.; Atabati, O.; Oxoby, R.J.; Mourali, M.; Shaffer, B.; Sheikh, H.; Boucher, J.-C.; Constantinescu, C.; Parsons Leigh, J.; Ivers, N.M.; et al. COVID-19 Vaccine–Related Attitudes and Beliefs in Canada: National Cross-sectional Survey and Cluster Analysis. JMIR Public Health Surveill. 2021, 7, e30424. [Google Scholar] [CrossRef]
- Chaudhary, F.A.; Ahmad, B.; Khalid, M.D.; Fazal, A.; Javaid, M.M.; Butt, D.Q. Factors influencing COVID-19 vaccine hesitancy and acceptance among the Pakistani population. Hum. Vaccines Immunother. 2021, 17, 3365–3370. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, X.; Gao, J.; Liu, X.; Mao, Y.; Wang, R.; Zheng, P.; Xiao, Q.; Jia, Y.; Fu, H.; et al. Health Belief Model Perspective on the Control of COVID-19 Vaccine Hesitancy and the Promotion of Vaccination in China: Web-Based Cross-sectional Study. J. Med. Internet Res. 2021, 23, e29329. [Google Scholar] [CrossRef] [PubMed]
- Danabal, K.G.M.; Magesh, S.S.; Saravanan, S.; Gopichandran, V. Attitude towards COVID 19 vaccines and vaccine hesitancy in urban and rural communities in Tamil Nadu, India—A community based survey. BMC Health Serv. Res. 2021, 21, 994. [Google Scholar] [CrossRef]
- Hossain, M.B.; Alam, M.Z.; Islam, M.S.; Sultan, S.; Faysal, M.M.; Rima, S.; Hossain, A.; Al Mamun, A.A. Health Belief Model, Theory of Planned Behavior, or Psychological Antecedents: What Predicts COVID-19 Vaccine Hesitancy Better Among the Bangladeshi Adults? Front. Public Health 2021, 9, 711066. [Google Scholar] [CrossRef]
- Hossain, E.; Islam, S.; Ghose, T.K.; Jahan, H.; Chakrobortty, S.; Hossen, M.S.; Ema, N.S. COVID-19 vaccine acceptability among public university students in Bangladesh: Highlighting knowledge, perceptions, and attitude. Hum. Vaccines Immunother. 2021, 17, 5089–5098. [Google Scholar] [CrossRef] [PubMed]
- Ikiışık, H.; Akif Sezerol, M.; Taşçı, Y.; Maral, I. COVID-19 vaccine hesitancy: A community-based research in Turkey. Int. J. Clin. Pract. 2021, 75, e14336. [Google Scholar] [CrossRef]
- Alabdulla, M.; Reagu, S.M.; Al-Khal, A.; Elzain, M.; Jones, R.M. COVID-19 vaccine hesitancy and attitudes in Qatar: A national cross-sectional survey of a migrant-majority population. Influenza Other Respir. Viruses 2021, 15, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef] [PubMed]
- Qunaibi, E.; Basheti, I.; Soudy, M.; Sultan, I. Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines 2021, 9, 446. [Google Scholar] [CrossRef]
- Asadi Faezi, N.; Gholizadeh, P.; Sanogo, M.; Oumarou, A.; Mohamed, M.N.; Cissoko, Y.; Saliou Sow, M.; Keita, B.S.; Baye, Y.A.M.; Pagliano, P.; et al. Peoples’ attitude toward COVID-19 vaccine, acceptance, and social trust among African and Middle East countries. Health Promot. Perspect. 2021, 11, 171–178. [Google Scholar] [CrossRef]
- Milan, S.; Dáu, A.L.B.T. The Role of Trauma in Mothers’ COVID-19 Vaccine Beliefs and Intentions. J. Pediatr. Psychol. 2021, 46, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zhang, R.; Zhou, Z.; Fan, J.; Liang, J.; Cai, L.; Peng, L.; Ren, F.; Lin, W. Parental psychological distress and attitudes towards COVID-19 vaccination: A cross-sectional survey in Shenzhen, China. J. Affect. Disord. 2021, 292, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Vasquez, D.E.; Ruiz-Padilla, J.P.; Botello-Hernandez, E. Vaccine Hesitancy against SARS-CoV-2 in Health Personnel of Northeastern Mexico and its Determinants. J. Occup. Environ. Med. 2021, 63, 633–637. [Google Scholar] [CrossRef]
- Bono, S.A.; Faria de Moura Villela, E.; Siau, C.S.; Chen, W.S.; Pengpid, S.; Hasan, M.T.; Sessou, P.; Ditekemena, J.D.; Amodan, B.O.; Hosseinipour, M.C.; et al. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines 2021, 9, 515. [Google Scholar] [CrossRef]
- Al-Sanafi, M.; Sallam, M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines 2021, 9, 701. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Hasan, H.; Taim, D.; Al-Mahzoum, K.; Al-Haidar, A.; Yaseen, A.; Ababneh, N.A.; Assaf, A.; et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int. J. Environ. Res. Public Health 2021, 18, 2407. [Google Scholar] [CrossRef]
- Kucukkarapinar, M.; Karadag, F.; Budakoglu, I.; Aslan, S.; Ucar, O.; Yay, A.; Timurcin, U.; Tumkaya, S.; Hocaoglu, C.; Kiraz, I. COVID-19 Vaccine Hesitancy and Its Relationship with Illness Risk Perceptions, Affect, Worry, and Public Trust: An Online Serial Cross-Sectional Survey from Turkey. Psychiatry Clin. Psychopharmacol. 2021, 31, 98–109. [Google Scholar] [CrossRef]
- Piltch-Loeb, R.; Savoia, E.; Goldberg, B.; Hughes, B.; Verhey, T.; Kayyem, J.; Miller-Idriss, C.; Testa, M. Examining the effect of information channel on COVID-19 vaccine acceptance. PLoS ONE 2021, 16, e0251095. [Google Scholar] [CrossRef]
- Alibrahim, J.; Awad, A. COVID-19 Vaccine Hesitancy among the Public in Kuwait: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 8836. [Google Scholar] [CrossRef] [PubMed]
- Acar-Burkay, S.; Cristian, D.-C. Cognitive underpinnings of COVID-19 vaccine hesitancy. Soc. Sci. Med. 2022, 301, 114911. [Google Scholar] [CrossRef] [PubMed]
- Dambadarjaa, D.; Altankhuyag, G.-E.; Chandaga, U.; Khuyag, S.-O.; Batkhorol, B.; Khaidav, N.; Dulamsuren, O.; Gombodorj, N.; Dorjsuren, A.; Singh, P.; et al. Factors Associated with COVID-19 Vaccine Hesitancy in Mongolia: A Web-Based Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 12903. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, O.V.; Johnson, M.S.; Ebling, S.; Amundsen, O.M.; Halsøy, Ø.; Hoffart, A.; Skjerdingstad, N.; Johnson, S.U. Risk, Trust, and Flawed Assumptions: Vaccine Hesitancy During the COVID-19 Pandemic. Front. Public Health 2021, 9, 700213. [Google Scholar] [CrossRef] [PubMed]
- Ehde, D.M.; Roberts, M.K.; Humbert, A.T.; Herring, T.E.; Alschuler, K.N. COVID-19 vaccine hesitancy in adults with multiple sclerosis in the United States: A follow up survey during the initial vaccine rollout in 2011. Mult. Scler. Relat. Disord. 2021, 54, 103163. [Google Scholar] [CrossRef] [PubMed]
- Almaghaslah, D.; Alsayari, A.; Kandasamy, G.; Vasudevan, R. COVID-19 Vaccine Hesitancy among Young Adults in Saudi Arabia: A Cross-Sectional Web-Based Study. Vaccines 2021, 9, 330. [Google Scholar] [CrossRef]
- Jain, J.; Saurabh, S.; Kumar, P.; Verma, M.K.; Goel, A.D.; Gupta, M.K.; Bhardwaj, P.; Raghav, P.R. COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect 2021, 149, e132. [Google Scholar] [CrossRef]
- Kumar, R.; Alabdulla, M.; Elhassan, N.M.; Reagu, S.M. Qatar Healthcare Workers’ COVID-19 Vaccine Hesitancy and Attitudes: A National Cross-Sectional Survey. Front. Public Health 2021, 9, 727748. [Google Scholar] [CrossRef]
- Luk, T.T.; Zhao, S.; Wu, Y.; Wong, J.Y.-H.; Wang, M.P.; Lam, T.H. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: A population-based survey. Vaccine 2021, 39, 3602–3607. [Google Scholar] [CrossRef]
- Maraqa, B.; Nazzal, Z.; Rabi, R.; Sarhan, N.; Al-Shakhra, K.; Al-Kaila, M. COVID-19 vaccine hesitancy among health care workers in Palestine: A call for action. Prev. Med. 2021, 149, 106618. [Google Scholar] [CrossRef]
- Mejri, N.; Berrazega, Y.; Ouertani, E.; Rachdi, H.; Bohli, M.; Kochbati, L.; Boussen, H. Understanding COVID-19 vaccine hesitancy and resistance: Another challenge in cancer patients. Support. Care Cancer 2021, 30, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Navarre, C.; Roy, P.; Ledochowski, S.; Fabre, M.; Esparcieux, A.; Issartel, B.; Dutertre, M.; Blanc-Gruyelle, A.-L.; Suy, F.; Adelaide, L.; et al. Determinants of COVID-19 vaccine hesitancy in French hospitals. Infect Dis. Now 2021, 51, 647–653. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, B.L.C.A.; Campos, M.A.G.; de Queiroz, R.C.S.; de Alves, M.T.S.S.B.E.; de Souza, B.F.; dos Santos, A.M.; da Silva, A.A.M. Prevalence and factors associated with covid-19 vaccine hesitancy in Maranhão, Brazil. Rev. Saude Publica 2021, 55, 12. [Google Scholar] [CrossRef]
- Park, H.K.; Ham, J.H.; Jang, D.H.; Lee, J.Y.; Jang, W.M. Political Ideologies, Government Trust, and COVID-19 Vaccine Hesitancy in South Korea: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 10655. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Kumar, A.; Mandal, A.; Shaikh, M.; Hall, C.A.; Kirk, J.M.W.; Moss, P.; Brookes, M.J.; Basu, S. The UPTAKE study: A cross-sectional survey examining the insights and beliefs of the UK population on COVID-19 vaccine uptake and hesitancy. BMJ Open 2021, 11, e048856. [Google Scholar] [PubMed]
- Sirikalyanpaiboon, M.; Ousirimaneechai, K.; Phannajit, J.; Pitisuttithum, P.; Jantarabenjakul, W.; Chaiteerakij, R.; Paitoonpong, L. COVID-19 vaccine acceptance, hesitancy, and determinants among physicians in a university-based teaching hospital in Thailand. BMC Infect Dis. 2021, 21, 1174. [Google Scholar] [CrossRef]
- Yahia, A.I.O.; Alshahrani, A.M.; Alsulmi, W.G.H.; Alqarni, M.M.M.; Abdulrahim, T.K.A.; Heba, W.F.H.; Alqarni, T.A.A.; Alharthi, K.A.Z.; Buhran, A.A.A. Determinants of COVID-19 vaccine acceptance and hesitancy: A cross-sectional study in Saudi Arabia. Hum. Vaccines Immunother. 2021, 17, 4015–4020. [Google Scholar] [CrossRef]
- Yeşiltepe, A.; Aslan, S.; Bulbuloglu, S. Investigation of perceived fear of COVID-19 and vaccine hesitancy in nursing students. Hum. Vaccines Immunother. 2021, 17, 5030–5037. [Google Scholar] [CrossRef]
- Albahri, A.H.; Alnaqbi, S.A.; Alshaali, A.O.; Alnaqbi, S.A.; Shahdoor, S.M. COVID-19 Vaccine Acceptance in a Sample from the United Arab Emirates General Adult Population: A Cross-Sectional Survey. Front. Public Health 2021, 9, 614499. [Google Scholar] [CrossRef]
- Singh, A.; Lai, A.H.Y.; Wang, J.; Asim, S.; Chan, P.S.-F.; Wang, Z.; Yeoh, E.K. Multilevel Determinants of COVID-19 Vaccine Uptake Among South Asian Ethnic Minorities in Hong Kong: Cross-sectional Web-Based Survey. JMIR Public Health Surveill. 2021, 7, e31707. [Google Scholar] [CrossRef]
- Ali, M.; Hossain, A. What is the extent of COVID-19 vaccine hesitancy in Bangladesh? A cross-sectional rapid national survey. BMJ Open 2021, 11, e050303. [Google Scholar] [CrossRef] [PubMed]
- Anjorin, A.A.; Odetokun, I.A.; Abioye, A.I.; Elnadi, H.; Umoren, M.V.; Damaris, B.F.; Eyedo, J.; Umar, H.I.; Nyandwi, J.B.; Abdalla, M.M.; et al. Will Africans take COVID-19 vaccination? PLoS ONE 2021, 16, e0260575. [Google Scholar] [CrossRef] [PubMed]
- Boon-Itt, S.; Rompho, N.; Jiarnkamolchurn, S.; Skunkan, Y. Interaction between age and health conditions in the intention to be vaccinated against COVID-19 in Thailand. Hum. Vaccines Immunother. 2021, 17, 4816–4822. [Google Scholar] [CrossRef]
- Yilma, D.; Mohammed, R.; Abdela, S.G.; Enbiale, W.; Seifu, F.; Pareyn, M.; Liesenborghs, L.; van Griensven, J.; van Henten, S. COVID-19 vaccine acceptability among healthcare workers in Ethiopia: Do we practice what we preach? Trop. Med. Int. Health 2022, 27, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Fakonti, G.; Kyprianidou, M.; Toumbis, G.; Giannakou, K. Attitudes and Acceptance of COVID-19 Vaccination among Nurses and Midwives in Cyprus: A Cross-Sectional Survey. Front. Public Health 2021, 9, 656138. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zheng, Y.; Luo, Y.; Ren, J.; Jiang, L.; Tang, J.; Yu, X.; Luo, D.; Fan, D.; Chen, Y. Hesitancy toward COVID-19 vaccines among medical students in Southwest China: A cross-sectional study. Hum. Vaccines Immunother. 2021, 17, 4021–4027. [Google Scholar] [CrossRef] [PubMed]
- Magadmi, R.M.; Kamel, F.O. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health 2021, 21, 1428. [Google Scholar] [CrossRef]
- Khairat, S.; Zou, B.; Adler-Milstein, J. Factors and reasons associated with low COVID-19 vaccine uptake among highly hesitant communities in the US. Am. J. Infect Control. 2022, 50, 262–267. [Google Scholar] [CrossRef]
- Holeva, V.; Parlapani, E.; Nikopoulou, V.; Nouskas, I.; Diakogiannis, I. COVID-19 vaccine hesitancy in a sample of Greek adults. Psychol. Health Med. 2021, 27, 113–119. [Google Scholar] [CrossRef]
- Hubach, R.D.; Shannon, B.; Morgan, K.D.; Alexander, C.; O’Neil, A.M.; Ernst, C.; Giano, Z. COVID-19 vaccine hesitancy among rural Oklahomans. Rural Remote Health 2022, 22, 7128. [Google Scholar] [CrossRef]
- Moro, G.L.; Cugudda, E.; Bert, F.; Raco, I.; Siliquini, R. Vaccine Hesitancy and Fear of COVID-19 Among Italian Medical Students: A Cross-Sectional Study. J. Community Health 2022, 47, 475–483. [Google Scholar] [CrossRef]
- Silva, T.M.; Estrela, M.; Roque, V.; Gomes, E.R.; Figueiras, A.; Roque, F.; Herdeiro, M.T. Perceptions, knowledge and attitudes about COVID-19 vaccine hesitancy in older Portuguese adults. Age Ageing 2022, 51, afac013. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.; Rocha, J.; Moniz, M.; Gama, A.; Laires, P.; Pedro, A.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, A.; Dickinson, H.; Dimov, S.; Shields, M.; McAllister, A. The COVID-19 vaccine intentions of Australian disability support workers. Aust. NZ J. Public Health 2022, 46, 314–321. [Google Scholar] [CrossRef]
- Hwang, S.E.; Kim, W.-H.; Heo, J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December. Hum. Vaccines Immunother. 2021, 18, 1–8. [Google Scholar] [CrossRef]
- Hong, J.; Xu, X.-W.; Yang, J.; Zheng, J.; Dai, S.-M.; Zhou, J.; Zhang, Q.-M.; Ruan, Y.; Ling, C.-Q. Knowledge about, attitude and acceptance towards, and predictors of intention to receive the COVID-19 vaccine among cancer patients in Eastern China: A cross-sectional survey. J. Integr. Med. 2021, 20, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Shareef, L.G.; Fawzi Al-Hussainy, A.; Majeed Hameed, S. COVID-19 vaccination hesitancy among Iraqi general population between beliefs and barriers: An observational study. F1000Research 2022, 11, 334. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; You, M. Direct and Indirect Associations of Media Use With COVID-19 Vaccine Hesitancy in South Korea: Cross-sectional Web-Based Survey. J. Med. Internet Res. 2022, 24, e32329. [Google Scholar] [CrossRef]
- Kumari, A.; Mahey, R.; Kachhawa, G.; Kumari, R.; Bhatla, N. Knowledge, attitude, perceptions, and concerns of pregnant and lactating women regarding COVID-19 vaccination: A cross-sectional survey of 313 participants from a tertiary care centre of North India. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102449. [Google Scholar] [CrossRef]
- Moscardino, U.; Musso, P.; Inguglia, C.; Ceccon, C.; Miconi, D.; Rousseau, C. Sociodemographic and psychological correlates of COVID-19 vaccine hesitancy and resistance in the young adult population in Italy. Vaccine 2022, 40, 2379–2387. [Google Scholar] [CrossRef]
- Mundagowa, P.T.; Tozivepi, S.N.; Chiyaka, E.T.; Mukora-Mutseyekwa, F.; Makurumidze, R. Assessment of COVID-19 vaccine hesitancy among Zimbabweans: A rapid national survey. PLoS ONE 2022, 17, e0266724. [Google Scholar] [CrossRef] [PubMed]
- Zammit, N.; Gueder, A.E.; Brahem, A.; Ayouni, I.; Ghammam, R.; Fredj, S.B.; Sridi, C.; Chouchene, A.; Kalboussi, H.; El Maalel, O.; et al. Studying SARS-CoV-2 vaccine hesitancy among health professionals in Tunisia. BMC Health Serv. Res. 2022, 22, 489. [Google Scholar] [CrossRef] [PubMed]
- Ekowo, O.E.; Manafa, C.; Isielu, R.C.; Okoli, C.M.; Chikodi, I.; Onwuasoanya, A.F.; Echendu, S.T.; Ihedoro, I.; Nwabueze, U.D.; Nwoke, O.C. A cross sectional regional study looking at the factors responsible for the low COVID-19 vaccination rate in Nigeria. Pan Afr. Med. J. 2022, 41, 114. [Google Scholar] [CrossRef] [PubMed]
- Skeens, M.A.; Hill, K.; Olsavsky, A.; Buff, K.; Stevens, J.; Akard, T.F.; Shah, N.; Gerhardt, C.A. Factors affecting COVID-19 vaccine hesitancy in parents of children with cancer. Pediatr. Blood Cancer 2022, 69, e29707. [Google Scholar] [CrossRef]
- Walsh, J.C.; Comar, M.; Folan, J.; Williams, S.; Kola-Palmer, S. The psychological and behavioural correlates of COVID-19 vaccine hesitancy and resistance in Ireland and the UK. Acta Psychol. 2022, 225, 103550. [Google Scholar] [CrossRef]
- Betsch, C.; Wicker, S. E-health use, vaccination knowledge and perception of own risk: Drivers of vaccination uptake in medical students. Vaccine 2012, 30, 1143–1148. [Google Scholar] [CrossRef]
- Maurer, J.; Uscher-Pines, L.; Harris, K.M. Perceived seriousness of seasonal and A(H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among U.S. adults: Does the source of information matter? Prev. Med. 2010, 51, 185–187. [Google Scholar] [CrossRef]
- Rubin, J.L.; McGarry, L.J.; Strutton, D.R.; Klugman, K.P.; Pelton, S.; Gilmore, K.E.; Weinstein, M.C. Public health and economic impact of the 13-valent pneumococcal conjugate vaccine (PCV13) in the United States. Vaccine 2010, 28, 7634–7643. [Google Scholar] [CrossRef]
- Chor, J.S.Y.; Pada, S.K.; Stephenson, I.; Goggins, W.B.; Tambyah, P.A.; Clarke, T.W.; Medina, M.; Lee, N.; Leung, T.F.; Ngai, K.L.; et al. Seasonal influenza vaccination predicts pandemic H1N1 vaccination uptake among healthcare workers in three countries. Vaccine 2011, 29, 7364–7369. [Google Scholar] [CrossRef]
- Seale, H.; Heywood, A.E.; McLaws, M.-L.; Ward, K.F.; Lowbridge, C.P.; Van, D.; MacIntyre, C.R. Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect Dis. 2010, 10, 99. [Google Scholar] [CrossRef]
- Medeiros, K.S.; Costa, A.P.F.; Sarmento, A.C.A.; Freitas, C.L.; Gonçalves, A.K. Side effects of COVID-19 vaccines: A systematic review and meta-analysis protocol of randomised trials. BMJ Open 2022, 12, e050278. [Google Scholar] [CrossRef] [PubMed]
- Edwards, K.M.; Hackell, J.M. Committee on Infectious Diseases, Committee on Practice and Ambulatory Medicine. Countering Vaccine Hesitancy. Pediatrics 2016, 138, e20162146. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, J.; Halkitis, P.N. Towards a More Inclusive and Dynamic Understanding of Medical Mistrust Informed by Science. Behav. Med. 2019, 45, 79–85. [Google Scholar] [CrossRef] [PubMed]
- LaVeist, T.A.; Isaac, L.A.; Williams, K.P. Mistrust of Health Care Organizations Is Associated with Underutilization of Health Services. Health Serv. Res. 2009, 44, 2093–2105. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Eastwood, K.; Durrheim, D.N.; Jones, A.; Butler, M. Acceptance of pandemic (H1N1) 2009 influenza vaccination by the Australian public. Med. J. Aust. 2010, 192, 33–36. [Google Scholar] [CrossRef]
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm—An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef]
- Betsch, C.; Ulshöfer, C.; Renkewitz, F.; Betsch, T. The Influence of Narrative v. Statistical Information on Perceiving Vaccination Risks. Med. Decis. Mak. 2011, 31, 742–753. [Google Scholar] [CrossRef]
- Naeem, S.B.; Bhatti, R.; Khan, A. An exploration of how fake news is taking over social media and putting public health at risk. Health Inf. Libr. J. 2020, 38, 143–149. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Siegrist, M.; Zingg, A. The Role of Public Trust during Pandemics: Implications for Crisis Communication. Eur. Psychol. 2014, 19, 23–32. [Google Scholar] [CrossRef]
| Sl. No. | Author(s) & Year | Country | Sample | Sample Size | Associated Psychological Factors |
|---|---|---|---|---|---|
| 1 | Murphy et al. [25] | Ireland & UK | General population | n = 3066 | Mistrust in authoritative and traditional information sources of pandemic, less trust in healthcare professionals, state and scientists, lower cognitive reflection, high social dominance and authoritarianism, negative attitudes toward migrants, lower levels of altruism, high conspiracy and religious beliefs, low personality trait agreeableness, high internal locus of control |
| 2 | Fisher et al. [38] | United States | General population | n = 991 | Not received the influenza vaccine in the previous year, vaccine-specific concerns, inadequate information, anti-vaccine attitudes or beliefs, lack of trust |
| 3 | Lin et al. [39] | China | General population | n = 3541 | Concerns about vaccine side effects and efficacy |
| 4 | Caserotti. [40] | Italy | General population | n = 2267 | Doubts about the vaccines in general |
| 5 | Alqudeimat et al. [41] | Kuwait | General population | n = 2368 | Vaccine’s health-related risks and concerns |
| 6 | Willis et al. [42] | United States | General population | n = 1205 | No fear of COVID-19 infection, low vaccine trust in general |
| 7 | Freeman et al. [43] | UK | General population | n = 15,014 | Injection fear |
| 8 | Cordina et al. [44] | Malta | General population | n = 3363 | Lack of vaccine safety, fear of injections, need more information about the vaccine |
| 9 | Yang et al. [45] | United States | Adults with a history of tobacco or marijuana use | n = 387 | Not stressed because of the COVID-19, previous influenza vaccination behaviour |
| 10 | Nazli et al. [46] | Turkey | General population | n = 467 | Belief in conspiracy theories, low fear of COVID-19 |
| 11 | Schernhammer et al. [47] | Austria | General population | n = 1007 | Voting behaviour or trust in the government |
| 12 | Altulahi et al. [48] | Saudi Arabia | General population | n = 8056 | Vaccine side effects and safety |
| 13 | Aloweidi et al. [49] | Jordan | Medical and non-medical workers | n = 646 | Rumour that vaccines are not safe |
| 14 | Benham et al. [50] | Canada | General population | n = 4498 | Vaccine side effects, low influence by peers or health care professionals, low trust in government institutions |
| 15 | Chaudhary et al. [51] | Pakistan | General population | n = 423 | Lack of knowledge, understanding, and perception of the risk, safety |
| 16 | Chen et al. [52] | China | General population | n = 2531 | Perception of COVID-19 susceptibility, perceived barriers to vaccination |
| 17 | Danabal et al. [53] | India | General population | n = 564 | Adverse effects, mistrust in vaccines |
| 18 | Hossain et al. [54] | Bangladesh | General population | n = 1497 | Conspiracy beliefs, widespread misinformation, superstitions about the COVID-19 vaccine |
| 19 | Hossain et al. [55] | Bangladesh | University students | n = 900 | Inadequate knowledge, negative vaccine perceptions and attitudes |
| 20 | İkiışık et al. [56] | Turkey | General population | n = 384 | COVID-19 risk perception |
| 21 | Alabdulla et al. [57] | Qatar | Migrant majority population | n = 7821 | Concerns around the COVID-19 vaccine safety and its longer-term side effects |
| 22 | Saied et al. [58] | Egypt | Medical students | n = 2133 | Concerns about the vaccine’s ineffectiveness and adverse effects, insufficient data on the adverse effects of vaccine, inadequate information regarding the vaccine. |
| 23 | Qunaibi et al. [59] | Jordan | General population | n = 36,220 | Concerns about vaccine side effects, expedited vaccine production, distrust in health care policies, vaccine-developing companies, and published studies, deficient data regarding vaccine type authorized in their countries |
| 24 | Faezi et al. [60] | Iran | General population | n = 1880 | Fear of vaccination-related illness, concern about vaccine side effects, lack of reliable information about vaccine promotion |
| 25 | Milan & Dau [61] | United States | Mothers with a mental health history | n = 240 | Low confidence in vaccinating against COVID-19, less belief in science, less influence from healthcare and governmental sources |
| 26 | Allington et al. [62] | UK | General population | n = 4343 | High reliance on social media information, less reliance on broadcast and print media information, reduced COVID-19 perceived risk, decreased trust in medics, scientists, and in government, coronavirus conspiracy suspicions |
| 27 | Xu et al. [63] | China | Parents | n = 4748 | Concerns about COVID-19 vaccine effectiveness and side effects |
| 28 | Castaneda-Vasquez [64] | Mexico | Health professionals | n = 543 | Misinformation related to vaccination and COVID-19 |
| 29 | Bono et al. [65] | Nine Low- and Middle-Income Countries | General population | n = 10,183 | Less confidence in vaccine effectiveness, fear of vaccine side effects |
| 30 | Al-Sanaf & Sallam [66] | Kuwait | Healthcare workers | n = 1019 | Vaccine conspiracy beliefs, sources of knowledge about COVID-19 vaccines, such as social media platforms |
| 31 | Sallam et al. [67] | Jordan, Kuwait and other Arab countries | General population | n = 3414 | Conspiracy beliefs, COVID-19 misinformation |
| 32 | Sallam et al. [68] | Jordan | University students | n = 1106 | Conspiracy beliefs, dependence on social media platforms |
| 33 | Kuçukkarapinar et al. [69] | Turkey | General population | n = 3888 | Conspiracy theories, lesser compliance with preventive measures, less knowledge about prevention, decreased risk perception, increased media hype, reduced trust in government and medical professionals |
| 34 | Plitch-loeb et al. [70] | United States | Vaccine priority population | n = 2650 | Vaccine information from social media or both social media and traditional channels |
| 35 | Alibrahim & Awad [71] | Kuwait | General population | n = 4147 | Possible side effects of the vaccine, quick development, efficacy in infection prevention, negative attitude regarding vaccines in general |
| 36 | Acar-Burkay & Cristian [72] | UK | General population | n = 435 | COVID-19 conspiracy beliefs, trust in healthcare authorities |
| 37 | Dambadarjaa et al. [73] | Mongolia | General population | n = 2875 | Social media reliance, COVID-19 vaccine type and side effects |
| 38 | Ebrahimi et al. [74] | Norway | General population | n = 4571 | Perceived risk of COVID-19 vaccines, belief in the power of natural immunity, preference to unmonitored media platforms |
| 39 | Ehde et al. [75] | United States | Adults with multiple sclerosis | n = 359 | Lower risk perception of COVID-19, lower trust in healthcare officials, concerns about the vaccine’s long-term effects, vaccine’s impact on health history/conditions |
| 40 | Almaghaslah et al. [76] | Saudi Arabia | General population | n = 862 | Vaccine effectiveness, news on social media |
| 41 | Jain et al. [77] | India | Medical students | n = 1068 | Vaccine efficacy and safety, lack of trust in government agencies, limited awareness about vaccination eligibility |
| 42 | Kumar et al. [78] | Qatar | Healthcare workers | n = 7821 | Safety and efficacy concerns of vaccine |
| 43 | Luk et al. [79] | Hong Kong | General population | n = 1501 | Insufficient knowledge about COVID-19 transmission, low COVID-19 perceived danger |
| 44 | Maraqa et al. [80] | Palestine | Healthcare workers | n = 1159 | Vaccine’s side effects |
| 45 | Mejri et al. [81] | Tunisia | Cancer patients | n = 329 | Vaccine’s interference with treatment efficacy or treatment outcome |
| 46 | Navarre et al. [82] | France | Hospital workers | n = 1964 | Distrust in health authorities and pharmaceutical lobbying |
| 47 | Oliveira et al. [83] | Brazil | General population | n = 4630 | Low confidence in vaccine safety and efficacy, in the healthcare system, or in policymakers’ and managers’ motivations to recommend vaccine, low immune preventable diseases risk perception, considering vaccination unnecessary |
| 48 | Park et al. [84] | South Korea | General population | n = 1000 | COVID-19 risk perceptions, vaccine safety, self-rated government trust, and political ideologies |
| 49 | Sethi et al. [85] | UK | General population | n = 4884 | Vaccine’s possible side effects |
| 50 | Sirikalyanpaiboon et al. [86] | Thailand | Physicians | n = 705 | Uncertainty of the vaccine efficacy, fear of adverse events |
| 51 | Yahia et al. [87] | Saudi Arabia | General population | n = 531 | Belief that vaccines are futile or hazardous |
| 52 | Yeşiltepe et al. [88] | Turkey | Nursing students | n = 1167 | Concerns regarding vaccine’s side effects, limited evidence on effectiveness and reliability |
| 53 | Albahri et al. [89] | UAE | General population | n = 2705 | Vaccine side effects and safety, belief that one needs to develop natural immunity |
| 54 | Singh et al. [90] | Hong Kong | General population | n = 245 | Negative attitudes towards COVID-19 vaccine |
| 55 | Ali & Hossain [91] | Bangladesh | General population | n = 1134 | Doubtful of the vaccine’s efficacy |
| 56 | Anjorin et al. [92] | Africa | General population | n = 5416 | Serious side effects of vaccine |
| 57 | Boon-Itt et al. [93] | Thailand | General population | n = 862 | Potential harmful side effects of a COVID-19 vaccine |
| 58 | Yilma et al. [94] | Ethiopia | Healthcare workers | n = 1314 | Perception that vaccines are unsafe |
| 59 | Fakonti et al. [95] | Cyprus | Nurses and Midwives | n = 437 | Expedited development of vaccines and fear of side effects |
| 60 | Li et al. [96] | China | Medical students | n = 2196 | Fear of vaccine’s consequences, concerns about short-term side effects and ineffectiveness |
| 61 | Magadmi et al. [97] | Saudi Arabia | General population | n = 3101 | Concerns about side effects |
| 62 | Khairat et al. [98] | United states | General population | n = 3142 | Lack of vaccine trust, concerns regarding vaccine side effects, lack of trust in government |
| 63 | Holeva et al. [99] | Greece | General population | n = 538 | Belief in a pre-planned pandemic |
| 64 | Hubach et al. [100] | United states | General population | n = 222 | Limited understanding and knowledge regarding the vaccine, including long-term complications, potential side effects, and scepticism around COVID-19 vaccine efficacy and development |
| 65 | Lo Moro et al. [101] | Italy | Medical students | n = 929 | Adverse reactions after a vaccination, relative’s advice against COVID-19 vaccination |
| 66 | Silva et al. [102] | United states | College students | n = 237 | Concerns about vaccine effectiveness and safety, limited information |
| 67 | Soares et al. [103] | Portugal | General population | n = 1943 | Reduced confidence in COVID-19 vaccine and the healthcare service, perception of the information provided as contradictory and inconsistent, worse perception of government actions |
| 68 | Kavanagh et al. [104] | Australia | Disability support workers | n = 252 | Inadequate safety data, side effects, distrust in the government |
| 69 | Hwang et al. [105] | South Korea | General population | n = 13,012 | Lack of COVID-19 vaccine confidence, less or no COVID-19 fear |
| 70 | Hong et al. [106] | China | Cancer patients | n = 2158 | Worry that the COVID-19 vaccine might worsen the prognosis of cancer |
| 71 | Shareef et al. [107] | Iraq | General population | n = 1221 | Concerns about vaccine’s future side effects |
| 72 | Lee & You [108] | South Korea | General population | n = 1016 | Perceived barriers of vaccination, lower trust in government |
| 73 | Kumari et al. [109] | India | Pregnant and lactating women | n = 313 | Concerns about the vaccine’s future effects on the foetus, rushed development |
| 74 | Moscardino et al. [110] | Italy | General population | n = 1177 | Conspiracy theories and negative attitudes toward vaccines |
| 75 | Mundagowa et al. [111] | Zimbabwe | General population | n = 1168 | Uncertainty about the safety and effectiveness of the vaccine, lack of trust in the government’s ability to ensure effective vaccine availability |
| 76 | Zammit et al. [112] | Tunisia | Health professionals | n = 493 | Concerns regarding components of vaccines |
| 77 | Ekowo et al. [113] | Nigeria | General population | n = 1283 | Belief in one’s own immunity, side effects of the vaccine |
| 78 | Skeens et al. [114] | United states | Parents of children with cancer | n = 491 | Concerns regarding vaccine side effects on children |
| 79 | Walsh et al. [115] | Ireland & UK | General population | n = 1079 | Low peer influence, lower satisfaction with government response, low fear of COVID-19, low civic responsibility, low adherence to healthcare guidelines, low trust in authorities, low positive vaccination attitudes, perceived risk of COVID-19 vaccine, low perceived vaccine benefit, perceived vaccine severity, low perceived susceptibility |
| Author(s) | No. of Studies | Major Themes | Sub-Themes |
|---|---|---|---|
| Willis et al. [42]; Yang et al. [45]; Nazli et al. [46]; Chaudhary et al. [51]; Chen et al. [52]; İkiışık et al. [56]; Allington et al. [62]; Kuçukkarapinar et al. [69]; Ehde et al. [75]; Luk et al. [79]; Oliveira et al. [83]; Park et al. [84]; Hwang et al. [105]; Walsh et al. [115] | 14 | Appraisal of COVID-19 | Low perceived susceptibility to virus Low perceived severity of disease No fear of COVID-19 |
| Fisher et al. [38]; Lin et al. [39]; Alqudeimat et al. [41]; Cordina et al. [44]; Altulahi et al. [48]; Aloweidi et al. [49]; Benham et al. [50]; Chaudhary et al. [51]; Danabal et al. [53]; Alabdulla et al. [57]; Saied et al. [58]; Qunaibi et al. [59]; Faezi et al. [60]; Xu et al. [63]; Bono et al. [65]; Alibrahim & Awad [71]; Dambadarjaa et al. [73]; Ebrahimi et al. [74]; Ehde et al. [75]; Almaghaslah et al. [76]; Jain et al. [77]; Kumar et al. [78]; Maraqa et al. [80]; Mejri et al. [81]; Park et al. [84]; Sethi et al. [85]; Sirikalyanpaiboon et al. [86]; Yahia et al. [87]; Yeşiltepe et al. [88]; Albahri et al. [89]; Ali & Hossain [91]; Anjorin et al. [92]; Boon-Itt et al. [93]; Yilma et al. [94]; Fakonti et al. [95]; Li et al. [96]; Magadmi et al. [97]; Khairat et al. [98]; Hubach et al. [100]; Lo Moro et al. [101]; Silva et al. [102]; Kavanagh et al. [104]; Shareef et al. [107]; Lee & You [108]; Kumari et al. [109]; Mundagowa et al. [111]; Ekowo et al. [113]; Skeens et al. [114]; Walsh et al. [115] | 49 | Vaccine safety and side effects | Vaccine is unsafe Vaccines are dangerous Concern about vaccination Vaccine causes side effects Vaccine’s health-related concerns Concerns about components of vaccines |
| Fisher et al. [38]; Caserotti. [40]; Willis et al. [42]; Danabal et al. [53]; Hossain et al. [55]; İkiışık et al. [56]; Milan & Dau [61]; Alibrahim & Awad [71]; Ebrahimi et al. [74]; Oliveira et al. [83]; Yahia et al. [87]; Albahri et al. [89]; Singh et al. [90]; Ali & Hossain [91]; Khairat et al. [98]; Soares et al. [103]; Hwang et al. [105]; Moscardino et al. [110]; Ekowo et al. [113]; Walsh et al. [115] | 20 | General vaccine confidence/trust | Disagree with immunization Vaccination is unnecessary No confidence in value of vaccines Anti-vaccine attitudes or beliefs Low vaccine trust in general Belief in the power of natural immunity |
| Murphy et al. [25]; Fisher et al. [38]; Schernhammer et al. [47]; Benham et al. [50]; Qunaibi et al. [59]; Milan & Dau [61]; Allington et al. [62]; Kuçukkarapinar et al. [69]; Acar-Burkay & Cristian [72]; Ehde et al. [75]; Jain et al. [77]; Navarre et al. [82]; Oliveira et al. [83]; Park et al. [84]; Khairat et al. [98]; Soares et al. [103]; Kavanagh et al. [104]; Lee & You [108]; Mundagowa et al. [111]; Walsh et al. [115] | 20 | Trust in the healthcare professionals and government | No trust in the government Perceived government pressure to vaccinate Low influence of healthcare provider |
| Murphy et al. [25]; Qunaibi et al. [59]; Milan & Dau [61]; Allington et al. [62]; Alibrahim & Awad [71]; Navarre et al. [82]; Oliveira et al. [83]; Fakonti et al. [95]; Hubach et al. [100]; Kumari et al. [109] | 10 | Scepticism around vaccine production | Expedited vaccine production Distrust in vaccine-developing companies Lack of trust in scientists Less belief in science Pharmaceutical lobbying |
| Murphy et al. [25]; Nazli et al. [46]; Aloweidi et al. [49]; Hossain et al. [54]; Allington et al. [62]; Castaneda-Vasquez [64]; Al-Sanaf & Sallam [66]; Sallam et al. [67]; Sallam et al. [68]; Kuçukkarapinar et al. [69]; Acar-Burkay & Cristian [72]; Holeva et al. [99]; Moscardino et al. [110] | 13 | Conspiracy beliefs | Origin of vaccine Biological weapon Media hype Misinformation/disinformation Belief in conspiracy theories |
| Freeman et al. [43]; Cordina et al. [44]; Yang et al. [45]; Nazli et al. [46]; Faezi et al. [60]; Xu et al. [63]; Sirikalyanpaiboon et al. [86] | 7 | Emotions | Worry about vaccine Injection fear No stress because of COVID-19 Fear of vaccine-related illness Fear of adverse events |
| Murphy et al. [25]; Fisher et al. [38]; Cordina et al. [44]; Chaudhary et al. [51]; Hossain et al. [55]; Saied et al. [58]; Qunaibi et al. [59]; Faezi et al. [60]; Allington et al. [62]; Al-Sanaf & Sallam [66]; Sallam et al. [68]; Kuçukkarapinar et al. [69]; Plitch-loeb et al. [70]; Dambadarjaa et al. [73]; Ebrahimi et al. [74]; Almaghaslah et al. [76]; Jain et al. [77]; Luk et al. [79]; Yeşiltepe et al. [88]; Hubach et al. [100]; Silva et al. [102]; Soares et al. [103]; Kavanagh et al. [104] | 23 | Information and knowledge about vaccine | Inadequate knowledge about vaccine Incorrect knowledge Lack of scientific data Less satisfaction with information Influence of information through social media Perceived lack of information for vaccination decision |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romate, J.; Rajkumar, E.; Gopi, A.; Abraham, J.; Rages, J.; Lakshmi, R.; Jesline, J.; Bhogle, S. What Contributes to COVID-19 Vaccine Hesitancy? A Systematic Review of the Psychological Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2022, 10, 1777. https://doi.org/10.3390/vaccines10111777
Romate J, Rajkumar E, Gopi A, Abraham J, Rages J, Lakshmi R, Jesline J, Bhogle S. What Contributes to COVID-19 Vaccine Hesitancy? A Systematic Review of the Psychological Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines. 2022; 10(11):1777. https://doi.org/10.3390/vaccines10111777
Chicago/Turabian StyleRomate, John, Eslavath Rajkumar, Aswathy Gopi, John Abraham, John Rages, R. Lakshmi, Joshy Jesline, and Sudha Bhogle. 2022. "What Contributes to COVID-19 Vaccine Hesitancy? A Systematic Review of the Psychological Factors Associated with COVID-19 Vaccine Hesitancy" Vaccines 10, no. 11: 1777. https://doi.org/10.3390/vaccines10111777
APA StyleRomate, J., Rajkumar, E., Gopi, A., Abraham, J., Rages, J., Lakshmi, R., Jesline, J., & Bhogle, S. (2022). What Contributes to COVID-19 Vaccine Hesitancy? A Systematic Review of the Psychological Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines, 10(11), 1777. https://doi.org/10.3390/vaccines10111777







