Ingraining Polio Vaccine Acceptance through Public Service Advertisements in the Digital Era: The Moderating Role of Misinformation, Disinformation, Fake News, and Religious Fatalism
Abstract
:1. Introduction
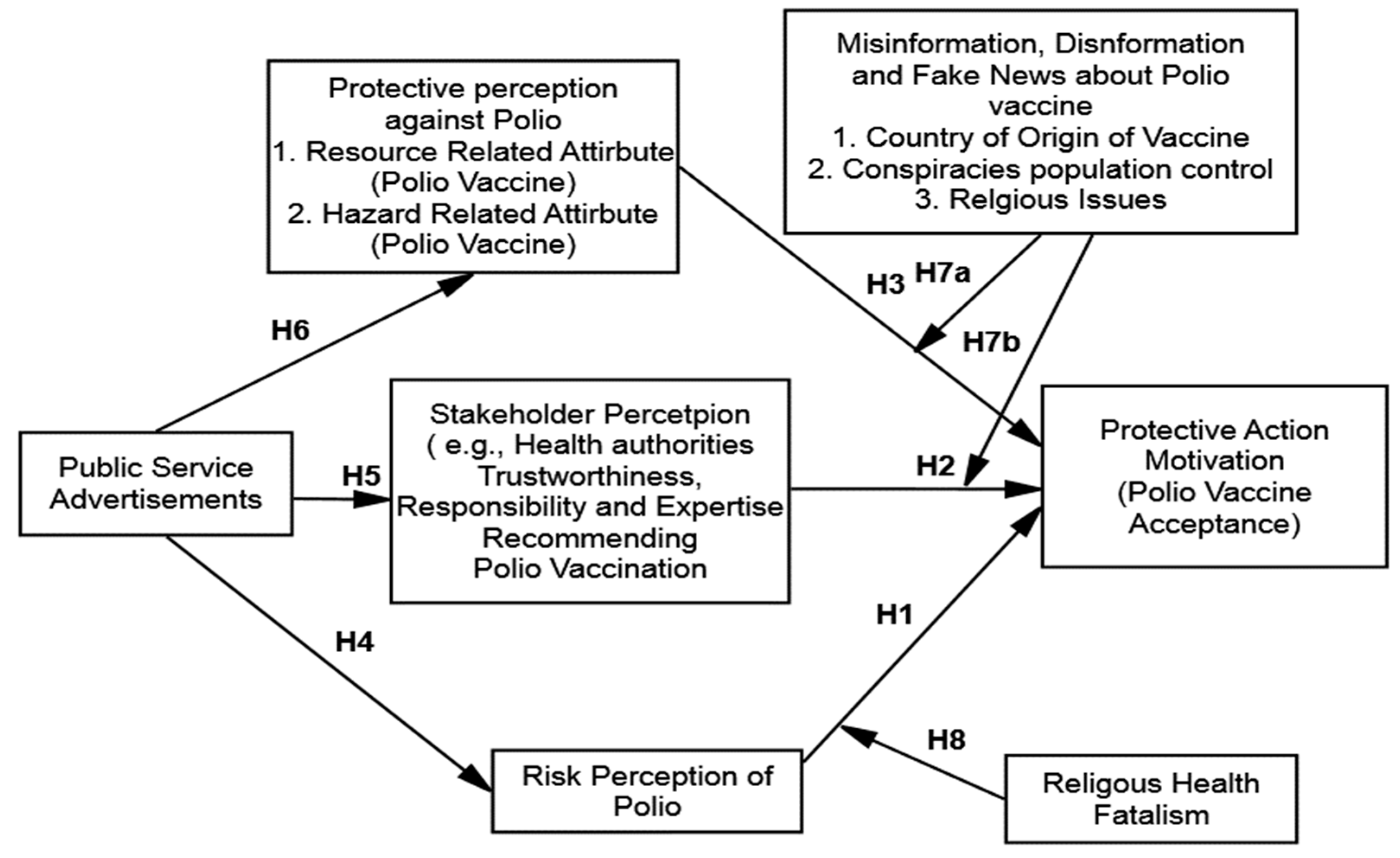
2. Literature Review
2.1. Protective Action Decision Theory
2.1.1. Risk Perception
2.1.2. Stakeholder Perception
2.1.3. Protective Action Perception
2.1.4. Public Service Advertisements
2.1.5. Misinformation, Disinformation, and Fake News
2.1.6. Religious Fatalism
3. Materials and Methods
3.1. Design, Participants, and Procedure
3.2. Instrumentation
4. Results
4.1. Demographic and Preliminary Analysis
4.2. Measurement Model
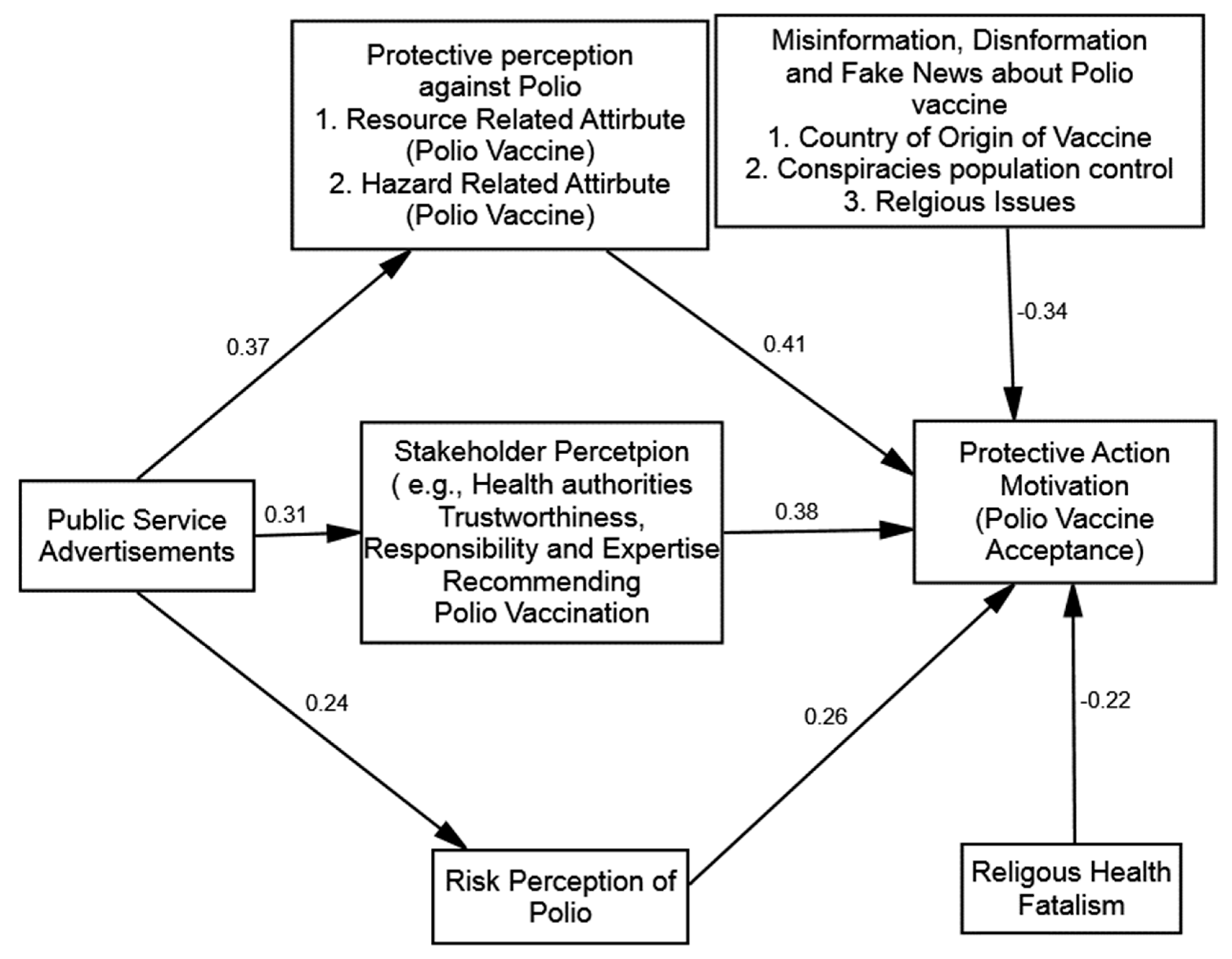
4.3. Hypothesis Testing
4.4. Moderation Analysis
5. Discussion
5.1. Managerial Implications
5.2. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GPEI Global Polio Eradication Initiative. 2020. Available online: https://polioeradication.org/ (accessed on 12 August 2022).
- GPEI Polio Eradication Strategy 2022–2026: Delivering on a Promise. 2021. Available online: https://polioeradication.org/wp-content/uploads/2022/06/Polio-Eradication-Strategy-2022-2026-Delivering-on-a-Promise.pdf (accessed on 9 August 2022).
- Brandão, L.G.P.; Lopes, G.S.; Oliveira, S.D.S.; da Silva, E.E.; Brasil, P.E.A.A.D. Seroprevalence of antibodies against the three serotypes of poliovirus and IPV vaccine response in adult solid organ transplant candidates. Vaccine 2018, 36, 4681–4686. [Google Scholar] [CrossRef]
- Molodecky, N.A.; Jafari, H.; Safdar, R.M.; Ahmed, J.A.; Mahamud, A.; Bandyopadhyay, A.S.; Shukla, H.; Quddus, A.; Zaffran, M.; Sutter, R.W.; et al. Modelling the spread of serotype-2 vaccine derived-poliovirus outbreak in Pakistan and Afghanistan to inform outbreak control strategies in the context of the COVID-19 pandemic. Vaccine 2021. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.M.; Kalkowska, D.A. Reflections on Modeling Poliovirus Transmission and the Polio Eradication Endgame. Risk Anal. 2021, 41, 229–247. [Google Scholar] [CrossRef] [PubMed]
- Ataullahjan, A.; Ahsan, H.; Soofi, S.; Habib, M.A.; Bhutta, Z.A. Eradicating polio in Pakistan: A systematic review of programs and policies. Expert Rev. Vaccines 2021, 20, 661–678. [Google Scholar] [CrossRef] [PubMed]
- WHO Poliomyelitis. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/poliomyelitis (accessed on 19 July 2022).
- Kalkowska, D.A.; Thompson, K. Insights from Modeling Preventive Supplemental Immunization Activities as a Strategy to Eliminate Wild Poliovirus Transmission in Pakistan and Afghanistan. Risk Anal. 2021, 41, 266–272. [Google Scholar] [CrossRef]
- Ittefaq, M.; Abwao, M.; Rafique, S. Polio vaccine misinformation on social media: Turning point in the fight against polio eradication in Pakistan. Hum. Vaccines Immunother. 2021, 17, 2575–2577. [Google Scholar] [CrossRef]
- PPEP Pakistan Polio Eradication Programme. Polio cases in Provinces: 2021. 2021. Available online: https://www.endpolio.com.pk/polioin-pakistan/polio-cases-in-provinces (accessed on 23 July 2022).
- Khan, M.U.; Ahmad, A.; Aqeel, T.; Salman, S.; Ibrahim, Q.; Idrees, J. Knowledge, attitudes and perceptions towards polio immunization among residents of two highly affected regions of Pakistan. BMC Public Health 2015, 15, 1100. [Google Scholar] [CrossRef] [Green Version]
- Hussain, S.F.; Boyle, P.; Patel, P.; Sullivan, R. Eradicating polio in Pakistan: An analysis of the challenges and solutions to this security and health issue. Glob. Health 2016, 12, 63. [Google Scholar] [CrossRef] [Green Version]
- Woods, T.P. (Ed.) Efficacy, Eugenics, and Law in the Modern Vaccine Regime, in Pandemic Police Power, Public Health and the Abolition Question; Springer: Dartmpouth, NH, USA, 2022; pp. 163–216. [Google Scholar]
- Bradshaw, A.S.; Shelton, S.S.; Fitzsimmons, A.; Treise, D. From cover-up to catastrophe: How the anti-vaccine propaganda documentary ‘Vaxxed’ impacted student perceptions and intentions about MMR vaccination. J. Commun. Healthc. 2022, 1–13. [Google Scholar] [CrossRef]
- Heath, R.L.; Lee, J.; Palenchar, M.J.; Lemon, L.L. Risk Communication Emergency Response Preparedness: Contextual Assessment of the Protective Action Decision Model. Risk Anal. 2018, 38, 333–344. [Google Scholar] [CrossRef]
- Raza, S.H.; Iftikhar, M.; Mohamad, B.; Pembecioğlu, N.; Altaf, M. Precautionary Behavior Toward Dengue Virus Through Public Service Advertisement: Mediation of the Individual’s Attention, Information Surveillance, and Elaboration. SAGE Open 2020, 10, 2158244020929301. [Google Scholar] [CrossRef]
- Lindell, M.K.; Perry, R.W. The Protective Action Decision Model: Theoretical Modifications and Additional Evidence. Risk Anal. 2012, 32, 616–632. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Wei, J.; Shi, X. Compliance with recommended protective actions during an H7N9 emergency: A risk perception perspective. Disasters 2018, 42, 207–232. [Google Scholar] [CrossRef]
- Yan, J.; Ji, J.; Gao, L. From Health Campaign to Interpersonal Communication: Does Traditional Diet Culture Hinder the Communication of the Chinese Gongkuai Campaign? Int. J. Environ. Res. Public Health 2022, 19, 9992. [Google Scholar] [CrossRef]
- Terpstra, T.; Lindell, M.K. Citizens’ perceptions of flood hazard adjustments: An application of the protective action decision model. Environ. Behav. 2013, 45, 993–1018. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Ouyang, Z.; Cheng, P. Predicting consumers’ adoption of electric vehicles during the city smog crisis: An application of the protective action decision model. J. Environ. Psychol. 2019, 64, 30–38. [Google Scholar] [CrossRef]
- Guo, Y.; An, S.; Comes, T. From warning messages to preparedness behavior: The role of risk perception and information interaction in the COVID-19 pandemic. Int. J. Disaster Risk Reduct. 2022, 73, 102871. [Google Scholar] [CrossRef]
- Jia, J.S.; Jia, J.; Hsee, C.K.; Shiv, B. The role of hedonic behavior in reducing perceived risk: Evidence from postearthquake mobile-app data. Psychol. Sci. 2017, 28, 23–35. [Google Scholar] [CrossRef] [Green Version]
- Zafri, N.M.; Khan, A.; Jamal, S.; Alam, B.M. Risk perceptions of COVID-19 transmission in different travel modes. Transp. Res. Interdiscip. Perspect. 2022, 13, 100548. [Google Scholar] [CrossRef]
- Beg, B.M.; Hussain, T.; Ahmad, M.; Areej, S.; Majeed, A.; Rasheed, M.A.; Ahmad, M.M.; Shoaib, Q.-U.; Aroosa, S. Perceived risk and perceptions of COVID-19 vaccine: A survey among general public in Pakistan. PLoS ONE 2022, 17, e0266028. [Google Scholar] [CrossRef]
- Shahani, R.; Chu, J.; Rufai, O.H.; Zawar, A.; Muhideen, S.; Dilawar, S.; Amosun, T.S. Understanding the Role of Psychosocial Factors in Pakistani Parents’ Hesitancy to Vaccinate Their Kids: The Mediating Role of Knowledge and Mistrust of Science about the COVID-19 Vaccine. Vaccines 2022, 10, 1260. [Google Scholar] [CrossRef] [PubMed]
- Hocevar, K.P.; Metzger, M.; Flanagin, A.J. Source credibility, expertise, and trust in health and risk messaging. In Oxford Research Encyclopedia of Communication; Nussbaum, J., Ed.; Oxford University Press: Oxford, UK, 2017. [Google Scholar]
- Trumbo, C.W.; McComas, K.A. The Function of Credibility in Information Processing for Risk Perception. Risk Anal. 2003, 23, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Xie, X.; Gan, Y. Information source and valence: How information credibility influences earthquake risk perception. J. Environ. Psychol. 2011, 31, 129–136. [Google Scholar] [CrossRef]
- Ellwanger, J.H.; da Veiga, A.B.G.; Kaminski, V.D.L.; Valverde-Villegas, J.M.; de Freitas, A.W.Q.; Chies, J.A.B. Control and prevention of infectious diseases from a One Health perspective. Genet. Mol. Biol. 2021, 44, e20200256. [Google Scholar] [CrossRef] [PubMed]
- Kremer, I. The Effect of Education, Age, and Gender on Disease Risk Perception and Disease Severity Perception at a Community College During the COVID-19 Pandemic. Ph.D. Thesis, AT Still University of Health Sciences, Kirksville, MO, USA, 2022. [Google Scholar]
- Fischhoff, B.; Brewer, N.T.; Downs, J.S. Communication Risks and Benefits: An evidence-based user’s guide. In Food and Drug Administration (FDA); US Department of Health and Human Services: Concord, NH, USA, 2011. [Google Scholar]
- Iftikhar, M.; Yousaf, M. The Impact of Climate Change Coverage on Public Adherence towards Health Threat: An Empirical Validation of the Health Belief Model. sjesr 2021, 4, 402–413. [Google Scholar] [CrossRef]
- Hallahan, K. Seven Models of Framing: Implications for Public Relations. J. Public Relations Res. 1999, 11, 205–242. [Google Scholar] [CrossRef]
- Jin, Q.; Raza, S.; Yousaf, M.; Zaman, U.; Siang, J. Can Communication Strategies Combat COVID-19 Vaccine Hesitancy with Trade-Off between Public Service Messages and Public Skepticism? Experimental Evidence from Pakistan. Vaccines 2021, 9, 757. [Google Scholar] [CrossRef]
- Yousaf, M.; Raza, S.H.; Mahmood, N.; Core, R.; Zaman, U.; Malik, A. Immunity debt or vaccination crisis? A multi-method evidence on vaccine acceptance and media framing for emerging COVID-19 variants. Vaccine 2022, 40, 1855–1863. [Google Scholar] [CrossRef]
- Wakefield, M.A.; Loken, B.; Hornik, R.C. Use of mass media campaigns to change health behaviour. Lancet 2010, 376, 1261–1271. [Google Scholar] [CrossRef] [Green Version]
- Lapointe, L.; Ramaprasad, J.; Vedel, I. Creating health awareness: A social media enabled collaboration. Health Technol. 2014, 4, 43–57. [Google Scholar] [CrossRef]
- Fetzer, J.H. Disinformation: The Use of False Information. Minds Mach. 2004, 14, 231–240. [Google Scholar] [CrossRef]
- Gelfert, A. Fake News: A Definition. Informal Log. 2018, 38, 84–117. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef] [PubMed]
- Ali, S. Combatting Against COVID-19 & Misinformation: A Systematic Review. Hum. Arenas 2020, 5, 337–352. [Google Scholar] [CrossRef]
- Basch, C.; Zybert, P.; Reeves, R.; Basch, C.E. What do popular You TubeTM videos say about vaccines? Child Care Health Dev. 2017, 43, 499–503. [Google Scholar] [CrossRef]
- A Gisondi, M.; Barber, R.; Faust, J.S.; Raja, A.; Strehlow, M.C.; Westafer, L.M.; Gottlieb, M. A Deadly Infodemic: Social Media and the Power of COVID-19 Misinformation. J. Med. Internet Res. 2022, 24, e35552. [Google Scholar] [CrossRef]
- Rad, R.E.; Mohseni, S.; Takhti, H.K.; Azad, M.H.; Shahabi, N.; Aghamolaei, T.; Norozian, F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: A cross-sectional study. BMC Public Health 2021, 21, 466. [Google Scholar] [CrossRef]
- Franklin, M.D.; Schlundt, D.G.; Wallston, K.A. Development and Validation of a Religious Health Fatalism Measure for the African-American Faith Community. J. Health Psychol. 2008, 13, 323–335. [Google Scholar] [CrossRef]
- Dettenborn, L.; Duhamel, K.; Butts, G.; Thompson, H.; Jandorf, L. Cancer fatalism and its demographic correlates among African American and Hispanic women: Effects on adherence to cancer screening. J. Psychosoc. Oncol. 2004, 22, 47–60. [Google Scholar] [CrossRef]
- Joshanloo, M. The relationship between fatalistic beliefs and well-being depends on personal and national religiosity: A study in 34 countries. Heliyon 2022, 8, e09814. [Google Scholar] [CrossRef]
- Salazar-Collier, C.L.; Reininger, B.M.; Wilkinson, A.V.; Kelder, S.H. Exploration of Fatalism and Religiosity by Gender and Varying Levels of Engagement Among Mexican-American Adults of a Type 2 Diabetes Management Program. Front. Public Health 2021, 9, 1414. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef] [PubMed]
- Yin, F.; Wu, Z.; Xia, X.; Ji, M.; Wang, Y.; Hu, Z. Unfolding the Determinants of COVID-19 Vaccine Acceptance in China. J. Med. Internet Res. 2021, 23, e26089. [Google Scholar] [CrossRef] [PubMed]
- Eveland, W.P., Jr. The cognitive mediation model of learning from the news: Evidence from nonelection, off-year election, and presidential election contexts. Commun. Res. 2001, 28, 571–601. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Nunnally, J.C. The assessment of reliability. Psychom. Theory 1994, 3, 248–292. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Ozawa, S.; Stack, M.L. Public trust and vaccine acceptance-international perspectives. Hum. Vaccines Immunother. 2013, 9, 1774–1778. [Google Scholar] [CrossRef]
- Eze, C.I. An Evaluation of Communication Strategies Used in Polio Immunization Campaigns in Kaduna and Sokoto States, Nigeria. Ph.D. Thesis, University of Ibadan, Ibadan, Nigeria, 2016. [Google Scholar]
- Bonu, S.; Rani, M.; Baker, T.D. The impact of the national polio immunization campaign on levels and equity in immunization coverage: Evidence from rural North India. Soc. Sci. Med. 2003, 57, 1807–1819. [Google Scholar] [CrossRef]



| Mean | PSA | RP | RF | SP | PPA | ID | PAM | |
|---|---|---|---|---|---|---|---|---|
| PSA | 3.25 | 1 | ||||||
| RP | 3.65 | 0.089 | 1 | |||||
| RF | 3.56 | −0.078 | −0.472 | 1 | ||||
| SP | 3.81 | 0.187 | −0.145 | −0.202 | 1 | |||
| PPA | 2.78 | 0.087 | 0.326 | 0.506 | −0.171 | 1 | ||
| ID | 4.09 | −0.127 | −0.063 | 0.151 | −0.234 | −0.072 | 1 | |
| PAM | 3.93 | 0.054 | 0.025 | 0.081 | 0.252 | 0.193 | 0.164 | 1 |
| Variables | Estimate |
|---|---|
| Public Service Advertisements | |
| PSA1 | 0.79 |
| PSA2 | 0.92 |
| PSA3 | 0.64 |
| Risk Perception | |
| RP1 | 0.97 |
| RP2 | 0.86 |
| RP3 | 0.76 |
| Stakeholder Perception | |
| SP1 | 0.81 |
| SP2 | 0.89 |
| SP3 | 0.77 |
| Religious Fatalism | |
| RF1 | 0.75 |
| RF2 | 0.69 |
| RF3 | 0.68 |
| RF4 | 0.77 |
| Protection Action Motivation (Polio Vaccine Acceptance) | |
| PAM1 | 0.80 |
| PAM2 | 0.77 |
| PAM3 | 0.83 |
| Protection Perception Attributes (Dimension: Resource-Related Attributes) | |
| RA1 | 0.85 |
| RA2 | 0.89 |
| RA3 | 0.87 |
| Protection Perception Attributes (Dimension: Hazard-Related Attributes) | |
| HA1 | 0.84 |
| HA2 | 0.79 |
| Misinformation | |
| MI1 | 0.83 |
| MI2 | 0.85 |
| MI3 | 0.72 |
| Variables | CR | AVE | PSA | RP | SP | PAM | PPA | RF | MI |
|---|---|---|---|---|---|---|---|---|---|
| PSA | 0.830 | 0.63 | 0.790 | ||||||
| RP | 0.898 | 0.75 | 0.158 | 0.865 | |||||
| SP | 0.864 | 0.68 | 0.182 | −0.042 | 0.824 | ||||
| PAM | 0.844 | 0.64 | 0.076 | 0.190 | 0.33 | 0.802 | |||
| PPA | 0.966 | 0.93 | 0.146 | 0.073 | 0.17 | 0.202 | 0.967 | ||
| RF | 0.815 | 0.53 | 0.124 | −0.17 | −0.24 | −0.16 | −0.53 | 0.725 | |
| MI | 0.844 | 0.65 | 0.105 | −0.15 | −0.16 | −0.23 | −0.36 | 0.505 | 0.802 |
| Direct Influence | β | p-Value | T-Vale | Hypothesis |
|---|---|---|---|---|
| Risk Perception → PAM (Polio Vaccine Acceptance) | 0.26 | 0.001 | 5.81 | H1 Supported |
| Stakeholder Perception → PAM (Polio Vaccine Acceptance) | 0.38 | 0.001 | 6.91 | H2 Supported |
| Protective Action Perception → PAM (Polio Vaccine Acceptance) | 0.41 | 0.001 | 7.18 | H3 Supported |
| PSA → Risk Perception | 0.24 | 0.001 | 4.25 | H4 Supported |
| PSA → Stakeholder Perception | 0.31 | 0.001 | 5.98 | H5 Supported |
| PSA → Protective Perception Against Polio | 0.37 | 0.001 | 6.34 | H6 Supported |
| Misinformation X Protective Perception → PAM | −0.27 | 0.012 | 3.57 | H7a Supported |
| Misinformation X Stakeholder Perception → PAM | −0.21 | 0.031 | 3.61 | H7b Supported |
| Religious Fatalism X Risk Perception → PAM | −0.18 | 0.001 | 4.38 | H8 Supported |
| Authors | Year | Barriers | Method | Context |
|---|---|---|---|---|
| Puri [41] | 2020 | Social Media Disinformation | Survey | Vaccine Hesitancy |
| Ali [42] | 2020 | Misinformation | Systematic Review | Positive Psychology |
| Basch [43] | 2017 | Vaccination Risks and Reactions | Content Analysis YouTube | Vaccine and Children |
| Gisondi [44] | 2022 | Infodemics and Misinformation | Opinion | Vaccine Hesitancy |
| Ittefaq et al. [9] | 2021 | Misleading Viral Videos | Commentary | Polio Vaccine |
| Dettenborn [47] | 2004 | Religious Fatalism | Cross-Sectional study | Health Behavior |
| Salazar-Collier [49] | 2021 | Religious Fatalism | Cross-Sectional study | Health Behavior |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, Q.; Raza, S.H.; Yousaf, M.; Munawar, R.; Shah, A.A.; Hassan, S.; Shaikh, R.S.; Ogadimma, E.C. Ingraining Polio Vaccine Acceptance through Public Service Advertisements in the Digital Era: The Moderating Role of Misinformation, Disinformation, Fake News, and Religious Fatalism. Vaccines 2022, 10, 1733. https://doi.org/10.3390/vaccines10101733
Jin Q, Raza SH, Yousaf M, Munawar R, Shah AA, Hassan S, Shaikh RS, Ogadimma EC. Ingraining Polio Vaccine Acceptance through Public Service Advertisements in the Digital Era: The Moderating Role of Misinformation, Disinformation, Fake News, and Religious Fatalism. Vaccines. 2022; 10(10):1733. https://doi.org/10.3390/vaccines10101733
Chicago/Turabian StyleJin, Qiang, Syed Hassan Raza, Muhammad Yousaf, Rehana Munawar, Amjad Ali Shah, Saima Hassan, Rehan Sadiq Shaikh, and Emenyonu C. Ogadimma. 2022. "Ingraining Polio Vaccine Acceptance through Public Service Advertisements in the Digital Era: The Moderating Role of Misinformation, Disinformation, Fake News, and Religious Fatalism" Vaccines 10, no. 10: 1733. https://doi.org/10.3390/vaccines10101733
APA StyleJin, Q., Raza, S. H., Yousaf, M., Munawar, R., Shah, A. A., Hassan, S., Shaikh, R. S., & Ogadimma, E. C. (2022). Ingraining Polio Vaccine Acceptance through Public Service Advertisements in the Digital Era: The Moderating Role of Misinformation, Disinformation, Fake News, and Religious Fatalism. Vaccines, 10(10), 1733. https://doi.org/10.3390/vaccines10101733










