Immunoinformatics Approach to Design Multi-Epitope-Based Vaccine against Machupo Virus Taking Viral Nucleocapsid as a Potential Candidate
Abstract
:1. Introduction
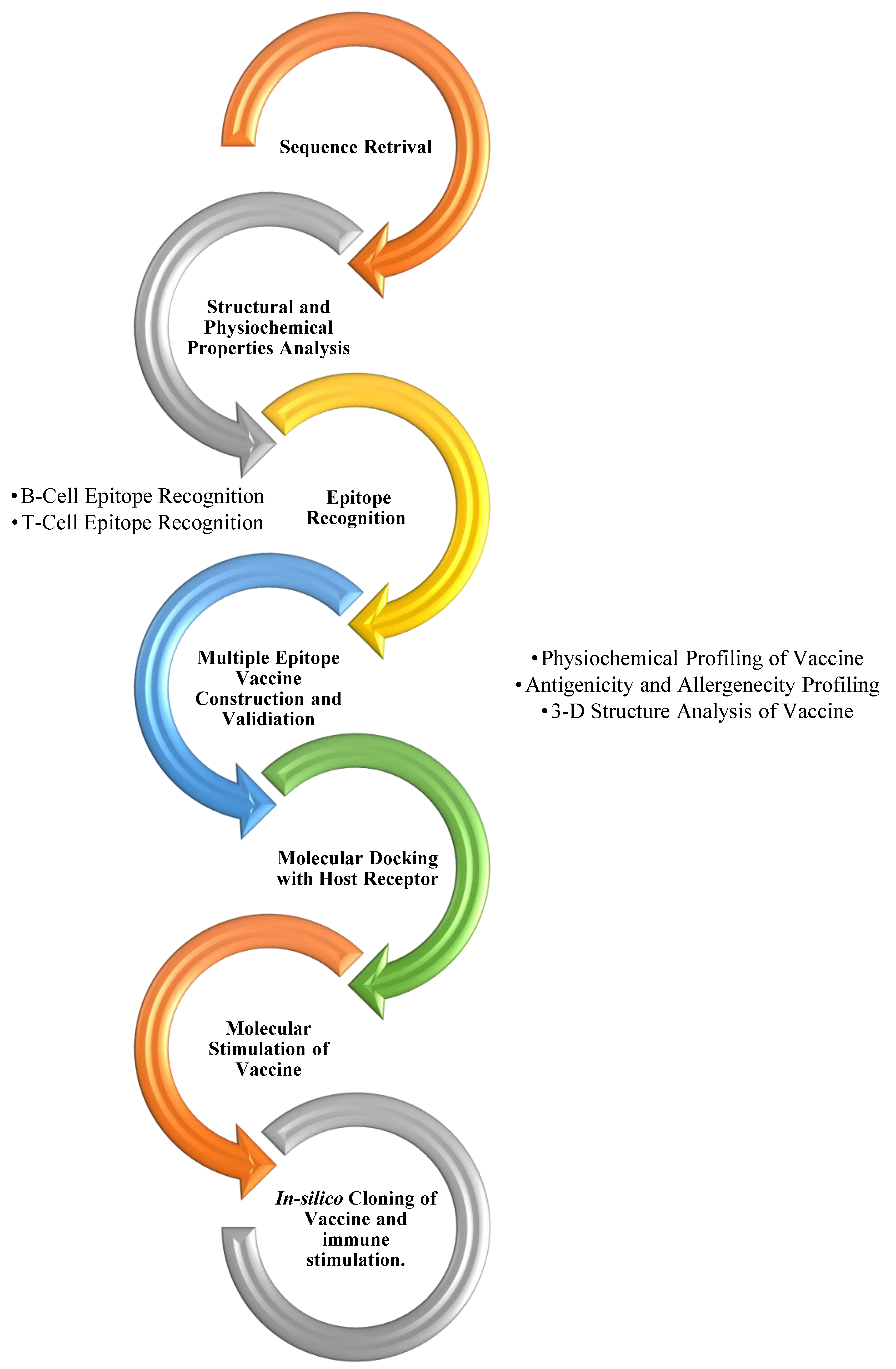
2. Materials and Methods
2.1. Sequence Retrieval
2.2. Physiochemical Analysis
2.3. Allergenicity and Antigenicity Profiling of Proteins
2.4. Prediction of the Linear B-Cell Epitopes
2.5. Prediction of the MHC-Specific Epitopes
2.6. Population Coverage
2.7. Finalizing the Construct
2.8. Physiochemical Properties of the Construct
2.9. 3-D Structural Analysis of Vaccines and Receptors
2.10. Refinement of the Construct and the Receptor
2.11. Vaccine Construct Validation
2.12. Molecular Docking with Host Receptor
2.13. Expression Analysis
2.14. Immune Stimulation
3. Results and Analysis
3.1. Sequence Retrieval
3.2. Physiochemical Analysis
3.3. Allergenicity and Antigenicity Profiling of Nucleocapsid Protein
3.4. B-Cell Epitope Prediction
3.5. T-Cell Epitope Recognition
3.5.1. MHC-I-Restricting Epitopes
3.5.2. MHC-II-Restricting Epitopes
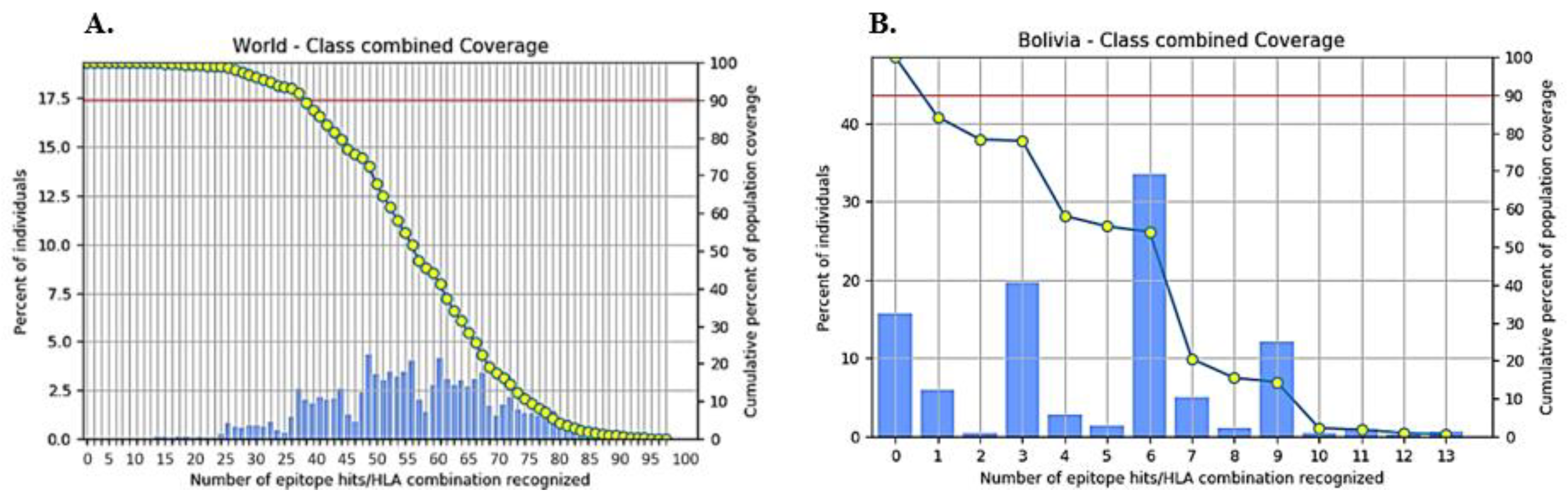
3.6. Population Coverage of the T-Cell-Specific Epitopes
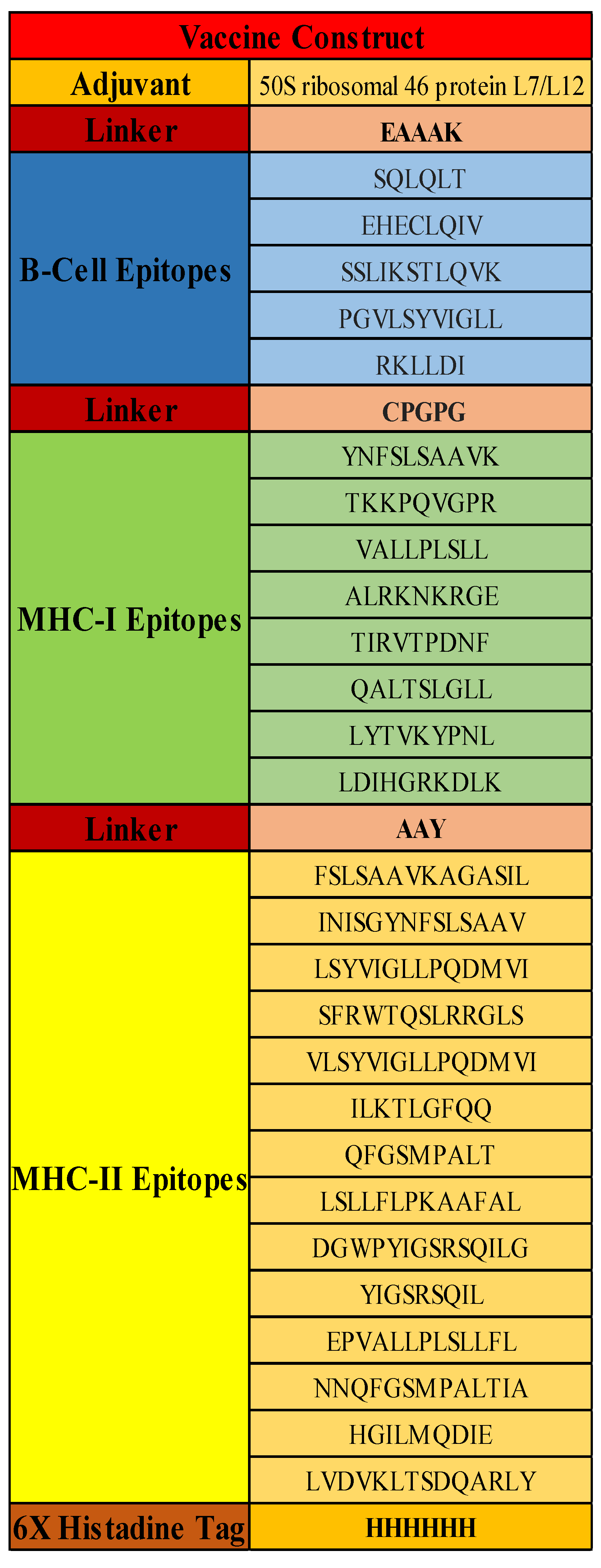
3.7. Vaccine Construct
3.8. Secondary Structure and Physiochemical Properties of Vaccine
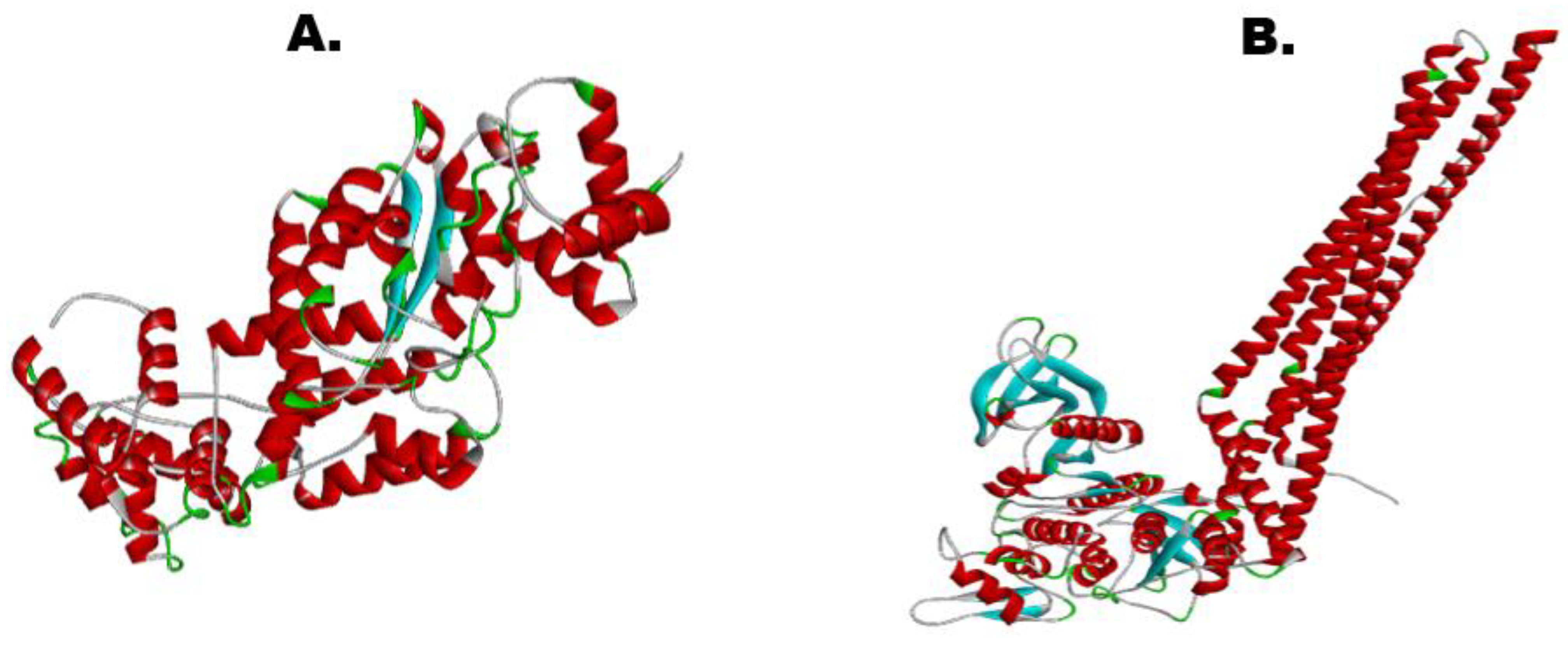
3.9. 3-D Structure of Vaccine and Receptor IKBKE
3.10. Protein Refinement of Vaccine and IKBKE Receptor
3.11. Vaccine Model Stability and Validation
3.12. Molecular Docking
3.13. Molecular Dynamics Simulation
3.14. In-Silico Cloning with Snapgene
3.15. Immune Stimulation Analysis
4. Discussion
5. Conclusions
Contribution/Prospects
- The vaccine design against Bolivian Hemorrhage Fever is among the top priorities of the U.S. Department of Health and Human Services Public Health Emergency Medical Countermeasures Enterprise’s implementation plan.
- At present, there is no FDA-approved treatment for Bolivian Hemorrhage Fever (BHF). This computational vaccine model against the nucleocapsid protein of the Machupo virus has the capacity to assist in this regard.
- In previous research, the vaccine against viral glycoprotein of Machupo virus is proposed, but there was no particular focus on the nucleocapsid protein of the Machupo virus, which is the main protein interacting with the IKBKE receptor of the host cell.
- The vaccine design in this study using the reverse vaccinology approach will help researchers in wet lab-based development of a vaccine against Machupo virus in treating Bolivian Hemorrhage Fever.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sarute, N.; Ross, S.R. New World Arenavirus Biology. Annu. Rev. Virol. 2017, 29, 141–158. [Google Scholar] [CrossRef]
- Silva-Ramos, C.R.; Faccini-Martínez, Á.A.; Calixto, O.J.; Hidalgo, M. Bolivian hemorrhagic fever: A narrative review. Travel Med. Infect. Dis. 2021, 40, 102001. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.; Grant, A.; Paessler, S. Epidemiology and pathogenesis of Bolivian hemorrhagic fever. Curr. Opin. Virol. 2014, 5, 82–90. [Google Scholar] [CrossRef] [Green Version]
- Maria, G.F.; Adamm, B.; Camille, M.W.; Vanessa, R. South American Hemorrhagic Fevers: A summary for clinicians. Int. J. Infect. Dis. 2021, 105, 505–515. [Google Scholar]
- Schwind, V. Chapter 142—Viral Hemorrhagic Fever Attack: Arenaviruses. In Ciottone’s Disaster Medicine, 2nd ed.; Ciottone, G.R., Ed.; Elsevier: Philadelphia, PA, USA, 2016; pp. 754–756. [Google Scholar]
- Papageorgiou, N.; Spiliopoulou, M.; Nguyen, T.-H.V.; Vaitsopoulou, A.; Laban, E.Y.; Alvarez, K.; Margiolaki, I.; Canard, B.; Ferron, F. Brothers in Arms: Structure, Assembly and Function of Arenaviridae Nucleoprotein. Viruses 2020, 12, 772. [Google Scholar] [CrossRef] [PubMed]
- Bell, T.M.; Shaia, C.I.; Bunton, T.E.; Robinson, C.G.; Wilkinson, E.R.; Hensley, L.E.; Cashman, K.A. Pathology of experimental Machupo virus infection, Chicava strain, in cynomolgus macaques (Macaca fascicularis) by intramuscular and aerosol exposure. Vet. Pathol. 2015, 52, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Kranzusch, P.J.; Schenk, A.D.; Rahmeh, A.A.; Radoshitzky, S.R.; Bavari, S.; Walz, T.; Whelan, S.P. Assembly of a functional Machupo virus polymerase complex. Proc. Natl. Acad. Sci. USA 2010, 107, 20069–20074. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.; Liu, Y.; Zhang, G.; Wang, S.; Guo, J.; Cao, J.; Jia, X.; Zhang, L.; Xiao, G.; Wang, W. Screening and Identification of Lassa Virus Entry Inhibitors from an FDA-Approved Drug Library. J. Virol. 2018, 31, e00954-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koma, T.; Patterson, M.; Huang, C.; Seregin, A.V.; Maharaj, P.D.; Miller, M.; Smith, J.N.; Walker, A.G.; Hallam, S.; Paessler, S. Machupo Virus Expressing GPC of the Candid#1 Vaccine Strain of Junin Virus Is Highly Attenuated and Immunogenic. J. Virol. 2015, 18, 1290–1297. [Google Scholar]
- Ortiz-Riaño, E.; Cheng, B.Y.; de la Torre, J.C.; Martínez-Sobrido, L. Self-association of lymphocytic choriomeningitis virus nucleoprotein is mediated by its N-terminal region and is not required for its anti-interferon function. J. Virol. 2012, 86, 3307–3317. [Google Scholar] [CrossRef] [Green Version]
- Šantak, M.; Matić, Z. The Role of Nucleoprotein in Immunity to Human Negative-Stranded RNA Viruses—Not Just Another Brick in the Viral Nucleocapsid. Viruses 2022, 14, 521. [Google Scholar] [CrossRef] [PubMed]
- Pandey, R.K.; Ali, M.; Ojha, R.; Bhatt, T.K.; Prajapati, V.K. Development of multi-epitope driven subunit vaccine in secretory and membrane protein of Plasmodium falciparum to convey protection against malaria infection. Vaccine 2018, 36, 4555–4565. [Google Scholar] [CrossRef]
- Soltan, M.A.; Elbassiouny, N.; Gamal, H.; Elkaeed, E.B.; Eid, R.A.; Eldeen, M.A.; Al-Karmalawy, A.A. In Silico Prediction of a Multitope Vaccine against Moraxella catarrhalis: Reverse Vaccinology and Immunoinformatics. Vaccines 2021, 9, 669. [Google Scholar] [CrossRef] [PubMed]
- Oro, B.; McKee, K.T. Toward a vaccine against Argentine hemorrhagic fever. Bull. Pan Am. Health Organ. 1991, 25, 118–126. [Google Scholar]
- Maiztegui, J.I.; McKee, K.T.; Oro, B.; Harrison, L.H.; Gibbsa, P.H.; Feuillade, M.R.; Enria, D.A.; Briggiler, A.M.; Levis, S.C.; Ambrosio, A.M.; et al. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J. Infect. Dis. 1998, 177, 277–283. [Google Scholar] [CrossRef] [Green Version]
- Pruitt, K.D.; Tatusova, T.; Brown, G.R.; Maglott, D.R. NCBI Reference Sequences (RefSeq): Current status, new features and genome annotation policy. Nucleic Acids Res. 2011, 40, D130–D135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gasteiger, E. ExPASy: The proteomics server for in-depth protein knowledge and analysis. Nucleic Acids Res. 2003, 31, 3784–3788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A server for prediction of protective antigens, tumor antigens and subunit vaccines. BMC Bioinform. 2007, 8, 4. [Google Scholar] [CrossRef] [Green Version]
- Dimitrov, I.; Flower, D.R.; Doytchinova, I. AllerTOP—A server for in silico prediction of allergens. BMC Bioinform. 2013, 14 (Suppl. 6), S4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsen, J.; Lund, O.; Nielsen, M. Improved method for predicting linear B-cell epitopes. Immunome Res. 2006, 2, 2. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, M.; Lundegaard, C.; Worning, P.; Lauemøller, S.L.; Lamberth, K.; Buus, S.; Brunak, S.; Lund, O. Reliable prediction of T-cell epitopes using neural networks with novel sequence representations. Protein Sci. 2003, 12, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.K.; Andreatta, M.; Marcatili, P.; Buus, S.; Greenbaum, J.A.; Yan, Z.; Sette, A.; Peters, B.; Nielsen, M. Improved methods for predicting peptide binding affinity to MHC class II molecules. Immunology 2018, 154, 394–406. [Google Scholar] [CrossRef]
- Bui, H.-H.; Sidney, J.; Dinh, K.; Southwood, S.; Newman, M.J.; Sette, A. Predicting population coverage of T-cell epitope-based diagnostics and vaccines. BMC Bioinform. 2006, 7, 153. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Xu, J. Raptorx: Exploiting structure information for protein alignment by statistical inference. Proteins Struct. Funct. Bioinform. 2011, 79, 161–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, Z.; Su, H.; Wang, W.; Ye, L.; Wei, H.; Peng, Z.; Anishchenko, I.; Baker, D.; Yang, J. The trRosetta server for fast and accurate protein structure prediction. Nat. Protoc. 2021, 16, 5634–5651. [Google Scholar] [CrossRef]
- Pundir, S.; Martin, M.J.; O’Donovan, C. UniProt Tools. Curr. Protoc. Bioinform. 2016, 53, 1.29.1–1.29.15. [Google Scholar] [CrossRef] [Green Version]
- Ko, J.; Park, H.; Heo, L.; Seok, C. GalaxyWEB server for protein structure prediction and refinement. Nucleic Acids Res. 2012, 40, W294–W297. [Google Scholar] [CrossRef] [PubMed]
- Lovell, S.C.; Davis, I.W.; Arendall, W.B.; de Bakker, P.I.W.; Word, J.M.; Prisant, M.G.; Richardson, J.S.; Richardson, D.C. Structure validation by Calpha geometry: Phi, psi and Cbeta deviation. Proteins 2003, 50, 437–450. [Google Scholar] [CrossRef]
- Desta, I.; Porter, K.; Xia, B.; Kozakov, D.; Vajda, S. Performance and Its Limits in Rigid Body Protein-Protein Docking. SSRN Electron. J. 2020, 28, 1071–1081.e3. [Google Scholar]
- López-Blanco, J.R.; Aliaga, J.I.; Quintana-Ortí, E.S.; Chacón, P. iMODS: Internal coordinates normal mode analysis server. Nucleic Acids Res. 2014, 42, W271–W276. [Google Scholar] [CrossRef]
- Snapgene. SnapGene|Software for Everyday Molecular Biology. SnapGene, 2022. Available online: https://www.snapgene.com/ (accessed on 2 August 2022).
- Castiglione, F.; Deb, D.; Srivastava, A.P.; Liò, P.; Liso, A. From Infection to Immunity: Understanding the Response to SARS-CoV2 Through In-Silico Modeling. Front. Immunol. 2021, 12, 646972. [Google Scholar] [CrossRef]
- Berrouet, C.; Dorilas, N.; Rejniak, K.A.; Tuncer, N. Comparison of drug inhibitory effects (IC50) in monolayer and spheroid cultures. Preprints. Bull. Math. Biol. 2020, 82, 68. [Google Scholar] [CrossRef]
- Banerjee, A.; Santra, D.; Maiti, S. Energetics and IC50 based epitope screening in SARS CoV-2 (COVID 19) spike protein by immunoinformatic analysis implicating for a suitable vaccine development. J. Transl. Med. 2020, 18, 281. [Google Scholar] [CrossRef]
- Chen, X.; Zaro, J.L.; Shen, W.-C. Fusion protein linkers: Property, design and functionality. Adv. Drug Deliv. Rev. 2013, 65, 1357–1369. [Google Scholar] [CrossRef]
- Yin, M.; Wang, X.; Lu, J. Advances in IKBKE as a potential target for cancer therapy. Cancer Med. 2019, 9, 247–258. [Google Scholar] [CrossRef]
- Findlater, A.; Bogoch, I.I. Human Mobility and the Global Spread of Infectious Diseases: A Focus on Air Travel. Trends Parasitol. 2018, 34, 772–783. [Google Scholar] [CrossRef]
- Murray, K.A.; Allen, T.; Loh, E.; Machalaba, C.; Daszak, P. Emerging Viral Zoonoses from Wildlife Associated with Animal-Based Food Systems: Risks and Opportunities. Food Saf. Risks Wildl. 2015, 31–57. [Google Scholar]
- Khatoon, N.; Pandey, R.K.; Ojha, R.; Aathmanathan, V.S.; Krishnan, M.; Prajapati, V.K. Exploratory algorithm to devise multi-epitope subunit vaccine by investigating Leishmania donovani membrane proteins. J. Biomol. Struct. Dyn. 2018, 37, 2381–2393. [Google Scholar] [CrossRef]
- Sharma, A.; Sanduja, P.; Anand, A.; Mahajan, P.; Guzman, C.A.; Yadav, P.; Awasthi, A.; Hanski, E.; Dua, M.; Johri, A.K. Advanced strategies for development of vaccines against human bacterial pathogens. World J. Microbiol. Biotechnol. 2021, 37, 67. [Google Scholar] [CrossRef]
- Sjöström, D.J.; Lundgren, A.; Garforth, S.J.; Bjelic, S. Tuning the binding interface between Machupo virus glycoprotein and human transferrin receptor. Proteins Struct. Funct. Genet. 2021, 89, 311–321. [Google Scholar] [CrossRef]
- Naveed, M.; Sheraz, M.; Amin, A.; Waseem, M.; Aziz, T.; Khan, A.A.; Ghani, M.; Shahzad, M.; Alruways, M.W.; Dablool, A.S.; et al. Designing a Novel Peptide-Based Multi-Epitope Vaccine to Evoke a Robust Immune Response against Pathogenic Multidrug-Resistant Providencia heimbachae. Vaccines 2022, 10, 1300. [Google Scholar] [CrossRef]
- Jackson, N.A.C.; Kester, K.E.; Casimiro, D.; Gurunathan, S.; DeRosa, F. The promise of mRNA vaccines: A biotech and industrial perspective. npj Vaccines 2020, 5, 11. [Google Scholar] [CrossRef] [Green Version]
- Pyle, J.D.; Whelan, S.P.J. RNA ligands activate the Machupo virus polymerase and guide promoter usage. Proc. Natl. Acad. Sci. USA 2019, 116, 10518–10524. [Google Scholar] [CrossRef] [Green Version]
- Clemens, E.; van de Sandt, C.; Wong, S.; Wakim, L.; Valkenburg, S. Harnessing the Power of T Cells: The Promising Hope for a Universal Influenza Vaccine. Vaccines 2018, 6, 18. [Google Scholar] [CrossRef] [Green Version]
- Yasmin, T.; Akter, S.; Debnath, M.; Ebihara, A.; Nakagawa, T.; Nabi, A.H.M.N. In silico proposition to predict cluster of B- and T-cell epitopes for the usefulness of vaccine design from invasive, virulent and membrane associated proteins of C. jejuni. Silico Pharmacol. 2016, 4, 5. [Google Scholar] [CrossRef]
- Parvizpour, S.; Pourseif, M.M.; Razmara, J.; Rafi, M.A.; Omidi, Y. Epitope-based vaccine design: A comprehensive overview of bioinformatics approaches. Drug Discov. Today 2020, 25, 1034–1042. [Google Scholar] [CrossRef]
- Heo, L.; Park, H.; Seok, C. GalaxyRefine: Protein structure refinement driven by side-chain repacking. Nucleic Acids Res. 2013, 41, W384–W388. [Google Scholar] [CrossRef] [Green Version]
- Ferron, F.; Weber, F.; de la Torre, J.C.; Reguera, J. Transcription, and replication mechanisms of Bunyaviridae and Arenaviridae L proteins. Virus Res. 2017, 234, 118–134. [Google Scholar] [CrossRef]




| No. | Start | End | Peptide | Length | Antigenicity Score |
|---|---|---|---|---|---|
| 1 | 129 | 134 | SQLQLT | 6 | 1.4796 |
| 2 | 220 | 227 | EHECLQIV | 8 | 1.3906 |
| 3 | 271 | 281 | SSLIKSTLQVK | 11 | 0.6508 |
| 4 | 434 | 444 | PGVLSYVIGLL | 11 | 0.6472 |
| 5 | 459 | 464 | RKLLDI | 6 | 0.9124 |
| No. | Peptide | Alleles | Length | Antigenicity Score |
|---|---|---|---|---|
| 1 | YNFSLSAAVK | HLA-B*15:01, HLA-A*23:01, HLA-A*24:02, HLA-B*08:01, HLA-A*02:06, HLA-A*02:01, HLA-B*58:01, HLA-A*02:03, HLA-B*57:01, HLA-A*32:01, HLA-A*03:01, HLA-A*30:02, HLA-E*01:01, HLA-B*53:01, HLA-A*31:01, HLA-B*35:01, HLA-A*11:0, HLA-A*01:01, HLA-B*44:02, HLA-A*68:02, HLA-A*33:01, HLA-C*14:02, HLA-A*68:01, HLA-B*51:01, HLA-B*40:01, HLA-B*58:02, HLA-B*44:03, HLA-C*07:02, HLA-C*04:01, HLA-C*12:03, HLA-C*07:01, HLA-C*06:02, HLA-C*15:02, HLA-C*05:01, HLA-C*03:03 | 10 | 1.1965 |
| 2 | TKKPQVGPR | HLA-A*02:06, HLA-C*08:02, HLA-C*04:01, HLA-A*02:01, HLA-C*15:02, HLA-B*40:01, HLA-A*23:01, HLA-B*35:01, HLA-A*68:02, HLA-A*01:01, HLA-B*15:01, HLA-B*51:01, HLA-A*02:03, HLA-C*05:01, HLA-B*58:01, HLA-B*53:01, HLA-A*30:01, HLA-B*44:02, HLA-B*58:02, HLA-B*57:01, HLA-A*26:01, HLA-B*07:02, HLA-A*24:02, HLA-E*01:01, HLA-A*33:01, HLA-A*30:02, HLA-A*31:01, HLA-B*44:03, HLA-A*11:01, HLA-A*03:01, HLA-A*32:01, HLA-A*68:01 | 10 | 1.6985 |
| 3 | VALLPLSLL | HLA-A*23:01, HLA-B*44:02, HLA-A*30:02, HLA-A*24:02, HLA-B*15:01, HLA-B*44:03, HLA-A*02:06, HLA-A*26:01, HLA-B*07:02, HLA-A*02:01, HLA-B*08:01, HLA-B*57:01, HLA-A*01:01, HLA-A*68:02, HLA-B*58:01, HLA-B*40:01, HLA-C*14:02, HLA-A*32:01, HLA-B*53:01, HLA-E*01:01, HLA-B*58:02, HLA-C*04:01, HLA-B*35:01, HLA-B*51:01, HLA-C*07:01, HLA-C*07:02, HLA-C*06:02, HLA-C*12:03, HLA-C*15:02, HLA-C*08:02, HLA-C*05:01, HLA-C*03:03 | 9 | 1.0977 |
| 4 | ALRKNKRGE | HLA-A*02:01, HLA-B*58:01, HLA-A*01:01, HLA-A*68:01, HLA-A*30:01, HLA-A*02:03, HLA-A*26:01, HLA-A*31:01, HLA-B*53:01, HLA-B*44:02, HLA-B*57:01, HLA-B*08:01, HLA-B*40:01, HLA-A*33:01, HLA-B*51:01, HLA-B*07:02 | 9 | 1.2132 |
| 5 | TIRVTPDNF | HLA-B*08:01, HLA-A*02:06, HLA-A*02:01, HLA-B*15:01, HLA-B*53:01, HLA-A*23:01, HLA-A*24:02, HLA-B*35:01, HLA-B*51:01, HLA-A*68:02, HLA-B*40:01, HLA-A*30:01, HLA-A*01:01, HLA-A*26:01, HLA-B*58:01, HLA-B*57:01, HLA-B*44:02, HLA-A*31:01, HLA-A*33:01, HLA-A*30:02, HLA-A*32:01, HLA-A*03:01 | 9 | 0.8575 |
| 6 | QALTSLGLL | HLA-A*02:03, HLA-A*24:02, HLA-A*30:01, HLA-B*58:01, HLA-B*08:01, HLA-B*53:01, HLA-A*32:01, HLA-A*02:01, HLA-B*35:01, HLA-A*23:01, HLA-B*44:02, HLA-B*57:01, HLA-A*30:02, HLA-A*01:01, HLA-B*07:02, HLA-A*03:01, HLA-A*11:01, HLA-A*31:01, HLA-B*40:01, HLA-A*33:01, HLA-B*44:03 | 9 | 0.8575 |
| 7 | LYTVKYPNL | HLA-B*08:01, HLA-A*02:03, HLA-B*44:03, HLA-B*44:02, HLA-B*40:01, HLA-A*30:01, HLA-A*02:01, HLA-B*57:01, HLA-B*58:01, HLA-B*07:02, HLA-B*51:01, HLA-A*31:01 | 9 | 0.7742 |
| 8 | LDIHGRKDLK | HLA-A*33:01, HLA-B*40:01, HLA-B*07:02, HLA-A*01:01, HLA-A*24:02, HLA-A*30:02, HLA-A*30:01, HLA-B*44:02, HLA-A*68:01, HLA-B*57:01, HLA-B*51:01, HLA-A*11:01, HLA-A*32:01, HLA-B*44:03 | 10 | 1.0902 |
| No. | Peptide | Alleles | Length | Antigenicity Score |
|---|---|---|---|---|
| 1 | FSLSAAVKAGASIL | HLA-DPA1*02:01/DPB1*14:01, HLA-DQA1*01:02/DQB1*06:02, HLA-DQA1*05:01/DQB1*03:01, HLA-DRB1*01:01, HLA-DRB1*04:01, HLA-DRB1*04:05, HLA-DRB1*07:01, HLA-DRB1*08:02, HLA-DRB1*09:01, HLA-DRB1*11:01, HLA-DRB1*12:01, HLA-DRB1*13:02, HLA-DRB1*15:01, HLA-DRB3*01:01, HLA-DRB3*02:02, HLA-DRB5*01:01 | 14 | 0.8104 |
| 2 | INISGYNFSLSAAV | HLA-DPA1*01:03/DPB1*02:01, HLA-DPA1*02:01/DPB1*01:01, HLA-DPA1*02:01/DPB1*05:01, HLA-DPA1*03:01/DPB1*04:02, HLA-DQA1*01:01/DQB1*05:01, HLA-DQA1*05:01/DQB1*03:01, HLA-DRB1*01:01 | 14 | 0.6191 |
| 3 | LSYVIGLLPQDMVI | HLA-DPA1*01:03/DPB1*06:01, HLA-DPA1*02:01/DPB1*01:01, HLA-DQA1*04:01/DQB1*04:02, HLA-DPA1*02:01/DPB1*05:01, HLA-DPA1*01:03/DPB1*06:01, HLA-DQA1*04:01/DQB1*04:02, HLA-DRB1*04:05, HLA-DRB4*01:01, HLA-DRB5*01:01, HLA-DRB1*10:01, HLA-DRB1*11:01, HLA-DRB1*04:01, HLA-DQA1*03:01/DQB1*03:01 | 14 | 0.7864 |
| 4 | SFRWTQSLRRGLS | HLA-DQA1*02:01/DQB1*03:03, HLA-DQA1*02:01/DQB1*03:01, HLA-DQA1*05:01/DQB1*03:02, HLA-DQA1*05:01/DQB1*03:01, HLA-DQA1*02:01/DQB1*04:02, HLA-DQA1*04:01/DQB1*04:02, HLA-DQA1*05:01/DQB1*04:02, HLA-DQA1*03:01/DQB1*03:02 | 14 | 0.5757 |
| 5 | VLSYVIGLLPQDMVI | HLA-DPA1*02:01/DPB1*05:01, HLA-DRB1*03:01, HLA-DRB1*04:01, HLA-DRB1*08:02, HLA-DRB1*11:01 | 14 | 0.5388 |
| 6 | ILKTLGFQQ | HLA-DRB1*11:01, HLA-DRB1*08:02, HLA-DPA1*02:01/DPB1*05:01, HLA-DRB5*01:01, HLA-DPA1*03:01/DPB1*04:02, HLA-DPA1*02:01/DPB1*01:01, HLA-DRB4*01:01, HLA-DPA1*01:03/DPB1*02:01, HLA-DRB1*04:05, HLA-DRB1*04:01, HLA-DRB1*15:01, HLA-DRB1*07:01 | 9 | 0.1852 |
| 7 | QFGSMPALT | HLA-DRB1*10:01, HLA-DRB1*08:01, HLA-DRB1*15:01, HLA-DRB1*04:01, HLA-DRB1*08:01, HLA-DRB1*07:01, HLA-DQA1*01:02/DQB1*05:01, HLA-DRB1*16:02, HLA-DRB1*04:05, HLA-DRB1*08:02, HLA-DRB1*12:01, HLA-DQA1*02:01/DQB1*03:01, HLA-DQA1*02:01/DQB1*03:03, HLA-DPA1*01:03/DPB1*04:02, HLA-DQA1*01:04/DQB1*05:03 | 9 | 0.8106 |
| 8 | LSLLFLPKAAFAL | HLA-DRB1*03:01, HLA-DRB3*01:01, HLA-DRB1*04:01, HLA-DPA1*03:01/DPB1*04:02, HLA-DPA1*02:01/DPB1*01:01, HLA-DRB5*01:01, HLA-DRB4*01:01, HLA-DRB1*13:02 | 13 | 0.7809 |
| 9 | DGWPYIGSRSQILG | HLA-DPA1*02:01/DPB1*01:01, HLA-DPA1*02:01/DPB1*05:01, HLA-DPA1*03:01/DPB1*04:02, HLA-DQA1*05:01/DQB1*03:01 | 14 | 0.7941 |
| 10 | YIGSRSQIL | HLA-DPA1*02:01/DPB1*05:01, HLA-DRB1*08:02, HLA-DRB5*01:01, HLA-DRB4*01:01, HLA-DPA1*03:01/DPB1*04:02, HLA-DPA1*02:01/DPB1*01:01, HLA-DRB1*03:01, HLA-DPA1*01:03/DPB1*02:01, HLA-DRB1*12:01, HLA-DPA1*01:03/DPB1*04:01, HLA-DRB1*04:05 | 9 | 0.6841 |
| 11 | EPVALLPLSLLFL | HLA-DPA1*01:03/DPB1*04:01, HLA-DPA1*01:03/DPB1*02:01, HLA-DRB4*01:01, HLA-DRB1*04:05, HLA-DRB1*12:01, HLA-DRB1*15:01, HLA-DRB1*04:01, HLA-DRB1*07:01, HLA-DRB1*01:01, HLA-DRB1*13:02, HLA-DRB1*09:01 | 14 | 0.9988 |
| 12 | NNQFGSMPALTIA | HLA-DPA1*03:01/DPB1*04:02, HLA-DQA1*01:02/DQB1*06:02, HLA-DQA1*03:01/DQB1*03:02, HLA-DQA1*04:01/DQB1*04:02, HLA-DQA1*05:01/DQB1*03:01, HLA-DRB1*01:01, HLA-DRB1*03:01 | 14 | 0.7757 |
| 13 | HGILMQDIE | HLA-DPA1*02:01/DPB1*01:01, HLA-DRB4*01:01, HLA-DPA1*01:03/DPB1*02:01, HLA-DQA1*03:01/DQB1*03:02, HLA-DRB1*04:05, HLA-DRB1*04:01, HLA-DRB1*15:01, HLA-DRB1*07:01 | 9 | 0.4930 |
| 14 | LVDVKLTSDQARLY | HLA-DPA1*02:01/DPB1*14:01, HLA-DQA1*01:02/DQB1*06:02, HLA-DQA1*05:01/DQB1*03:01, HLA-DRB1*01:01, HLA-DRB1*03:01, HLA-DRB1*04:01, HLA-DRB1*07:01, HLA-DRB1*08:02, HLA-DRB1*09:01 | 14 | 0.5489 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naveed, M.; Makhdoom, S.I.; Ali, U.; Jabeen, K.; Aziz, T.; Khan, A.A.; Jamil, S.; Shahzad, M.; Alharbi, M.; Alshammari, A. Immunoinformatics Approach to Design Multi-Epitope-Based Vaccine against Machupo Virus Taking Viral Nucleocapsid as a Potential Candidate. Vaccines 2022, 10, 1732. https://doi.org/10.3390/vaccines10101732
Naveed M, Makhdoom SI, Ali U, Jabeen K, Aziz T, Khan AA, Jamil S, Shahzad M, Alharbi M, Alshammari A. Immunoinformatics Approach to Design Multi-Epitope-Based Vaccine against Machupo Virus Taking Viral Nucleocapsid as a Potential Candidate. Vaccines. 2022; 10(10):1732. https://doi.org/10.3390/vaccines10101732
Chicago/Turabian StyleNaveed, Muhammad, Syeda Izma Makhdoom, Urooj Ali, Khizra Jabeen, Tariq Aziz, Ayaz Ali Khan, Sumbal Jamil, Muhammad Shahzad, Metab Alharbi, and Abdulrahman Alshammari. 2022. "Immunoinformatics Approach to Design Multi-Epitope-Based Vaccine against Machupo Virus Taking Viral Nucleocapsid as a Potential Candidate" Vaccines 10, no. 10: 1732. https://doi.org/10.3390/vaccines10101732
APA StyleNaveed, M., Makhdoom, S. I., Ali, U., Jabeen, K., Aziz, T., Khan, A. A., Jamil, S., Shahzad, M., Alharbi, M., & Alshammari, A. (2022). Immunoinformatics Approach to Design Multi-Epitope-Based Vaccine against Machupo Virus Taking Viral Nucleocapsid as a Potential Candidate. Vaccines, 10(10), 1732. https://doi.org/10.3390/vaccines10101732






