Effectiveness of COVID-19 Vaccines against Delta (B.1.617.2) Variant: A Systematic Review and Meta-Analysis of Clinical Studies
Abstract
:1. Introduction
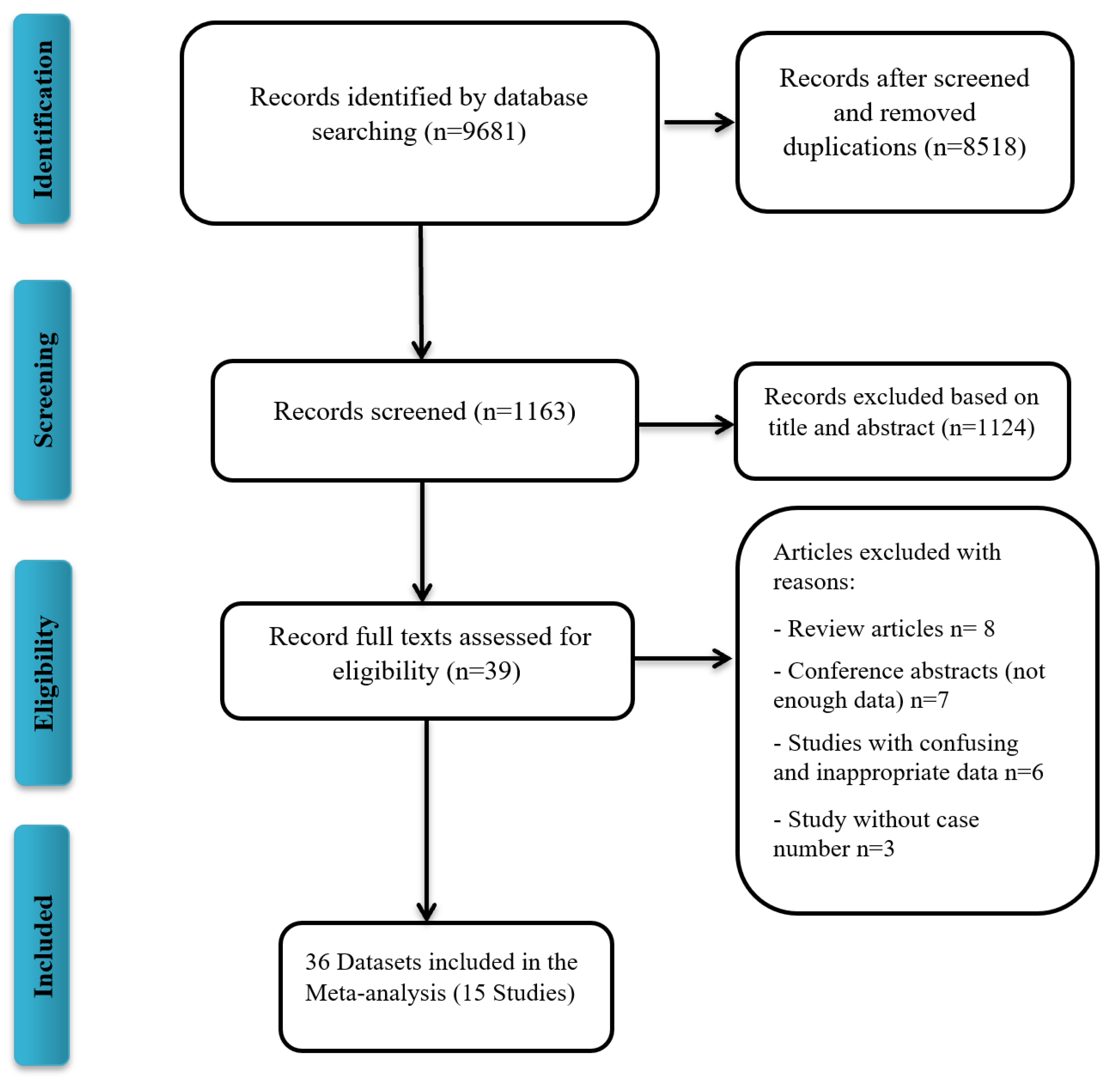
2. Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Eligibility and Inclusion Criteria
2.4. Exclusion Criteria
2.5. Data Extraction
2.6. Quality Assessment
2.7. Analysis
3. Result
3.1. Characteristics of Included Studies
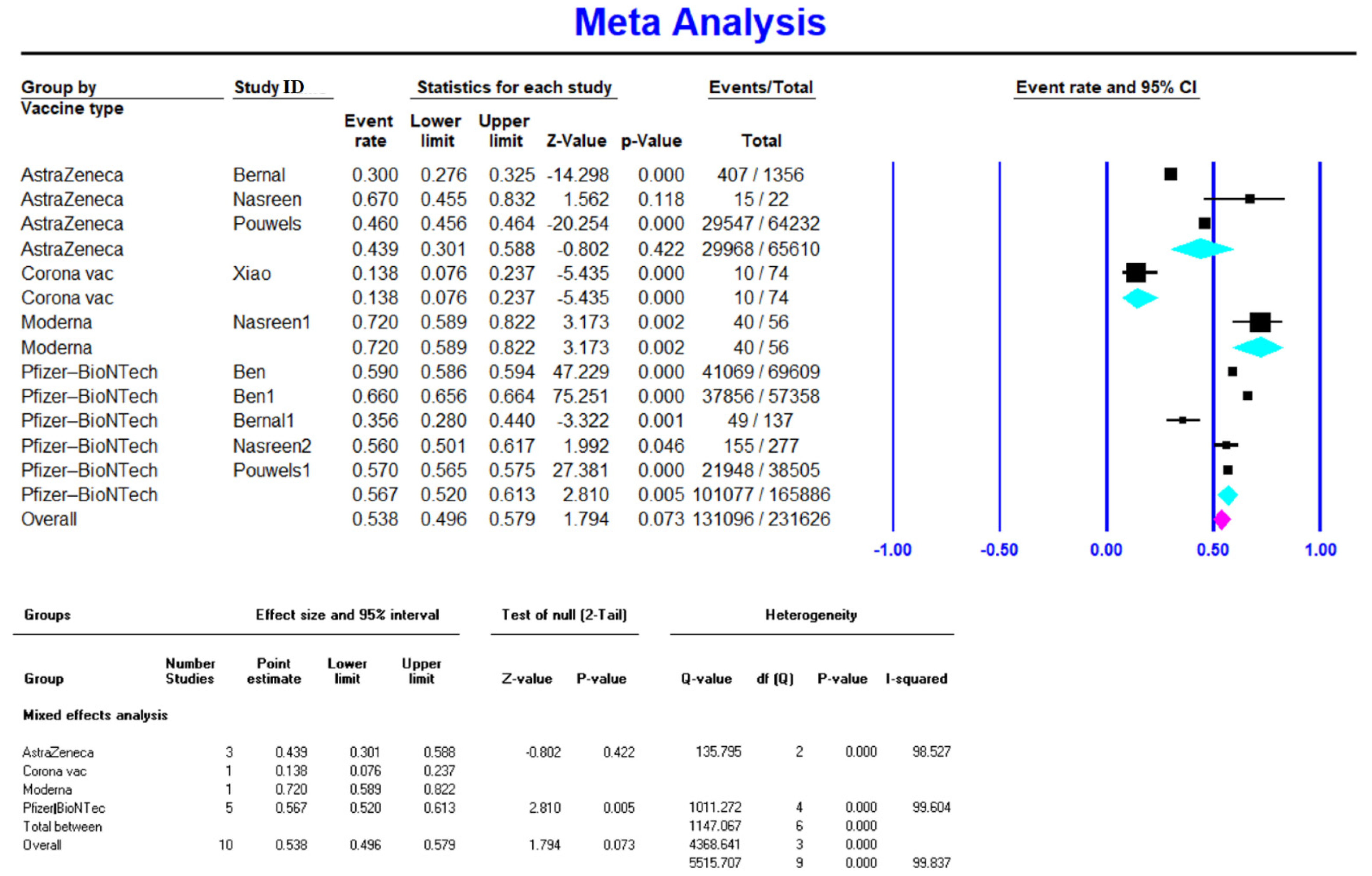
3.2. Efficacy of Different COVID-19 Vaccines against Delta Variant Infection
3.2.1. Pfizer-BioNTech Efficacy against COVID-19 Delta Variant Infection
3.2.2. Moderna Efficacy against COVID-19 Delta Variant Infection
3.2.3. AstraZeneca Efficacy against COVID-19 Delta Variant Infection
3.2.4. CoronaVac Efficacy against COVID-19 Delta Variant Infection
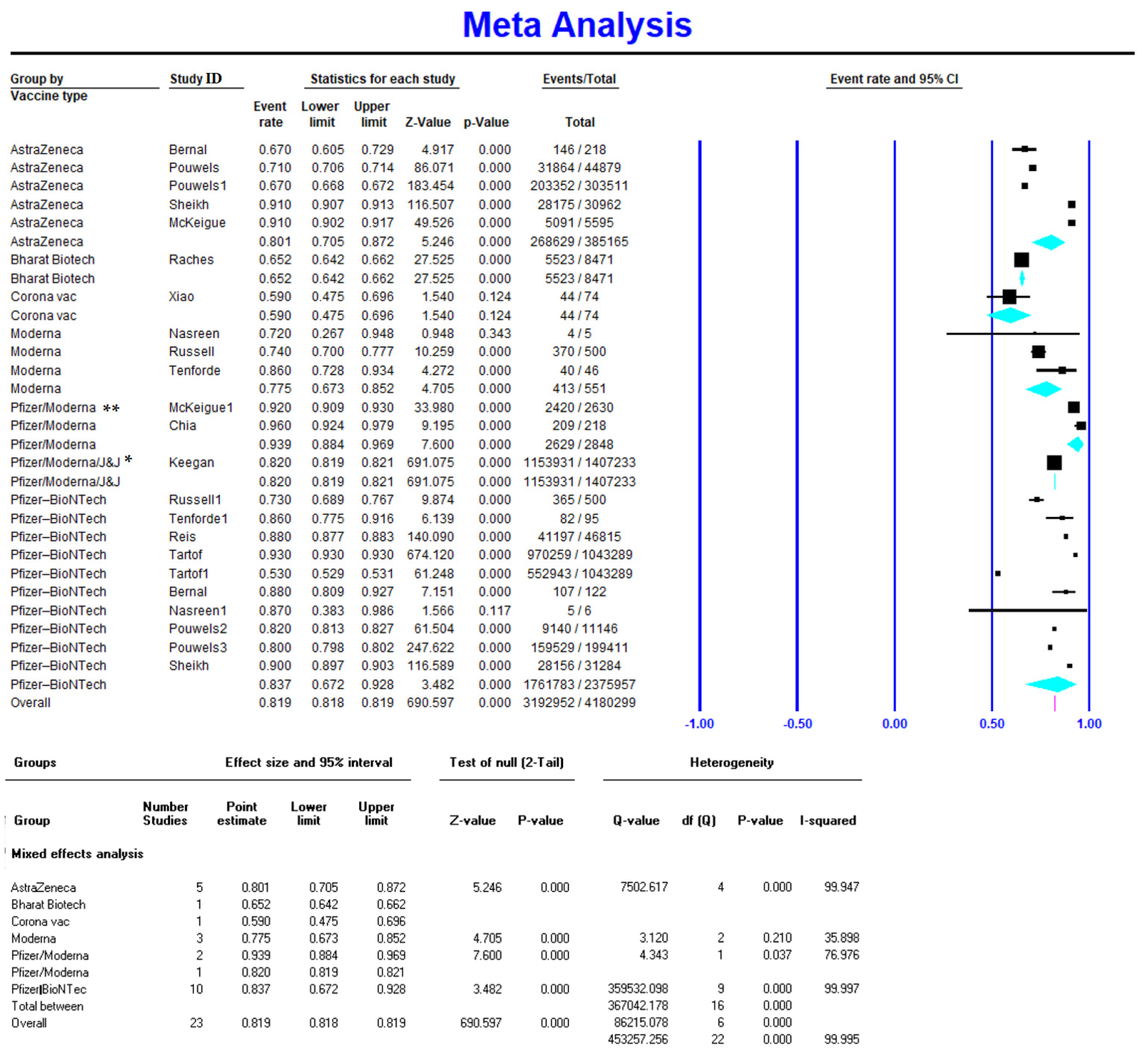
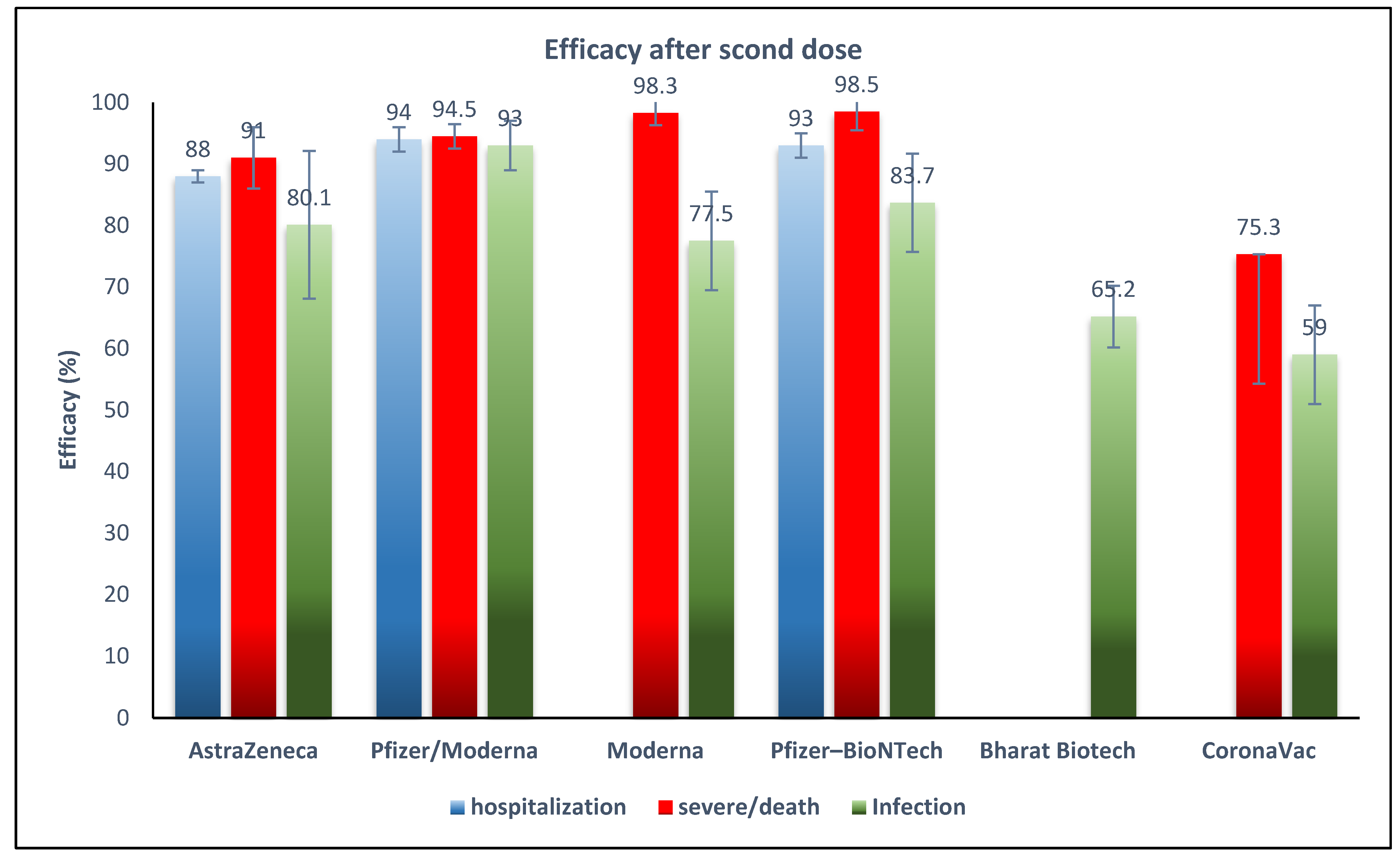
3.3. Efficacy of COVID-19 Vaccines against Delta Variant for Preventing Severe Infection or Death
3.4. Efficacy of COVID-19 Vaccines against Delta Variant Hospitalization
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Outbreak.info. Available online: https://outbreak.info/ (accessed on 14 November 2021).
- World Health Organization. COVID-19 Vaccines WHO EUL Issued. Available online: https://extranet.who.int/pqweb/vaccines/vaccinescovid-19-vaccine-eul-issued (accessed on 14 November 2021).
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Bijker, E. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Dagan, N.; Barda, N.; Kepten, E.; Miron, O.; Perchik, S.; Katz, M.A. BNT162b2 mRNA COVID-19 caccine in a nationwide mass vaccination setting. N. Engl. J. Med. 2021, 384, 1412–1423. [Google Scholar] [CrossRef]
- Hall, V.J.; Foulkes, S.; Saei, A.; Andrews, N.; Oguti, B.; Charlett, A.; Wellington, E.; Stowe, J.; Gillson, N.; Cowley, A.; et al. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): A prospective, multicentre, cohort study. Lancet 2021, 397, 1725–1735. [Google Scholar] [CrossRef]
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Robertson, C.; Stowe, J.; Tessier, E. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on COVID-19 related symptoms, hospital admissions, and mortality in older adults in England: Test negative case-control study. BMJ 2021, 373, n1088. [Google Scholar] [CrossRef]
- Shrotri, M.; Krutikov, M.; Palmer, T.; Giddings, R.; Azmi, B.; Subbarao, S. Vaccine effectiveness of the first dose of ChAdOx1 nCoV-19 and BNT162b2 against SARS-CoV-2 infection in residents of long-term care facilities in England (VIVALDI): A prospective cohort study. Lancet Infect. Dis. 2021, 21, 1529–1538. [Google Scholar] [CrossRef]
- Updates on COVID-19 Variants of Concern. Available online: https://nccid.ca/covid-19-variants/ (accessed on 10 December 2021).
- Konings, F.; Perkins, M.D.; Kuhn, J.H.; Pallen, M.J.; Alm, E.J.; Archer, B.N. SARS-CoV-2 variants of interest and concern naming scheme conducive for global discourse. Nat. Microbiol. 2021, 6, 821–823. [Google Scholar] [CrossRef] [PubMed]
- Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html (accessed on 26 November 2021).
- Dai, L.; Gao, G.F. Viral targets for vaccines against COVID-19. Nat. Rev. Immunol. 2021, 21, 73–82. [Google Scholar] [CrossRef]
- Letko, M.; Marzi, A.; Munster, V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat. Microbiol. 2020, 5, 562–569. [Google Scholar] [CrossRef] [Green Version]
- Elena, S.F.; Sanjuán, R. Adaptive value of high mutation rates of RNA viruses: Separating causes from consequences. J. Virol. 2005, 79, 11555–11558. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Wu, J.; Nie, J.; Zhang, L.; Hao, H.; Liu, S. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell 2020, 182, 1284–1294. [Google Scholar] [CrossRef]
- Jia, Z.; Gong, W. Will mutations in the spike protein of SARS-CoV-2 lead to the failure of COVID-19 vaccines? J. Korean Med. Sci. 2021, 36, e124. [Google Scholar] [CrossRef]
- Chen, X.; Wang, W.; Chen, X.; Wu, Q.; Sun, R.; Ge, S. Prediction of long-term kinetics of vaccine-elicited neutralizing antibody and time-varying vaccine-specific efficacy against the SARS-CoV-2 Delta variant by clinical endpoint. medRxiv 2021. [Google Scholar] [CrossRef]
- Public Health England. SARS-CoV-2 Variants of Concern and Variants under Investigation in England. Technical Briefing 11. SARS-CoV-2 Variants of Concern and Variants under Investigation in England. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/986380/Variants_of_Concern_VOC_Technical_Briefing_11_England.pdf (accessed on 13 May 2021).
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Gallagher, E.; Simmons, R.; Thelwall, S. Effectiveness of COVID-19 vaccines against the B.1.617.2 (Delta) variant. N. Engl. J. Med. 2021, 385, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Viera, A.J.; Garrett, J.M. Understanding interobserver agreement: The kappa statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar]
- The Joanna Briggs Institute. The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews. Checklist for Qualitative Research; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Perdices, M. Null hypothesis significance testing, p-values, effects sizes and confidence intervals. Brain Impair. 2018, 19, 70–80. [Google Scholar] [CrossRef]
- Nasreen, S.; He, S.; Chung, H.; Brown, K.A.; Gubbay, J.B.; Buchan, S.A. Effectiveness of COVID-19 vaccines against variants of concern in Ontario, Canada. medRxiv 2021. [Google Scholar] [CrossRef]
- Pouwels, K.B.; Pritchard, E.; Matthews, P.C.; Stoesser, N.; Eyre, D.W.; Vihta, K.-D. Effect of Delta variant on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. Nat. Med. 2021, 27, 2127–2135. [Google Scholar] [PubMed]
- Li, X.-N.; Huang, Y.; Wang, W.; Jing, Q.-L.; Zhang, C.-H.; Qin, P.-Z. Effectiveness of inactivated SARS-CoV-2 vaccines against the Delta variant infection in Guangzhou: A test-negative case-control real-world study. Emerg. Microbes Infect. 2021, 10, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Reis, B.Y.; Barda, N.; Leshchinsky, M.; Kepten, E.; Hernán, M.A.; Lipsitch, M. Effectiveness of BNT162b2 vaccine against Delta variant in adolescents. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef]
- Sheikh, A.; McMenamin, J.; Taylor, B.; Robertson, C. SARS-CoV-2 Delta VOC in Scotland: Demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021, 397, 2461–2462. [Google Scholar] [CrossRef]
- McKeigue, P.M.; McAllister, D.; Hutchinson, S.J.; Robertson, C.; Stockton, D.; Colhoun, H.M. Efficacy of vaccination against severe COVID-19 in relation to Delta variant and time since second dose: The REACT-SCOT case-control study. medRxiv 2021. [Google Scholar] [CrossRef]
- Ella, R.; Reddy, S.; Blackwelder, W.; Potdar, V.; Yadav, P.; Sarangi, V. Efficacy, safety, and lot to lot immunogenicity of an inactivated SARS-CoV-2 vaccine (BBV152): A double-blind, randomised, controlled phase 3 trial. medRxiv 2021. [Google Scholar] [CrossRef]
- Barlow, R.S.; Larson, L.; Jian, K. Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection during a Delta variant epidemic surge in Multnomah County, Oregon, July 2021. medRxiv 2021. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Self, W.H.; Naioti, E.A.; Ginde, A.A.; Douin, D.J.; Olson, S.M. Sustained effectiveness of Pfizer-BioNTech and Moderna vaccines against COVID-19 associated hospitalizations among adults—United States, March–July 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1156. [Google Scholar] [CrossRef]
- Chia, P.Y.; Ong, S.W.X.; Chiew, C.J.; Ang, L.W.; Chavatte, J.-M.; Mak, T.-M. Virological and serological kinetics of SARS-CoV-2 Delta variant vaccine-breakthrough infections: A multi-center cohort study. medRxiv 2021. [Google Scholar] [CrossRef] [PubMed]
- Keegan, L.; Truelove, S.A.; Lessler, J. Progress of the Delta variant and erosion of vaccine effectiveness, a warning from Utah. medRxiv 2021. [Google Scholar] [CrossRef]
- Tartof, S.Y.; Slezak, J.M.; Fischer, H.; Hong, V.; Ackerson, B.K.; Ranasinghe, O.N. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 2021, 398, 1407–1416. [Google Scholar] [CrossRef]
- Shah, S.M.; Alsaab, H.O.; Rawas-Qalaji, M.M.; Uddin, M.N. A review on current COVID-19 vaccines and evaluation of particulate vaccine delivery systems. Vaccines 2021, 9, 1086. [Google Scholar] [CrossRef]
- Milken Institute. COVID-19 Treatment and Vaccination Trackers. 2021. Available online: https://covid-19tracker.milkeninstitute.org/#vaccines_intro (accessed on 14 December 2021).
- Liu, Q.; Qin, C.; Liu, M.; Liu, J. Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: A systematic review and meta-analysis. Infect. Dis. Poverty 2021, 10, 1–15. [Google Scholar]
- Puranik, A.; Lenehan, P.J.; Silvert, E.; Niesen, M.J.; Corchado-Garcia, J.; O’Horo, J.C. Comparison of two highly-effective mRNA vaccines for COVID-19 during periods of Alpha and Delta variant prevalence. medRxiv 2021. [Google Scholar] [CrossRef]
- Nanduri, S.; Pilishvili, T.; Derado, G.; Soe, M.M.; Dollard, P.; Wu, H. Effectiveness of Pfizer-BioNTech and Moderna vaccines in preventing SARS-CoV-2 infection among nursing home residents before and during widespread circulation of the SARS-CoV-2 B. 1.617. 2 (Delta) variant—National Healthcare Safety Network, March 1–August 1, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1163. [Google Scholar]
- Rosenberg, E.S.; Holtgrave, D.R.; Dorabawila, V.; Conroy, M.; Greene, D.; Lutterloh, E. New COVID-19 cases and hospitalizations among adults, by vaccination status—New York, May 3–July 25, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1306. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.; Hasan, M.R.; Chemaitelly, H.; Yassine, H.M.; Benslimane, F.; Al Khatib, H.A. BNT162b2 and mRNA-1273 COVID-19 vaccine effectiveness against the Delta (B. 1.617. 2) variant in Qatar. medRxiv 2021. [Google Scholar] [CrossRef]
- Herlihy, R.; Bamberg, W.; Burakoff, A.; Alden, N.; Severson, R.; Bush, E.; Rapid increase in circulation of the SARS-CoV-2, B. 1.617. 2 (Delta) variant—Mesa County, Colorado, April–June 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1084. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Garcia-Knight, M.A.; Khalid, M.M.; Servellita, V.; Wang, C.; Morris, M.K. Transmission, infectivity, and antibody neutralization of an emerging SARS-CoV-2 variant in California carrying a L452R spike protein mutation. medRxiv 2021. [Google Scholar] [CrossRef]
- Adam, D. What Scientists Know about New, Fast-Spreading Coronavirus Variants. 2021. Available online: https://www.nature.com/articles/d41586-021-01390-4 (accessed on 14 December 2021).
- Harder, T.; Külper-Schiek, W.; Reda, S.; Treskova-Schwarzbach, M.; Koch, J.; Vygen-Bonnet, S. Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B. 1.617. 2) variant: Second interim results of a living systematic review and meta-analysis, 1 January to 25 August 2021. Eurosurveillance 2021, 26, 2100920. [Google Scholar]
- Zeng, B.; Gao, L.; Zhou, Q.; Yu, K.; Sun, F. Effectiveness of COVID-19 vaccines against SARS-CoV-2 variants of concern: A systematic review and meta-analysis. medRxiv 2021. [Google Scholar] [CrossRef]
- World Health Organization. WHO Target Product Profiles for COVID-19 Vaccines. Available online: https://www.who.int/publications/m/item/who-target-product-profiles-for-covid-19-vaccines (accessed on 14 December 2021).
- Pormohammad, A.; Zarei, M.; Ghorbani, S.; Mohammadi, M.; Razizadeh, M.H.; Turner, D.L. Efficacy and safety of COVID-19 vaccines: A systematic review and meta-analysis of randomized clinical trials. Vaccines 2021, 9, 467. [Google Scholar] [CrossRef]
- Zimmermann, P.; Curtis, N. Factors that influence the immune response to vaccination. Clin. Microbiol. Rev. 2019, 32, e00084-18. [Google Scholar] [CrossRef] [Green Version]
- Moustsen-Helms, I.R.; Emborg, H.-D.; Nielsen, J.; Nielsen, K.F.; Krause, T.G.; Molbak, K. Vaccine effectiveness after 1st and 2nd dose of the BNT162b2 mRNA Covid-19 vaccine in long-term care facility residents and healthcare workers—A Danish cohort study. medRxiv 2021. [Google Scholar] [CrossRef]
- Bartsch, S.M.; O’Shea, K.J.; Ferguson, M.C.; Bottazzi, M.E.; Wedlock, P.T.; Strych, U. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am. J. Prev. Med. 2020, 59, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Rocklöv, J. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J. Travel Med. 2021, 28. [Google Scholar] [CrossRef] [PubMed]
- Ferré, V.M.; Peiffer-Smadja, N.; Visseaux, B.; Descamps, D.; Ghosn, J.; Charpentier, C. Omicron SARS-CoV-2 variant: What we know and what we don’t. Anaesth Crit Care Pain Med. 2021, 41, 100998. [Google Scholar] [CrossRef] [PubMed]
| Study ID | Country | Name | Company | Study Type | Vaccine Type | Dose | Day * | Efficacy Against (%) | Ref | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Infection | Hospitalization | Severe/Death | |||||||||
| Bernal et al. | England | ChAdOx1 nCoV-19 | AstraZeneca | case– control | Adeno vector | 1 | 21 | 30.00 | NA | NA | [25] |
| Nasreen et al. | Canada | ChAdOx1 nCoV-19 | AstraZeneca | case– control | Adeno vector | 1 | 14 | 67.00 | NA | NA | [25] |
| Pouwels et al. | England | ChAdOx1 nCoV-19 | AstraZeneca | case– control | Adeno vector | 1 | 21 | 46.00 | NA | NA | [26] |
| Xiao-Ning Li | China | CoronaVac | Sinovac Biotech | case– control | Inactivated | 1 | 14 | 13.80 | NA | NA | [27] |
| Nasreen et al. | Canada | mRNA-1273 | Moderna | case– control | mRNA | 1 | 14 | 72.00 | NA | NA | [25] |
| Ben Y. Reis | NA | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 1 | 14–20 | 59.00 | NA | NA | [28] |
| Ben Y. Reis | NA | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 1 | 21–27 | 66.00 | NA | NA | [28] |
| Bernal et al. | England | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 1 | 21–56 | 35.60 | NA | NA | [25] |
| Nasreen et al. | Canada | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 1 | 14 | 56.00 | NA | NA | [25] |
| Pouwels et al. | England | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 1 | 21 | 57.00 | NA | NA | [26] |
| Bernal et al. | England | ChAdOx1 nCoV-19 | AstraZeneca | case– control | Adeno vector | 2 | 14 | 67 | NA | NA | [25] |
| Pouwels et al. | England | AdOx1 nCoV-19 | AstraZeneca | case– control | Adeno vector | 2 | 14 | 71 | NA | NA | [26] |
| Pouwels et al. | England | ChAdOx1 nCoV-19 | AstraZeneca | case– control | Adeno vector | 2 | >14 | 67 | NA | NA | [26] |
| Sheikh et al. | Scotland | AdOx1 nCoV-19 | AstraZeneca | cohort | Adeno vector | 2 | >14 | 91 | NA | 91 | [29] |
| Paul M McKeigue | Scotland | AdOx1 nCoV-19 | AstraZeneca | case– control | Live | 2 | >14 | 91 | 88 | NA | [30] |
| Raches Ella | India | BBV152 | Bharat Biotech | clinical trial III | Inactivated | 2 | 14 | 65.2 | NA | NA | [31] |
| xiao-Ning Li | China | CoronaVac | Sinovac Biotech | case– control | Inactivated | 2 | 14 | 59 | NA | NA | [27] |
| Nasreen et al. | Canada | mRNA-1273 | Moderna | case– control | mRNA | 2 | 14 | 72 | NA | NA | [25] |
| Russell S | NA | mRNA-1273 | Moderna | case– control | mRNA | 2 | 28 | 74 | NA | NA | [32] |
| Tenforde | NA | mRNA-1273 | Moderna | case– control | mRNA | 2 | 91–168 | 86 | NA | NA | [33] |
| Paul M McKeigue | Scotland | BNT162b2/mRNA-1273 | Pfizer/Moderna ** | case– control | mRNA | 2 | >14 | 92 | 91 | NA | [30] |
| Po Ying Chia | Singapore | BNT162b2/mRNA-1273 | Pfizer/ Moderna * | cohort | mRNA | 2 | >14 | 96 | NA | NA | [34] |
| Lindsay T. Keegan | USA | BNT162b2/mRNA-1273/Ad26.COV2.S | Pfizer/ Moderna/ J&J *** | mRNA/ adeno vector | 2 | >14 | 82 | NA | NA | [35] | |
| Russell S | NA | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | 28 | 73 | NA | NA | [32] |
| Tenforde | NA | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | 14–84 | 86 | NA | NA | [33] |
| Ben Y. Reis | NA | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | 7–21 | 88 | NA | NA | [28] |
| Sara Y. Tartof | USA | BNT162b2 | Pfizer- BioNTech | cohort | mRNA | 2 | 7 | 93 | 93 | NA | [36] |
| Sara Y. Tartof | USA | BNT162b2 | Pfizer- BioNTech | cohort | mRNA | 2 | 120 | 53 | NA | NA | [36] |
| Bernal et al. | England | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | 14 | 88 | NA | NA | [25] |
| Nasreen et al. | Canada | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | 7 | 87 | NA | NA | [25] |
| Pouwels et al. | England | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | 0–13 | 82 | NA | NA | [26] |
| Pouwels et al. | England | BNT162b2 | Pfizer- BioNTech | case– control | mRNA | 2 | >14 | 80 | NA | NA | [26] |
| Sheikh et al. | Scotland | BNT162b2 | Pfizer- BioNTech | cohort | mRNA | 2 | >14 | 90.00 | NA | 90.00 | [29] |
| Xinhua Chen | NA | mRNA-1273 | Moderna | cohort | mRNA | 3 | 14–30 | 97.00 | NA | 98.30 | [18] |
| Xinhua Chen | NA | BNT162b2 | Pfizer- BioNTech | cohort | mRNA | 3 | 14–30 | 97.20 | NA | 98.90 | [18] |
| Xinhua Chen | NA | CoronaVac | Sinovac Biotech | cohort | Inactivated | 3 | 60 | 63.80 | NA | 75.30 | [18] |
| Dose | Group | Number of Studies | Vaccine Effectiveness | 95% Interval | Test of Null (2-Tailed) | Heterogeneity | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | Z-Value | p-Value | Q-Value | df (Q) | p-Value | I-Squared | ||||
| After First Dose | AstraZeneca | 3 | 0.439 | 0.301 | 0.588 | −0.802 | 0.422 | 135.8 | 2.0 | <0.001 | 98.5 |
| CoronaVac | 1 | 0.138 | 0.076 | 0.237 | |||||||
| Moderna | 1 | 0.720 | 0.589 | 0.822 | |||||||
| Pfizer-BioNTech | 5 | 0.567 | 0.520 | 0.613 | 2.810 | 0.005 | 1011.3 | 4.0 | <0.001 | 99.6 | |
| Overall | 10 | 0.538 | 0.496 | 0.579 | 1.794 | 0.073 | 5515.7 | 9.0 | <0.001 | 99.8 | |
| After Second Dose | Pfizer/Moderna * | 2 | 0.939 | 0.884 | 0.969 | 7.6 | <0.001 | 4.3 | 1.0 | <0.001 | 77.0 |
| Pfizer-BioNTech | 10 | 0.837 | 0.672 | 0.928 | 3.5 | <0.001 | 359,532.1 | 9.0 | <0.001 | 100.0 | |
| Pfizer/Moderna/ J&J ** | 1 | 0.820 | 0.819 | 0.821 | |||||||
| AstraZeneca | 5 | 0.801 | 0.705 | 0.872 | 5.2 | <0.001 | 7502.6 | 4.0 | <0.001 | 99.9 | |
| Moderna | 3 | 0.775 | 0.673 | 0.852 | 4.7 | <0.001 | 3.1 | 2.0 | 0.2 | 35.9 | |
| Bharat Biotech | 1 | 0.652 | 0.642 | 0.662 | |||||||
| CoronaVac | 1 | 0.590 | 0.475 | 0.696 | |||||||
| Overall | 23 | 0.819 | 0.818 | 0.819 | 690.6 | <0.001 | 453,257.3 | 22.0 | <0.001 | 100.0 | |
| After Third Dose | Moderna | 1 | 0.970 | 0.964 | 0.978 | ||||||
| Pfizer-BioNTech | 1 | 0.972 | 0.960 | 0.978 | |||||||
| CoronaVac | 1 | 0.638 | 0.631 | 0.643 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pormohammad, A.; Zarei, M.; Ghorbani, S.; Mohammadi, M.; Aghayari Sheikh Neshin, S.; Khatami, A.; Turner, D.L.; Djalalinia, S.; Mousavi, S.A.; Mardani-Fard, H.A.; et al. Effectiveness of COVID-19 Vaccines against Delta (B.1.617.2) Variant: A Systematic Review and Meta-Analysis of Clinical Studies. Vaccines 2022, 10, 23. https://doi.org/10.3390/vaccines10010023
Pormohammad A, Zarei M, Ghorbani S, Mohammadi M, Aghayari Sheikh Neshin S, Khatami A, Turner DL, Djalalinia S, Mousavi SA, Mardani-Fard HA, et al. Effectiveness of COVID-19 Vaccines against Delta (B.1.617.2) Variant: A Systematic Review and Meta-Analysis of Clinical Studies. Vaccines. 2022; 10(1):23. https://doi.org/10.3390/vaccines10010023
Chicago/Turabian StylePormohammad, Ali, Mohammad Zarei, Saied Ghorbani, Mehdi Mohammadi, Saeideh Aghayari Sheikh Neshin, Alireza Khatami, Diana L. Turner, Shirin Djalalinia, Seied Asadollah Mousavi, Heydar Ali Mardani-Fard, and et al. 2022. "Effectiveness of COVID-19 Vaccines against Delta (B.1.617.2) Variant: A Systematic Review and Meta-Analysis of Clinical Studies" Vaccines 10, no. 1: 23. https://doi.org/10.3390/vaccines10010023
APA StylePormohammad, A., Zarei, M., Ghorbani, S., Mohammadi, M., Aghayari Sheikh Neshin, S., Khatami, A., Turner, D. L., Djalalinia, S., Mousavi, S. A., Mardani-Fard, H. A., Kasaeian, A., & Turner, R. J. (2022). Effectiveness of COVID-19 Vaccines against Delta (B.1.617.2) Variant: A Systematic Review and Meta-Analysis of Clinical Studies. Vaccines, 10(1), 23. https://doi.org/10.3390/vaccines10010023









