Modulation of Oxidative Stress by Ozone Therapy in the Prevention and Treatment of Chemotherapy-Induced Toxicity: Review and Prospects
Abstract
1. Introduction
2. Chemotherapy-Induced Toxicity and Free Radicals
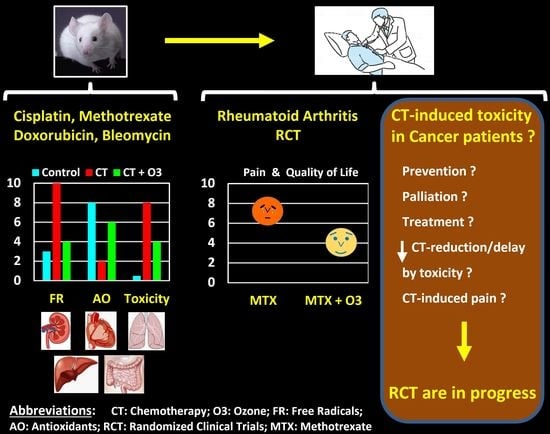
2.1. Cisplatin-Induced Toxicity
2.2. Methotrexate-Induced Toxicity
2.3. Doxorubicin-Induced Toxicity
2.4. Bleomycin-Induced Toxicity
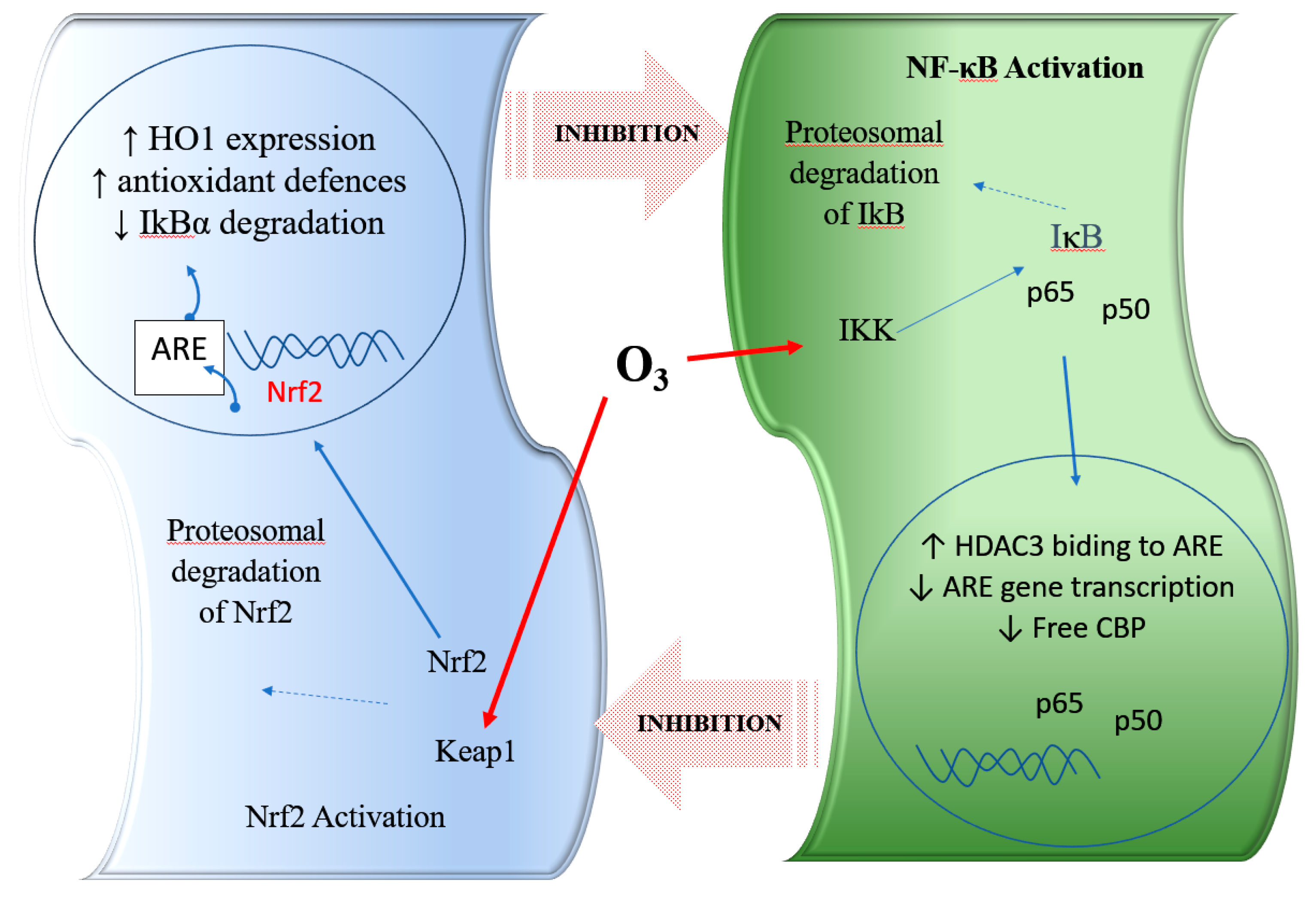
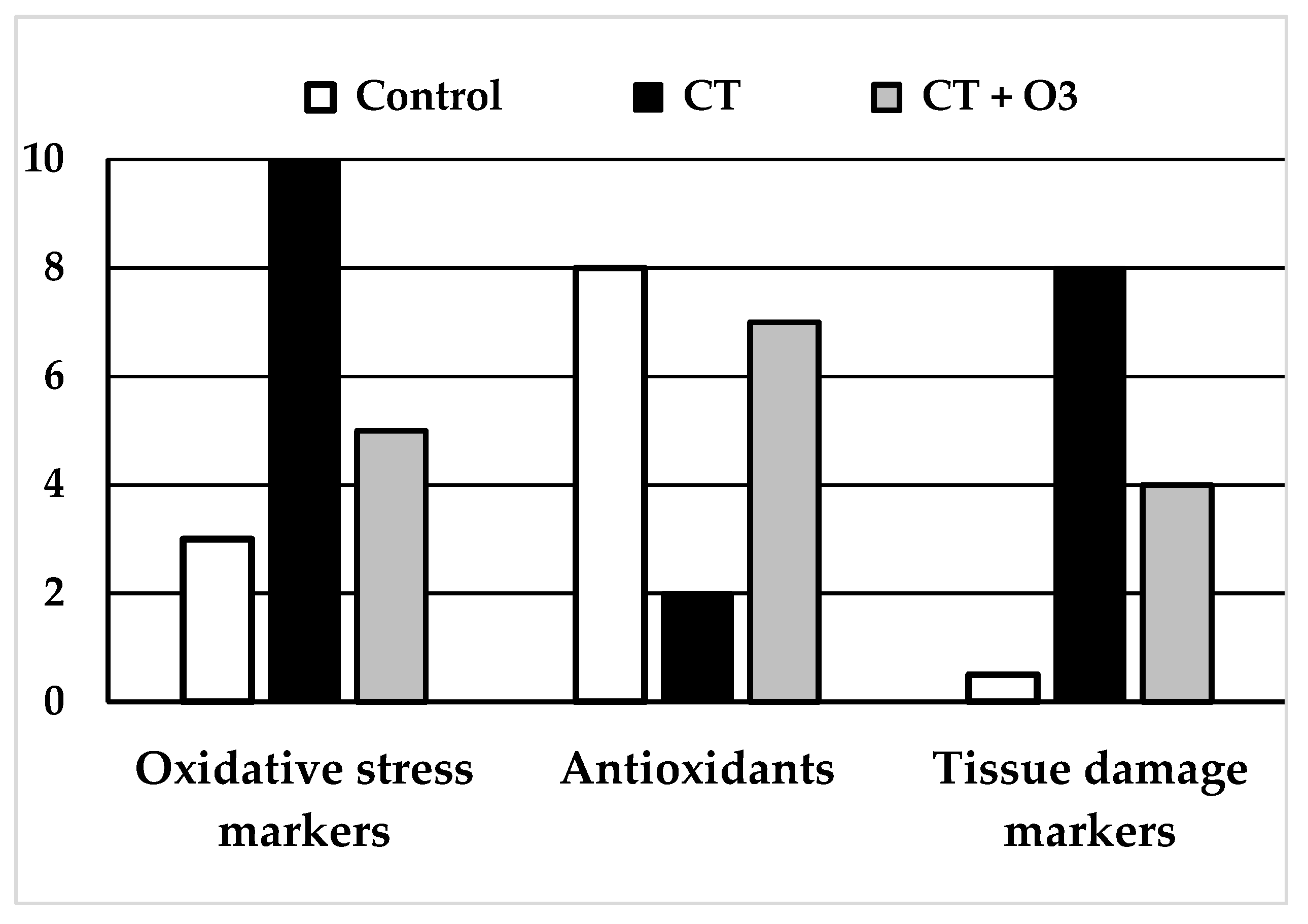
3. Modulation of Oxidative Stress by Ozone Therapy
4. Ozone Therapy in Chemotherapy-Induced Toxicity
4.1. Ozone and Cisplatin-Induced Toxicity
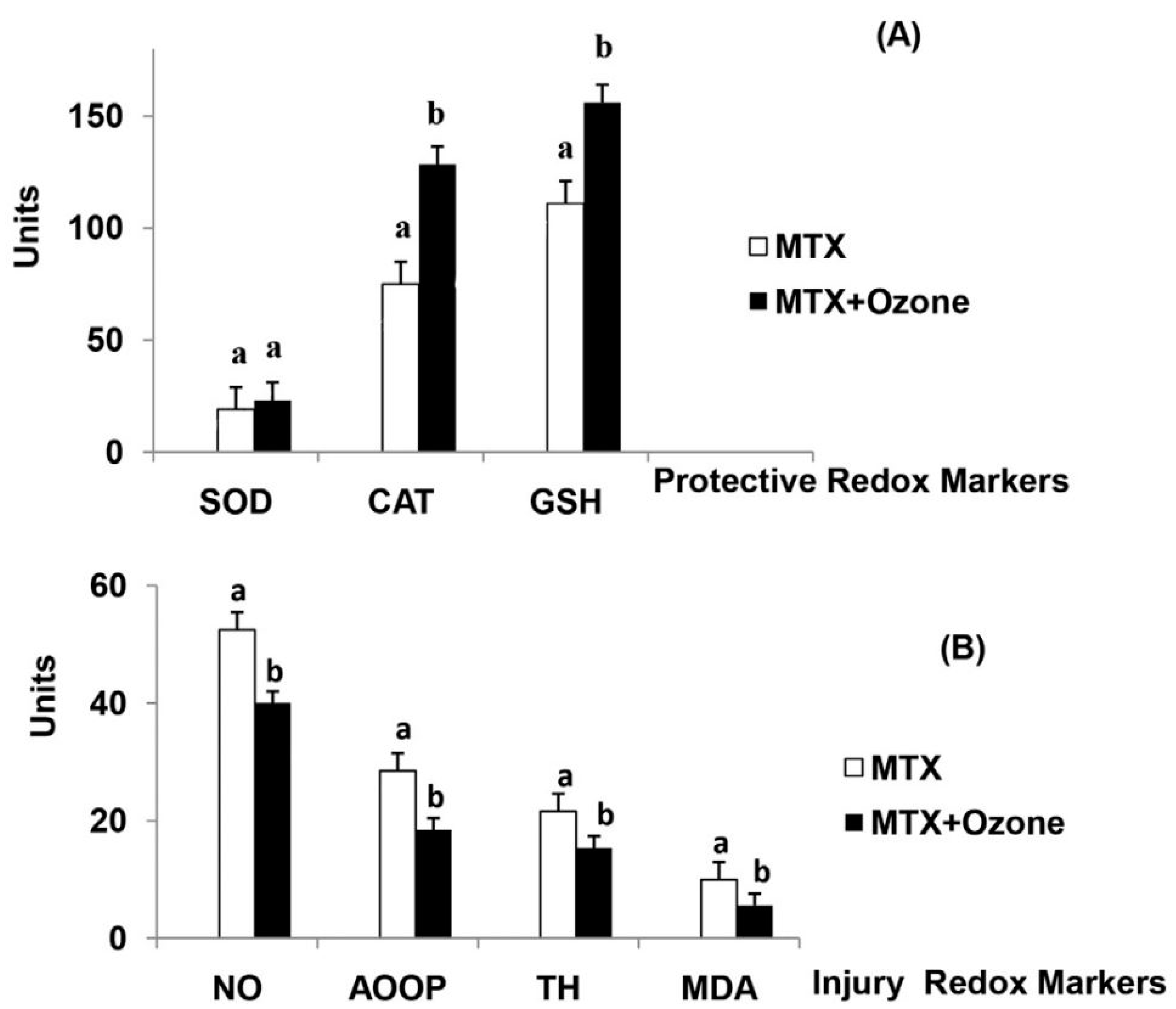
4.2. Ozone in Methotrexate-Induced Toxicity
4.3. Ozone in Doxorubicin-Induced Toxicity
4.4. Ozone in Bleomycin-Induced Toxicity
4.5. Other Related Studies
5. Discussion and Prospects
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Zuo, L.; Prather, E.R.; Stetskiv, M.; Garrison, D.E.; Meade, J.R.; Peace, T.I.; Zhou, T. Inflammaging and Oxidative Stress in Human Diseases: From Molecular Mechanisms to Novel Treatments. Int. J. Mol. Sci. 2019, 20, 4472. [Google Scholar] [CrossRef] [PubMed]
- Milkovic, L.; Cipak Gasparovic, A.; Zarkovic, N. Overview on major lipid peroxidation bioactive factor 4-hydroxynonenal as pluripotent growth-regulating factor. Free Radic. Res. 2015, 49, 850–860. [Google Scholar] [CrossRef]
- Bocci, V. Ozone A New Medical Drug, 2nd ed.; Springer Publishing: Dordrecht, The Netherlands, 2011. [Google Scholar]
- Schwartz-Tapia, A.; Martínez-Sánchez, G.; Sabah, F. Madrid Declaration on Ozone Therapy; ISCO3 (International Scientific Committee of Ozone Therapy): Madrid, Spain, 2015. [Google Scholar]
- Andrady, A.; Aucamp, P.J.; Bais, A.; Ballare, C.L.; Bjorn, L.O.; Bornman, J.F.; Caldwell, M.; Cullen, A.P.; Erickson, D.J.; de Gruijl, F.R.; et al. Environmental effects of ozone depletion and its interactions with climate change: Progress report, 2008. Photochem. Photobiol. Sci. 2009, 8, 13–22. [Google Scholar]
- Bocci, V. Is it true that ozone is always toxic? The end of a dogma. Toxicol. Appl. Pharmacol. 2006, 216, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Galie, M.; Covi, V.; Tabaracci, G.; Malatesta, M. The Role of Nrf2 in the Antioxidant Cellular Response to Medical Ozone Exposure. Int. J. Mol. Sci. 2019, 20, 4009. [Google Scholar] [CrossRef] [PubMed]
- Hakiminia, B.; Goudarzi, A.; Moghaddas, A. Has vitamin E any shreds of evidence in cisplatin-induced toxicity. J. Biochem. Mol. Toxicol. 2019, 33, e22349. [Google Scholar] [CrossRef]
- Pabla, N.; Dong, Z. Cisplatin nephrotoxicity: Mechanisms and renoprotective strategies. Kidney Int. 2008, 73, 994–1007. [Google Scholar] [CrossRef] [PubMed]
- Dugbartey, G.J.; Peppone, L.J.; de Graaf, I.A. An integrative view of cisplatin-induced renal and cardiac toxicities: Molecular mechanisms, current treatment challenges and potential protective measures. Toxicology 2016, 371, 58–66. [Google Scholar] [CrossRef]
- Howard, S.C.; McCormick, J.; Pui, C.H.; Buddington, R.K.; Harvey, R.D. Preventing and Managing Toxicities of High-Dose Methotrexate. Oncologist 2016, 21, 1471–1482. [Google Scholar] [CrossRef]
- Wessels, J.A.; Huizinga, T.W.; Guchelaar, H.J. Recent insights in the pharmacological actions of methotrexate in the treatment of rheumatoid arthritis. Rheumatology (Oxford) 2008, 47, 249–255. [Google Scholar] [CrossRef]
- Miyazono, Y.; Gao, F.; Horie, T. Oxidative stress contributes to methotrexate-induced small intestinal toxicity in rats. Scand. J. Gastroenterol. 2004, 39, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.M.; Hussein, O.E.; Hozayen, W.G.; Abd El-Twab, S.M. Methotrexate hepatotoxicity is associated with oxidative stress, and down-regulation of PPARgamma and Nrf2: Protective effect of 18beta-Glycyrrhetinic acid. Chem. Biol. Interact. 2017, 270, 59–72. [Google Scholar] [CrossRef]
- Pugazhendhi, A.; Edison, T.; Velmurugan, B.K.; Jacob, J.A.; Karuppusamy, I. Toxicity of Doxorubicin (Dox) to different experimental organ systems. Life Sci. 2018, 200, 26–30. [Google Scholar] [CrossRef]
- Luo, X.; Evrovsky, Y.; Cole, D.; Trines, J.; Benson, L.N.; Lehotay, D.C. Doxorubicin-induced acute changes in cytotoxic aldehydes, antioxidant status and cardiac function in the rat. Biochim. Biophys. Acta 1997, 1360, 45–52. [Google Scholar] [PubMed]
- Sikic, B.I. Biochemical and cellular determinants of bleomycin cytotoxicity. Cancer Surv. 1986, 5, 81–91. [Google Scholar]
- Yu, Z.; Yan, B.; Gao, L.; Dong, C.; Zhong, J.; DOrtenzio, M.; Nguyen, B.; Seong Lee, S.; Hu, X.; Liang, F. Targeted Delivery of Bleomycin: A Comprehensive Anticancer Review. Curr. Cancer Drug Targets 2016, 16, 509–521. [Google Scholar] [CrossRef] [PubMed]
- Shariati, S.; Kalantar, H.; Pashmforoosh, M.; Mansouri, E.; Khodayar, M.J. Epicatechin protective effects on bleomycin-induced pulmonary oxidative stress and fibrosis in mice. Biomed. Pharmacother. 2019, 114, 108776. [Google Scholar] [CrossRef]
- Chen, W.; Li, S.; Li, J.; Zhou, W.; Wu, S.; Xu, S.; Cui, K.; Zhang, D.D.; Liu, B. Artemisitene activates the Nrf2-dependent antioxidant response and protects against bleomycin-induced lung injury. FASEB J. 2016, 30, 2500–2510. [Google Scholar] [CrossRef]
- Bocci, V.; Borrelli, E.; Travagli, V.; Zanardi, I. The ozone paradox: Ozone is a strong oxidant as well as a medical drug. Med. Res. Rev. 2009, 29, 646–682. [Google Scholar] [CrossRef]
- Bocci, V.A.; Zanardi, I.; Travagli, V. Ozone acting on human blood yields a hormetic dose-response relationship. J. Transl. Med. 2011, 9, 66. [Google Scholar] [CrossRef]
- Viebahn-Hansler, R.; Leon Fernandez, O.S.; Fahmy, Z. Ozone in Medicine: The Low-Dose Ozone Concept—Guidelines and Treatment Strategies. Ozone-Sci. Eng. 2012, 34, 408–424. [Google Scholar] [CrossRef]
- Re, L.; Malcangi, G.; Martínez-Sánchez, G. Medical ozone is now ready for a scientific challenge: Current status and future perspectives. J. Exp. Integr. Med. 2012, 2, 193–196. [Google Scholar] [CrossRef]
- Hamilton, R.F., Jr.; Li, L.; Eschenbacher, W.L.; Szweda, L.; Holian, A. Potential involvement of 4-hydroxynonenal in the response of human lung cells to ozone. Am. J. Physiol. 1998, 274 (Pt 1), L8–L16. [Google Scholar] [CrossRef]
- Pryor, W.A.; Squadrito, G.L.; Friedman, M. The cascade mechanism to explain ozone toxicity: The role of lipid ozonation products. Free Radic. Biol. Med. 1995, 19, 935–941. [Google Scholar] [CrossRef]
- Pecorelli, A.; Bocci, V.; Acquaviva, A.; Belmonte, G.; Gardi, C.; Virgili, F.; Ciccoli, L.; Valacchi, G. NRF2 activation is involved in ozonated human serum upregulation of HO-1 in endothelial cells. Toxicol. Appl. Pharmacol. 2013, 267, 30–40. [Google Scholar] [CrossRef]
- Oliveira-Marques, V.; Marinho, H.S.; Cyrne, L.; Antunes, F. Role of hydrogen peroxide in NF-kappaB activation: From inducer to modulator. Antioxid. Redox Signal. 2009, 11, 2223–2243. [Google Scholar] [CrossRef]
- Huth, K.C.; Saugel, B.; Jakob, F.M.; Cappello, C.; Quirling, M.; Paschos, E.; Ern, K.; Hickel, R.; Brand, K. Effect of aqueous ozone on the NF-kappaB system. J. Dent. Res. 2007, 86, 451–456. [Google Scholar] [CrossRef]
- Kafoury, R.M.; Hernandez, J.M.; Lasky, J.A.; Toscano, W.A., Jr.; Friedman, M. Activation of transcription factor IL-6 (NF-IL-6) and nuclear factor-kappaB (NF-kappaB) by lipid ozonation products is crucial to interleukin-8 gene expression in human airway epithelial cells. Environ. Toxicol. 2007, 22, 159–168. [Google Scholar] [CrossRef]
- Wang, L.; Chen, Z.; Liu, Y.; Du, Y.; Liu, X. Ozone oxidative postconditioning inhibits oxidative stress and apoptosis in renal ischemia and reperfusion injury through inhibition of MAPK signaling pathway. Drug Des. Devel. Ther. 2018, 12, 1293–1301. [Google Scholar] [CrossRef]
- Galie, M.; Costanzo, M.; Nodari, A.; Boschi, F.; Calderan, L.; Mannucci, S.; Covi, V.; Tabaracci, G.; Malatesta, M. Mild ozonisation activates antioxidant cell response by the Keap1/Nrf2 dependent pathway. Free Radic. Biol. Med. 2018, 124, 114–121. [Google Scholar] [CrossRef]
- Siniscalco, D.; Trotta, M.C.; Brigida, A.L.; Maisto, R.; Luongo, M.; Ferraraccio, F.; D’Amico, M.; Di Filippo, C. Intraperitoneal Administration of Oxygen/Ozone to Rats Reduces the Pancreatic Damage Induced by Streptozotocin. Biology (Basel) 2018, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Nakasone, M.; Nakaso, K.; Horikoshi, Y.; Hanaki, T.; Kitagawa, Y.; Takahashi, T.; Inagaki, Y.; Matsura, T. Preconditioning by Low Dose LPS Prevents Subsequent LPS-Induced Severe Liver Injury via Nrf2 Activation in Mice. Yonago Acta Med. 2016, 59, 223–231. [Google Scholar] [PubMed]
- Ayala, A.; Munoz, M.F.; Arguelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef] [PubMed]
- Breitzig, M.; Bhimineni, C.; Lockey, R.; Kolliputi, N. 4-Hydroxy-2-nonenal: A critical target in oxidative stress? Am. J. Physiol. Cell Physiol. 2016, 311, C537–C543. [Google Scholar] [CrossRef] [PubMed]
- Re, L.; Martínez-Sánchez, G.; Bordicchia, M.; Malcangi, G.; Pocognoli, A.; Angel Morales-Segura, M.; Rothchild, J.; Rojas, A. Is ozone pre-conditioning effect linked to Nrf2/EpRE activation pathway in vivo? A preliminary result. Eur. J. Pharmacol. 2014, 742, 158–162. [Google Scholar] [CrossRef]
- Delgado-Roche, L.; Riera-Romo, M.; Mesta, F.; Hernandez-Matos, Y.; Barrios, J.M.; Martinez-Sanchez, G.; Al-Dalaien, S.M. Medical ozone promotes Nrf2 phosphorylation reducing oxidative stress and pro-inflammatory cytokines in multiple sclerosis patients. Eur. J. Pharmacol. 2017, 811, 148–154. [Google Scholar] [CrossRef]
- Ahmed, S.M.; Luo, L.; Namani, A.; Wang, X.J.; Tang, X. Nrf2 signaling pathway: Pivotal roles in inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 585–597. [Google Scholar] [CrossRef]
- Ganesh Yerra, V.; Negi, G.; Sharma, S.S.; Kumar, A. Potential therapeutic effects of the simultaneous targeting of the Nrf2 and NF-kappaB pathways in diabetic neuropathy. Redox Biol. 2013, 1, 394–397. [Google Scholar] [CrossRef]
- Mohan, S.; Gupta, D. Crosstalk of toll-like receptors signaling and Nrf2 pathway for regulation of inflammation. Biomed. Pharmacother. 2018, 108, 1866–1878. [Google Scholar] [CrossRef]
- Wardyn, J.D.; Ponsford, A.H.; Sanderson, C.M. Dissecting molecular cross-talk between Nrf2 and NF-kappaB response pathways. Biochem. Soc. Trans. 2015, 43, 621–626. [Google Scholar] [CrossRef]
- Yu, G.; Liu, X.; Chen, Z.; Chen, H.; Wang, L.; Wang, Z.; Qiu, T.; Weng, X. Ozone therapy could attenuate tubulointerstitial injury in adenine-induced CKD rats by mediating Nrf2 and NF-kappaB. Iran. J. Basic Med. Sci. 2016, 19, 1136–1143. [Google Scholar] [PubMed]
- Borrego, A.; Zamora, Z.B.; Gonzalez, R.; Romay, C.; Menendez, S.; Hernandez, F.; Montero, T.; Rojas, E. Protection by ozone preconditioning is mediated by the antioxidant system in cisplatin-induced nephrotoxicity in rats. Mediators Inflamm. 2004, 13, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, R.; Borrego, A.; Zamora, Z.; Romay, C.; Hernandez, F.; Menendez, S.; Montero, T.; Rojas, E. Reversion by ozone treatment of acute nephrotoxicity induced by cisplatin in rats. Mediators Inflamm. 2004, 13, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Borrego, A.; Zamora, Z.B.; Gonzalez, R.; Romay, C.; Menendez, S.; Hernandez, F.; Berlanga, J.; Montero, T. Ozone/oxygen mixture modifies the subcellular redistribution of Bax protein in renal tissue from rats treated with cisplatin. Arch. Med. Res. 2006, 37, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Sheikh-Hamad, D.; Cacini, W.; Buckley, A.R.; Isaac, J.; Truong, L.D.; Tsao, C.C.; Kishore, B.K. Cellular and molecular studies on cisplatin-induced apoptotic cell death in rat kidney. Arch. Toxicol. 2004, 78, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Redza-Dutordoir, M.; Averill-Bates, D.A. Activation of apoptosis signalling pathways by reactive oxygen species. Biochim. Biophys. Acta 2016, 1863, 2977–2992. [Google Scholar] [CrossRef]
- Shiraishi, F.; Curtis, L.M.; Truong, L.; Poss, K.; Visner, G.A.; Madsen, K.; Nick, H.S.; Agarwal, A. Heme oxygenase-1 gene ablation or expression modulates cisplatin-induced renal tubular apoptosis. Am. J. Physiol. Renal. Physiol. 2000, 278, F726–F736. [Google Scholar] [CrossRef]
- Bolisetty, S.; Traylor, A.; Joseph, R.; Zarjou, A.; Agarwal, A. Proximal tubule-targeted heme oxygenase-1 in cisplatin-induced acute kidney injury. Am. J. Physiol. Renal. Physiol. 2016, 310, F385–F394. [Google Scholar] [CrossRef]
- Bocci, V.; Valacchi, G. Nrf2 activation as target to implement therapeutic treatments. Front. Chem. 2015, 3, 4. [Google Scholar] [CrossRef]
- Kocak, H.E.; Taskin, U.; Aydin, S.; Oktay, M.F.; Altinay, S.; Celik, D.S.; Yucebas, K.; Altas, B. Effects of ozone (O3) therapy on cisplatin-induced ototoxicity in rats. Eur. Arch. Otorhinolaryngol. 2016, 273, 4153–4159. [Google Scholar] [CrossRef]
- Kesik, V.; Uysal, B.; Kurt, B.; Kismet, E.; Koseoglu, V. Ozone ameliorates methotrexate-induced intestinal injury in rats. Cancer Biol. Ther. 2009, 8, 1623–1628. [Google Scholar] [CrossRef] [PubMed]
- Aslaner, A.; Cakir, T.; Celik, B.; Dogan, U.; Mayir, B.; Akyuz, C.; Polat, C.; Basturk, A.; Soyer, V.; Koc, S.; et al. Does intraperitoneal medical ozone preconditioning and treatment ameliorate the methotrexate induced nephrotoxicity in rats? Int. J. Clin. Exp. Med. 2015, 8, 13811–13817. [Google Scholar] [PubMed]
- Aslaner, A.; Cakir, T.; Celik, B.; Dogan, U.; Akyuz, C.; Basturk, A.; Polat, C.; Gunduz, U.; Mayir, B.; Sehirli, A.O. The protective effect of intraperitoneal medical ozone preconditioning and treatment on hepatotoxicity induced by methotrexate. Int. J. Clin. Exp. Med. 2015, 8, 13303–13309. [Google Scholar] [PubMed]
- Leon Fernandez, O.S.; Viebahn-Haensler, R.; Cabreja, G.L.; Espinosa, I.S.; Matos, Y.H.; Roche, L.D.; Santos, B.T.; Oru, G.T.; Polo Vega, J.C. Medical ozone increases methotrexate clinical response and improves cellular redox balance in patients with rheumatoid arthritis. Eur. J. Pharmacol. 2016, 789, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Roche, L.; Hernandez-Matos, Y.; Medina, E.A.; Morejon, D.A.; Gonzalez, M.R.; Martinez-Sanchez, G. Ozone-Oxidative Preconditioning Prevents Doxorubicin-induced Cardiotoxicity in Sprague-Dawley Rats. Sultan Qaboos Univ. Med. J. 2014, 14, e342–e348. [Google Scholar]
- Calunga Fernández, J.L.; Bello Ferro, M.; Chaple La Hoz, M.; Barber Gutierrez, E.; Menendez Cepero, S.; Merino, N. Ozonoterapia en la glomerulonefritis tóxica experimental por adriamicina. Rev. Cubana Investig. Biomed. 2004, 23, 139–143. [Google Scholar]
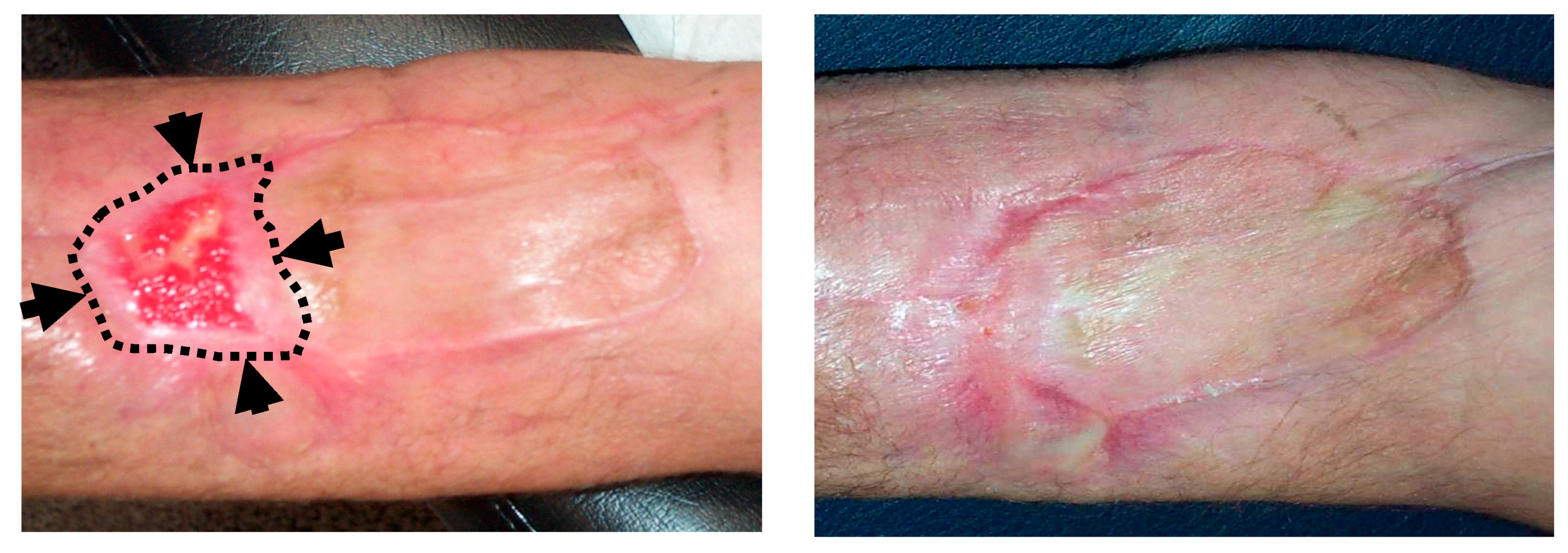
- Kesik, V.; Yuksel, R.; Yigit, N.; Saldir, M.; Karabacak, E.; Erdem, G.; Babacan, O.; Gulgun, M.; Korkmazer, N.; Bayrak, Z. Ozone Ameliorates Doxorubicine-Induced Skin Necrosis - results from an animal model. Int. J. Low Extrem. Wounds 2016, 15, 248–254. [Google Scholar] [CrossRef]
- Salem, E.A.; Salem, N.A.; Hellstrom, W.J. Therapeutic effect of ozone and rutin on adriamycin-induced testicular toxicity in an experimental rat model. Andrologia 2017, 49, e12603. [Google Scholar] [CrossRef]
- Kamble, S.M.; Patil, C.R. Asiatic Acid Ameliorates Doxorubicin-Induced Cardiac and Hepato-Renal Toxicities with Nrf2 Transcriptional Factor Activation in Rats. Cardiovasc Toxicol. 2018, 18, 131–141. [Google Scholar] [CrossRef]
- Santana-Rodriguez, N.; Santisteban, P.L.; Clavo, B.; Camacho, R.; Santana, C.; Fiuza, M.D. Protective effect of ozone in an experimental model of pulmonary fibrosis. Br. J. Surg. 2015, 102, 11. [Google Scholar]
- Menendez Cepero, S.; Gonzalez Alvarez, R.; Ledea Lozano, O.E.; Hernandez Rosales, F.; Leon Fernandez, O.S.; Diaz Gomez, M. Ozono, Aspectos Básicos y Aplicaciones Clínicas; Centro de Investigaciones del Ozono: La Habana, Cuba, 2008. [Google Scholar]
- Borrelli, E. Treatment of advanced non-small-cell lung cancer with oxygen ozone therapy and mistletoe: An integrative approach. Eur. J. Integr. Med. 2012, 4, 130. [Google Scholar]
- Velasco, R.; Bruna, J. Chemotherapy-induced peripheral neuropathy: An unresolved issue. Neurologia 2010, 25, 116–131. [Google Scholar] [CrossRef]
- Velasco, R.; Santos, C.; Soler, G.; Gil-Gil, M.; Pernas, S.; Galan, M.; Palmero, R.; Bruna, J. Serum micronutrients and prealbumin during development and recovery of chemotherapy-induced peripheral neuropathy. J. Peripher. Nerv. Syst. 2016, 21, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Starobova, H.; Vetter, I. Pathophysiology of Chemotherapy-Induced Peripheral Neuropathy. Front. Mol. Neurosci. 2017, 10, 174. [Google Scholar] [CrossRef] [PubMed]
- Albers, J.W.; Chaudhry, V.; Cavaletti, G.; Donehower, R.C. Interventions for preventing neuropathy caused by cisplatin and related compounds. Cochrane Database Syst. Rev. 2014, 3, CD005228. [Google Scholar] [CrossRef]
- Hershman, D.L.; Lacchetti, C.; Dworkin, R.H.; Lavoie Smith, E.M.; Bleeker, J.; Cavaletti, G.; Chauhan, C.; Gavin, P.; Lavino, A.; Lustberg, M.B.; et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. 2014, 32, 1941–1967. [Google Scholar] [CrossRef]
- Clavo, B. Ozone therapy in the management of side effects related to cancer treatments. In Proceedings of the 2nd International Traditional and Complementary Medicine Congress (Organized with technical sponsorship of the World Health Organization), Istanbul, Turkey, 24 April 2019. [Google Scholar]
- Bakkal, B.H.; Gultekin, F.A.; Guven, B.; Turkcu, U.O.; Bektas, S.; Can, M. Effect of ozone oxidative preconditioning in preventing early radiation-induced lung injury in rats. Braz J. Med. Biol. Res. 2013, 46, 789–796. [Google Scholar] [CrossRef]
- Gultekin, F.A.; Bakkal, B.H.; Guven, B.; Tasdoven, I.; Bektas, S.; Can, M.; Comert, M. Effects of ozone oxidative preconditioning on radiation-induced organ damage in rats. J. Radiat. Res. 2013, 54, 36–44. [Google Scholar] [CrossRef]
- Menendez, S.; Cepero, J.; Borrego, L.R. Ozone therapy in cancer treatment: State of the art. Ozone Sci. Eng. 2008, 30, 398–404. [Google Scholar] [CrossRef]
- Clavo, B.; Ceballos, D.; Gutierrez, D.; Rovira, G.; Suarez, G.; Lopez, L.; Pinar, B.; Cabezon, A.; Morales, V.; Oliva, E.; et al. Long-term control of refractory hemorrhagic radiation proctitis with ozone therapy. J. Pain Symptom Manag. 2013, 46, 106–112. [Google Scholar] [CrossRef]
- Clavo, B.; Santana-Rodriguez, N.; Llontop, P.; Gutierrez, D.; Ceballos, D.; Mendez, C.; Rovira, G.; Suarez, G.; Rey-Baltar, D.; Garcia-Cabrera, L.; et al. Ozone Therapy in the Management of Persistent Radiation-Induced Rectal Bleeding in Prostate Cancer Patients. Evid. Based Complement. Alternat. Med. 2015, 2015, 480369. [Google Scholar] [CrossRef] [PubMed]
- Milkovic, L.; Zarkovic, N.; Saso, L. Controversy about pharmacological modulation of Nrf2 for cancer therapy. Redox Biol. 2017, 12, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.; Yin, H. Role of lipid peroxidation derived 4-hydroxynonenal (4-HNE) in cancer: Focusing on mitochondria. Redox Biol. 2015, 4, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.G.; Bhatia, S.K.; Buatti, J.M.; Brandt, K.E.; Lindholm, K.E.; Button, A.M.; Szweda, L.I.; Smith, B.J.; Spitz, D.R.; Fath, M.A. Ketogenic diets enhance oxidative stress and radio-chemo-therapy responses in lung cancer xenografts. Clin. Cancer Res. 2013, 19, 3905–3913. [Google Scholar] [CrossRef]
- DiDonato, J.A.; Mercurio, F.; Karin, M. NF-kappaB and the link between inflammation and cancer. Immunol. Rev. 2012, 246, 379–400. [Google Scholar] [CrossRef]
- Garg, A.; Aggarwal, B.B. Nuclear transcription factor-kappaB as a target for cancer drug development. Leukemia 2002, 16, 1053–1068. [Google Scholar] [CrossRef]
- El-Deek, H.E.M.; Ahmed, A.M.; Mohammed, R.A.A. Aberration of Nrf2Bach1 pathway in colorectal carcinoma; role in carcinogenesis and tumor progression. Ann. Diagn. Pathol. 2019, 38, 138–144. [Google Scholar] [CrossRef]
- Rocha, C.R.; Kajitani, G.S.; Quinet, A.; Fortunato, R.S.; Menck, C.F. NRF2 and glutathione are key resistance mediators to temozolomide in glioma and melanoma cells. Oncotarget 2016, 7, 48081–48092. [Google Scholar] [CrossRef]
- Zheng, H.; Nong, Z.; Lu, G. Correlation Between Nuclear Factor E2-Related Factor 2 Expression and Gastric Cancer Progression. Med. Sci. Monit. 2015, 21, 2893–2899. [Google Scholar] [CrossRef]
- Rojo de la Vega, M.; Chapman, E.; Zhang, D.D. NRF2 and the Hallmarks of Cancer. Cancer Cell 2018, 34, 21–43. [Google Scholar] [CrossRef]
- Yasueda, A.; Urushima, H.; Ito, T. Efficacy and Interaction of Antioxidant Supplements as Adjuvant Therapy in Cancer Treatment: A Systematic Review. Integr. Cancer Ther. 2016, 15, 17–39. [Google Scholar] [CrossRef] [PubMed]
- Conklin, K.A. Chemotherapy-associated oxidative stress: Impact on chemotherapeutic effectiveness. Integr. Cancer Ther. 2004, 3, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Clavo, B.; Santana-Rodriguez, N.; Llontop, P.; Gutierrez, D.; Suarez, G.; Lopez, L.; Rovira, G.; Martinez-Sanchez, G.; Gonzalez, E.; Jorge, I.J.; et al. Ozone Therapy as Adjuvant for Cancer Treatment: Is Further Research Warranted? Evid. Based Complement. Alternat. Med. 2018, 2018, 7931849. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clavo, B.; Rodríguez-Esparragón, F.; Rodríguez-Abreu, D.; Martínez-Sánchez, G.; Llontop, P.; Aguiar-Bujanda, D.; Fernández-Pérez, L.; Santana-Rodríguez, N. Modulation of Oxidative Stress by Ozone Therapy in the Prevention and Treatment of Chemotherapy-Induced Toxicity: Review and Prospects. Antioxidants 2019, 8, 588. https://doi.org/10.3390/antiox8120588
Clavo B, Rodríguez-Esparragón F, Rodríguez-Abreu D, Martínez-Sánchez G, Llontop P, Aguiar-Bujanda D, Fernández-Pérez L, Santana-Rodríguez N. Modulation of Oxidative Stress by Ozone Therapy in the Prevention and Treatment of Chemotherapy-Induced Toxicity: Review and Prospects. Antioxidants. 2019; 8(12):588. https://doi.org/10.3390/antiox8120588
Chicago/Turabian StyleClavo, Bernardino, Francisco Rodríguez-Esparragón, Delvys Rodríguez-Abreu, Gregorio Martínez-Sánchez, Pedro Llontop, David Aguiar-Bujanda, Leandro Fernández-Pérez, and Norberto Santana-Rodríguez. 2019. "Modulation of Oxidative Stress by Ozone Therapy in the Prevention and Treatment of Chemotherapy-Induced Toxicity: Review and Prospects" Antioxidants 8, no. 12: 588. https://doi.org/10.3390/antiox8120588
APA StyleClavo, B., Rodríguez-Esparragón, F., Rodríguez-Abreu, D., Martínez-Sánchez, G., Llontop, P., Aguiar-Bujanda, D., Fernández-Pérez, L., & Santana-Rodríguez, N. (2019). Modulation of Oxidative Stress by Ozone Therapy in the Prevention and Treatment of Chemotherapy-Induced Toxicity: Review and Prospects. Antioxidants, 8(12), 588. https://doi.org/10.3390/antiox8120588