Pyroptosis Modulators: New Insights of Gasdermins in Health and Disease
Abstract
1. Introduction
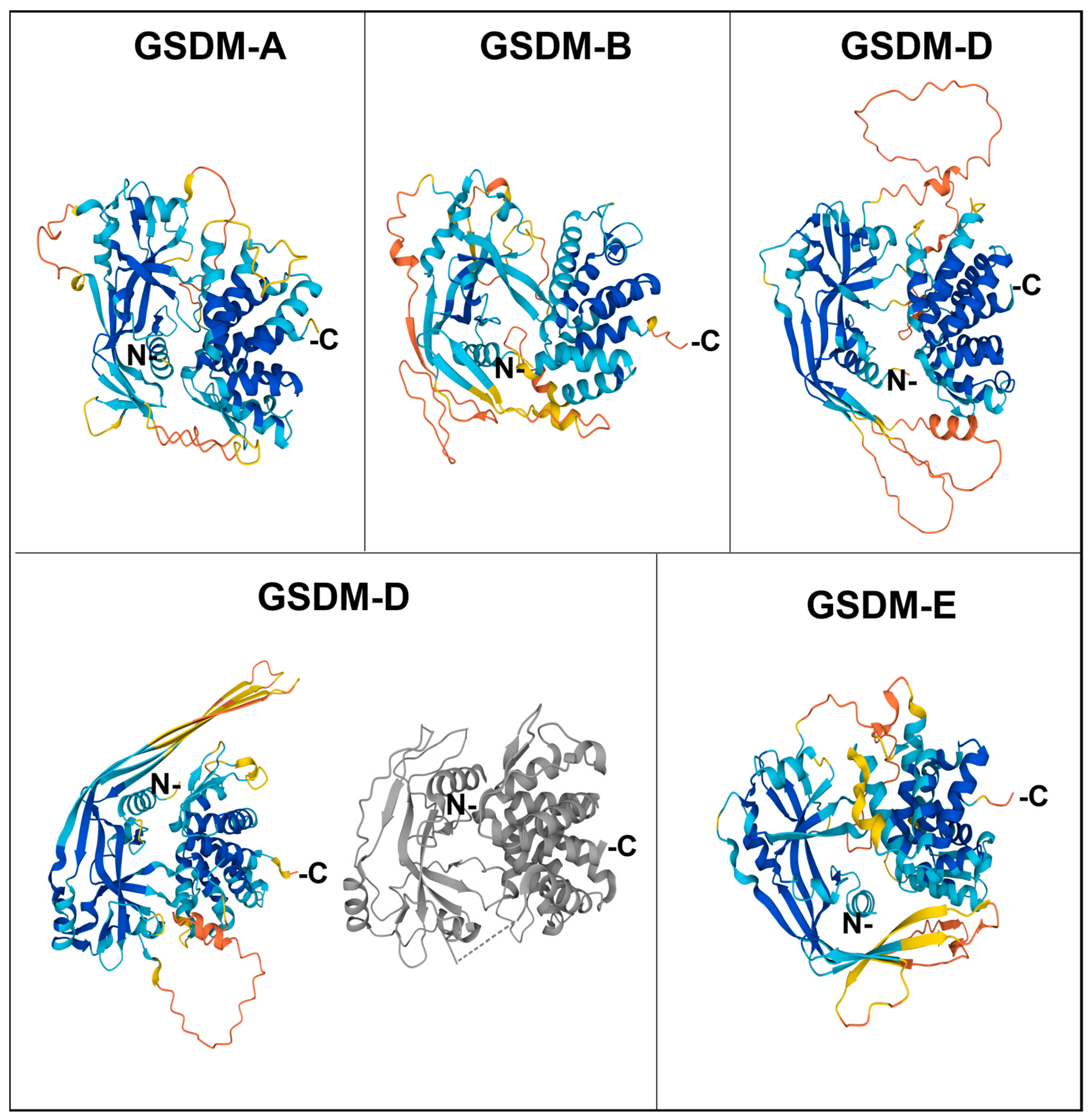
2. Structural Aspects of the Gasdermin Family in Humans
| Human GSDM | Chromosomal Location | Expression Pattern | Pore Formation |
|---|---|---|---|
| GSDMA | 17q21 | Gastrointestinal tract and skin | Yes |
| GSDMB | 17q21 | Cells of the gastrointestinal and respiratory tracts, T cells, and cervix and breast cells | Yes |
| GSDMC | 8q24.2 | Cells of the gastrointestinal tract, trachea, and skin | Yes |
| GSDMD | 8q24.2 | Cells of the gastrointestinal tract, macrophages, neutrophiles, monocytes, and T and B cells | Yes |
| GSDME | 7p15 | Cells of the gastrointestinal tract, placenta, cochlea, and brain | Yes |
| GSDMF | 2q31.1-q31.3 | Cells of the inner ear | ND |
3. Functional Features of the Different Members of the Human Gasdermin Family
3.1. GSDMA
3.2. GSDMB
3.3. GSDMC
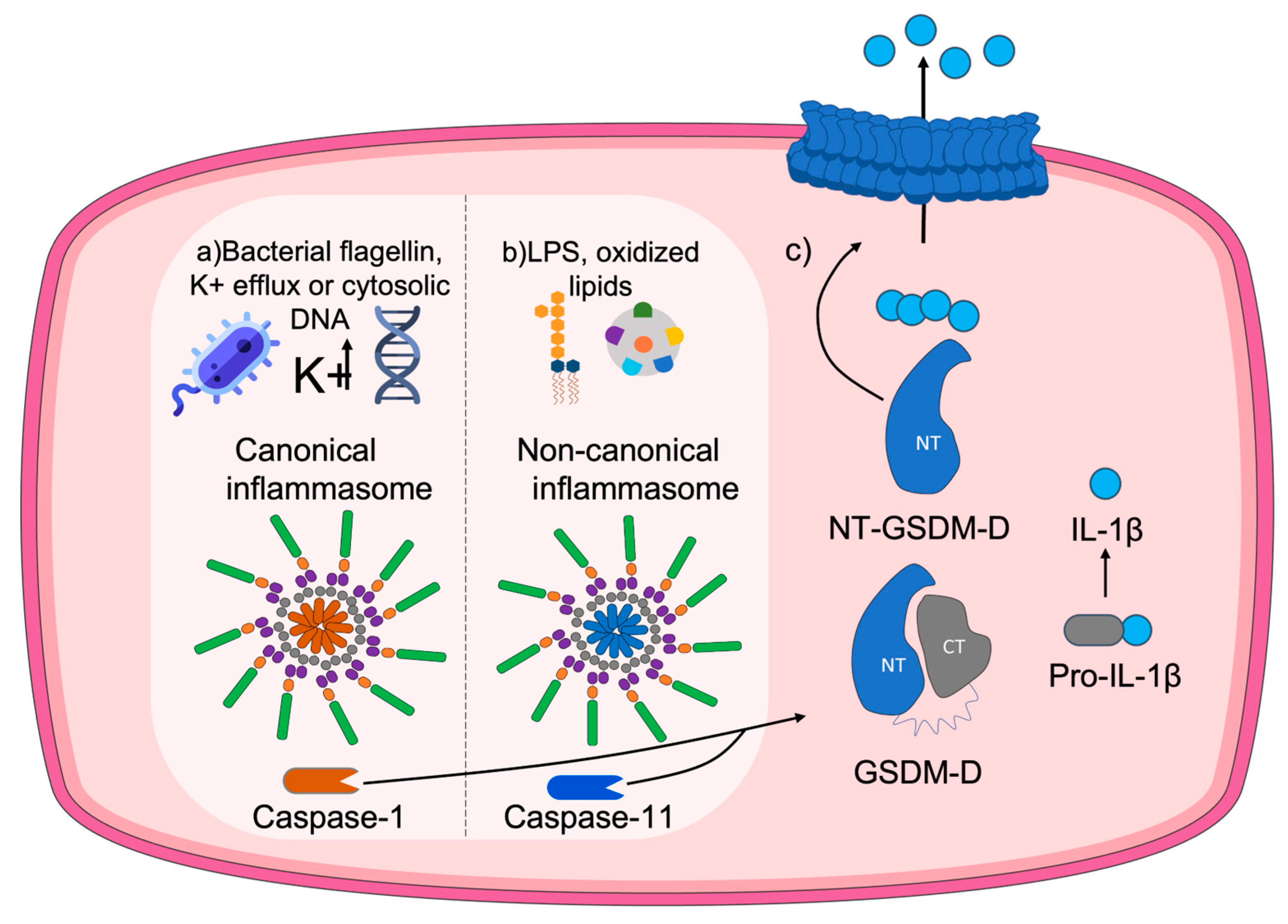
3.4. GSDMD
3.5. GSDME
3.6. GSDMF
4. Involvement of Gasdermin Pore Formation in Pyroptosis
5. Gasdermins, Pyroptosis, and Cancer
| Compound | Type of Cancer | Pyroptosis-Related Mechanism | Experimental Models | Reference |
|---|---|---|---|---|
| Aloe-emodin | - | Increased pyroptosis via activation of the caspase 3/9-GSDME axis in HeLa cells | HeLa cells | [123] |
| Anthocyanin | Oral squamous cell carcinoma (OSCC) | Activation of pyroptosis through enhanced expression of NLRP3, caspase-1, and IL-1β | HaCaT, Tca8113, and SCC15 cells | [100] |
| Bexarotene | Ovarian cancer (OC) | Induction of Caspase-4-gasdermin E mediated pyroptosis | ES2 and NIH:OVCAR3 OC cell lines. | [127] |
| Combination of BRAF inhibitors and MEK inhibitors (BRAFi + MEKi) | BRAF V600E/K-mutant melanoma | Increased GSDME-mediated pyroptosis related to ERK1/2 pathway inhibition | Human and syngeneic mouse melanoma models | [103] |
| Curcumin | Hepatocellular Carcinoma | Augmented pyroptosis through increased expression of GSDME N-terminal domain | HepG2 cells | [121] |
| Dihydroartemisinin | Breast cancer (BC) | Induced pyroptosis through promotion of the caspase-3/GSDME axis | MCF-7 and MDA-MB-231 cell lines. BC xenografts in BALB/c nude mice | [126] |
| Dimethyl⍺-ketoglutarate | - | Induced GSDMC-dependent pyroptosis through death receptor 6-activated caspase-8 | HeLa and other cell lines. Male nude mice and C57BL/6J mice | [110] |
| Galangin | Human glioblastoma multiforme (GBM) | Simultaneous induction of apoptosis, pytoptosis, and autophagy | U251, U87MG, and A172 cells. Orthotopic xenograft model in nude mice derived from U87MG cells | [101] |
| Germacrone | Liver cancer | Induced GSDME-dependent pyroptosis through caspase 3 activation | HepG2 cells. HepG2 cell xenograft models | [122] |
| N,N-dimethylbiguanide metformin | Esophageal squamous cell carcinoma (ESCC) | Induction of gasdermin D (GSDMD)-mediated pyroptosis by targeting miR-497/PELP1 axis | Tumor samples of human primary ESCC | [102] |
| Phenylsulfonimide PPAR⍺antagonists | Breast cancer (BC) | Induction of apoptosis and pyroptosis via Nrf2 activation and promotion of oxidative stress | MCF7 cell line | [104] |
| Secoisolariciresinol diglucoside | Colorectal cancer (CC) | GSDMD-dependent pyroptosis through generation of ROS/P13K/AKT/BAK-mitochondrial pathway apoptosis | HCT116 cells. HCT116-CRC xenograft model in nude mice | [117] |
| Simvastatin + DNA methyltransferase inhibitor | Gastric Cancer (GC) | Increased GSDME-mediated pyroptosis | Human samples of GC tissue. GC cell lines AGS, MKN45, HGC-27, and MGC-803. GC xenograft model in mice. | [128] |
| Trichosanthin | Non-small cell lung cancer (NSCLC) | Increased pyroptosis via expression of GSDMD and NLRP3 | NSCLC cells. Tumor xenograft model in nude mice derived from A549 cells | [116] |
| Wedelolactone | Retinoblastoma (RB) | Pyroptosis and apoptosis induction via simultaneous activation of GSDMD and GSDME, and caspases 1 and 3 | RB cell lines Y79 and Weri-Rb1. Xenograft experiments on BALB/c nude mice derived from Y79 cells. | [125] |
6. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shearer, A.E.; Hildebrand, M.S.; Smith, R.J. Hereditary Hearing Loss and Deafness Overview. In GeneReviews® [Internet]; Adam, M.P., Ed.; University of Washington: Seattle, WA, USA, 1999. [Google Scholar]
- Saeki, N.; Kuwahara, Y.; Sasaki, H.; Satoh, H.; Shiroishi, T. Gasdermin (Gsdm) Localizing to Mouse Chromosome 11 Is Predominantly Expressed in Upper Gastrointestinal Tract but Significantly Suppressed in Human Gastric Cancer Cells. Mamm. Genome 2000, 11, 718–724. [Google Scholar] [CrossRef]
- Sun, Q.; Zhang, L.Q.; He, F.C. Progress of Researches on Gene Function of GSDMDC Family. Yi Chuan 2006, 28, 596–600. [Google Scholar]
- Shi, J.; Zhao, Y.; Wang, K.; Shi, X.; Wang, Y.; Huang, H.; Zhuang, Y.; Cai, T.; Wang, F.; Shao, F. Cleavage of GSDMD by Inflammatory Caspases Determines Pyroptotic Cell Death. Nature 2015, 526, 660–665. [Google Scholar] [CrossRef] [PubMed]
- De Vasconcelos, N.M.; Lamkanfi, M. Recent Insights on Inflammasomes, Gasdermin Pores, and Pyroptosis. Cold Spring Harb. 2020, 12, a036392. [Google Scholar] [CrossRef]
- De Schutter, E.; Roelandt, R.; Riquet, F.B.; Van Camp, G.; Wullaert, A.; Vandenabeele, P. Punching Holes in Cellular Membranes: Biology and Evolution of Gasdermins. Trends Cell Biol. 2021, 31, 500–513. [Google Scholar] [CrossRef] [PubMed]
- Devant, P.; Boršić, E.; Ngwa, E.M.; Xiao, H.; Chouchani, E.T.; Thiagarajah, J.R.; Hafner-Bratkovič, I.; Evavold, C.L.; Kagan, J.C. Gasdermin D Pore-Forming Activity Is Redox-Sensitive. Cell Rep. 2023, 42, 112008. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Tian, S.; Pan, Y.; Li, W.; Wang, Q.; Tang, Y.; Yu, T.; Wu, X.; Shi, Y.; Ma, P.; et al. Pyroptosis: A New Frontier in Cancer. Biomed. Pharmacother. 2020, 121, 109595. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Xia, S.; Zhang, Z.; Wu, H.; Lieberman, J. Channelling Inflammation: Gasdermins in Physiology and Disease. Nat. Rev. Drug Discov. 2021, 20, 384–405. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Liu, X.L.; Zhao, R. Induction of Pyroptosis and Its Implications in Cancer Management. Front. Oncol. 2019, 9, 971. [Google Scholar] [CrossRef]
- Ding, J.; Wang, K.; Liu, W.; She, Y.; Sun, Q.; Shi, J.; Sun, H.; Wang, D.C.; Shao, F. Pore-Forming Activity and Structural Autoinhibition of the Gasdermin Family. Nature 2016, 535, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Hergueta-Redondo, M.; Sarrió, D.; Molina-Crespo, Á.; Megias, D.; Mota, A.; Rojo-Sebastian, A.; García-Sanz, P.; Morales, S.; Abril, S.; Cano, A.; et al. Gasdermin-B Promotes Invasion and Metastasis in Breast Cancer Cells. PLoS ONE 2014, 9, e90099. [Google Scholar] [CrossRef]
- Chen, X.; He, W.T.; Hu, L.; Li, J.; Fang, Y.; Wang, X.; Xu, X.; Wang, Z.; Huang, K.; Han, J. Pyroptosis Is Driven by Non-Selective Gasdermin-D Pore and Its Morphology Is Different from MLKL Channel-Mediated Necroptosis. Cell Res. 2016, 26, 1007–1020. [Google Scholar] [CrossRef]
- Shi, J.; Gao, W.; Shao, F. Pyroptosis: Gasdermin-Mediated Programmed Necrotic Cell Death. Trends Biochem. Sci. 2017, 42, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Kesavardhana, S.; Malireddi, R.K.S.; Kanneganti, T.D. Caspases in Cell Death, Inflammation, and Pyroptosis. Annu. Rev. Immunol. 2020, 38, 567–595. [Google Scholar] [CrossRef] [PubMed]
- Mulvihill, E.; Sborgi, L.; Mari, S.A.; Pfreundschuh, M.; Hiller, S.; Müller, D.J. Mechanism of Membrane Pore Formation by Human Gasdermin-D. EMBO J. 2018, 37, e98321. [Google Scholar] [CrossRef] [PubMed]
- Broz, P.; Pelegrín, P.; Shao, F. The Gasdermins, a Protein Family Executing Cell Death and Inflammation. Nat. Rev. Immunol. 2020, 20, 143–157. [Google Scholar] [CrossRef]
- Ruan, J.; Xia, S.; Liu, X.; Lieberman, J.; Wu, H. Cryo-EM Structure of the Gasdermin A3 Membrane Pore. Nature 2018, 557, 62–67. [Google Scholar] [CrossRef]
- Xia, S. Biological Mechanisms and Therapeutic Relevance of the Gasdermin Family. Mol. Asp. Med. 2020, 76, 100890. [Google Scholar] [CrossRef]
- Lin, P.H.; Lin, H.Y.; Kuo, C.C.; Yang, L.T. N-Terminal Functional Domain of Gasdermin A3 Regulates Mitochondrial Homeostasis via Mitochondrial Targeting. J. Biomed. Sci. 2015, 22, 44. [Google Scholar] [CrossRef]
- Lluis, A.; Schedel, M.; Liu, J.; Illi, S.; Depner, M.; Von Mutius, E.; Kabesch, M.; Schaub, B. Asthma-Associated Polymorphisms in 17q21 Influence Cord Blood ORMDL3 and GSDMA Gene Expression and IL-17 Secretion. J. Allergy Clin. Immunol. 2011, 127, 1587–1594. [Google Scholar] [CrossRef]
- Xia, S.; Ruan, J.; Wu, H. Monitoring Gasdermin Pore Formation in Vitro. Methods Enzymol. 2019, 625, 95–107. [Google Scholar] [CrossRef]
- Li, L.; Li, Y.; Bai, Y. Role of GSDMB in Pyroptosis and Cancer. Cancer Manag. Res. 2020, 12, 3033–3043. [Google Scholar] [CrossRef] [PubMed]
- Orning, P.; Lien, E.; Fitzgerald, K.A. Gasdermins and Their Role in Immunity and Inflammation. J. Exp. Med. 2019, 216, 2453–2465. [Google Scholar] [CrossRef] [PubMed]
- Kayagaki, N.; Stowe, I.B.; Lee, B.L.; O’Rourke, K.; Anderson, K.; Warming, S.; Cuellar, T.; Haley, B.; Roose-Girma, M.; Phung, Q.T.; et al. Caspase-11 Cleaves Gasdermin D for Non-Canonical Inflammasome Signalling. Nature 2015, 526, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, Z.; Ruan, J.; Pan, Y.; Magupalli, V.G.; Wu, H.; Lieberman, J. Inflammasome-Activated Gasdermin D Causes Pyroptosis by Forming Membrane Pores. Nature 2016, 535, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Qu, Z.; Zhou, J.; Zhou, Y.; Xie, Y.; Jiang, Y.; Wu, J.; Luo, Z.; Liu, G.; Yin, L.; Zhang, X.L. Mycobacterial EST12 Activates a RACK1-NLRP3-Gasdermin D Pyroptosis-IL-1β Immune Pathway. Sci. Adv. 2020, 6, eaba4733. [Google Scholar] [CrossRef]
- He, W.T.; Wan, H.; Hu, L.; Chen, P.; Wang, X.; Huang, Z.; Yang, Z.H.; Zhong, C.Q.; Han, J. Gasdermin D Is an Executor of Pyroptosis and Required for Interleukin-1β Secretion. Cell Res. 2015, 25, 1285–1298. [Google Scholar] [CrossRef]
- Sarhan, J.; Liu, B.C.; Muendlein, H.I.; Li, P.; Nilson, R.; Tang, A.Y.; Rongvaux, A.; Bunnell, S.C.; Shao, F.; Green, D.R.; et al. Caspase-8 Induces Cleavage of Gasdermin D to Elicit Pyroptosis during Yersinia Infection. Proc. Natl. Acad. Sci. USA 2018, 115, e10888–e10897. [Google Scholar] [CrossRef]
- Gaidt, M.M.; Hornung, V. Pore Formation by GSDMD Is the Effector Mechanism of Pyroptosis. EMBO J. 2016, 35, 2169. [Google Scholar] [CrossRef]
- Sollberger, G.; Choidas, A.; Burn, G.L.; Habenberger, P.; Di Lucrezia, R.; Kordes, S.; Menninger, S.; Eickhoff, J.; Nussbaumer, P.; Klebl, B.; et al. Gasdermin D Plays a Vital Role in the Generation of Neutrophil Extracellular Traps. Sci. Immunol. 2018, 3, eaar6689. [Google Scholar] [CrossRef]
- Chen, K.W.; Demarco, B.; Broz, P. Beyond Inflammasomes: Emerging Function of Gasdermins during Apoptosis and NETosis. EMBO J. 2020, 39, e103397. [Google Scholar] [CrossRef]
- Kang, R.; Zeng, L.; Zhu, S.; Xie, Y.; Liu, J.; Wen, Q.; Cao, L.; Xie, M.; Ran, Q.; Kroemer, G.; et al. Lipid Peroxidation Drives Gasdermin D-Mediated Pyroptosis in Lethal Polymicrobial Sepsis. Cell Host Microbe 2018, 24, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Rathkey, J.K.; Zhao, J.; Liu, Z.; Chen, Y.; Yang, J.; Kondolf, H.C.; Benson, B.L.; Chirieleison, S.M.; Huang, A.Y.; Dubyak, G.R.; et al. Chemical Disruption of the Pyroptotic Pore-Forming Protein Gasdermin D Inhibits Inflammatory Cell Death and Sepsis. Sci. Immunol. 2018, 3, eaat2738. [Google Scholar] [CrossRef] [PubMed]
- Pandeya, A.; Li, L.; Li, Z.; Wei, Y. Gasdermin D (GSDMD) as a New Target for the Treatment of Infection. MedChemComm 2019, 10, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.; Wu, H.; Kagan, J.C. Gasdermin D Activity in Inflammation and Host Defense. Sci. Immunol. 2019, 4, eaav1447. [Google Scholar] [CrossRef]
- Kambara, H.; Liu, F.; Zhang, X.; Liu, P.; Bajrami, B.; Teng, Y.; Zhao, L.; Zhou, S.; Yu, H.; Zhou, W.; et al. Gasdermin D Exerts Anti-Inflammatory Effects by Promoting Neutrophil Death. Cell Rep. 2018, 22, 2924–2936. [Google Scholar] [CrossRef]
- Tonnus, W.; Linkermann, A. Gasdermin D and Pyroptosis in Acute Kidney Injury. Kidney Int. 2019, 96, 1061–1063. [Google Scholar] [CrossRef]
- Wang, K.; Sun, Z.; Ru, J.; Wang, S.; Huang, L.; Ruan, L.; Lin, X.; Jin, K.; Zhuge, Q.; Yang, S. Ablation of GSDMD Improves Outcome of Ischemic Stroke Through Blocking Canonical and Non-Canonical Inflammasomes Dependent Pyroptosis in Microglia. Front. Neurol. 2020, 11, 577927. [Google Scholar] [CrossRef]
- Hu, J.J.; Liu, X.; Xia, S.; Zhang, Z.; Zhang, Y.; Zhao, J.; Ruan, J.; Luo, X.; Lou, X.; Bai, Y.; et al. FDA-Approved Disulfiram Inhibits Pyroptosis by Blocking Gasdermin D Pore Formation. Nat. Immunol. 2020, 21, 736–745. [Google Scholar] [CrossRef]
- Ye, B.; Chen, X.; Dai, S.; Han, J.; Liang, X.; Lin, S.; Cai, X.; Huang, Z.; Huang, W. Emodin Alleviates Myocardial Ischemia/Reperfusion Injury by Inhibiting Gasdermin D-Mediated Pyroptosis in Cardiomyocytes. Drug Des. Devel Ther. 2019, 13, 990. [Google Scholar] [CrossRef]
- Rogers, C.; Erkes, D.A.; Nardone, A.; Aplin, A.E.; Fernandes-Alnemri, T.; Alnemri, E.S. Gasdermin Pores Permeabilize Mitochondria to Augment Caspase-3 Activation during Apoptosis and Inflammasome Activation. Nat. Commun. 2019, 10, 1689. [Google Scholar] [CrossRef]
- Defourny, J.; Aghaie, A.; Perfettini, I.; Avan, P.; Delmaghani, S.; Petit, C. Pejvakin-Mediated Pexophagy Protects Auditory Hair Cells against Noise-Induced Damage. Proc. Natl. Acad. Sci. USA 2019, 116, 8010–8017. [Google Scholar] [CrossRef] [PubMed]
- Galluzzi, L.; Vitale, I.; Aaronson, S.A.; Abrams, J.M.; Adam, D.; Agostinis, P.; Alnemri, E.S.; Altucci, L.; Amelio, I.; Andrews, D.W.; et al. Molecular mechanisms of cell death: Recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018, 25, 486–541. [Google Scholar] [CrossRef] [PubMed]
- Burdette, B.E.; Esparza, A.N.; Zhu, H.; Wang, S. Gasdermin D in Pyroptosis. Acta Pharm. Sin. B 2021, 11, 2768–2782. [Google Scholar] [CrossRef]
- Aglietti, R.A.; Dueber, E.C. Recent Insights into the Molecular Mechanisms Underlying Pyroptosis and Gasdermin Family Functions. Trends Immunol. 2017, 38, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Kita, H. Gasdermin D Pores for IL-33 Release. Nat. Immunol. 2022, 23, 989–991. [Google Scholar] [CrossRef]
- Tan, G.; Huang, C.; Chen, J.; Chen, B.; Zhi, F. Gasdermin-E-Mediated Pyroptosis Participates in the Pathogenesis of Crohn’s Disease by Promoting Intestinal Inflammation. Cell Rep. 2021, 35, 109265. [Google Scholar] [CrossRef]
- Hooftman, A.; Angiari, S.; Hester, S.; Corcoran, S.E.; Runtsch, M.C.; Ling, C.; Ruzek, M.C.; Slivka, P.F.; McGettrick, A.F.; Banahan, K.; et al. The Immunomodulatory Metabolite Itaconate Modifies NLRP3 and Inhibits Inflammasome Activation. Cell Metab. 2020, 32, 468–478. [Google Scholar] [CrossRef]
- Yang, S.; Zhang, X.; Zhang, H.; Lin, X.; Chen, X.; Zhang, Y.; Lin, X.; Huang, L.; Zhuge, Q. Dimethyl Itaconate Inhibits LPS-induced Microglia Inflammation and Inflammasome-mediated Pyroptosis via Inducing Autophagy and Regulating the Nrf-2/HO-1 Signaling Pathway. Mol. Med. Rep. 2021, 24, 672. [Google Scholar] [CrossRef]
- Hoyle, C.; Green, J.P.; Allan, S.M.; Brough, D.; Lemarchand, E. Itaconate and Fumarate Derivatives Inhibit Priming and Activation of the Canonical NLRP3 Inflammasome in Macrophages. Immunology 2022, 165, 460–480. [Google Scholar] [CrossRef]
- Humphries, F.; Shmuel-Galia, L.; Ketelut-Carneiro, N.; Li, S.; Wang, B.; Nemmara, V.V.; Wilson, R.; Jiang, Z.; Khalighinejad, F.; Muneeruddin, K.; et al. Succination Inactivates Gasdermin D and Blocks Pyroptosis. Science 2020, 369, 1633–1637. [Google Scholar] [CrossRef]
- Shi, F.-L.; Ni, S.-T.; Luo, S.-Q.; Hu, B.; Xu, R.; Liu, S.-Y.; Huang, X.-D.; Zeng, B.; Liang, Q.-Q.; Chen, S.-Y.; et al. Dimethyl Fumarate Ameliorates Autoimmune Hepatitis in Mice by Blocking NLRP3 Inflammasome Activation. Int. Immunopharmacol. 2022, 108, 108867. [Google Scholar] [CrossRef]
- Wang, N.; Kong, R.; Han, W.; Bao, W.; Shi, Y.; Ye, L.P.; Lu, J. Honokiol Alleviates Ulcerative Colitis by Targeting PPAR-γ-TLR4-NF-ΚB Signaling and Suppressing Gasdermin-D-Mediated Pyroptosis in Vivo and in Vitro. Int. Immunopharmacol. 2022, 111, 109058. [Google Scholar] [CrossRef]
- Wu, L.; Chen, M.; Li, M.; Wang, Y.; Li, Y.; Zheng, L.; Ke, Z.; Liu, K.; Qiao, Y.; Shi, X. Oridonin Alleviates Kanamycin-Related Hearing Loss by Inhibiting NLRP3/Caspase-1/Gasdermin D-Induced Inflammasome Activation and Hair Cell Pyroptosis. Mol. Immunol. 2022, 149, 66–76. [Google Scholar] [CrossRef]
- Boots, A.W.; Haenen, G.R.M.M.; Bast, A. Health Effects of Quercetin: From Antioxidant to Nutraceutical. Eur. J. Pharmacol. 2008, 585, 325–337. [Google Scholar] [CrossRef]
- Zhao, X.; Wang, C.; Dai, S.; Liu, Y.; Zhang, F.; Peng, C.; Li, Y. Quercetin Protects Ethanol-Induced Hepatocyte Pyroptosis via Scavenging Mitochondrial ROS and Promoting PGC-1 α-Regulated Mitochondrial Homeostasis in L02 Cells. Oxid. Med. Cell Longev. 2022, 2022, 4591134. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Weng, X.; Bao, X.; Bai, X.; Lv, Y.; Zhang, S.; Chen, Y.; Zhao, C.; Zeng, M.; Huang, J.; et al. A Novel Anti-Atherosclerotic Mechanism of Quercetin: Competitive Binding to KEAP1 via Arg483 to Inhibit Macrophage Pyroptosis. Redox Biol. 2022, 57, 102511. [Google Scholar] [CrossRef] [PubMed]
- Jia, C.; Chen, H.; Zhang, J.; Zhou, K.; Zhuge, Y.; Niu, C.; Qiu, J.; Rong, X.; Shi, Z.; Xiao, J.; et al. Role of Pyroptosis in Cardiovascular Diseases. Int. Immunopharmacol. 2019, 67, 311–318. [Google Scholar] [CrossRef]
- Ji, N.; Qi, Z.; Wang, Y.; Yang, X.; Yan, Z.; Li, M.; Ge, Q.; Zhang, J. Pyroptosis: A New Regulating Mechanism in Cardiovascular Disease. J. Inflamm. Res. 2021, 14, 2647–2666. [Google Scholar] [CrossRef] [PubMed]
- De Miguel, C.; Pelegrín, P.; Baroja-Mazo, A.; Cuevas, S. Emerging Role of the Inflammasome and Pyroptosis in Hypertension. Int. J. Mol. Sci. 2021, 22, 1064. [Google Scholar] [CrossRef]
- Gao, Y.; Shi, H.; Dong, Z.; Zhang, F.; Sun, A.; Ge, J. Current Knowledge of Pyroptosis in Heart Diseases. J. Mol. Cell Cardiol. 2022, 171, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Tian, P.-C.; Wang, K.; Wang, M.; Wang, K. Pyroptosis: Role and Mechanisms in Cardiovascular Disease. Front. Cardiovasc. Med. 2022, 9, 897815. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Antonio, I.; López-Sánchez, G.N.; Uribe, M.; Chávez-Tapia, N.C.; Nuño-Lámbarri, N. Role of the Inflammasome, Gasdermin D, and Pyroptosis in Non-Alcoholic Fatty Liver Disease. J. Gastroenterol. Hepatol. 2021, 36, 2720–2727. [Google Scholar] [CrossRef]
- Hurtado-Navarro, L.; Angosto-Bazarra, D.; Pelegrín, P.; Baroja-Mazo, A.; Cuevas, S. NLRP3 Inflammasome and Pyroptosis in Liver Pathophysiology: The Emerging Relevance of Nrf2 Inducers. Antioxidants 2022, 11, 870. [Google Scholar] [CrossRef] [PubMed]
- Ju, X.; Yang, Z.; Zhang, H.; Wang, Q. Role of Pyroptosis in Cancer Cells and Clinical Applications. Biochimie 2021, 185, 78–86. [Google Scholar] [CrossRef]
- Tan, Y.; Chen, Q.; Li, X.; Zeng, Z.; Xiong, W.; Li, G.; Li, X.; Yang, J.; Xiang, B.; Yi, M. Pyroptosis: A New Paradigm of Cell Death for Fighting against Cancer. J. Exp. Clin. Cancer Res. 2021, 40, 153. [Google Scholar] [CrossRef]
- Lu, X.; Guo, T.; Zhang, X. Pyroptosis in Cancer: Friend or Foe? Cancers 2021, 13, 3620. [Google Scholar] [CrossRef]
- Xia, X.; Wang, X.; Cheng, Z.; Qin, W.; Lei, L.; Jiang, J.; Hu, J. The Role of Pyroptosis in Cancer: Pro-Cancer or pro-“host”? Cell Death Dis. 2019, 10, 650. [Google Scholar] [CrossRef]
- McKenzie, B.A.; Dixit, V.M.; Power, C. Fiery Cell Death: Pyroptosis in the Central Nervous System. Trends Neurosci. 2020, 43, 55–73. [Google Scholar] [CrossRef]
- Wan, T.; Li, X.; Fu, M.; Gao, X.; Li, P.; Guo, W. NLRP3-Dependent Pyroptosis: A Candidate Therapeutic Target for Depression. Front. Cell Neurosci. 2022, 16, 863426. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, B.; Li, S.; Yang, S. Pyroptosis, and Its Role in Central Nervous System Disease. J. Mol. Biol. 2022, 434, 167379. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Sun, X.; Liu, S.; Tang, Y.; Shi, Y.; Bai, Y.; Wang, Y.; Yang, Q.; Yang, Q.; Jiang, W.; et al. Caspase-11-Gasdermin D-Mediated Pyroptosis Is Involved in the Pathogenesis of Atherosclerosis. Front. Pharmacol. 2021, 12, 657486. [Google Scholar] [CrossRef]
- Qian, Z.; Zhao, Y.; Wan, C.; Deng, Y.; Zhuang, Y.; Xu, Y.; Zhu, Y.; Lu, S.; Bao, Z. Pyroptosis in the Initiation and Progression of Atherosclerosis. Front. Pharmacol. 2021, 12, 652963. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yao, J.; Liu, Y.; Huang, L. Targeting the Gasdermin D as a Strategy for Ischemic Stroke Therapy. Biochem. Pharmacol. 2021, 188, 114585. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; Jin, Z.; Lv, X.; Zheng, Z.; Gao, H.; Deng, Y.; Liu, Y.; Chen, L.; Wang, W.; He, J.; et al. Hydroxytyrosol Acetate Inhibits Vascular Endothelial Cell Pyroptosis via the HDAC11 Signaling Pathway in Atherosclerosis. Front. Pharmacol. 2021, 12, 656272. [Google Scholar] [CrossRef] [PubMed]
- Cuevas, S.; Pelegrín, P. Pyroptosis and Redox Balance in Kidney Diseases. Antioxid. Redox Signal 2021, 35, 40–60. [Google Scholar] [CrossRef]
- Zhang, K.J.; Wu, Q.; Jiang, S.M.; Ding, L.; Liu, C.X.; Xu, M.; Wang, Y.; Zhou, Y.; Li, L. Pyroptosis: A New Frontier in Kidney Diseases. Oxid. Med. Cell Longev. 2021, 2021, 6686617. [Google Scholar] [CrossRef]
- Ferreira, A.C.; Soares, V.C.; de Azevedo-Quintanilha, I.G.; Dias, S.D.S.G.; Fintelman-Rodrigues, N.; Sacramento, C.Q.; Mattos, M.; de Freitas, C.S.; Temerozo, J.R.; Teixeira, L.; et al. SARS-CoV-2 Engages Inflammasome and Pyroptosis in Human Primary Monocytes. Cell Death Discov. 2021, 7, 43. [Google Scholar] [CrossRef]
- Ma, J.; Zhu, F.; Zhao, M.; Shao, F.; Yu, D.; Ma, J.; Zhang, X.; Li, W.; Qian, Y.; Zhang, Y.; et al. SARS-CoV-2 Nucleocapsid Suppresses Host Pyroptosis by Blocking Gasdermin D Cleavage. EMBO J. 2021, 40, e108249. [Google Scholar] [CrossRef]
- Bittner, Z.A.; Schrader, M.; George, S.E.; Amann, R. Pyroptosis and Its Role in SARS-CoV-2 Infection. Cells 2022, 11, 1717. [Google Scholar] [CrossRef]
- Mamun, A.A.; Wu, Y.; Nasrin, F.; Akter, A.; Taniya, M.A.; Munir, F.; Jia, C.; Xiao, J. Role of Pyroptosis in Diabetes and Its Therapeutic Implications. J. Inflamm. Res. 2021, 14, 2187–2206. [Google Scholar] [CrossRef] [PubMed]
- Coll, R.C.; Schroder, K.; Pelegrín, P. NLRP3 and Pyroptosis Blockers for Treating Inflammatory Diseases. Trends Pharmacol. Sci. 2022, 43, 653–668. [Google Scholar] [CrossRef] [PubMed]
- Rao, Z.; Zhu, Y.; Yang, P.; Chen, Z.; Xia, Y.; Qiao, C.; Liu, W.; Deng, H.; Li, J.; Ning, P.; et al. Pyroptosis in Inflammatory Diseases and Cancer. Theranostics 2022, 12, 4310–4329. [Google Scholar] [CrossRef]
- Feng, Y.; Li, M.; Yangzhong, X.; Zhang, X.; Zu, A.; Hou, Y.; Li, L.; Sun, S. Pyroptosis in Inflammation-Related Respiratory Disease. J. Physiol. Biochem. 2022, 78, 721–737. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Fan, G.; Tao, N.; Sun, T. Role of Pyroptosis in Respiratory Diseases and Its Therapeutic Potential. J. Inflamm. Res. 2022, 15, 2033–2050. [Google Scholar] [CrossRef]
- Zhang, S.; Liang, Y.; Yao, J.; Li, D.F.; Wang, L.S. Role of Pyroptosis in Inflammatory Bowel Disease (IBD): From Gasdermins to DAMPs. Front. Pharmacol. 2022, 13, 833588. [Google Scholar] [CrossRef]
- Strzyz, P. The Healing Role of Gasdermin B in IBD. Nat. Rev. Mol. Cell Biol. 2022, 23, 167. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Z.; Yang, F.; Xu, W.; Han, J.; Luo, G.; Li, Y.; Zhuang, J.; Jie, H.; Li, X.; Shi, X.; et al. Attenuation of Rheumatoid Arthritis Through the Inhibition of Tumor Necrosis Factor–Induced Caspase 3/Gasdermin E–Mediated Pyroptosis. Arthritis Rheumatol. 2022, 74, 427–440. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Shi, L.Y.; Xu, M.H.; Jing, Y.; Sun, C.C.; Yang, J.H.; Wang, R.N.; Sheng, N.N.; Zhang, C.F.; Zhang, L.; et al. A Pan-Cancer Analysis of the Expression of Gasdermin Genes in Tumors and Their Relationship with the Immune Microenvironment. Transl. Cancer Res. 2021, 10, 4125–4147. [Google Scholar] [CrossRef]
- Sarrió, D.; Martínez-Val, J.; Molina-Crespo, Á.; Sánchez, L.; Moreno-Bueno, G. The Multifaceted Roles of Gasdermins in Cancer Biology and Oncologic Therapies. Biochim. Biophys. Acta Rev. Cancer 2021, 1876, 188635. [Google Scholar] [CrossRef]
- Mu, M.; Yu, Q.; Zhang, Q.; Guo, J.; Wang, X.; Sun, X.; Yu, J. A Pan-Cancer Analysis of Molecular Characteristics and Oncogenic Role of Gasdermins. Cancer Cell Int. 2022, 22, 80. [Google Scholar] [CrossRef]
- Magnani, L.; Colantuoni, M.; Mortellaro, A. Gasdermins: New Therapeutic Targets in Host Defense, Inflammatory Diseases, and Cancer. Front. Immunol. 2022, 13, 898298. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zhang, L.; Sun, Z. Eliciting Pyroptosis to Fuel Cancer Immunotherapy: Mechanisms and Strategies. Cancer Biol. Med. 2022, 19, 948–964. [Google Scholar] [CrossRef]
- Huo, C.L.; Deng, Y.; Sun, Z.G. A Comprehensive Analysis of Gasdermin Family Gene as Therapeutic Targets in Pan-Cancer. Sci. Rep. 2022, 12, 13329. [Google Scholar] [CrossRef]
- Nadeem, S.; Chen, Z.; Wei, M.; Li, F.; Ling, D. Nanomedicine-Induced Pyroptosis for Cancer Therapy. Nanomedicine 2021, 16, 1071–1074. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, J.W.; Huang, J.; Tang, L.; Xu, Y.H.; Sun, H.; Tang, J.; Wang, G. Pyroptosis, a Target for Cancer Treatment? Apoptosis 2022, 27, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Bettadapura, S.N.; Smeltzer, M.S.; Zhu, H.; Wang, S. Pyroptosis and Pyroptosis-Inducing Cancer Drugs. Acta Pharmacol. Sin. 2022, 43, 2462–2473. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Yue, P.; Dickinson, C.F.; Yang, J.K.; Datanagan, K.; Zhai, N.; Zhang, Y.; Miklossy, G.; Lopez-Tapia, F.; Tius, M.A.; et al. Natural Product Preferentially Targets Redox and Metabolic Adaptations and Aberrantly Active STAT3 to Inhibit Breast Tumor Growth in Vivo. Cell Death Dis. 2022, 13, 1022. [Google Scholar] [CrossRef]
- Yue, E.; Tuguzbaeva, G.; Chen, X.; Qin, Y.; Li, A.; Sun, X.; Dong, C.; Liu, Y.; Yu, Y.; Zahra, S.M.; et al. Anthocyanin Is Involved in the Activation of Pyroptosis in Oral Squamous Cell Carcinoma. Phytomedicine 2019, 56, 286–294. [Google Scholar] [CrossRef]
- Kong, Y.; Feng, Z.; Chen, A.; Qi, Q.; Han, M.; Wang, S.; Zhang, Y.; Zhang, X.; Yang, N.; Wang, J.; et al. The Natural Flavonoid Galangin Elicits Apoptosis, Pyroptosis, and Autophagy in Glioblastoma. Front. Oncol. 2019, 9, 942. [Google Scholar] [CrossRef]
- Wang, L.; Li, K.; Lin, X.; Yao, Z.; Wang, S.; Xiong, X.; Ning, Z.; Wang, J.; Xu, X.; Jiang, Y.; et al. Metformin Induces Human Esophageal Carcinoma Cell Pyroptosis by Targeting the MiR-497/PELP1 Axis. Cancer Lett. 2019, 450, 22–31. [Google Scholar] [CrossRef]
- Erkes, D.A.; Cai, W.; Sanchez, I.M.; Purwin, T.J.; Rogers, C.; Field, C.O.; Berger, A.C.; Hartsough, E.J.; Rodeck, U.; Alnemri, E.S.; et al. Mutant BRAF and MEK Inhibitors Regulate the Tumor Immune Microenvironment via Pyroptosis. Cancer Discov. 2020, 10, 254. [Google Scholar] [CrossRef]
- Gallorini, M.; Di Valerio, V.; Bruno, I.; Carradori, S.; Amoroso, R.; Cataldi, A.; Ammazzalorso, A. Phenylsulfonimide PPARα Antagonists Enhance Nrf2 Activation and Promote Oxidative Stress-Induced Apoptosis/Pyroptosis in MCF7 Breast Cancer Cells. Int. J. Mol. Sci. 2023, 24, 1316. [Google Scholar] [CrossRef] [PubMed]
- Hergueta-Redondo, M.; Sarrio, D.; Molina-Crespo, Á.; Vicario, R.; Bernadó-Morales, C.; Martínez, L.; Rojo-Sebastián, A.; Serra-Musach, J.; Mota, A.; Martínez-Ramírez, Á.; et al. Gasdermin B Expression Predicts Poor Clinical Outcome in HER2-Positive Breast Cancer. Oncotarget 2016, 7, 56295–56308. [Google Scholar] [CrossRef] [PubMed]
- Molina-Crespo, Á.; Cadete, A.; Sarrio, D.; Gámez-Chiachio, M.; Martinez, L.; Chao, K.; Olivera, A.; Gonella, A.; Díaz, E.; Palacios, J.; et al. Intracellular Delivery of an Antibody Targeting Gasdermin-B Reduces HER2 Breast Cancer Aggressiveness. Clin. Cancer Res. 2019, 25, 4846–4858. [Google Scholar] [CrossRef] [PubMed]
- Miguchi, M.; Hinoi, T.; Shimomura, M.; Adachi, T.; Saito, Y.; Niitsu, H.; Kochi, M.; Sada, H.; Sotomaru, Y.; Ikenoue, T.; et al. Gasdermin C Is Upregulated by Inactivation of Transforming Growth Factor β Receptor Type II in the Presence of Mutated Apc, Promoting Colorectal Cancer Proliferation. PLoS ONE 2016, 11, e0166422. [Google Scholar] [CrossRef]
- Wei, J.; Xu, Z.; Chen, X.; Wang, X.; Zeng, S.; Qian, L.; Yang, X.; Ou, C.; Lin, W.; Gong, Z.; et al. Overexpression of GSDMC Is a Prognostic Factor for Predicting a Poor Outcome in Lung Adenocarcinoma. Mol. Med. Rep. 2020, 21, 360–370. [Google Scholar] [CrossRef]
- Hou, J.; Zhao, R.; Xia, W.; Chang, C.W.; You, Y.; Hsu, J.M.; Nie, L.; Chen, Y.; Wang, Y.C.; Liu, C.; et al. PD-L1-Mediated Gasdermin C Expression Switches Apoptosis to Pyroptosis in Cancer Cells and Facilitates Tumour Necrosis. Nat. Cell Biol. 2020, 22, 1264–1275. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Zhou, B.; Sun, R.Y.; Ai, Y.L.; Cheng, K.; Li, F.N.; Wang, B.R.; Liu, F.J.; Jiang, Z.H.; Wang, W.J.; et al. The Metabolite α-KG Induces GSDMC-Dependent Pyroptosis through Death Receptor 6-Activated Caspase-8. Cell Res. 2021, 31, 980–997. [Google Scholar] [CrossRef]
- Wang, W.J.; Chen, D.; Jiang, M.Z.; Bing, X.U.; Li, X.W.; Chu, Y.; Zhang, Y.J.; Mao, R.; Liang, J.; Fan, D.M. Downregulation of Gasdermin D Promotes Gastric Cancer Proliferation by Regulating Cell Cycle-Related Proteins. J. Dig. Dis. 2018, 19, 74–83. [Google Scholar] [CrossRef]
- Gao, J.; Qiu, X.; Xi, G.; Liu, H.; Zhang, F.; Lv, T.; Song, Y. Downregulation of GSDMD Attenuates Tumor Proliferation via the Intrinsic Mitochondrial Apoptotic Pathway and Inhibition of EGFR/Akt Signaling and Predicts a Good Prognosis in Non-small Cell Lung Cancer. Oncol. Rep. 2018, 40, 1971–1984. [Google Scholar] [CrossRef]
- Shen, X.; Zhang, Q.; He, Z.; Xiao, S.; Li, H.; Huang, Z. Overexpression of Gasdermin D Promotes Invasion of Adenoid Cystic Carcinoma. Int. J. Clin. Exp. Pathol. 2020, 13, 1811. [Google Scholar]
- Xi, G.; Gao, J.; Wan, B.; Zhan, P.; Xu, W.; Lv, T.; Song, Y. GSDMD Is Required for Effector CD8+ T Cell Responses to Lung Cancer Cells. Int. Immunopharmacol. 2019, 74, 105713. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Yang, Y.; Hu, Y.; Yang, R.; Huang, J.; Liu, Y.; Wu, Y.; Li, S.; Ma, C.; Humphries, F.; et al. Gasdermin D Restricts Anti-Tumor Immunity during PD-L1 Checkpoint Blockade. Cell Rep. 2022, 41, 111553. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Xiang, J.; Huang, Z.; Wang, L.; Huang, Y. Trichosanthin Inhibits Cell Growth and Metastasis by Promoting Pyroptosis in Non-Small Cell Lung Cancer. J. Thorac. Dis. 2022, 14, 1193–1202. [Google Scholar] [CrossRef]
- Chen, T.; Wang, Z.; Zhong, J.; Zhang, L.; Zhang, H.; Zhang, D.; Xu, X.; Zhong, X.; Wang, J.; Li, H. Secoisolariciresinol Diglucoside Induces Pyroptosis by Activating Caspase-1 to Cleave GSDMD in Colorectal Cancer Cells. Drug Dev. Res. 2022, 83, 1152–1166. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Y.; Xia, S.; Kong, Q.; Li, S.; Liu, X.; Junqueira, C.; Meza-Sosa, K.F.; Mok, T.M.Y.; Ansara, J.; et al. Gasdermin E Suppresses Tumour Growth by Activating Anti-Tumour Immunity. Nature 2020, 579, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Gao, W.; Shi, X.; Ding, J.; Liu, W.; He, H.; Wang, K.; Shao, F. Chemotherapy Drugs Induce Pyroptosis through Caspase-3 Cleavage of a Gasdermin. Nature 2017, 547, 99–103. [Google Scholar] [CrossRef]
- Li, F.; Xia, Q.; Ren, L.; Nie, Y.; Ren, H.; Guo, X.; Yu, J.; Xing, Y.; Chen, Z. GSDME Increases Chemotherapeutic Drug Sensitivity by Inducing Pyroptosis in Retinoblastoma Cells. Oxid. Med. Cell Longev. 2022, 2022, 2371807. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.F.; Gong, Y.X.; Li, H.F.; Sun, F.L.; Li, W.L.; Chen, D.Q.; Xie, D.P.; Ren, C.X.; Guo, X.Y.; Wang, Z.Y.; et al. Curcumin Activates ROS Signaling to Promote Pyroptosis in Hepatocellular Carcinoma HepG2 Cells. In Vivo 2021, 35, 249–257. [Google Scholar] [CrossRef]
- Sun, X.; Zhong, X.; Ma, W.; Feng, W.; Huang, Q.; Ma, M.; Lv, M.; Hu, R.; Han, Z.; Li, J.; et al. Germacrone Induces Caspase-3/GSDME Activation and Enhances ROS Production, Causing HepG2 Pyroptosis. Exp. Ther. Med. 2022, 24, 456. [Google Scholar] [CrossRef]
- Li, T.; Shi, L.; Liu, W.; Hu, X.; Hui, Y.; Di, M.; Xue, S.; Zheng, Y.; Yao, M.; Li, C.; et al. Aloe-Emodin Induces Mitochondrial Dysfunction and Pyroptosis by Activation of the Caspase-9/3/Gasdermin E Axis in HeLa Cells. Front. Pharmacol. 2022, 13, 854526. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, J.; De Schutter, E.; Op de Beeck, K. GSDME: A Potential Ally in Cancer Detection and Treatment. Trends Cancer 2021, 7, 392–394. [Google Scholar] [CrossRef]
- Jiang, H.; Niu, C.; Guo, Y.; Liu, Z.; Jiang, Y. Wedelolactone Induces Apoptosis and Pyroptosis in Retinoblastoma through Promoting ROS Generation. Int. Immunopharmacol. 2022, 111, 108855. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, W.; Li, A.; Huang, W.; Chen, S.; Han, F.; Wang, L. Dihydroartemisinin Induces Pyroptosis by Promoting the AIM2/Caspase-3/DFNA5 Axis in Breast Cancer Cells. Chem. Biol. Interact. 2021, 340, 109434. [Google Scholar] [CrossRef]
- Kobayashi, T.; Mitsuhashi, A.; Hongying, P.; Shioya, M.; Kojima, K.; Nishikimi, K.; Yahiro, K.; Shozu, M. Bexarotene-Induced Cell Death in Ovarian Cancer Cells through Caspase-4-Gasdermin E Mediated Pyroptosis. Sci. Rep. 2022, 12, 11123. [Google Scholar] [CrossRef]
- Xia, Y.; Jin, Y.; Cui, D.; Wu, X.; Song, C.; Jin, W.; Huang, H. Antitumor Effect of Simvastatin in Combination With DNA Methyltransferase Inhibitor on Gastric Cancer via GSDME-Mediated Pyroptosis. Front. Pharmacol. 2022, 13, 860546. [Google Scholar] [CrossRef]
- Tan, G.; Huang, C.; Chen, J.; Zhi, F. HMGB1 Released from GSDME-Mediated Pyroptotic Epithelial Cells Participates in the Tumorigenesis of Colitis-Associated Colorectal Cancer through the ERK1/2 Pathway. J. Hematol. Oncol. 2020, 13, 149. [Google Scholar] [CrossRef]
- De Schutter, E.; Croes, L.; Ibrahim, J.; Pauwels, P.; Op de Beeck, K.; Vandenabeele, P.; Van Camp, G. GSDME and Its Role in Cancer: From behind the Scenes to the Front of the Stage. Int. J. Cancer 2021, 148, 2872–2883. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhao, S.; Yang, H.; Chen, Y.; Feng, H.; An, M.; Chen, B. Prognostic and Immunological Role of Gasdermin E in Pan-Cancer Analysis. Front. Oncol. 2021, 11, 706266. [Google Scholar] [CrossRef] [PubMed]
- Brunello, L. Gasdermin E Shields PDAC. Nat. Rev. Cancer 2022, 22, 319. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.; Xu, J.; Zhang, B.; Liu, J.; Liang, C.; Hua, J.; Meng, Q.; Yu, X.; Shi, S. Ferroptosis, Necroptosis, and Pyroptosis in Anticancer Immunity. J. Hematol. Oncol. 2020, 13, 110. [Google Scholar] [CrossRef] [PubMed]
- The Effect and Mechanism of LncRNA NBR2 Regulating Endothelial Pyroptosis by Targeting GSDMD in Sepsis. Available online: https://clinicaltrials.gov/ct2/show/NCT04427371?term=pyroptosis%2C+gasdermin&draw=2&rank=1 (accessed on 31 May 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allali-Boumara, I.; Marrero, A.D.; Quesada, A.R.; Martínez-Poveda, B.; Medina, M.Á. Pyroptosis Modulators: New Insights of Gasdermins in Health and Disease. Antioxidants 2023, 12, 1551. https://doi.org/10.3390/antiox12081551
Allali-Boumara I, Marrero AD, Quesada AR, Martínez-Poveda B, Medina MÁ. Pyroptosis Modulators: New Insights of Gasdermins in Health and Disease. Antioxidants. 2023; 12(8):1551. https://doi.org/10.3390/antiox12081551
Chicago/Turabian StyleAllali-Boumara, Imane, Ana Dácil Marrero, Ana R. Quesada, Beatriz Martínez-Poveda, and Miguel Ángel Medina. 2023. "Pyroptosis Modulators: New Insights of Gasdermins in Health and Disease" Antioxidants 12, no. 8: 1551. https://doi.org/10.3390/antiox12081551
APA StyleAllali-Boumara, I., Marrero, A. D., Quesada, A. R., Martínez-Poveda, B., & Medina, M. Á. (2023). Pyroptosis Modulators: New Insights of Gasdermins in Health and Disease. Antioxidants, 12(8), 1551. https://doi.org/10.3390/antiox12081551







