Role of Enzymic Antioxidants in Mediating Oxidative Stress and Contrasting Wound Healing Capabilities in Oral Mucosal/Skin Fibroblasts and Tissues
Abstract
1. Introduction
2. Materials and Methods
2.1. Oral Mucosal and Skin Fibroblasts and Tissues
2.2. Oxidative Stress Biomarker and Enzymic Antioxidant Immunohistochemistry
2.3. Oral Mucosal and Patient-Matched Skin Fibroblast Cultures
2.4. Determination of Endogenous Reactive Oxygen Species (ROS) Generation
2.5. Oxidative DNA Biomarker Detection
2.6. Oxidative Protein Biomarker Detection
2.7. Microarray Analysis of Enzymic Antioxidant Gene Expression
2.8. Validation of Cellular Superoxide Dismutase 3 (SOD3) Expression Levels
2.9. Validation of Cellular Superoxide Dismutase 3 (SOD3) Protein Levels
2.10. Quantification of Total Cellular Superoxide Dismutase (SOD) Activities
2.11. Statistical Analysis
3. Results
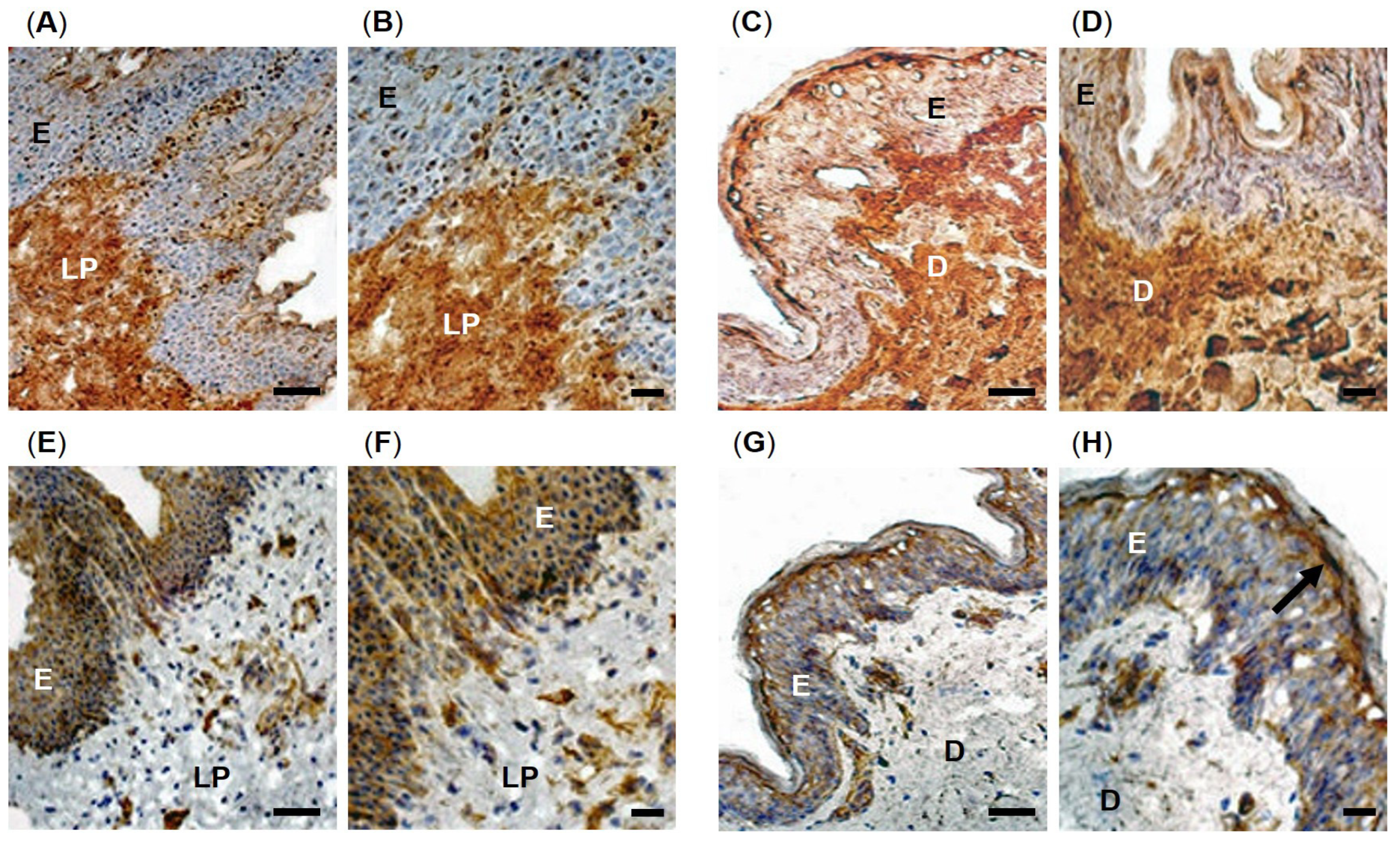
3.1. Oxidative Stress Biomarker Detection in Oral Mucosal and Skin Tissues
3.2. Enzymic Antioxidant Detection in Oral Mucosal and Skin Tissues
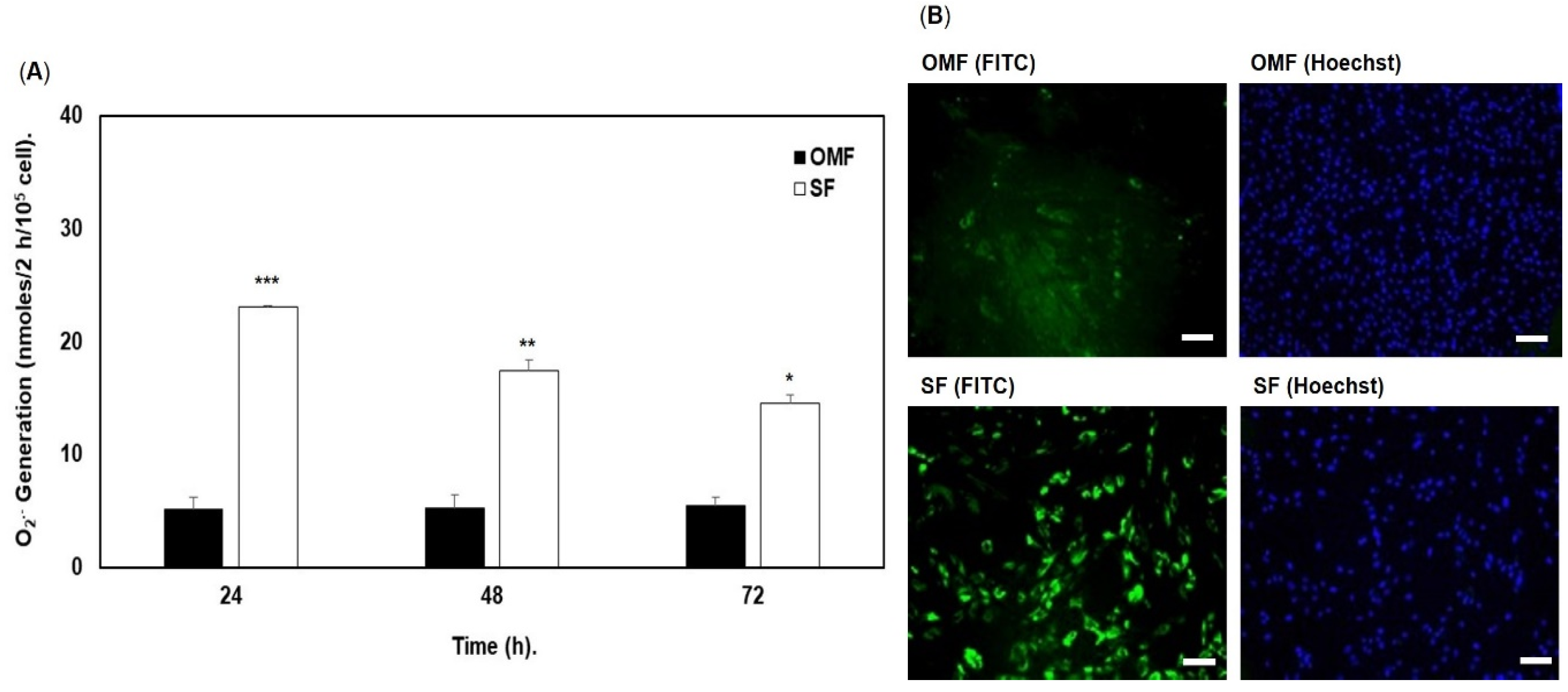
3.3. Endogenous Reactive Oxygen Species (ROS) Generation by Oral Mucosal and Skin Fibroblasts
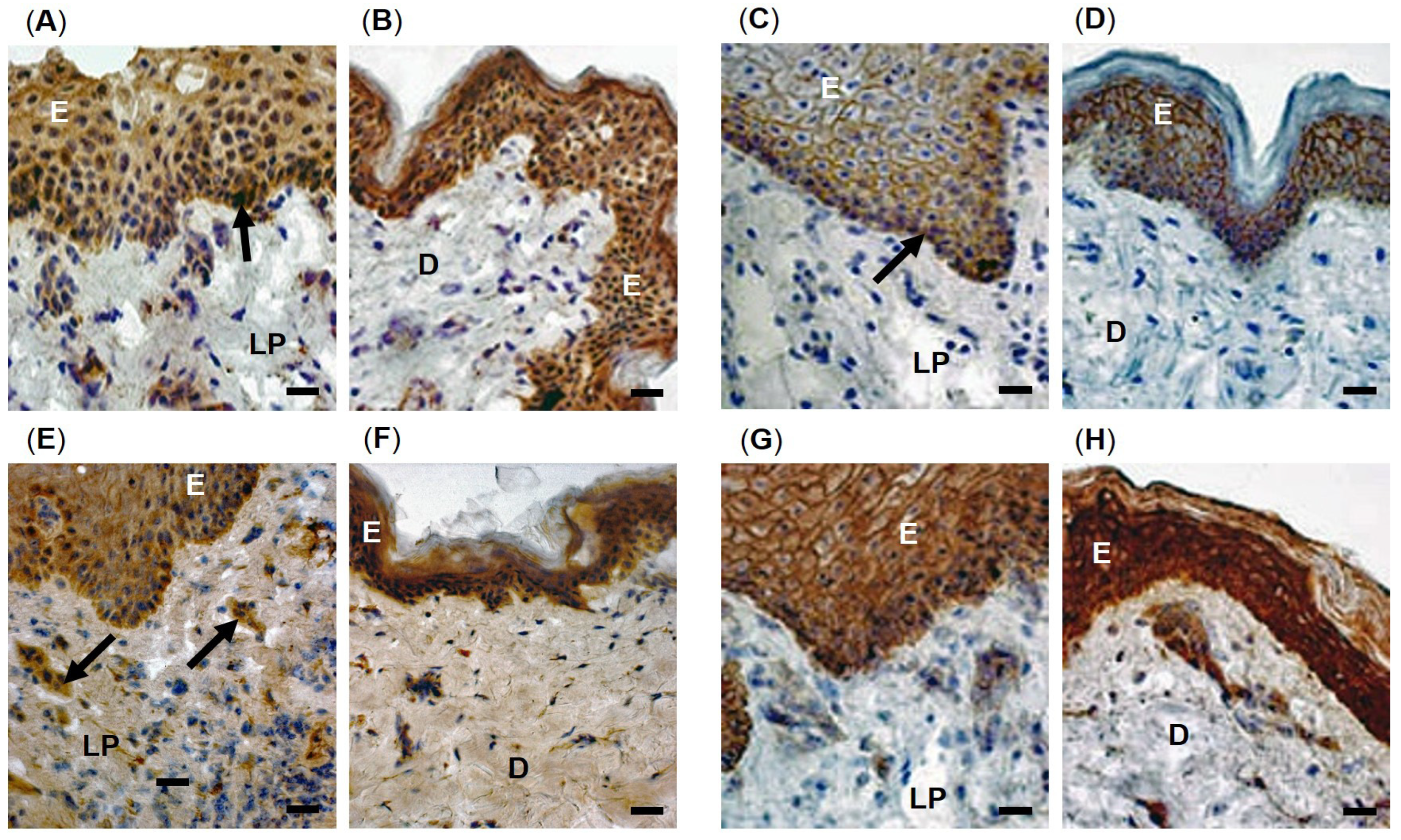
3.4. Oxidative Stress Biomarker Detection in Oral Mucosal and Skin Fibroblasts
3.5. Enzymic Antioxidant Gene Expression Analysis
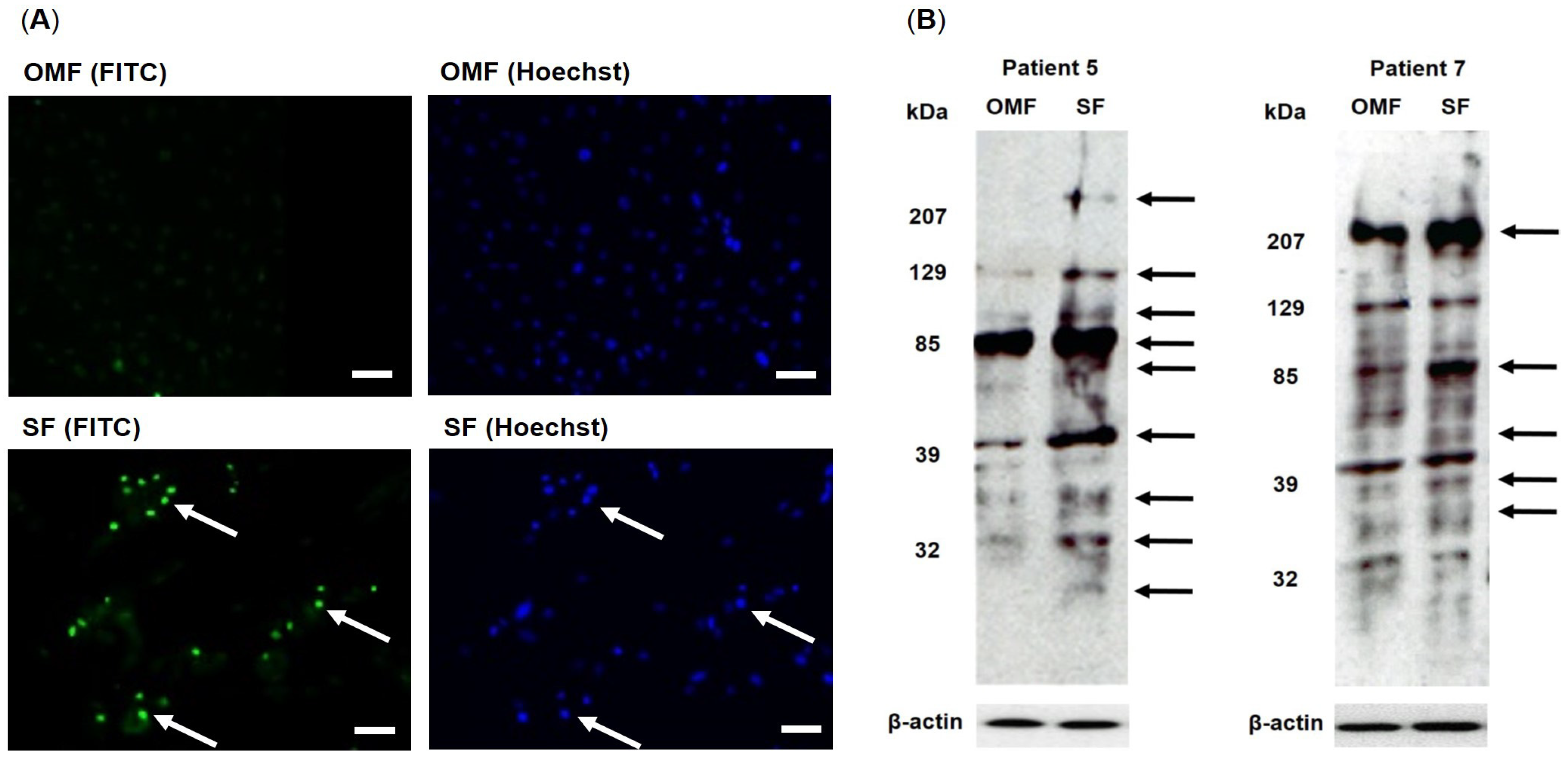
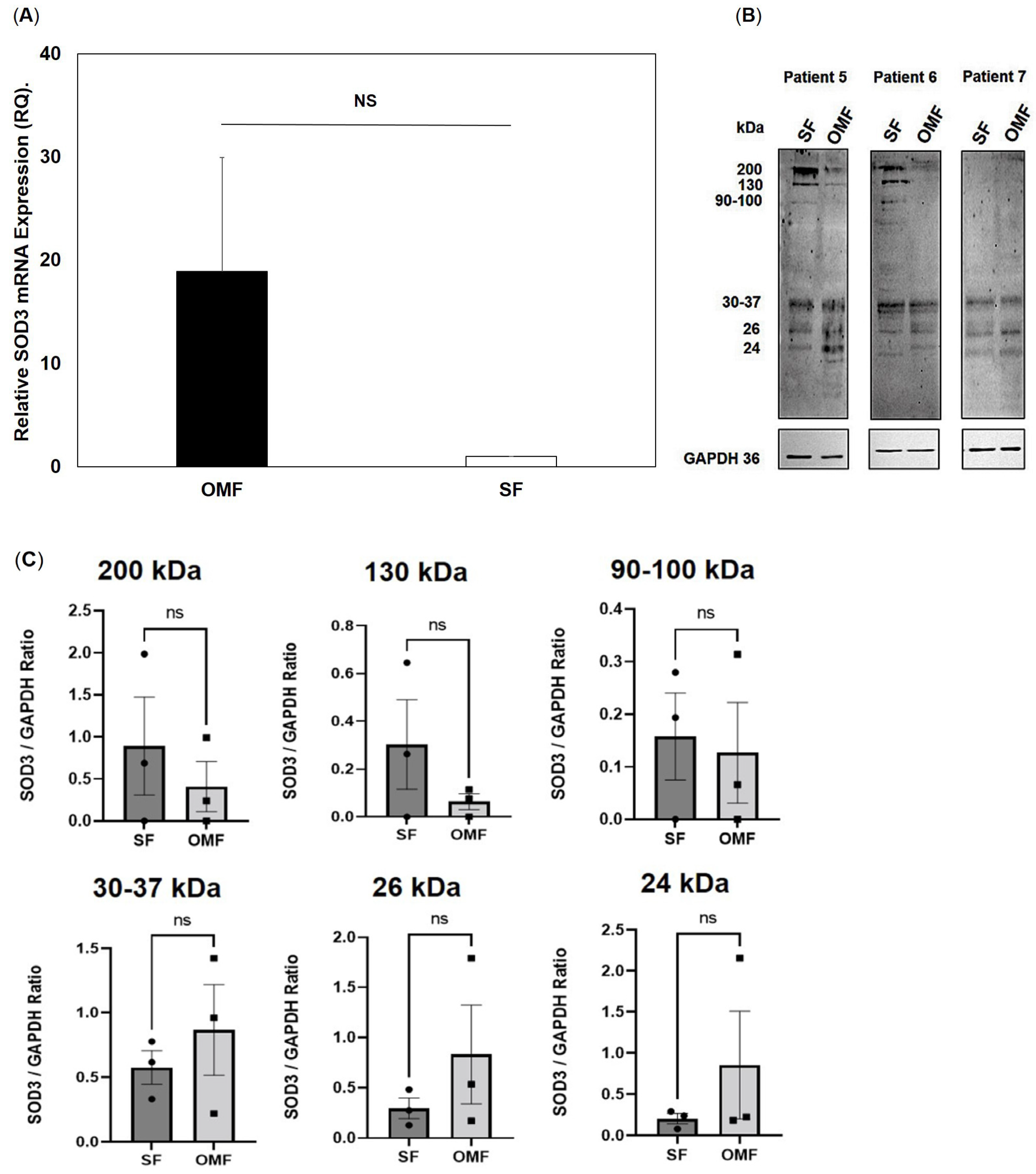
3.6. Superoxide Dismutase 3 (SOD3) Expression and Protein Levels in Oral Mucosal and Skin Fibroblasts
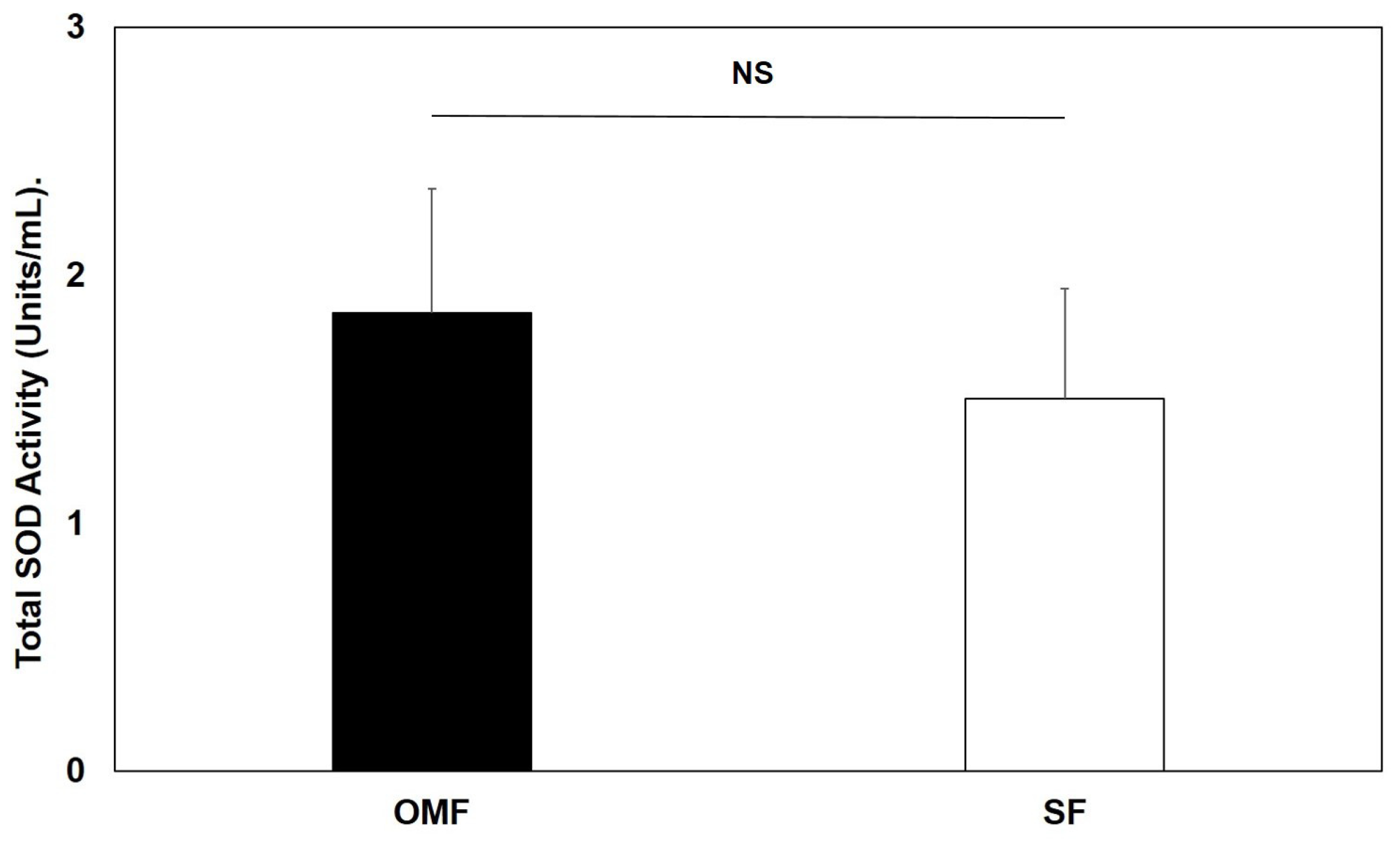
3.7. Total Superoxide Dismutase (SOD) Activity Levels in Oral Mucosal and Skin Fibroblasts
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Enoch, S.; Moseley, R.; Stephens, P.; Thomas, D.W. The oral mucosa: A model of wound healing with reduced scarring. Oral Surg. 2008, 1, 11–21. [Google Scholar] [CrossRef]
- Glim, J.E.; van Egmond, M.; Niessen, F.B.; Everts, V.; Beelen, R.H. Detrimental dermal wound healing: What can we learn from the oral mucosa? Wound Repair Regen. 2013, 21, 648–660. [Google Scholar] [CrossRef]
- Moore, A.L.; Marshall, C.D.; Barnes, L.A.; Murphy, M.P.; Ransom, R.C.; Longaker, M.T. Scarless wound healing: Transitioning from fetal research to regenerative healing. Wiley Interdiscip. Rev. Dev. Biol. 2018, 7, 10. [Google Scholar] [CrossRef]
- Stephens, P.; Davies, K.J.; Occleston, N.; Pleass, R.D.; Kon, C.; Daniels, J.; Khaw, P.T.; Thomas, D.W. Skin and oral fibroblasts exhibit phenotypic differences in extracellular matrix reorganization and matrix metalloproteinase activity. Br. J. Dermatol. 2001, 144, 229–237. [Google Scholar] [CrossRef]
- Shannon, D.B.; McKeown, S.T.; Lundy, F.T.; Irwin, C.R. Phenotypic differences between oral and skin fibroblasts in wound contraction and growth factor expression. Wound Repair Regen. 2006, 14, 172–178. [Google Scholar] [CrossRef]
- McKeown, S.T.W.; Barnes, J.J.; Hyland, P.L.; Lundy, F.T.; Fray, M.J.; Irwin, C.R. Matrix metalloproteinase-3 differences in oral and skin fibroblasts. J. Dent. Res. 2007, 86, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Meran, S.; Thomas, D.W.; Stephens, P.; Enoch, S.; Martin, J.; Steadman, R.; Phillips, A.O. Hyaluronan facilitates transforming growth factor-β1-mediated fibroblast proliferation. J. Biol. Chem. 2008, 283, 6530–6545. [Google Scholar] [CrossRef] [PubMed]
- Enoch, S.; Wall, I.; Peake, M.; Davies, L.; Farrier, J.; Giles, P.; Baird, D.; Kipling, D.; Price, P.; Moseley, R.; et al. Increased oral fibroblast lifespan is telomerase-independent. J. Dent. Res. 2009, 88, 916–921. [Google Scholar] [CrossRef]
- Enoch, S.; Wall, I.; Peake, M.; Davies, L.C.; Farrier, J.; Giles, P.; Kipling, D.; Price, P.; Moseley, R.; Thomas, D.; et al. “Young” oral fibroblasts are geno/phenotypically distinct. J. Dent. Res. 2010, 89, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Tai, Y.; Woods, E.L.; Dally, J.; Kong, D.; Steadman, R.; Moseley, R.; Midgley, A.C. Myofibroblasts: Function, formation, and scope of molecular therapies for skin fibrosis. Biomolecules 2021, 11, 1095. [Google Scholar] [CrossRef]
- Meran, S.; Thomas, D.W.; Stephens, P.; Martin, J.; Bowen, T.; Phillips, A.O.; Steadman, R. Involvement of hyaluronan in regulation of fibroblast phenotype. J. Biol. Chem. 2007, 282, 25687–25697. [Google Scholar] [CrossRef]
- Schrementi, M.E.; Ferreira, A.M.; Zender, C.; DiPietro, L.A. Site-specific production of TGF-β in oral mucosal and cutaneous wounds. Wound Rep. Regen. 2008, 16, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Dally, J.; Khan, J.S.; Voisey, A.; Charalambous, C.; John, H.L.; Woods, E.L.; Steadman, R.; Moseley, R.; Midgley, A.C. Hepatocyte growth factor mediates enhanced wound healing responses and resistance to transforming growth factor-β1-driven myofibroblast differentiation in oral mucosal fibroblasts. Int. J. Mol. Sci. 2017, 18, 1843. [Google Scholar] [CrossRef] [PubMed]
- Peake, M.A.; Caley, M.; Giles, P.J.; Wall, I.; Enoch, S.; Davies, L.C.; Kipling, D.; Thomas, D.W.; Stephens, P. Identification of a transcriptional signature for the wound healing continuum. Wound Rep. Regen. 2014, 22, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, K.; Horiguchi, T.; Tanimura, A.; Hagita, H.; Noma, T. Gene signature of human oral mucosa fibroblasts: Comparison with dermal fibroblasts and induced pluripotent stem cells. Biomed Res. Int. 2015, 2015, 121575. [Google Scholar] [CrossRef]
- Stephens, P.; Hiscox, S.; Cook, H.; Jiang, W.G.; Zhiquiang, W.; Thomas, D.W. Phenotypic variation in the production of bioactive hepatocyte growth factor/scatter factor by oral mucosal and skin fibroblasts. Wound Rep. Regen. 2001, 9, 34–43. [Google Scholar] [CrossRef]
- Okazaki, M.; Yoshimura, K.; Uchida, G.; Harii, K. Elevated expression of hepatocyte and keratinocyte growth factor in cultured buccal-mucosa-derived fibroblasts compared with normal skin-derived fibroblasts. J. Dermatol. Sci. 2002, 30, 108–115. [Google Scholar] [CrossRef]
- Moseley, R.; Stewart, J.E.; Stephens, P.; Waddington, R.J.; Thomas, D.W. Extracellular matrix metabolites as potential biomarkers of disease activity in wound fluid: Lessons learned from other inflammatory diseases? Br. J. Dermatol. 2004, 150, 401–413. [Google Scholar] [CrossRef]
- Wlaschek, M.; Scharffetter-Kochanek, K. Oxidative stress in chronic venous leg ulcers. Wound Repair Regen. 2005, 13, 452–461. [Google Scholar] [CrossRef]
- Shroff, A.; Mamalis, A.; Jagdeo, J. Oxidative stress and skin fibrosis. Curr. Pathobiol. Rep. 2014, 2, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Siani, A.; Tirelli, N. Myofibroblast differentiation: Main features, biomedical relevance, and the role of reactive oxygen species. Antioxid. Redox Signal. 2014, 21, 768–785. [Google Scholar] [CrossRef] [PubMed]
- Choudhari, S.K.; Chaudhary, M.; Gadbail, A.R.; Sharma, A.; Tekade, S. Oxidative and antioxidative mechanisms in oral cancer and precancer: A review. Oral Oncol. 2014, 50, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Katakwar, P.; Metgud, R.; Naik, S.; Mittal, R. Oxidative stress marker in oral cancer: A review. J. Cancer Res. Ther. 2016, 12, 438–446. [Google Scholar] [CrossRef]
- Obrador, E.; Liu-Smith, F.; Dellinger, R.W.; Salvador, R.; Meyskens, F.L.; Estrela, J.M. Oxidative stress and antioxidants in the pathophysiology of malignant melanoma. Biol. Chem. 2019, 400, 589–612. [Google Scholar] [CrossRef] [PubMed]
- Sardaro, N.; Della Vella, F.; Incalza, M.A.; Di Stasio, D.; Lucchese, A.; Contaldo, M.; Laudadio, C.; Petruzzi, M. Oxidative stress and oral mucosal diseases: An overview. In Vivo 2019, 33, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Waddington, R.J.; Moseley, R.; Embery, G. Reactive oxygen species: A potential role in the pathogenesis of periodontal diseases. Oral Dis. 2000, 6, 138–151. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, X.; Vikash, V.; Ye, Q.; Wu, D.; Liu, Y.; Dong, W. ROS and ROS-mediated cellular signaling. Oxid. Med. Cell. Longev. 2016, 2016, 4350965. [Google Scholar] [CrossRef]
- Waddington, R.J.; Alraies, A.; Colombo, J.S.; Sloan, A.J.; Okazaki, J.; Moseley, R. Characterization of oxidative stress status during diabetic bone healing. Cells Tissues Organs 2011, 194, 307–312. [Google Scholar] [CrossRef]
- Blander, G.; de Oliveira, R.M.; Conboy, C.M.; Haigis, M.; Guarente, L. Superoxide dismutase 1 knock-down induces senescence in human fibroblasts. J. Biol. Chem. 2003, 278, 38966–38969. [Google Scholar] [CrossRef]
- Serra, V.; von Zglinicki, T.; Lorenz, M.; Saretzki, G. Extracellular superoxide dismutase is a major antioxidant in human fibroblasts and slows telomere shortening. J. Biol. Chem. 2003, 278, 6824–6830. [Google Scholar] [CrossRef]
- Brown, M.F.; Stuart, J.A. Correlation of mitochondrial superoxide dismutase and DNA polymerase β in mammalian dermal fibroblasts with species maximal lifespan. Mech. Ageing Dev. 2007, 128, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Kirkman, H.N.; Gaetani, G.F. Mammalian catalase: A venerable enzyme with new mysteries. Trends Biochem. Sci. 2007, 32, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Fukai, T.; Ushio-Fukai, M. Superoxide dismutases: Role in redox signaling, vascular function, and diseases. Antioxid. Redox Signal. 2011, 15, 1583–1606. [Google Scholar] [CrossRef]
- Shakunthala, G.K.; Annigeri, R.G.; Arunkumar, S. Role of oxidative stress in the pathogenesis of oral submucous fibrosis: A preliminary prospective study. Contemp. Clin. Dent. 2015, 6, S172–S174. [Google Scholar] [CrossRef] [PubMed]
- Rai, V.; Bose, S.; Saha, S.; Chakraborty, C. Evaluation of oxidative stress and the microenvironment in oral submucous fibrosis. Heliyon 2019, 5, e01502. [Google Scholar] [CrossRef]
- Rokad, F.; Moseley, R.; Hardy, R.S.; Chukkapalli, S.; Crean, S.; Kesavalu, L.; Singhrao, S.K. Cerebral oxidative stress and microvasculature defects in TNF-α expressing transgenic and Porphyromonas gingivalis-infected ApoE-/- mice. J. Alzheimers Dis. 2017, 60, 359–369. [Google Scholar] [CrossRef]
- Wall, I.B.; Moseley, R.; Baird, D.M.; Kipling, D.; Giles, P.; Laffafian, I.; Price, P.E.; Thomas, D.W.; Stephens, P. Fibroblast dysfunction is a key factor in the non-healing of chronic venous leg ulcers. J. Investig. Dermatol. 2008, 128, 2526–2540. [Google Scholar] [CrossRef]
- Alaidaroos, N.Y.A.; Alraies, A.; Waddington, R.J.; Sloan, A.J.; Moseley, R. Differential SOD2 and GSTZ1 profiles contribute to contrasting dental pulp stem cell susceptibilities to oxidative damage and premature senescence. Stem Cell Res. Ther. 2021, 12, 142. [Google Scholar] [CrossRef]
- Moseley, R.; Hilton, J.R.; Waddington, R.J.; Harding, K.G.; Stephens, P.; Thomas, D.W. Comparison of oxidative stress biomarker profiles between acute and chronic wound environments. Wound Repair Regen. 2004, 12, 419–429. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2–ΔΔCt method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Ookawara, T.; Eguchi, H.; Nishimura, M.; Kizaki, T.; Takayama, E.; Saitoh, D.; Ohno, H.; Suzuki, K. Effects of oxidative stress on the nuclear translocation of extracellular superoxide dismutase. Biochem. Biophys. Res. Commun. 2003, 303, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.V.; Enghild, J.J. Extracellular superoxide dismutase: Structural and functional considerations of a protein shaped by two different disulphide bridge patterns. Biomed. Pharmacother. 2005, 59, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Due, A.V.; Petersen, S.V.; Valnickova, Z.; Østergaard, L.; Oury, T.D.; Crapo, J.D.; Enghild, J.J. Extracellular superoxide dismutase exists as an octamer. FEBS Lett. 2006, 580, 1485–1489. [Google Scholar] [CrossRef]
- Fattman, C.L.; Schaefer, L.M.; Oury, T.D. Extracellular superoxide dismutase in biology and medicine. Free Radic. Biol. Med. 2003, 35, 236–256. [Google Scholar] [CrossRef] [PubMed]
- Nozik-Grayck, E.; Suliman, H.B.; Piantadosi, C.A. Extracellular superoxide dismutase. Int. J. Biochem. Cell Biol. 2005, 37, 2466–2471. [Google Scholar] [CrossRef] [PubMed]
- Rhie, G.; Shin, M.H.; Seo, J.Y.; Choi, W.W.; Cho, K.H.; Kim, K.H.; Park, K.C.; Eun, H.C.; Chung, J.H. Aging- and photoaging-dependent changes of enzymic and nonenzymic antioxidants in the epidermis and dermis of human skin in vivo. J. Investig. Dermatol. 2001, 117, 1212–1217. [Google Scholar] [CrossRef]
- Zavadskiy, S.; Sologova, S.; Moldogazieva, N. Oxidative distress in aging and age-related diseases: Spatiotemporal dysregulation of protein oxidation and degradation. Biochimie 2022, 195, 114–134. [Google Scholar] [CrossRef]
- Shindo, Y.; Witt, E.; Han, D.; Epstein, W.; Packer, L. Enzymic and non-enzymic antioxidants in epidermis and dermis of human skin. J. Investig. Dermatol. 1994, 102, 122–124. [Google Scholar] [CrossRef]
- Sander, C.S.; Chang, H.; Salzmann, S.; Müller, C.S.; Ekanayake-Mudiyanselage, S.; Elsner, P.; Thiele, J.J. Photoaging is associated with protein oxidation in human skin in vivo. J. Investig. Dermatol. 2002, 118, 618–625. [Google Scholar] [CrossRef]
- Yang, J.; Lam, E.W.N.; Hammad, H.M.; Oberley, T.D.; Oberley, L.W. Antioxidant enzyme levels in oral squamous cell carcinoma and normal human oral epithelium. J. Oral Pathol. Med. 2002, 31, 71–77. [Google Scholar] [CrossRef]
- Hamanaka, H.; Miyachi, Y.; Tachibana, T.; Imamura, S. Lowered Cu, Zn-superoxide dismutase activity in human malignant skin tumors. J. Dermatol. 1991, 18, 258–261. [Google Scholar] [CrossRef]
- Lam, E.W.; Hammad, H.M.; Zwacka, R.; Darby, C.J.; Baumgardner, K.R.; Davidson, B.L.; Oberley, T.D.; Engelhardt, J.F.; Oberley, L.W. Immunolocalization and adenoviral vector-mediated manganese superoxide dismutase gene transfer to experimental oral tumors. J. Dent Res. 2000, 79, 1410–1417. [Google Scholar] [CrossRef]
- Shukla, A.; Rasik, A.M.; Dhawan, B.N. Asiaticoside-induced elevation of antioxidant levels in healing wounds. Phytother. Res. 1999, 13, 50–54. [Google Scholar] [CrossRef]
- Steiling, H.; Munz, B.; Werner, S.; Brauchle, M. Different types of ROS-scavenging enzymes are expressed during cutaneous wound repair. Exp. Cell Res. 1999, 247, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Barrera, G.; Pizzimenti, S.; Daga, M.; Dianzani, C.; Arcaro, A.; Cetrangolo, G.P.; Giordano, G.; Cucci, M.A.; Graf, M.; Gentile, F. Lipid peroxidation-derived aldehydes, 4-hydroxynonenal and malondialdehyde in aging-related disorders. Antioxidants 2018, 7, 102. [Google Scholar] [CrossRef] [PubMed]
- Killilea, D.W.; Wong, S.L.; Cahaya, H.S.; Atamna, H.; Ames, B.N. Iron accumulation during cellular senescence. Ann. N. Y. Acad. Sci. 2004, 1019, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Krause, K.H. Aging: A revisited theory based on free radicals generated by NOX family NADPH oxidases. Exp. Gerontol. 2007, 42, 256–262. [Google Scholar] [CrossRef]
- Chapman, J.; Fielder, E.; Passos, J.F. Mitochondrial dysfunction and cell senescence: Deciphering a complex relationship. FEBS Lett. 2019, 593, 1566–1579. [Google Scholar] [CrossRef]
- Evans, M.D.; Dizdaroglu, M.; Cooke, M.S. Oxidative DNA damage and disease: Induction, repair and significance. Mutat. Res. 2004, 567, 1–61. [Google Scholar] [CrossRef]
- Davies, M.J. Protein oxidation and peroxidation. Biochem. J. 2016, 473, 805–825. [Google Scholar] [CrossRef]
- Grune, T.; Merker, K.; Jung, T.; Sitte, N.; Davies, K.J. Protein oxidation and degradation during postmitotic senescence. Free Radic. Biol. Med. 2005, 39, 1208–1215. [Google Scholar] [CrossRef]
- Barnes, R.P.; Fouquerel, E.; Opresko, P.L. The impact of oxidative DNA damage and stress on telomere homeostasis. Mech. Ageing Dev. 2019, 177, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, L.M.; Jonsson, J.; Edlund, T.; Marklund, S.L. Mice lacking extracellular superoxide dismutase are more sensitive to hyperoxia. Proc. Natl. Acad. Sci. USA 1995, 92, 6264–6268. [Google Scholar] [CrossRef] [PubMed]
- Bowler, R.P.; Nicks, M.; Tran, K.; Tanner, G.; Chang, L.-Y.; Young, S.K.; Worthen, G.S. Extracellular superoxide dismutase attenuates lipopolysaccharide-induced neutrophilic inflammation. Am. J. Respir. Cell Mol. Biol. 2004, 31, 432–439. [Google Scholar] [CrossRef]
- Ross, A.D.; Banda, N.K.; Muggli, M.; Arend, W.P. Enhancement of collagen-induced arthritis in mice genetically deficient in extracellular superoxide dismutase. Arthritis Rheumatol. 2004, 50, 3702–3711. [Google Scholar] [CrossRef] [PubMed]
- Fattman, C.L.; Tan, R.J.; Tobelowki, J.M.; Oury, T.D. Increased sensitivity to asbestos-induced injury in mice lacking extracellular superoxide dismutase. Free Radic. Biol. Med. 2006, 40, 601–607. [Google Scholar] [CrossRef]
- Ha, H.-Y.; Kim, Y.; Ryoo, Z.Y.; Kim, T.-Y. Inhibition of the TPA-induced cutaneous inflammation and hyperplasia by EC-SOD. Biochem. Biophys. Res. Commun. 2006, 348, 450–458. [Google Scholar] [CrossRef]
- Lee, M.J.; Agrahari, G.; Kim, H.Y.; An, E.J.; Chun, K.H.; Kang, H.; Kim, Y.S.; Bang, C.W.; Tak, L.J.; Kim, T.Y. Extracellular superoxide dismutase prevents skin aging by promoting collagen production through the activation of AMPK and Nrf2/HO-1 cascades. J. Investig. Dermatol. 2021, 141, 2344–2353. [Google Scholar] [CrossRef]
- Fujiwara, T.; Duscher, D.; Rustad, K.C.; Kosaraju, R.; Rodrigues, M.; Whittam, A.J.; Januszyk, M.; Maan, Z.N.; Gurtner, G.C. Extracellular superoxide dismutase deficiency impairs wound healing in advanced age by reducing neovascularization and fibroblast function. Exp. Dermatol. 2016, 25, 206–211. [Google Scholar] [CrossRef]
- Bowler, R.P.; Nicks, M.; Warnick, K.; Crapo, J.D. Role of extracellular superoxide dismutase in bleomycin-induced pulmonary fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 2002, 282, L719–L726. [Google Scholar] [CrossRef]
- Kang, S.K.; Rabbani, Z.N.; Folz, R.J.; Golson, M.L.; Huang, H.; Yu, D.; Samulski, T.S.; Dewhirst, M.W.; Anscher, M.S.; Vujaskovic, Z. Overexpression of extracellular superoxide dismutase protects mice from radiation-induced lung injury. Int. J. Radiat. Oncol. Biol. Phys. 2003, 57, 1056–1066. [Google Scholar] [CrossRef]
- Kliment, C.R.; Suliman, H.B.; Tobolewski, J.M.; Reynolds, C.M.; Day, B.J.; Zhu, X.; McTiernan, C.F.; McGaffin, K.R.; Piantadosi, C.A.; Oury, T.D. Extracellular superoxide dismutase regulates cardiac function and fibrosis. J. Mol. Cell. Cardiol. 2009, 47, 730–742. [Google Scholar] [CrossRef]
- Sun, Y.-L.; Bai, T.; Zhou, L.; Zhu, R.-T.; Wang, W.-J.; Liang, R.-P.; Li, J.; Zhang, C.-X.; Gou, J.-J. SOD3 deficiency induces liver fibrosis by promoting hepatic stellate cell activation and epithelial-mesenchymal transition. J. Cell. Physiol. 2021, 236, 4313–4329. [Google Scholar] [CrossRef] [PubMed]
- Conway, K.; Price, P.; Harding, K.G.; Jiang, W.G. The molecular and clinical impact of hepatocyte growth factor, its receptor, activators, and inhibitors in wound healing. Wound Repair Regen. 2006, 14, 2–10. [Google Scholar] [CrossRef]
- Li, H.; Jiang, T.; Lin, Y.; Zhao, Z.; Zhang, N. HGF protects rat mesangial cells from high-glucose-mediated oxidative stress. Am. J. Nephrol. 2006, 26, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Arends, B.; Slump, E.; Spee, B.; Rothuizen, J.; Penning, L.C. Hepatocyte growth factor improves viability after H2O2-induced toxicity in bile duct epithelial cells. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2008, 147, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Hui, L.; Hong, Y.; Jingjing, Z.; Yuan, H.; Qi, C.; Nong, Z. HGF suppresses high glucose-mediated oxidative stress in mesangial cells by activation of PKG and inhibition of PKA. Free Radic. Biol. Med. 2010, 49, 467–473. [Google Scholar] [CrossRef] [PubMed]
| Enzymic Antioxidant | Affymetrix™ Probe ID | Log2-Fold Difference (FDR p Value) |
|---|---|---|
| SOD1 | 200642_at | 0.078 (0.9996) |
| SOD2 | 215078_at | −0.047 (0.9996) |
| 215223_s_at | −0.336 (0.9996) | |
| 216841_s_at | −0.375 (0.9996) | |
| 221477_s_at | −0.531 (0.9996) | |
| SOD3 | 205236_x_at | 1.706 (0.1848) |
| Catalase | 201432_at | 0.342 (0.9996) |
| 211922_s_at | 0.432 (0.9593) | |
| 215573_at | −0.032 (0.9996) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lohana, P.; Suryaprawira, A.; Woods, E.L.; Dally, J.; Gait-Carr, E.; Alaidaroos, N.Y.A.; Heard, C.M.; Lee, K.Y.; Ruge, F.; Farrier, J.N.; et al. Role of Enzymic Antioxidants in Mediating Oxidative Stress and Contrasting Wound Healing Capabilities in Oral Mucosal/Skin Fibroblasts and Tissues. Antioxidants 2023, 12, 1374. https://doi.org/10.3390/antiox12071374
Lohana P, Suryaprawira A, Woods EL, Dally J, Gait-Carr E, Alaidaroos NYA, Heard CM, Lee KY, Ruge F, Farrier JN, et al. Role of Enzymic Antioxidants in Mediating Oxidative Stress and Contrasting Wound Healing Capabilities in Oral Mucosal/Skin Fibroblasts and Tissues. Antioxidants. 2023; 12(7):1374. https://doi.org/10.3390/antiox12071374
Chicago/Turabian StyleLohana, Parkash, Albert Suryaprawira, Emma L. Woods, Jordanna Dally, Edward Gait-Carr, Nadia Y. A. Alaidaroos, Charles M. Heard, Kwok Y. Lee, Fiona Ruge, Jeremy N. Farrier, and et al. 2023. "Role of Enzymic Antioxidants in Mediating Oxidative Stress and Contrasting Wound Healing Capabilities in Oral Mucosal/Skin Fibroblasts and Tissues" Antioxidants 12, no. 7: 1374. https://doi.org/10.3390/antiox12071374
APA StyleLohana, P., Suryaprawira, A., Woods, E. L., Dally, J., Gait-Carr, E., Alaidaroos, N. Y. A., Heard, C. M., Lee, K. Y., Ruge, F., Farrier, J. N., Enoch, S., Caley, M. P., Peake, M. A., Davies, L. C., Giles, P. J., Thomas, D. W., Stephens, P., & Moseley, R. (2023). Role of Enzymic Antioxidants in Mediating Oxidative Stress and Contrasting Wound Healing Capabilities in Oral Mucosal/Skin Fibroblasts and Tissues. Antioxidants, 12(7), 1374. https://doi.org/10.3390/antiox12071374








