Effects of Physical Exercise and Motor Activity on Oxidative Stress and Inflammation in Post-Mastectomy Pain Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Methodology
2.3.1. Demographic and Surgical Variables
2.3.2. Numerical Rating Scale (NRS)
2.3.3. Brief Pain Inventory (BPI)
2.3.4. International Physical Activity Questionnaire (IPAQ)
2.3.5. Biomarkers of Oxidative Stress and Inflammation
2.3.6. Statistics
3. Results
3.1. Numerical Rating Scale Score (NRSs) and Brief Pain Inventory (BPI)
3.2. Biomarkers of Oxidative Stress and Inflammation
3.3. IPAQ Score
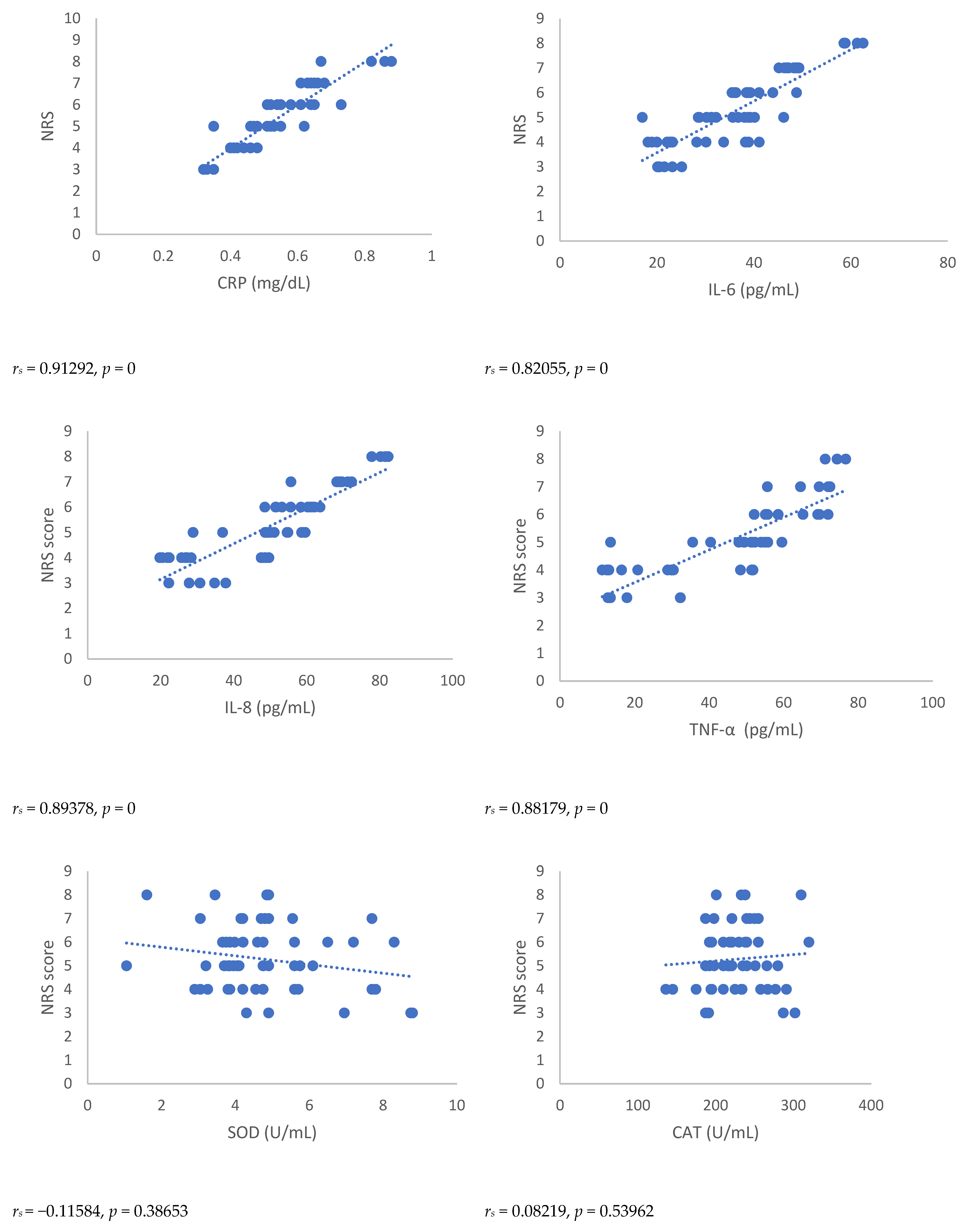
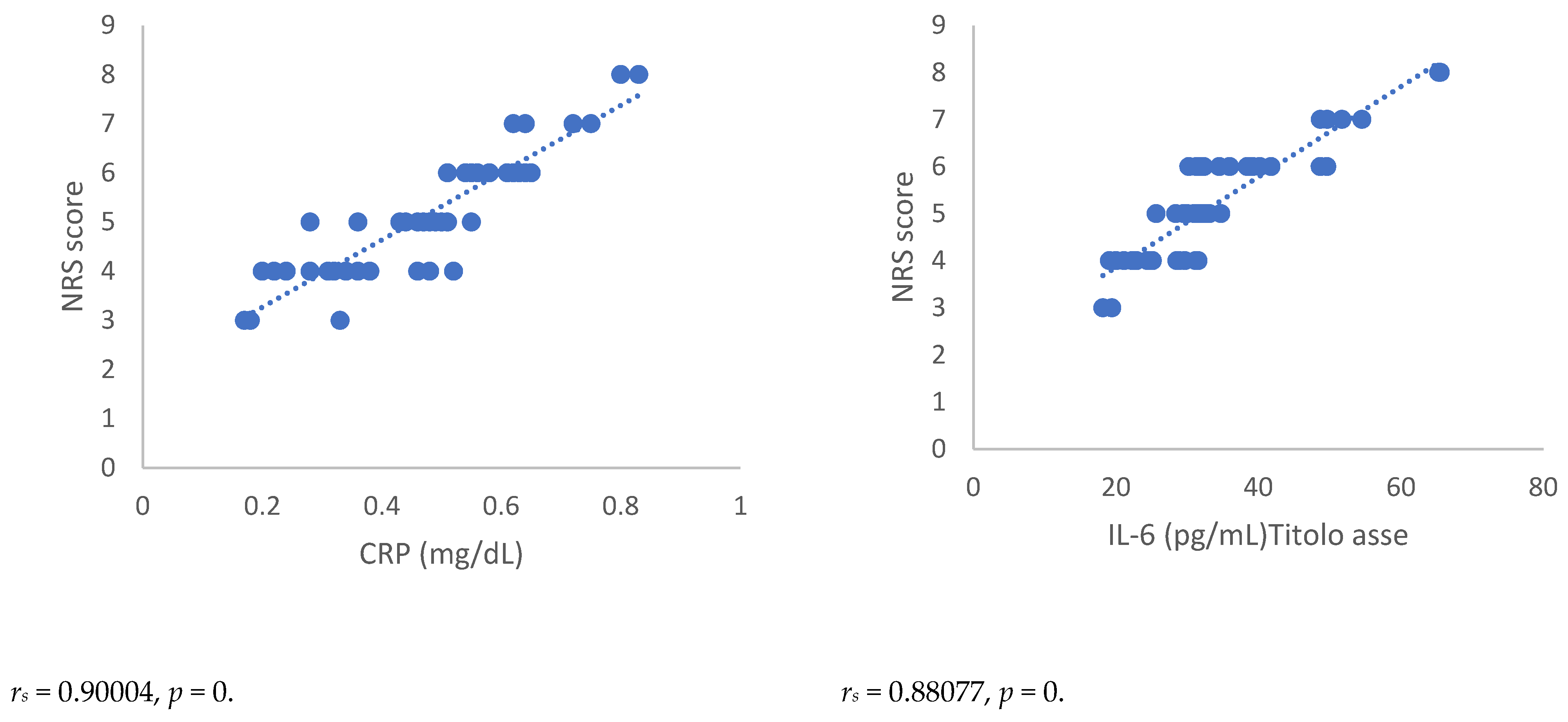
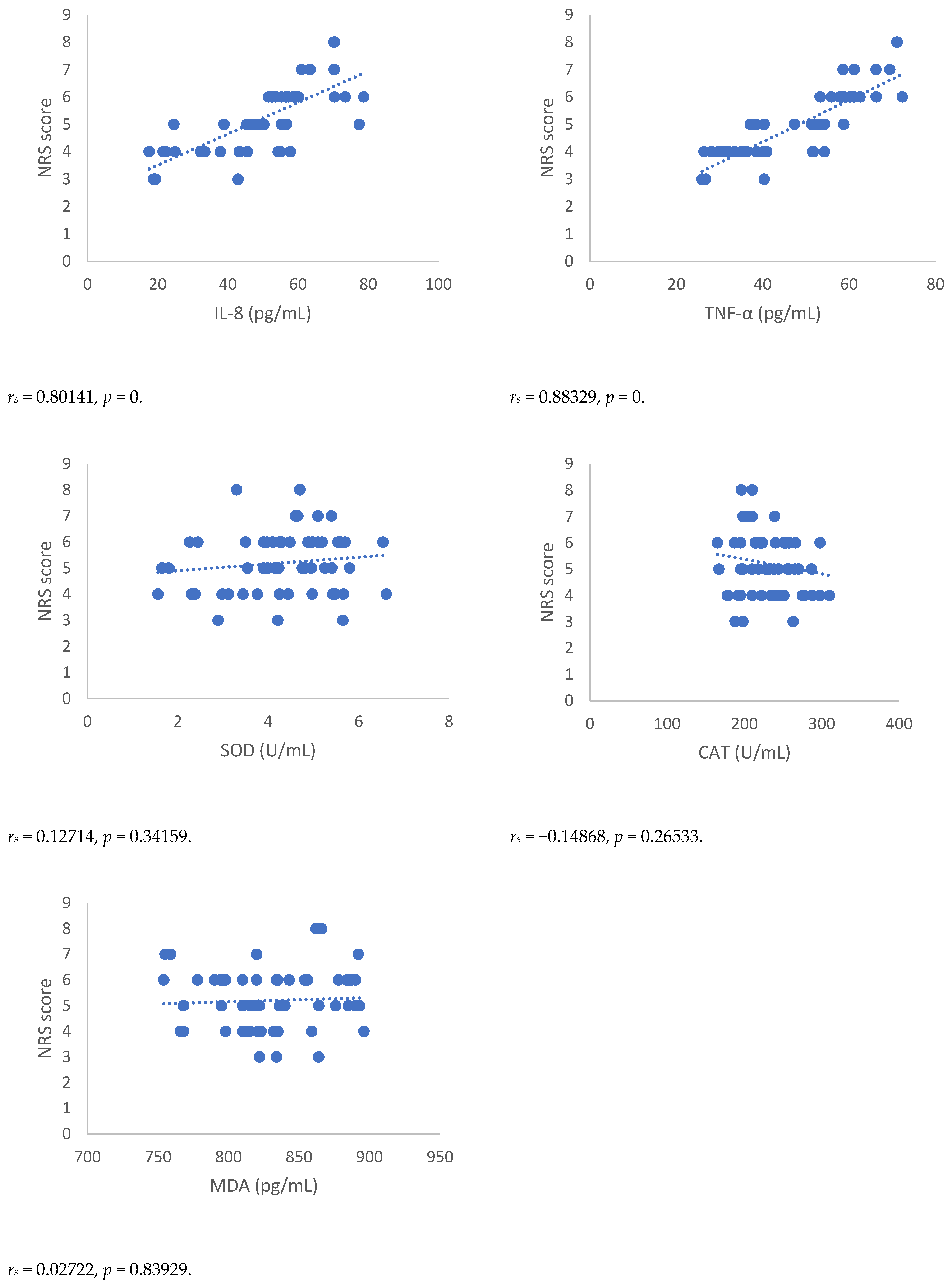
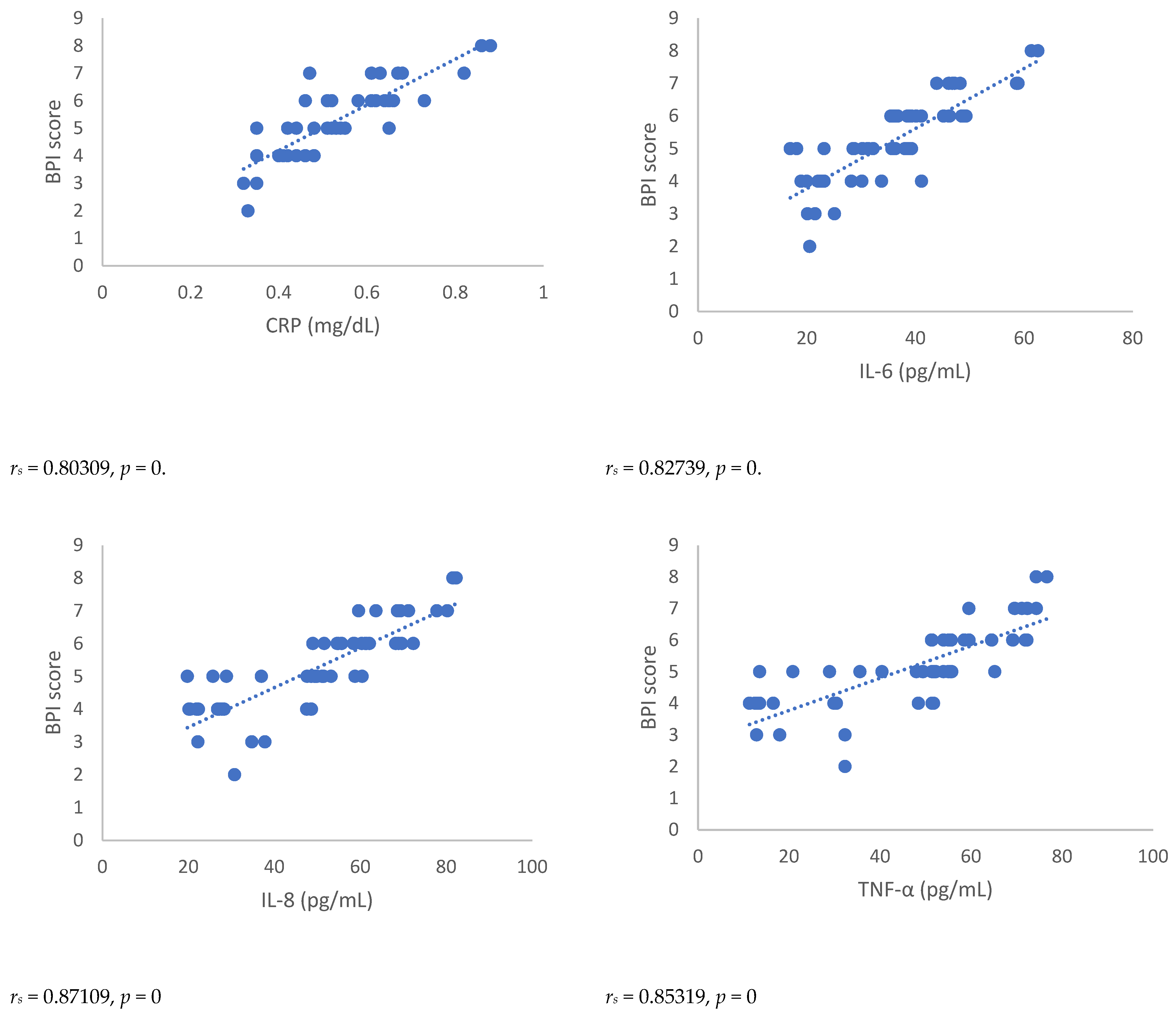
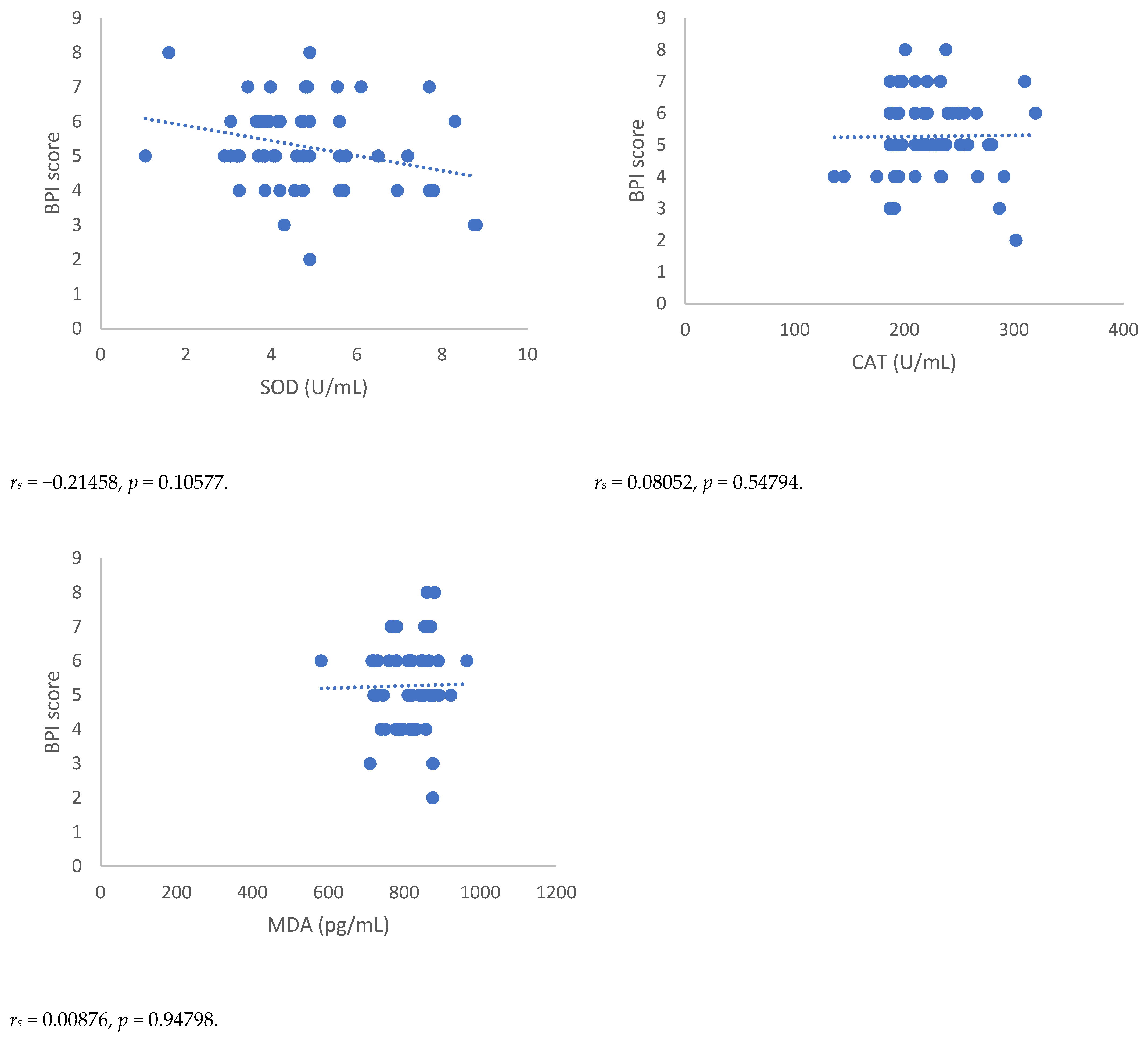
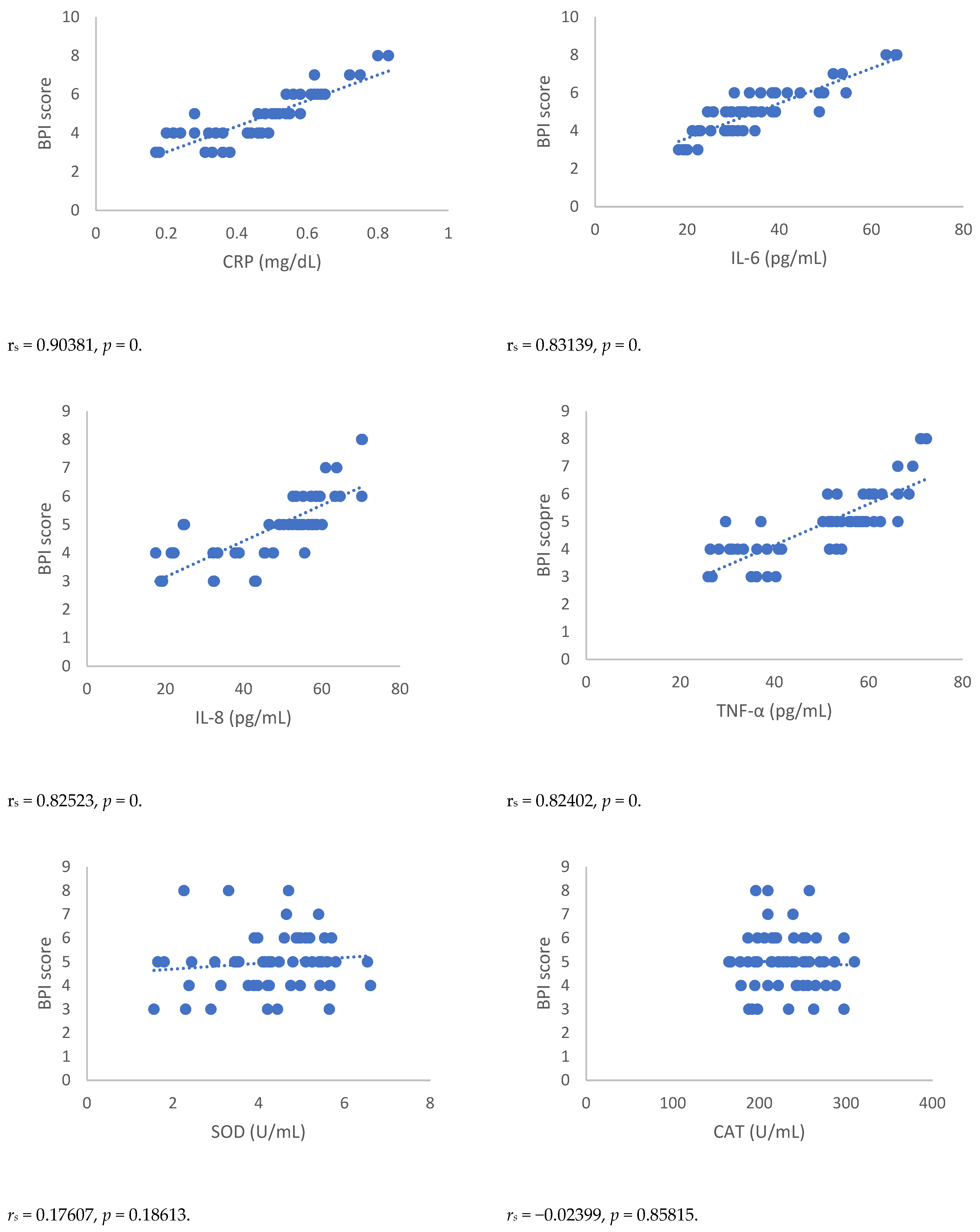
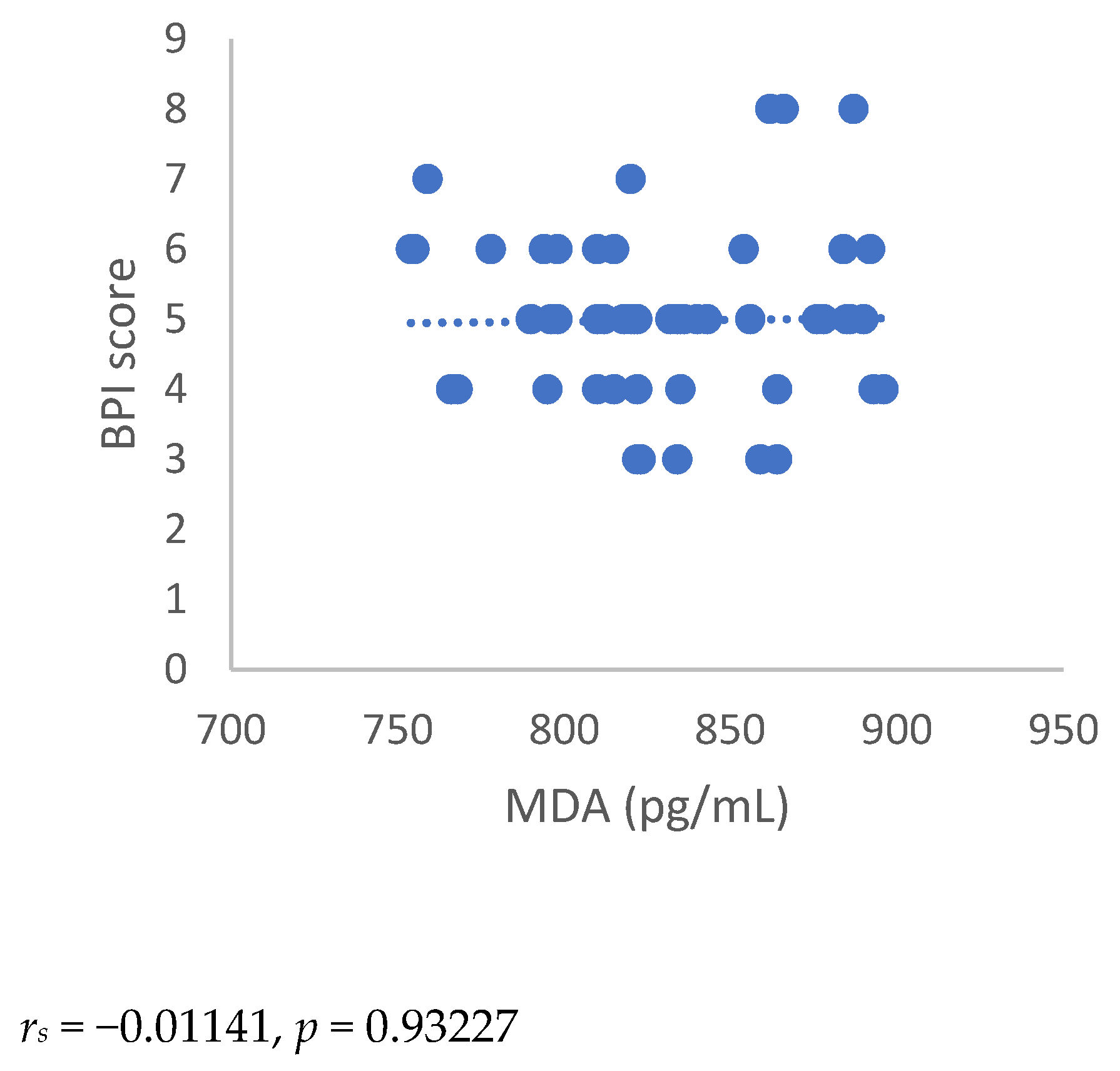
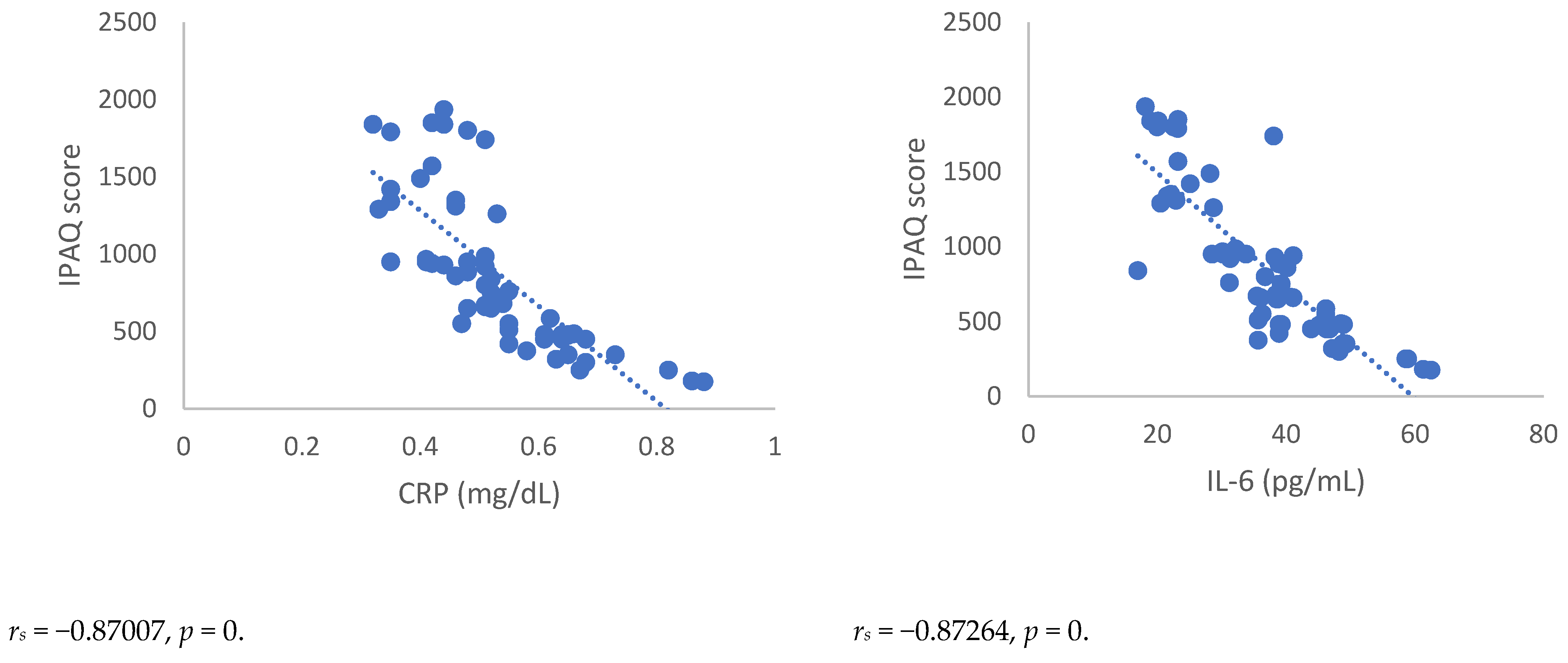
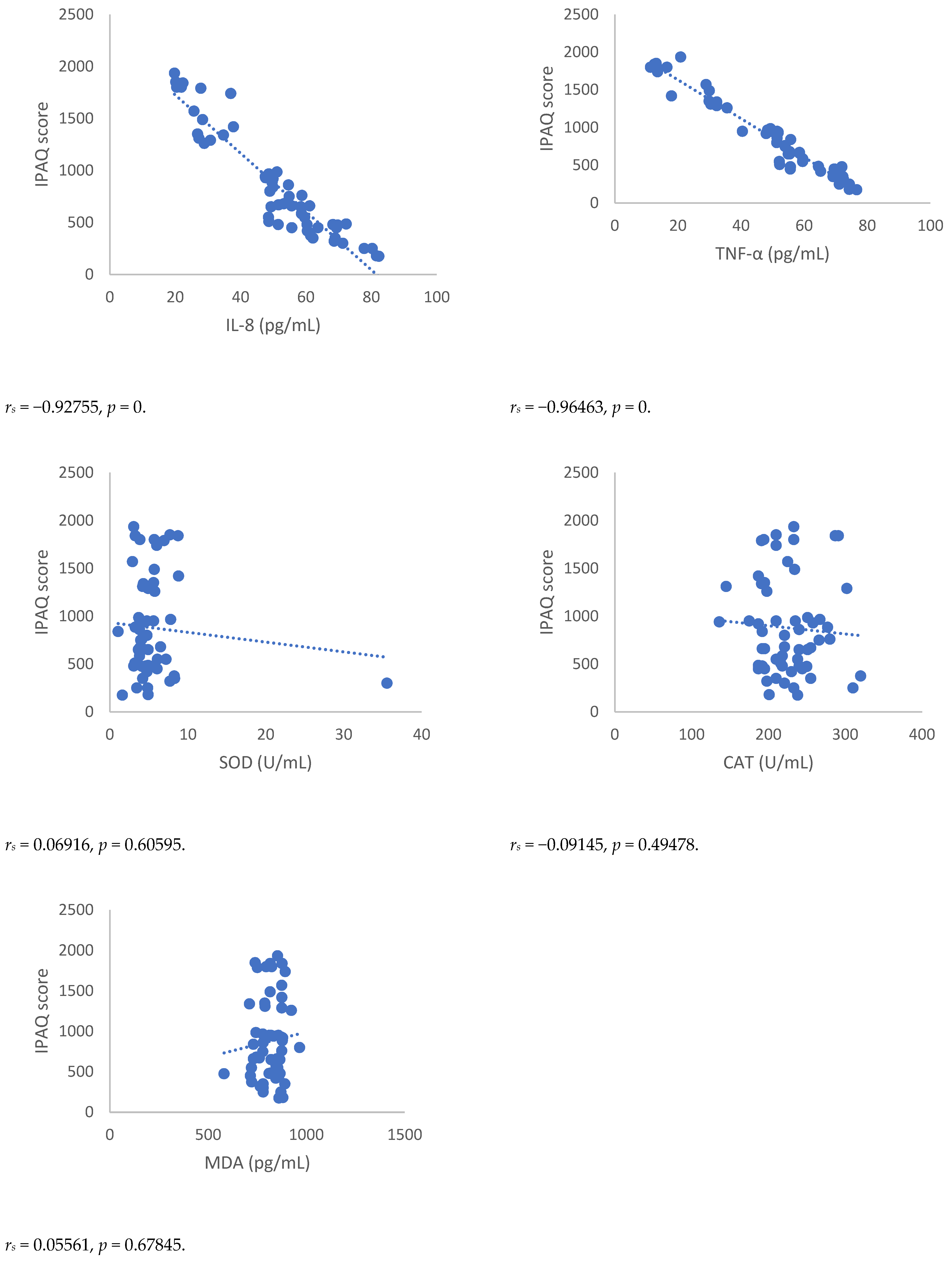
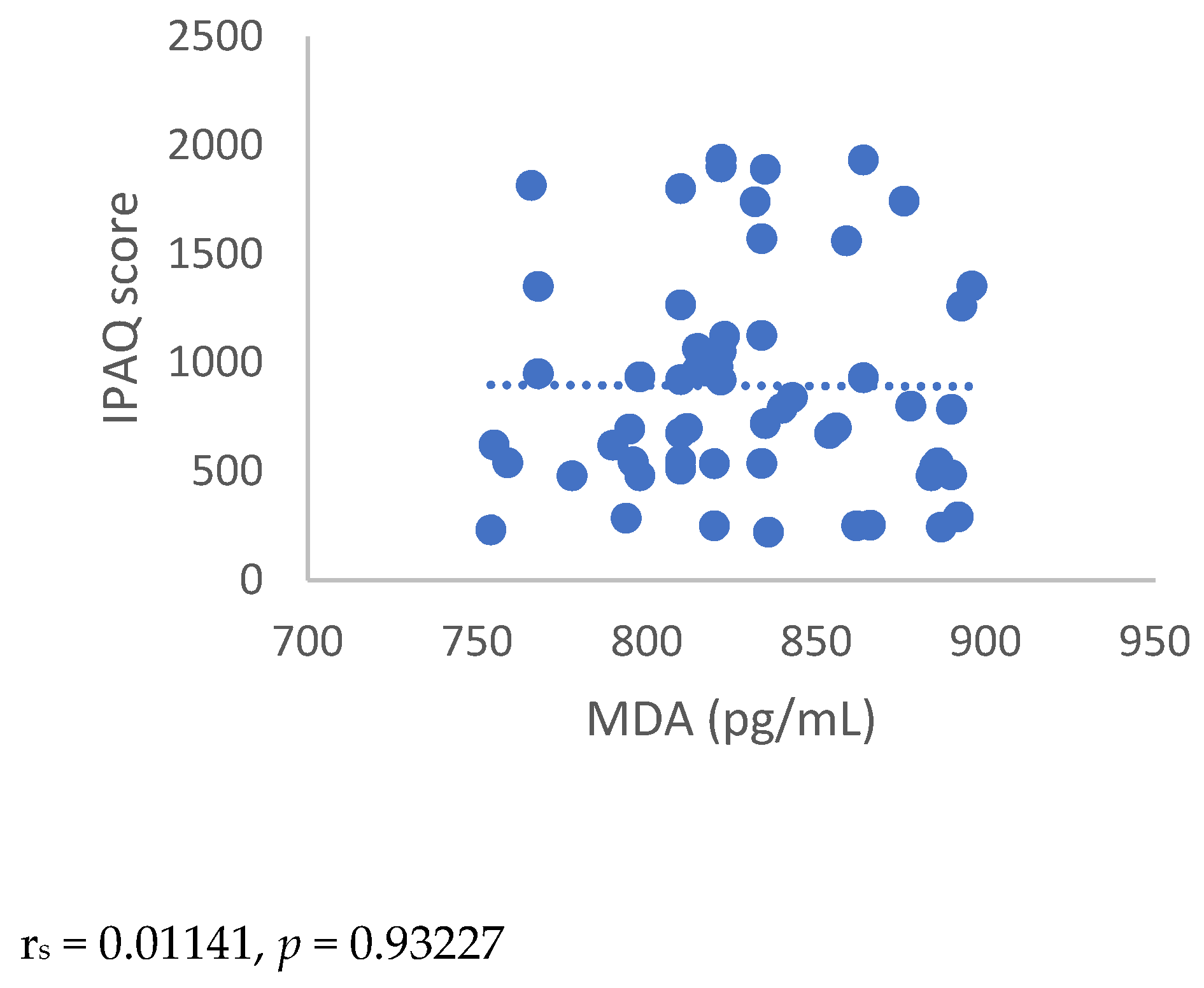
3.4. Spearman’s Correlation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brennan, T.J. Pathophysiology of postoperative pain. Pain 2011, 152 (Suppl. 3), S33–S40. [Google Scholar] [CrossRef]
- Schug, S.A.; Lavand’homme, P.; Barke, A.; Korwisi, B.; Rief, W.; Treede, R.D. IASP Taskforce for the Classification of Chronic Pain. The IASP classification of chronic pain for ICD-11: Chronic postsurgical or posttraumatic pain. Pain 2019, 160, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef] [PubMed]
- Tait, R.C.; Zoberi, K.; Ferguson, M.; Levenhagen, K.; Luebbert, R.A.; Rowland, K.; Salsich, G.B.; Herndon, C. Persistent Post-Mastectomy Pain: Risk Factors and Current Approaches to Treatment. J. Pain 2018, 19, 1367–1383. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152 (Suppl. 3), S2–S15. [Google Scholar] [CrossRef]
- Nijs, J.; Lahousse, A.; Fernández-de-Las-Peñas, C.; Madeleine, P.; Fontaine, C.; Nishigami, T.; Desmedt, C.; Vanhoeij, M.; Mostaqim, K.; Cuesta-Vargas, A.I.; et al. Towards precision pain medicine for pain after cancer: The Cancer Pain Phenotyping Network multidisciplinary international guidelines for pain phenotyping using nociplastic pain criteria. Br. J. Anaesth. 2023; Online ahead of print. [Google Scholar]
- International Association for the Study of Pain (IASP). IASP Terminology. Available online: https://www.iasp-pain.org/terminology?navItemNumber=576#Centralsensitization (accessed on 21 February 2023).
- Chappell, A.G.; Yuksel, S.; Sasson, D.C.; Wescott, A.B.; Connor, L.M.; Ellis, M.F. Post-Mastectomy Pain Syndrome: An Up-to-Date Review of Treatment Outcomes. JPRAS Open 2021, 30, 97–109. [Google Scholar] [CrossRef]
- Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986, 3, S1-226. Available online: https://pubmed.ncbi.nlm.nih.gov/3461421/ (accessed on 30 January 2023).
- Calapai, M.; Esposito, E.; Puzzo, L.; Vecchio, D.A.; Blandino, R.; Bova, G.; Quattrone, D.; Mannucci, C.; Ammendolia, I.; Mondello, C.; et al. Post-Mastectomy Pain: An Updated Overview on Risk Factors, Predictors, and Markers. Life 2021, 11, 1026. [Google Scholar] [CrossRef]
- Wang, L.; Cohen, J.C.; Devasenapathy, N.; Hong, B.Y.; Kheyson, S.; Lu, D.; Oparin, Y.; Kennedy, S.A.; Romerosa, B.; Arora, N.; et al. Prevalence and intensity of persistent post-surgical pain following breast cancer surgery: A systematic review and meta-analysis of observational studies. Br. J. Anaesth. 2020, 125, 346–357. [Google Scholar] [CrossRef]
- Chang, P.J.; Asher, A.; Smith, S.R. A Targeted Approach to Post-Mastectomy Pain and Persistent Pain following Breast Cancer Treatment. Cancers 2021, 13, 5191. [Google Scholar] [CrossRef] [PubMed]
- Scaffidi, M.; Vulpiani, M.C.; Vetrano, M.; Conforti, F.; Marchetti, M.R.; Bonifacino, A.; Marchetti, P.; Saraceni, V.M.; Ferretti, A. Early rehabilitation reduces the onset of complications in the upper limb following breast cancer surgery. Eur. J. Phys. Rehabil. Med. 2012, 48, 601–611. [Google Scholar] [PubMed]
- Ambrose, K.R.; Golightly, Y.M. Physical exercise as non-pharmacological treatment of chronic pain: Why and when. Best Pract. Res. Clin. Rheumatol. 2015, 29, 120–130. [Google Scholar] [CrossRef]
- Mittal, M.; Siddiqui, M.R.; Tran, K.; Reddy, S.P.; Malik, A.B. Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox Signal. 2014, 20, 1126–1167. [Google Scholar] [CrossRef] [PubMed]
- Klafke, J.Z.; da Silva, M.A.; Rossato, M.F.; de Prá, S.D.; Rigo, F.K.; Walker, C.I.; Bochi, G.V.; Moresco, R.N.; Ferreira, J.; Trevisan, G. Acute and chronic nociceptive phases observed in a rat hind paw ischemia/reperfusion model depend on different mechanisms. Pflug. Arch. 2016, 468, 229–241. [Google Scholar] [CrossRef]
- Breivik, H.; Borchgrevink, P.C.; Allen, S.M.; Rosseland, L.A.; Romundstad, L.; Hals, E.K.; Kvarstein, G.; Stubhaug, A. Assessment of pain. Br. J. Anaesth. 2008, 101, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Farrar, J.T.; Young, J.P., Jr.; LaMoreaux, L.; Werth, J.L.; Poole, M.R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.; Hoggart, B. Pain: A review of three commonly used pain rating scales. J. Clin. Nurs. 2005, 14, 798–804. [Google Scholar] [CrossRef]
- Cleeland, C.S. The Brief Pain Inventory User Guide; The University of Texas MD Anderson Cancer Center: Houston, TX, USA, 2009. [Google Scholar]
- Stanhope, J. Brief Pain Inventory review. Occup. Med. 2016, 66, 496–497. [Google Scholar] [CrossRef]
- Keller, S.; Bann, C.M.; Dodd, S.L.; Schein, J.; Mendoza, T.R.; Cleeland, C.S. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin. J. Pain 2004, 20, 309–318. [Google Scholar] [CrossRef]
- de Andrés Ares, J.; Cruces Prado, L.M.; Canos Verdecho, M.A.; Penide Villanueva, L.; Del Valle Hoyos, M.; Herdman, M.; Traseira Lugilde, S.; Velázquez Rivera, I. Validation of the Short Form of the Brief Pain Inventory (BPI-SF) in Spanish Patients with Non-Cancer-Related Pain. Pain Pract. 2015, 15, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef] [PubMed]
- Borisovskaya, A.; Chmelik, E.; Karnik, A. Exercise and Chronic Pain. Adv. Exp. Med. Biol. 2020, 1228, 233–253. [Google Scholar] [PubMed]
- Maddocks, M. Physical activity and exercise training in cancer patients. Clin. Nutr. ESPEN 2020, 40, 1–6. [Google Scholar] [CrossRef]
- Waltho, D.; Rockwell, G. Post-breast surgery pain syndrome: Establishing a consensus for the definition of post-mastectomy pain syndrome to provide a standardized clinical and research approach—A review of the literature and discussion. Can. J. Surg. 2016, 59, 342–350. [Google Scholar] [CrossRef]
- Capuco, A.; Urits, I.; Orhurhu, V.; Chun, R.; Shukla, B.; Burke, M.; Kaye, R.J.; Garcia, A.J.; Kaye, A.D.; Viswanath, O. A Comprehensive Review of the Diagnosis, Treatment, and Management of Postmastectomy Pain Syndrome. Curr. Pain Headache Rep. 2020, 24, 41. [Google Scholar] [CrossRef] [PubMed]
- Chappell, A.G.; Bai, J.; Yuksel, S.; Ellis, M.F. Post-Mastectomy Pain Syndrome: Defining Perioperative Etiologies to Guide New Methods of Prevention for Plastic Surgeons. World J. Plast. Surg. 2020, 9, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Bruce, J.; Poobalan, A.S.; Smith, W.C.; Chambers, W.A. Quantitative assessment of chronic postsurgical pain using the McGill Pain Questionnaire. Clin. J. Pain 2004, 20, 70–75. [Google Scholar] [CrossRef]
- Starkweather, A.R.; Lyon, D.E.; Schubert, C.M. Pain and inflammation in women with early-stage breast cancer prior to induction of chemotherapy. Biol. Res. Nurs. 2013, 15, 234–241. [Google Scholar] [CrossRef]
- Lee, E.; Nelson, O.L.; Puyana, C.; Takita, C.; Wright, J.L.; Zhao, W.; Reis, I.M.; Lin, R.Y.; Hlaing, W.M.; Bakalar, J.L.; et al. Association between C-reactive protein and radiotherapy-related pain in a tri-racial/ethnic population of breast cancer patients: A prospective cohort study. Breast Cancer Res. 2019, 21, 70. [Google Scholar] [CrossRef] [PubMed]
- Fazzari, J.; Sidhu, J.; Motkur, S.; Inman, M.; Buckley, N.; Clemons, M.; Vandermeer, L.; Singh, G. Applying Serum Cytokine Levels to Predict Pain Severity in Cancer Patients. J. Pain Res. 2020, 13, 313–321. [Google Scholar] [CrossRef]
- Spence, R.R.; Sandler, C.X.; Newton, R.U.; Galvão, D.A.; Hayes, S.C. Physical Activity and Exercise Guidelines for People With Cancer: Why Are They Needed, Who Should Use Them, and When? Semin. Oncol. Nurs. 2020, 36, 151075. [Google Scholar] [CrossRef] [PubMed]
- Friedenreich, C.M.; Neilson, H.K.; Farris, M.S.; Courneya, K.S. Physical Activity and Cancer Outcomes: A Precision Medicine Approach. Clin. Cancer Res. 2016, 22, 4766–4775. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Tchou, J. Barriers to rehabilitation following surgery for primary breast cancer. J. Surg. Oncol. 2007, 95, 409–418. [Google Scholar] [CrossRef]
- Johnsson, A.; Broberg, P.; Krüger, U.; Johnsson, A.; Tornberg, Å.B.; Olsson, H. Physical activity and survival following breast cancer. Eur. J. Cancer Care 2019, 28, e13037. [Google Scholar] [CrossRef] [PubMed]
- Arena, S.K.; Doherty, D.J.; Bellford, A.; Hayman, G. Effects of Aerobic Exercise on Oxidative Stress in Patients Diagnosed with Cancer: A Narrative Review. Cureus 2019, 11, e5382. [Google Scholar] [CrossRef] [PubMed]
- Hjermstad, M.J.; Fayers, P.M.; Haugen, D.F.; Caraceni, A.; Hanks, G.W.; Loge, J.H.; Fainsinger, R.; Aass, N.; Kaasa, S. European Palliative Care Research Collaborative (EPCRC). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: A systematic literature review. J. Pain Symptom Manag. 2011, 41, 1073–1093. [Google Scholar] [CrossRef]



| Group | Age (Years) | Education Level | Lymph Nodes Dissection | Marital Status | NRS |
|---|---|---|---|---|---|
| Non-PMP | 56.5 ± 10 | Secondary = 11.9% Post-secondary = 31.0% Graduation = 11.1% | 30.2% | 42.9% | 1.33 ± 1.73 |
| PMP | 56.5 ± 9.7 | Secondary = 9.5% Post-secondary = 23.0% Graduation = 13.5% | 34.9% | 40.5% | 5.27 ± 1.38 * |
| Non-PMP n = 68 | PMP n = 58 | |||
|---|---|---|---|---|
| 3 Months | 6 Months | 3 Months | 6 Months | |
| NRS score (intensity of pain) | 1.33 ± 1.73 | 1.33 ± 1.73 | 5.27 ± 1.38 * | 5.20 ± 1.16 * |
| BPI score (interference of pain) | 0.88 ± 1.26 | 0.77 ± 1.17 | 5.27 ± 1.25 * | 4.98 ± 1.20 * |
| CRP (mg/dL) | 0.14 ± 0.12 | 0.16 ± 0.14 | 0.53 ± 0.12 * | 0.49 ± 0.15 * |
| IL-6 (pg/mL) | 13.26 ± 2.11 | 12.32 ± 2.06 | 36.30 ± 11.40 * | 34.91 ± 11.51 * |
| IL-8 (pg/mL) | 12.44 ± 2.32 | 12.77 ± 2.31 | 50.20 ± 17.13 * | 48.86 ± 14.26 * |
| TNF- α (pg/mL) | 5.80 ± 2.22 | 5.6 ± 2.20 | 49.35 ± 19.37 * | 50.84 ± 12.95 * |
| SOD activity (U/mL) | 19.04 ± 1.47 | 18.54 ± 1.52 | 5.43 ± 4.35 * | 5.81 ± 4.38 * |
| CAT activity (U/mL) | 369.17 ± 1.47 | 344 ± 1.69 | 225.70 ± 38.11 * | 231.54 ± 37.95 * |
| MDA (pg/mL) | 31.32 ± 2.4 | 32.66 ± 2.11 | 801.45 ± 96.93 * | 798 ± 96.93 * |
| IPAQ Score | ||
|---|---|---|
| METs | PMP n = 58 | |
| 3 Months after Surgery | 6 Months after Surgery | |
| <700 (Inactive) (N = 26) | 451.9 ± 152.57 | 476.3 ± 172.83 |
| 700–2509 (Adequate active) (N = 32) | 1226.4 ± 445.06 * | 1233.9 ± 421.32 * |
| >2510 (Active) (N = 0) | N.D | N.D. |
| Inactive n = 26 | Adequate Active n = 32 | |||
|---|---|---|---|---|
| 3 Months | 6 Months | 3 Months | 6 Months | |
| NRS score (Intensity of pain) | 6.53 ± 0.85 | 6.11 ± 0.81 | 4.25 ± 0.71 * | 4.46 ± 0.84 * |
| BPI score (Interference of pain) | 6.15 ± 0.88 | 5.88 ± 0.99 | 4.56 ± 1.02 * | 4.25 ± 0.80 * |
| CRP (mg/dL) | 0.62 ± 0.10 | 0.60 ± 0.09 | 0.45 ± 0.07 * | 0.40 ± 0.12 * |
| IL-6 (pg/mL) | 44.91 ± 8.24 | 43.48 ± 11.23 | 29.31 ± 8.47 * | 27.95 ± 5.30 * |
| IL-8 (pg/mL) | 63.54 ± 10.34 | 59.33 ± 8.76 | 39.36 ± 13.52 * | 38.56 ± 14.08 * |
| TNF- α (pg/mL) | 64.73 ± 8.12 | 61.43 ± 5.93 | 36.85 ± 16.6 * | 41.55 ± 11.68 * |
| SOD activity (U/mL) | 4.71 ± 1.46 | 4.33 ± 1.15 | 4.84 ± 1.73 | 4.58 ± 1.67 * |
| CAT activity (U/mL) | 228.34 ± 33.97 | 223.40 ± 41.02 | 223.40 ± 41.02 | 228 ± 29.81 * |
| MDA (pg/mL) | 801.03 ± 70.90 | 830.76 ± 45.61 | 827.68 ± 59.33 | 832.62 ± 38.06 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calapai, M.; Puzzo, L.; Bova, G.; Vecchio, D.A.; Blandino, R.; Barbagallo, A.; Ammendolia, I.; Cardia, L.; De Pasquale, M.; Calapai, F.; et al. Effects of Physical Exercise and Motor Activity on Oxidative Stress and Inflammation in Post-Mastectomy Pain Syndrome. Antioxidants 2023, 12, 643. https://doi.org/10.3390/antiox12030643
Calapai M, Puzzo L, Bova G, Vecchio DA, Blandino R, Barbagallo A, Ammendolia I, Cardia L, De Pasquale M, Calapai F, et al. Effects of Physical Exercise and Motor Activity on Oxidative Stress and Inflammation in Post-Mastectomy Pain Syndrome. Antioxidants. 2023; 12(3):643. https://doi.org/10.3390/antiox12030643
Chicago/Turabian StyleCalapai, Marco, Luisa Puzzo, Giuseppe Bova, Daniele Alfio Vecchio, Rosario Blandino, Alessia Barbagallo, Ilaria Ammendolia, Luigi Cardia, Maria De Pasquale, Fabrizio Calapai, and et al. 2023. "Effects of Physical Exercise and Motor Activity on Oxidative Stress and Inflammation in Post-Mastectomy Pain Syndrome" Antioxidants 12, no. 3: 643. https://doi.org/10.3390/antiox12030643
APA StyleCalapai, M., Puzzo, L., Bova, G., Vecchio, D. A., Blandino, R., Barbagallo, A., Ammendolia, I., Cardia, L., De Pasquale, M., Calapai, F., Esposito, E., Trimarchi, F., Di Mauro, D., Calapai, G., & Mannucci, C. (2023). Effects of Physical Exercise and Motor Activity on Oxidative Stress and Inflammation in Post-Mastectomy Pain Syndrome. Antioxidants, 12(3), 643. https://doi.org/10.3390/antiox12030643








