Differential Effects of Very-Low-Volume Exercise Modalities on Telomere Length, Inflammation, and Cardiometabolic Health in Obese Metabolic Syndrome Patients: A Subanalysis from Two Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Pre- and Post-Intervention Examinations
2.2.1. Measurement of Blood Pressure
2.2.2. Sampling of Blood and Analyses
2.2.3. Determination of Telomere Length
2.2.4. Measurement of Anthropometric Values and Body Composition
2.2.5. Determination of the Metabolic Syndrome Severity Score
2.2.6. Cardiopulmonary Exercise Testing
2.3. Analysis of Food Intake and Nutritional Counseling
2.4. Exercise Protocols
2.4.1. Very-Low-Volume High-Intensity Interval Training
2.4.2. One-Set Resistance Training
2.4.3. Whole-Body Electromyostimulation Exercise
2.5. Statistical Analysis
3. Results
3.1. Study Flow, Training Data, Dietary Intakes, and Adverse Events
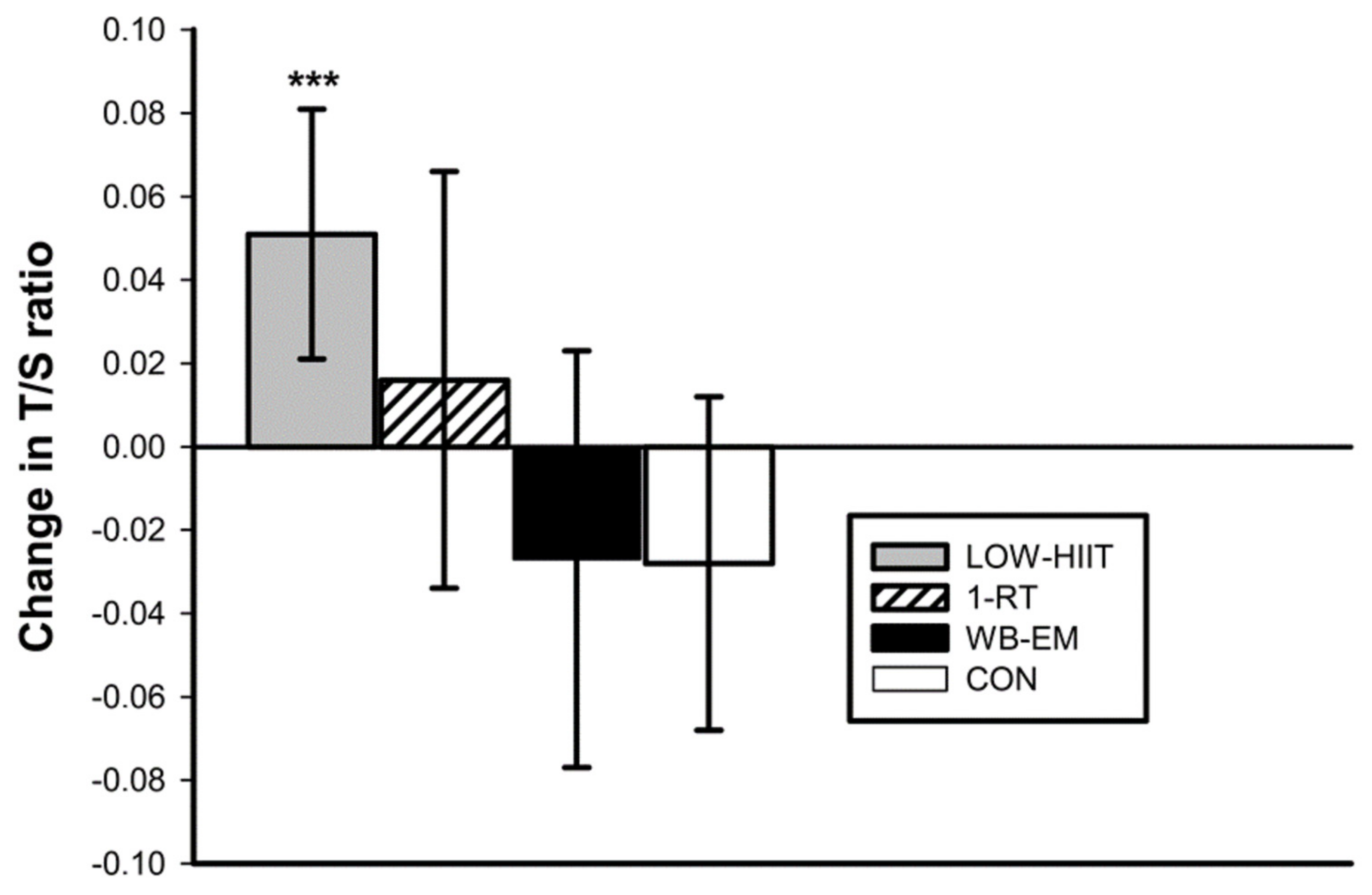
3.2. Telomere Length
3.3. Inflammatory Markers
3.4. Anthropometric Variables
3.5. Cardiometabolic Variables
3.6. Cardiorespiratory Fitness Variables
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, S.H.; Liu, W.; Ho, S.C. Metabolic syndrome and all-cause mortality: A meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 2010, 25, 375–384. [Google Scholar] [CrossRef]
- Saklayen, M.G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Noubiap, J.J.; Nansseu, J.R.; Lontchi-Yimagou, E.; Nkeck, J.R.; Nyaga, U.F.; Ngouo, A.T.; Tounouga, D.N.; Tianyi, F.L.; Foka, A.J.; Ndoadoumgue, A.L.; et al. Geographic distribution of metabolic syndrome and its components in the general adult population: A meta-analysis of global data from 28 million individuals. Diabetes Res. Clin. Pract. 2022, 188, 109924. [Google Scholar] [CrossRef] [PubMed]
- Auriemma, R.S.; Pirchio, R.; Liccardi, A.; Scairati, R.; Del Vecchio, G.; Pivonello, R.; Colao, A. Metabolic syndrome in the era of COVID-19 outbreak: Impact of lockdown on cardiometabolic health. J. Endocrinol. Investig. 2021, 44, 2845–2847. [Google Scholar] [CrossRef]
- Daniels, N.F.; Burrin, C.; Chan, T.; Fusco, F. A systematic review of the impact of the first year of COVID-19 on obesity risk factors: A pandemic fueling a pandemic? Curr. Dev. Nutr. 2022, 6, nzac011. [Google Scholar] [CrossRef]
- Xu, W.; Li, Y.; Yan, Y.; Zhang, L.; Zhang, J.; Yang, C. Effects of coronavirus disease 2019 lockdown on metabolic syndrome and its components among Chinese employees: A retrospective cohort study. Front. Public Health 2022, 10, 885013. [Google Scholar] [CrossRef] [PubMed]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef]
- Marott, S.C.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Benn, M. Components of the metabolic syndrome and risk of type 2 diabetes. J. Clin. Endocrinol. Metab. 2016, 101, 3212–3221. [Google Scholar] [CrossRef]
- Esposito, K.; Chiodini, P.; Colao, A.; Lenzi, A.; Giugliano, D. Metabolic syndrome and risk of cancer: A systematic review and meta-analysis. Diabetes Care 2012, 35, 2402–2411. [Google Scholar] [CrossRef]
- Monserrat-Mesquida, M.; Quetglas-Llabrés, M.; Capó, X.; Bouzas, C.; Mateos, D.; Pons, A.; Tur, J.A.; Sureda, A. Metabolic syndrome is associated with oxidative stress and proinflammatory state. Antioxidants 2020, 9, 236. [Google Scholar] [CrossRef]
- Fernández-Sánchez, A.; Madrigal-Santillán, E.; Bautista, M.; Esquivel-Soto, J.; Morales-González, A.; Esquivel-Chirino, C.; Durante-Montiel, I.; Sánchez-Rivera, G.; Valadez-Vega, C.; Morales-González, J.A. Inflammation, oxidative stress, and obesity. Int. J. Mol. Sci. 2011, 12, 3117–3132. [Google Scholar] [CrossRef]
- Liu, S.; Nong, W.; Ji, L.; Zhuge, X.; Wei, H.; Luo, M.; Zhou, L.; Chen, S.; Zhang, S.; Lei, X.; et al. The regulatory feedback of inflammatory signaling and telomere/telomerase complex dysfunction in chronic inflammatory diseases. Exp. Gerontol. 2023, 174, 112132. [Google Scholar] [CrossRef] [PubMed]
- Gavia-García, G.; Rosado-Pérez, J.; Arista-Ugalde, T.L.; Aguiñiga-Sánchez, I.; Santiago-Osorio, E.; Mendoza-Núñez, V.M. Telomere length and oxidative stress and its relation with metabolic syndrome components in the aging. Biology 2021, 10, 253. [Google Scholar] [CrossRef]
- Nannini, D.R.; Joyce, B.T.; Zheng, Y.; Gao, T.; Liu, L.; Yoon, G.; Huan, T.; Ma, J.; Jacobs, D.R., Jr.; Wilkins, J.T.; et al. Epigenetic age acceleration and metabolic syndrome in the coronary artery risk development in young adults study. Clin. Epigenet. 2019, 11, 160. [Google Scholar] [CrossRef]
- Lejawa, M.; Osadnik, K.; Osadnik, T.; Pawlas, N. Association of metabolically healthy and unhealthy obesity phenotypes with oxidative stress parameters and telomere length in healthy young adult men. Analysis of the MAGNETIC Study. Antioxidants 2021, 10, 93. [Google Scholar] [CrossRef]
- Vaiserman, A.; Krasnienkov, D. Telomere length as a marker of biological age: State-of-the-art, open issues, and future perspectives. Front. Genet. 2021, 11, 630186. [Google Scholar] [CrossRef]
- Galiè, S.; Canudas, S.; Muralidharan, J.; García-Gavilán, J.; Bulló, M.; Salas-Salvadó, J. Impact of nutrition on telomere health: Systematic review of observational cohort studies and randomized clinical trials. Adv. Nutr. 2020, 11, 576–601. [Google Scholar] [CrossRef]
- Schellnegger, M.; Lin, A.C.; Hammer, N.; Kamolz, L.P. Physical activity on telomere length as a biomarker for aging: A systematic review. Sports Med. Open. 2022, 8, 111. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, S.S.; Sousa, C.V.; Santos, P.A.; Barbosa, L.P.; Maciel, L.A.; Coelho-Júnior, H.J.; Motta-Santos, D.; Rosa, T.S.; Degens, H.; Simões, H.G. Master athletes have longer telomeres than age-matched non-athletes. A systematic review, meta-analysis and discussion of possible mechanisms. Exp. Gerontol. 2021, 146, 111212. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.M.; Hecksteden, A.; Morsch, A.; Zundler, J.; Wegmann, M.; Kratzsch, J.; Thiery, J.; Hohl, M.; Bittenbring, J.T.; Neumann, F.; et al. Differential effects of endurance, interval, and resistance training on telomerase activity and telomere length in a randomized, controlled study. Eur. Heart J. 2019, 40, 34–46. [Google Scholar] [CrossRef]
- Qiu, Y.; Fernández-García, B.; Lehmann, H.I.; Li, G.; Kroemer, G.; López-Otín, C.; Xiao, J. Exercise sustains the hallmarks of health. J. Sport Health Sci. 2023, 12, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Brashear, M.M.; Johnson, W.D.; Katzmarzyk, P.T. Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese U.S. men and women. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 60. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Cavallini, M.F.; Callaghan, M.E.; Premo, C.B.; Scott, J.W.; Dyck, D.J. Lack of time is the consistent barrier to physical activity and exercise in 18 to 64 year-old males and females from both South Carolina and Southern Ontario. J. Phys. Act. Res. 2020, 5, 100–106. [Google Scholar] [CrossRef]
- Herazo-Beltrán, Y.; Pinillos, Y.; Vidarte, J.; Crissien, E.; Suarez, D.; García, R. Predictors of perceived barriers to physical activity in the general adult population: A cross-sectional study. Braz. J. Phys. Ther. 2017, 21, 44–50. [Google Scholar] [CrossRef]
- Hoare, E.; Stavreski, B.; Jennings, G.L.; Kingwell, B.A. Exploring motivation and barriers to physical activity among active and inactive Australian adults. Sports 2017, 5, 47. [Google Scholar] [CrossRef]
- Gibala, M.J.; Little, J.P. Physiological basis of brief vigorous exercise to improve health. J. Physiol. 2020, 598, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Gibala, M.J.; Gillen, J.B.; Percival, M.E. Physiological and health-related adaptations to low-volume interval training: Influences of nutrition and sex. Sports Med. 2014, 44, S127–S137. [Google Scholar] [CrossRef]
- Gillen, J.B.; Gibala, M.J. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl. Physiol. Nutr. Metab. 2014, 39, 409–412. [Google Scholar] [CrossRef]
- Iversen, V.M.; Norum, M.; Schoenfeld, B.J.; Fimland, M.S. No time to lift? Designing time-efficient training programs for strength and hypertrophy: A narrative review. Sports Med. 2021, 51, 2079–2095. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Kleinöder, H.; Fröhlich, M. Editorial: Whole-body electromyostimulation: A training technology to improve health and performance in humans? Front. Physiol. 2020, 11, 523. [Google Scholar] [CrossRef]
- Reljic, D.; Dieterich, W.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. “HIIT the inflammation”: Comparative effects of low-volume interval training and resistance exercises on inflammatory indices in obese metabolic syndrome patients undergoing caloric restriction. Nutrients 2022, 14, 1996. [Google Scholar] [CrossRef]
- Reljic, D.; Frenk, F.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Maximum heart rate- and lactate threshold-based low-volume high-intensity interval training prescriptions provide similar health benefits in metabolic syndrome patients. Healthcare 2023, 11, 711. [Google Scholar] [CrossRef] [PubMed]
- Reljic, D.; Frenk, F.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Low-volume high-intensity interval training improves cardiometabolic health, work ability and well-being in severely obese individuals: A randomized-controlled trial sub-study. J. Transl. Med. 2020, 18, 419. [Google Scholar] [CrossRef]
- Reljic, D.; Frenk, F.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Effects of very low volume high intensity versus moderate intensity interval training in obese metabolic syndrome patients: A randomized controlled study. Sci. Rep. 2021, 11, 2836. [Google Scholar] [CrossRef] [PubMed]
- Reljic, D.; Konturek, P.C.; Herrmann, H.J.; Siebler, J.; Neurath, M.F.; Zopf, Y. Very low-volume interval training improves nonalcoholic fatty liver disease fibrosis score and cardiometabolic health in adults with obesity and metabolic syndrome. J. Physiol. Pharmacol. 2021, 72, 927–938. [Google Scholar] [CrossRef]
- Sabag, A.; Way, K.L.; Sultana, R.N.; Keating, S.E.; Gerofi, J.A.; Chuter, V.H.; Byrne, N.M.; Baker, M.K.; George, J.; Caterson, I.D.; et al. The effect of a novel low-volume aerobic exercise intervention on liver fat in type 2 diabetes: A randomized controlled trial. Diabetes Care 2020, 43, 2371–2378. [Google Scholar] [CrossRef]
- Winding, K.M.; Munch, G.W.; Iepsen, U.W.; Van Hall, G.; Pedersen, B.K.; Mortensen, S.P. The effect on glycaemic control of low-volume high-intensity interval training versus endurance training in individuals with type 2 diabetes. Diabetes Obes. Metab. 2018, 20, 1131–1139. [Google Scholar] [CrossRef]
- Alvarez, C.; Ramirez-Campillo, R.; Martinez-Salazar, C.; Mancilla, R.; Flores-Opazo, M.; Cano-Montoya, J.; Ciolac, E.G. Low-volume high-intensity interval training as a therapy for type 2 diabetes. Int. J. Sports Med. 2016, 37, 723–729. [Google Scholar] [CrossRef]
- Reljic, D.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Iron beats electricity: Resistance training but not whole-body electromyostimulation improves cardiometabolic health in obese metabolic syndrome patients during caloric restriction—A randomized-controlled study. Nutrients 2021, 13, 1640. [Google Scholar] [CrossRef]
- Little, J.P.; Gillen, J.B.; Percival, M.E.; Safdar, A.; Tarnopolsky, M.A.; Punthakee, Z.; Jung, M.E.; Gibala, M.J. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J. Appl. Physiol. 2011, 111, 1554–1560. [Google Scholar] [CrossRef] [PubMed]
- Madsen, S.M.; Thorup, A.C.; Overgaard, K.; Jeppesen, P.B. High intensity interval training improves glycaemic control and pancreatic β cell function of type 2 diabetes patients. PLoS ONE 2015, 10, e0133286. [Google Scholar] [CrossRef] [PubMed]
- Aristizabal, J.C.; Montoya, E.; Sánchez, Y.L.; Yepes-Calderón, M.; Narvaez-Sanchez, R.; Gallo-Villegas, J.A.; Calderón, J.C. Effects of low-volume, high-intensity interval training compared with continuous training on regional and global body composition in adults with metabolic syndrome: A post hoc analysis of a randomized clinical trial. Ann. Nutr. Metab. 2021, 77, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Reljic, D.; Konturek, P.C.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Effects of whole-body electromyostimulation exercise and caloric restriction on cardiometabolic risk profile and muscle strength in obese women with the metabolic syndrome: A pilot study. J. Physiol. Pharmacol. 2020, 71, 89–98. [Google Scholar] [CrossRef]
- Saghaei, M.; Saghaei, S. Implementation of an open-source customizable minimization program for allocation of patients to parallel groups in clinical trials. J. Biomed. Sci. Eng. 2011, 4, 734–739. [Google Scholar] [CrossRef]
- National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 8th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010; pp. 26–27. [Google Scholar]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 2018, 138, e426–e483. [Google Scholar] [CrossRef]
- Koller, A.; Brandl, C.; Lamina, C.; Zimmermann, M.E.; Summerer, M.; Stark, K.J.; Würzner, R.; Heid, I.M.; Kronenberg, F. Relative telomere length is associated with age-related macular degeneration in women. Invest. Ophthalmol. Vis. Sci. 2022, 63, 30. [Google Scholar] [CrossRef]
- Ruijter, J.M.; Ramakers, C.; Hoogaars, W.M.; Karlen, Y.; Bakker, O.; van den Hoff, M.J.; Moorman, A.F. Amplification efficiency: Linking baseline and bias in the analysis of quantitative PCR data. Nucleic Acids Res. 2009, 37, e45. [Google Scholar] [CrossRef]
- Bosy-Westphal, A.; Jensen, B.; Braun, W.; Pourhassan, M.; Gallagher, D.; Müller, M.J. Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8-electrode medical bioelectrical impedance devices. Eur. J. Clin. Nutr. 2017, 71, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.L.; Slentz, C.A.; Houmard, J.A.; Samsa, G.P.; Duscha, B.D.; Aiken, L.B.; McCartney, J.S.; Tanner, C.J.; Kraus, W.E. Exercise training amount and intensity effects on metabolic syndrome (from Studies of a Targeted Risk Reduction Intervention through Defined Exercise). Am. J. Cardiol. 2007, 100, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Earnest, C.P.; Artero, E.G.; Sui, X.; Lee, D.C.; Church, T.S.; Blair, S.N. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. Mayo Clin. Proc. 2013, 88, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Howley, E.T.; Bassett, D.R., Jr.; Welch, H.G. Criteria for maximal oxygen uptake: Review and commentary. Med. Sci. Sports Exerc. 1995, 27, 1292–1301. [Google Scholar] [CrossRef] [PubMed]
- Borg, G. Ratings of perceived exertion and heart rates during shortterm cycle exercise and their use in a new cycling strength test. Int. J. Sports Med. 1982, 3, 153–158. [Google Scholar] [CrossRef]
- Beaver, W.L.; Wasserman, K.; Whipp, B.J. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 1986, 60, 2020–2027. [Google Scholar] [CrossRef] [PubMed]
- Hausmann, M.; Heister, J.; Erdmann, J.; Schusdziarra, V. Stellenwert des 24-h-Recalls im Vergleich zum Ernährungsprotokoll in der Adipositasambulanz—Value of the 24-h-recall in comparison to dietary records in an obesity outpatient clinic. Aktuel. Ernaehr. Med. 2007, 32, 185–190. [Google Scholar] [CrossRef]
- Carels, R.A.; Young, K.M.; Coit, C.; Clayton, A.M.; Spencer, A.; Hobbs, M. Can following the caloric restriction recommendations from the Dietary Guidelines for Americans help individuals lose weight? Eat Behav. 2008, 9, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Al-Nimr, R.I. Optimal protein intake during weight loss interventions in older adults with obesity. J. Nutr. Gerontol. Geriatr. 2019, 38, 50–68. [Google Scholar] [CrossRef]
- Reljic, D.; Wittmann, F.; Fischer, J.E. Effects of low-volume high-intensity interval training in a community setting: A pilot study. Eur. J. Appl. Physiol. 2018, 118, 1153–1167. [Google Scholar] [CrossRef]
- Strauss, J.A.; Ranasinghe, C.; Cowley, E.; Schwingshackl, L.; Shepherd, S.O.; Chaplin, M.; Garner, P. High-intensity interval training for reducing cardiometabolic syndrome in healthy but sedentary populations. Cochrane Database Syst Rev. 2020, 2020, CD013617. [Google Scholar] [CrossRef]
- American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. 2009, 41, 687–708. [Google Scholar] [CrossRef]
- Lopez, P.; Radaelli, R.; Taaffe, D.R.; Newton, R.U.; Galvão, D.A.; Trajano, G.S.; Teodoro, J.L.; Kraemer, W.J.; Häkkinen, K.; Pinto, R.S. Resistance training load effects on muscle hypertrophy and strength gain: Systematic review and network meta-analysis. Med. Sci. Sports Exerc. 2021, 53, 1206–1216. [Google Scholar] [CrossRef]
- Mattocks, K.T.; Dankel, S.J.; Buckner, S.L.; Jessee, M.B.; Counts, B.R.; Mouser, J.G.; Laurentino, G.C.; Loenneke, J.P. Periodization: What is it good for? J. Trainol. 2016, 5, 6–12. [Google Scholar] [CrossRef]
- Kemmler, W.; Weissenfels, A.; Willert, S.; Shojaa, M.; von Stengel, S.; Filipovic, A.; Kleinöder, H.; Berger, J.; Fröhlich, M. Efficacy and safety of low frequency whole-body electromyostimulation (WB-EMS) to improve health-related outcomes in non-athletic adults. A systematic review. Front. Physiol. 2018, 9, 573. [Google Scholar] [CrossRef] [PubMed]
- Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Hernández-González, V.; Reverter-Masia, J. Effects of whole-body electromyostimulation on health and performance: A systematic review. BMC Complement. Altern. Med. 2019, 19, 87. [Google Scholar] [CrossRef]
- Kemmler, W.; Fröhlich, M.; Ludwig, O.; Eifler, C.; von Stengel, S.; Willert, S.; Teschler, M.; Weissenfels, A.; Kleinöder, H.; Micke, F.; et al. Position statement and updated international guideline for safe and effective whole-body electromyostimulation training-the need for common sense in WB-EMS application. Front. Physiol. 2023, 14, 1174103. [Google Scholar] [CrossRef]
- Borg, E.; Kaijser, L. A comparison between three rating scales for perceived exertion and two different work tests. Scand. J. Med. Sci. Sports 2006, 16, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Taylor and Francis: Routledge, UK, 1988. [Google Scholar]
- D’Mello, M.J.; Ross, S.A.; Briel, M.; Anand, S.S.; Gerstein, H.; Paré, G. Association between shortened leukocyte telomere length and cardiometabolic outcomes: Systematic review and meta-analysis. Circ. Cardiovasc. Genet. 2015, 8, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Sagris, M.; Theofilis, P.; Antonopoulos, A.S.; Tsioufis, K.; Tousoulis, D. Telomere length: A cardiovascular biomarker and a novel therapeutic target. Int. J. Mol. Sci. 2022, 23, 16010. [Google Scholar] [CrossRef]
- Yin, H.; Pickering, J.G. Telomere length: Implications for atherogenesis. Curr. Atheroscler. Rep. 2023, 25, 95–103. [Google Scholar] [CrossRef]
- Cheng, F.; Carroll, L.; Joglekar, M.V.; Januszewski, A.S.; Wong, K.K.; Hardikar, A.A.; Jenkins, A.J.; Ma, R.C. Diabetes, metabolic disease, and telomere length. Lancet Diabetes Endocrinol. 2021, 9, 117–126. [Google Scholar] [CrossRef]
- Shin, Y.A. How does obesity and physical activity affect aging?: Focused on telomere as a biomarker of aging. J. Obes. Metab. Syndr. 2019, 28, 92–104. [Google Scholar] [CrossRef]
- Nomikos, N.N.; Nikolaidis, P.T.; Sousa, C.V.; Papalois, A.E.; Rosemann, T.; Knechtle, B. Exercise, telomeres, and cancer: “the exercise-telomere hypothesis”. Front. Physiol. 2018, 9, 1798. [Google Scholar] [CrossRef] [PubMed]
- Rode, L.; Nordestgaard, B.G.; Bojesen, S.E. Peripheral blood leukocyte telomere length and mortality among 64,637 individuals from the general population. J. Natl. Cancer Inst. 2015, 107, djv074. [Google Scholar] [CrossRef] [PubMed]
- Willeit, P.; Willeit, J.; Mayr, A.; Weger, S.; Oberhollenzer, F.; Brandstätter, A.; Kronenberg, F.; Kiechl, S. Telomere length and risk of incident cancer and cancer mortality. JAMA 2010, 304, 69–75. [Google Scholar] [CrossRef]
- Deng, Y.; Li, Q.; Zhou, F.; Li, G.; Liu, J.; Lv, J.; Li, L.; Chang, D. Telomere length and the risk of cardiovascular diseases: A Mendelian randomization study. Front. Cardiovasc. Med. 2022, 9, 1012615. [Google Scholar] [CrossRef]
- Pauleck, S.; Sinnott, J.A.; Zheng, Y.L.; Gadalla, S.M.; Viskochil, R.; Haaland, B.; Cawthon, R.M.; Hoffmeister, A.; Hardikar, S. Association of telomere length with colorectal cancer risk and prognosis: A systematic review and meta-analysis. Cancers 2023, 15, 1159. [Google Scholar] [CrossRef]
- Zhang, C.; Chen, X.; Li, L.; Zhou, Y.; Wang, C.; Hou, S. The Association between telomere length and cancer prognosis: Evidence from a meta-analysis. PLoS ONE 2015, 10, e0133174. [Google Scholar] [CrossRef]
- Schneider, C.V.; Schneider, K.M.; Teumer, A.; Rudolph, K.L.; Hartmann, D.; Rader, D.J.; Strnad, P. Association of telomere length with risk of disease and mortality. JAMA Intern. Med. 2022, 182, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Balan, E.; Decottignies, A.; Deldicque, L. Physical activity and nutrition: Two promising strategies for telomere maintenance? Nutrients 2018, 10, 1942. [Google Scholar] [CrossRef] [PubMed]
- Fernández de la Puente, M.; Hernández-Alonso, P.; Canudas, S.; Marti, A.; Fitó, M.; Razquin, C.; Salas-Salvadó, J. Modulation of telomere length by mediterranean diet, caloric restriction, and exercise: Results from PREDIMED-Plus Study. Antioxidants 2021, 10, 1596. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Sng, E. Mode-specific physical activity and leukocyte telomere length among U.S. adults: Implications of running on cellular aging. Prev. Med. 2016, 85, 17–19. [Google Scholar] [CrossRef]
- Ogawa, E.F.; Leveille, S.G.; Wright, J.A.; Shi, L.; Camhi, S.M.; You, T. Physical activity domains/recommendations and leukocyte telomere length in U.S. adults. Med. Sci. Sports Exerc. 2017, 49, 1375–1382. [Google Scholar] [CrossRef] [PubMed]
- Tucker, L.A. Physical activity and telomere length in U.S. men and women: An NHANES investigation. Prev. Med. 2017, 100, 145–151. [Google Scholar] [CrossRef]
- Du, M.; Prescott, J.; Kraft, P.; Han, J.; Giovannucci, E.; Hankinson, S.E.; De Vivo, I. Physical activity, sedentary behavior, and leukocyte telomere length in women. Am. J. Epidemiol. 2012, 175, 414–422. [Google Scholar] [CrossRef]
- Saßenroth, D.; Meyer, A.; Salewsky, B.; Kroh, M.; Norman, K.; Steinhagen-Thiessen, E.; Demuth, I. Sports and exercise at different ages and leukocyte telomere length in later life-data from the Berlin Aging Study II (BASE-II). PLoS ONE 2015, 10, e0142131. [Google Scholar] [CrossRef]
- Shadyab, A.H.; LaMonte, M.J.; Kooperberg, C.; Reiner, A.P.; Carty, C.L.; Manini, T.M.; Hou, L.; Di, C.; LaCroix, A.Z. Association of accelerometer-measured physical activity with leukocyte telomere length among older women. J. Gerontol. 2017, 72, 1532–1537. [Google Scholar] [CrossRef] [PubMed]
- Stenbäck, V.; Mutt, S.J.; Leppäluoto, J.; Gagnon, D.D.; Mäkelä, K.A.; Jokelainen, J.; Keinänen-Kiukaanniemi, S.; Herzig, K.H. Association of physical activity with telomere length among elderly adults—The Oulu Cohort 1945. Front. Physiol. 2019, 10, 444. [Google Scholar] [CrossRef]
- Cherkas, L.F.; Hunkin, J.L.; Kato, B.S.; Richards, J.B.; Gardner, J.P.; Surdulescu, G.L.; Kimura, M.; Lu, X.; Spector, T.D.; Aviv, A. The association between physical activity in leisure time and leukocyte telomere length. Arch. Intern. Med. 2008, 168, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Sillanpää, E.; Törmäkangas, T.; Rantanen, T.; Kaprio, J.; Sipilä, S. Does telomere length predict decline in physical functioning in older twin sisters during an 11-year follow-up? Age 2016, 38, 34. [Google Scholar] [CrossRef]
- Eigendorf, J.; Melk, A.; Haufe, S.; Boethig, D.; Berliner, D.; Kerling, A.; Kueck, M.; Stenner, H.; Bara, C.; Stiesch, M.; et al. Effects of personalized endurance training on cellular age and vascular function in middle-aged sedentary women. Eur. J. Prev. Cardiol. 2019, 26, 1903–1906. [Google Scholar] [CrossRef]
- Mosallanezhad, Z.; Hemmatinafar, M.; Sotoodeh, A.; Erfanian, S. The effect of high-intensity interval training on telomere length, telomerase, and telomere related factors of leukocytes in sedentary young women. J. Urmia Univ. Med. Sci. 2019, 29, 913–919. [Google Scholar]
- Noorimofrad, S.; Ebrahim, K. The effect of high intensity interval training on telomere length and telomerase activity in non-athlete young men. J. Bas. Res. Med. Sci. 2018, 5, 1–7. [Google Scholar] [CrossRef][Green Version]
- Puterman, E.; Weiss, J.; Lin, J.; Schilf, S.; Slusher, A.L.; Johansen, K.L.; Epel, E.S. Aerobic exercise lengthens telomeres and reduces stress in family caregivers: A randomized controlled trial—Curt Richter Award Paper 2018. Psychoneuroendocrinology 2018, 98, 245–252. [Google Scholar] [CrossRef]
- Friedenreich, C.M.; Wang, Q.; Ting, N.S.; Brenner, D.R.; Conroy, S.M.; McIntyre, J.B.; Mickle, A.; Courneya, K.S.; Beattie, T. Effect of a 12-month exercise intervention on leukocyte telomere length: Results from the ALPHA Trial. Cancer Epidemiol. 2018, 56, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Hagstrom, A.D.; Denham, J. The effect of resistance training on telomere length in women recovering from breast cancer. J. Funct. Morphol. Kinesiol. 2018, 3, 9. [Google Scholar] [CrossRef]
- Mason, C.; Risques, R.A.; Xiao, L.; Duggan, C.R.; Imayama, I.; Campbell, K.L.; Kong, A.; Foster-Schubert, K.E.; Wang, C.Y.; Alfano, C.M.; et al. Independent and combined effects of dietary weight loss and exercise on leukocyte telomere length in postmenopausal women. Obesity 2013, 21, E549–E554. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, V.B.; Pedroso, D.C.; Kogure, G.S.; Lopes, I.P.; Santana, B.A.; Dutra de Souza, H.C.; Ferriani, R.A.; Calado, R.T.; Furtado, C.L.; Reis, R.M. Short-term aerobic exercise did not change telomere length while it reduced testosterone levels and obesity indexes in PCOS: A randomized controlled clinical trial study. Int. J. Environ. Res. Public Health 2021, 18, 11274. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.A.; Lee, J.H.; Song, W.; Jun, T.W. Exercise training improves the antioxidant enzyme activity with no changes of telomere length. Mech. Ageing Dev. 2008, 129, 254–260. [Google Scholar] [CrossRef]
- Tosevska, A.; Franzke, B.; Hofmann, M.; Vierheilig, I.; Schober-Halper, B.; Oesen, S.; Neubauer, O.; Wessner, B.; Wagner, K.H. Circulating cell-free DNA, telomere length and bilirubin in the Vienna Active Ageing Study: Exploratory analysis of a randomized, controlled trial. Sci. Rep. 2016, 6, 38084. [Google Scholar] [CrossRef]
- Krzysztofik, M.; Wilk, M.; Wojdała, G.; Gołaś, A. Maximizing muscle hypertrophy: A systematic review of advanced resistance training techniques and methods. Int. J. Environ. Res. Public Health 2019, 16, 4897. [Google Scholar] [CrossRef]
- Shailendra, P.; Baldock, K.L.; Li, L.S.; Bennie, J.A.; Boyle, T. Resistance training and mortality risk: A systematic review and meta-analysis. Am. J. Prev. Med. 2022, 63, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.; Fürster, T.; Widmann, T.; Pöss, J.; Roggia, C.; Hanhoun, M.; Scharhag, J.; Büchner, N.; Meyer, T.; Kindermann, W.; et al. Physical exercise prevents cellular senescence in circulating leukocytes and in the vessel wall. Circulation 2009, 120, 2438–2447. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, R.; Sharifi, M.; Khosravi, A.; Adeli, K. Relationship between C-reactive protein and atherosclerotic risk factors and oxidative stress markers among young persons 10–18 years old. Clin. Chem. 2007, 53, 456–464. [Google Scholar] [CrossRef]
- Park, S.; Kim, M.; Paik, J.K.; Jang, Y.J.; Lee, S.H.; Lee, J.H. Oxidative stress is associated with C-reactive protein in nondiabetic postmenopausal women, independent of obesity and insulin resistance. Clin. Endocrinol. 2013, 79, 65–70. [Google Scholar] [CrossRef]
- Didion, S.P. Cellular and oxidative mechanisms associated with interleukin-6 signaling in the vasculature. Int. J. Mol. Sci. 2017, 18, 2563. [Google Scholar] [CrossRef]
- Escribano, B.M.; Medina-Fernández, F.J.; Aguilar-Luque, M.; Agüera, E.; Feijoo, M.; Garcia-Maceira, F.I.; Lillo, R.; Vieyra-Reyes, P.; Giraldo, A.I.; Luque, E.; et al. Lipopolysaccharide binding protein and oxidative stress in a multiple sclerosis model. Neurotherapeutics 2017, 14, 199–211. [Google Scholar] [CrossRef]
- Kordinas, V.; Ioannidis, A.; Chatzipanagiotou, S. The telomere/telomerase system in chronic inflammatory diseases. Cause or effect? Genes 2016, 7, 60. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Colon, M.; Hodgson, A.; Donlon, E.; Murphy, J.E. Effects of competitive triathlon training on telomere length. J. Aging Phys. Act. 2019, 27, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Sellami, M.; Al-Muraikhy, S.; Al-Jaber, H.; Al-Amri, H.; Al-Mansoori, L.; Mazloum, N.A.; Donati, F.; Botre, F.; Elrayess, M.A. Age and sport intensity-dependent changes in cytokines and telomere length in elite athletes. Antioxidants 2021, 10, 1035. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.; Gouveira, É.R.; Peralta, M.; Martins, J.; Venturini, J.; Henriques-Neto, D.; Sarmento, H. Cardiorespiratory fitness and telomere length: A systematic review. J. Sports Sci. 2020, 38, 1690–1697. [Google Scholar] [CrossRef] [PubMed]
- Gormley, S.E.; Swain, D.P.; High, R.; Spina, R.J.; Dowling, E.A.; Kotipalli, U.S.; Gandrakota, R. Effect of intensity of aerobic training on VO2max. Med. Sci. Sports Exerc. 2008, 40, 1336–1343. [Google Scholar] [CrossRef] [PubMed]
- Milanović, Z.; Sporiš, G.; Weston, M. Effectiveness of high-intensity interval training (HIT) and continuous endurance training for VO2max improvements: A systematic review and meta-analysis of controlled trials. Sports Med. 2015, 45, 1469–1481. [Google Scholar] [CrossRef]
- Okamura, M.; Shimizu, M.; Yamamoto, S.; Nishie, K.; Konishi, M. High-intensity interval training versus moderate-intensity continuous training in patients with heart failure: A systematic review and meta-analysis. Heart Fail. Rev. 2023, 28, 1113–1128. [Google Scholar] [CrossRef]
- Powers, S.K.; Deminice, R.; Ozdemir, M.; Yoshihara, T.; Bomkamp, M.P.; Hyatt, H. Exercise-induced oxidative stress: Friend or foe? J. Sport Health Sci. 2020, 9, 415–425. [Google Scholar] [CrossRef]
- Lu, Y.; Wiltshire, H.D.; Baker, J.S.; Wang, Q. Effects of high intensity exercise on oxidative stress and antioxidant status in untrained humans: A systematic review. Biology 2021, 10, 1272. [Google Scholar] [CrossRef]
- Bogdanis, G.C.; Stavrinou, P.; Fatouros, I.G.; Philippou, A.; Chatzinikolaou, A.; Draganidis, D.; Ermidis, G.; Maridaki, M. Short-term high-intensity interval exercise training attenuates oxidative stress responses and improves antioxidant status in healthy humans. Food Chem. Toxicol. 2013, 61, 171–177. [Google Scholar] [CrossRef]
- Poblete Aro, C.E.; Russell Guzmán, J.A.; Soto Muñoz, M.E.; Villegas González, B.E. Effects of high intensity interval training versus moderate intensity continuous training on the reduction of oxidative stress in type 2 diabetic adult patients: CAT. Medwave 2015, 15, e6212. [Google Scholar] [CrossRef]
- Knox, E.C.; Webb, O.J.; Esliger, D.W.; Biddle, S.J.; Sherar, L.B. Using threshold messages to promote physical activity: Implications for public perceptions of health effects. Eur. J. Public Health 2014, 24, 195–199. [Google Scholar] [CrossRef]
- Reljic, D.; Lampe, D.; Wolf, F.; Zopf, Y.; Herrmann, H.J.; Fischer, J. Prevalence and predictors of dropout from high-intensity interval training in sedentary individuals: A meta-analysis. Scand. J. Med. Sci. Sports 2019, 29, 1288–1304. [Google Scholar] [CrossRef]
- Nettleton, J.A.; Diez-Roux, A.; Jenny, N.S.; Fitzpatrick, A.L.; Jacobs, D.R., Jr. Dietary patterns, food groups, and telomere length in the Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Clin. Nutr. 2008, 88, 1405–1412. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, T.; Mertens, D.J.; Hamm, L.F.; Beyene, J.; Kennedy, J.; Corey, P.; Shephard, R.J. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation 2002, 106, 666–671. [Google Scholar] [CrossRef]
- Law, M.R.; Morris, J.K.; Wald, N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009, 338, b1665. [Google Scholar] [CrossRef]
- Higgs, C.; Skinner, M.; Hale, L. Outcomes of a community-based lifestyle programme for adults with diabetes or pre-diabetes. J. Prim. Health Care 2016, 8, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Gasteyger, C.; Larsen, T.M.; Vercruysse, F.; Pedersen, D.; Toubro, S.; Astrup, A. Visceral fat loss induced by a low-calorie diet: A direct comparison between women and men. Diabetes Obes. Metab. 2009, 11, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Wirth, A.; Steinmetz, B. Gender differences in changes in subcutaneous and intra-abdominal fat during weight reduction: An ultrasound study. Obes. Res. 1998, 6, 393–399. [Google Scholar] [CrossRef]
- Strasser, B.; Schobersberger, W. Evidence for resistance training as a treatment therapy in obesity. J. Obes. 2011, 2011, 482564. [Google Scholar] [CrossRef] [PubMed]
- Westcott, W.L. Resistance training is medicine: Effects of strength training on health. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef]
- Crane, M.M.; Jeffery, R.W.; Sherwood, N.E. Exploring gender differences in a randomized trial of weight loss maintenance. Am. J. Men’s Health 2017, 11, 369–375. [Google Scholar] [CrossRef]
- Gill, R.S.; Karmali, S.; Hadi, G.; Al-Adra, D.P.; Shi, X.; Birch, D.W. Predictors of attrition in a multidisciplinary adult weight management clinic. Can. J. Surg. 2012, 55, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.B.; Herrick, K.A.; Sarafrazi, N.; Ogden, C.L. Attempts to lose weight among adults in the United States, 2013–2016. NCHS Data Brief 2018, 313, 1–8. [Google Scholar]
- Taylor, J.L.; Holland, D.J.; Spathis, J.G.; Beetham, K.S.; Wisløff, U.; Keating, S.E.; Coombes, J.S. Guidelines for the delivery and monitoring of high intensity interval training in clinical populations. Prog. Cardiovasc. Dis. 2019, 62, 140–146. [Google Scholar] [CrossRef] [PubMed]
| Variable | LV-HIIT (n = 52) | 1-RT (n = 19) | WB-EMS (n = 22) | CON (n = 30) |
|---|---|---|---|---|
| Age (years) | 53 (49 to 57) | 55 (50 to 60) | 52 (47 to 57) | 51 (46 to 57) |
| Sex, male/female (n) | 21/31 | 4/15 | 8/14 | 8/22 |
| Educational level | ||||
| Low 1 (n) | 13 (25%) | 4 (21%) | 7 (32%) | 9 (30%) |
| Medium 2 (n) | 19 (37%) | 9 (47%) | 8 (36%) | 12 (40%) |
| High 3 (n) | 20 (38%) | 6 (32%) | 7 (32%) | 9 (30%) |
| Anthropometric variables | ||||
| Body weight (kg) | 108.6 (102.3 to 114.9) | 106.0 (92.4 to 119.5) | 108.5 (98.9 to 116.3) | 105.9 (98.7 to 112.9) |
| Body mass index (kg/m2) | 37.5 (35.6 to 39.4) | 38.1 (34.3 to 42.0) | 37.7 (35.6 to 39.6) | 37.4 (35.4 to 39.4) |
| Body fat (%) | 44.0 (42.0 to 45.9) | 46.6 (44.1 to 49.1) | 44.0 (42.0 to 46.4) | 45.2 (42.9 to 48.0) |
| Waist circumference (cm) | 112 (108 to 116) | 111 (103 to 119) | 114 (109 to 119) | 110 (106 to 114) |
| Blood pressure | ||||
| SBP (mmHg) | 140 (135 to 144) | 146 (138 to 154) | 137 (130 to 143) | 135 (136 to 142) |
| DBP (mmHg) | 89 (87 to 92) | 90 (83 to 97) | 87 (83 to 91) | 86 (82 to 90) |
| MAB (mmHg) | 106 (103 to 109) | 109 (103 to 115) | 103 (99 to 108) | 103 (98 to 107) |
| Inflammatory markers | ||||
| CRP (mg/L) | 5.5 (4.1 to 7.0) | 5.1 (2.2 to 8.0) | 3.9 (2.8 to 5.1) | 3.9 (2.6 to 5.2) |
| IL-1β (pg/mL) | 4.8 (3.5 to 6.1) | 8.3 (3.4 to 13.1) | 8.9 (7.1 to 10.7) | 6.7 (4.8 to 8.6) |
| IL-6 (pg/mL) | 3.0 (2.3 to 3.7) | 2.8 (1.9 to 3.7) | 2.6 (2.0 to 3.2) | 3.0 (2.3 to 3.8) |
| INFγ (pg/mL) | 8.6 ± 5.5 | 7.0 ± 4.4 | 7.3 ± 2.9 | 8.1 ± 4.5 |
| Adiponectin (µg/mL) | 2.5 (2.0 to 3.0) | 4.1 (2.4 to 5.8) | 2.5 (1.8 to 3.1) | 2.7 (2.1 to 3.3) |
| LBP (ng/mL) | 12.5 ± 3.4 | 30.3 ± 7.8 | 23.0 ± 6.4 | 16.2 ± 8.4 |
| Clinical chemistry | ||||
| Glucose (mg/dL) | 104 (98 to 110) | 98 (91 to 106) | 104 (98 to 109) | 100 (93 to 107) |
| HbA1c (%) | 5.7 (5.5 to 5.9) | 5.6 (5.4 to 5.8) | 5.7 (5.4 to 5.9) | 5.6 (5.3 to 5.9) |
| Triglycerides (mg/dL) | 136 (117 to 156) | 123 (105 to 141) | 132 (105 to 159) | 155 (125 to 183) |
| Cholesterol (mg/dL) | 213 (203 to 223) | 229 (216 to 243) | 222 (207 to 238) | 228 (213 to 246) |
| HDL (mg/dL) | 49 (46 to 52) | 59 (51 to 67) | 55 (49 to 61) | 55 (50 to 60) |
| LDL (mg/dL) | 142 (134 to 150) | 150 (139 to 161) | 146 (133 to 158) | 147 (135 to 160) |
| MetS z-score | 2.6 (1.6 to 3.7) | 2.1 (1.3 to 3.9) | 2.3 (1.1 to 3.3) | 1.9 (1.2 to 3.0) |
| CPET variables | ||||
| VO2max (L) | 2.31 (2.13 to 2.49) | 2.10 (1.83 to2.37) | 2.30 (2.01 to 2.55) | 2.18 (1.86 to 2.49) |
| VO2max (mL/kg/min) | 21.5 (20.1 to 23.1) | 20.3 (17.9 to 22.7) | 21.1 (19.2 to 24.1) | 20.4 (17.9 to 23.0) |
| Wmax (W) | 146 (134 to 157) | 158 (139 to 177) | 167 (142 to 189) | 153 (130 to 176) |
| WVT (W) | 58 (51 to 65) | 78 (65 to 90) | 72 (63 to 82) | 67 (56 to 80) |
| Dietary inakes | ||||
| Energy (kcal) | 2144 (1885 to 2415) | 2297 (1898 to 2696) | 2448 (2127 to 2770) | 2249 (1936 to 2564) |
| Protein (g/kg) | 0.9 (0.7 to 1.1) | 1.0 (0.8 to 1.1) | 1.0 (0.8 to 1.1) | 0.9 (0.7 to 1.1) |
| Fat (g/kg) | 0.8 (0.7 to 0.9) | 0.9 (0.8 to 1.0) | 1.0 (0.8 to 1.2) | 0.9 (0.8 to 1.1) |
| Carbohydrates (g/kg) | 2.0 (1.8 to 2.3) | 2.1 (1.9 to 2.4) | 2.4 (1.9 to 2.8) | 2.1 (1.7 to 2.5) |
| Variable | LV-HIIT (n = 52) | 1-RT (n = 19) | WB-EMS (n = 22) | CON (n = 30) |
|---|---|---|---|---|
| CRP (mg/L) | −1.5 (−2.8 to −0.2) * | 0 (−0.6 to 0.6) | −0.4 (−1.1 to 0.4) | 1.5 (−1.1 to 4.2) |
| p-value | 0.015 | 0.943 | 0.311 | 0.243 |
| IL-6 (pg/mL) | −0.6 (−1.1 to −0.1) * | −0.2 (−0.8 to 0.3) | −0.3 (−0.8 to 0.2) | 0.7 (−0.4 to 1.8) |
| p-value | 0.014 | 0.410 | 0.242 | 0.182 |
| LBP (ng/mL) | −1.4 (−2.5 to −0.3) | −1.2 (−3.0 to 0.7) | −0.2 (−1.2 to 0.7) | 0.2 (−0.9 to 1.3) |
| p-value | 0.009 | 0.193 | 0.604 | 0.696 |
| Variable | LV-HIIT (n = 52) | 1-RT (n = 19) | WB-EMS (n = 22) | CON (n = 30) |
|---|---|---|---|---|
| Anthropometric variables | ||||
| Body weight (kg) | −3.8 (−5.1 to −2.5) | −3.0 (−5.6 to −0.5) | −4.2 (−5.8 to −2.5) | −2.8 (−3.7 to −1.9) |
| p-value | <0.001 | 0.012 | <0.001 | <0.001 |
| Body mass index (kg/m2) | −1.3 (−1.7 to −0.9) | −1.1 (−2.0 to −0.2) | −1.4 (−2.0 to −0.9) | −1.0 (−1.3 to −0.7) |
| p-value | <0.001 | 0.012 | <0.001 | <0.001 |
| Body fat (%) | −1.4 (−2.1 to −0.6) | −1.2 (−2.0 to −0.4) | −0.9 (−1.6 to −0.3) | −1.0 (−1.8 to −0.3) |
| p-value | <0.001 | 0.002 | 0.005 | 0.003 |
| Waist circumference (cm) | −6 (−7 to −4) ** | −5 (−8 to −2) | −3 (−5 to −1) | −1 (−3 to 1) |
| p-value | <0.001 | 0.001 | 0.001 | 0.054 |
| Blood pressure | ||||
| SBP (mmHg) | −10 (−14 to −7) ** | −9 (−17 to −1) | −3 (−10 to 4) | 1 (−4 to 6) |
| p-value | <0.001 | 0.024 | 0.193 | 0.335 |
| DBP (mmHg) | −6 (−8 to −4) ** ## | −4 (−11 to −2) | 2 (−1 to 5) | 0 (−3 to 3) |
| p-value | <0.001 | 0.085 | 0.056 | 0.769 |
| MAB (mmHg) | −8 (−10 to −5) *** ## | −6 (−12 to −1) * | 0 (−2 to 2) | 1 (−3 to 4) |
| p-value | <0.001 | 0.018 | 0.468 | 0.694 |
| Clinical chemistry | ||||
| HbA1c (%) | −0.1 (−0.2 to 0) | 0 (−0.1 to 0) | −0.1 (−0.2 to 0) | 0 (−0.1 to 0) |
| p-value | 0.036 | 0.240 | 0.010 | 0.113 |
| Cholesterol (mg/dL) | −1 (−8 to 7) | −7 (−16 to 2) | −8 (−16 to −1) | −9 (−18 to 0) |
| p-value | 0.438 | 0.054 | 0.017 | 0.023 |
| LDL (mg/dL) | −1 (−7 to 6) | −7 (−15 to 1) | −6 (−14 to 1) | −4 (−9 to 3) |
| p-value | 0.453 | 0.033 | 0.043 | 0.114 |
| MetS z-score | −1.8 (−2.3 to −1.4) ** | −1.1 (−2.1 to −0.1) | −0.4 (−0.9 to 0.2) | −0.5 (−1.2 to 0.2) |
| p-value | <0.001 | 0.014 | 0.080 | 0.087 |
| Variable | LV-HIIT (n = 52) | 1-RT (n = 19) | WB-EMS (n = 22) | CON (n = 30) |
|---|---|---|---|---|
| CPET variables | ||||
| VO2max (L) | 0.21 (0.14 to 0.27) *** †† | 0.08 (−0.07 to 0.23) | 0.05 (−0.04 to 0.13) | −0.13 (−2.5 to −0.01) |
| p-value | <0.001 | 0.148 | 0.266 | 0.014 |
| VO2max (mL/kg/min) | 2.9 (2.1 to 3.7) *** † | 1.2 (−0.1 to 2.4) | 1.4 (0.5 to 3.1) | −0.2 (−0.8 to 0.4) |
| p-value | <0.001 | 0.068 | 0.055 | 0.519 |
| Wmax (W) | 22 (18 to 26) *** ††† | 6 (−1 to 13) * | 8 (3 to 12) * | −4 (−8 to −0) |
| p-value | <0.001 | 0.090 | 0.003 | 0.020 |
| WVT (W) | 21 (16 to 25) *** # | 3 (−4 to 11) | 7 (2 to 12) | −2 (−6 to 2) |
| p-value | <0.001 | 0.370 | 0.010 | 0.345 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reljic, D.; Koller, A.; Herrmann, H.J.; Ekici, A.B.; Neurath, M.F.; Zopf, Y. Differential Effects of Very-Low-Volume Exercise Modalities on Telomere Length, Inflammation, and Cardiometabolic Health in Obese Metabolic Syndrome Patients: A Subanalysis from Two Randomized Controlled Trials. Antioxidants 2023, 12, 1847. https://doi.org/10.3390/antiox12101847
Reljic D, Koller A, Herrmann HJ, Ekici AB, Neurath MF, Zopf Y. Differential Effects of Very-Low-Volume Exercise Modalities on Telomere Length, Inflammation, and Cardiometabolic Health in Obese Metabolic Syndrome Patients: A Subanalysis from Two Randomized Controlled Trials. Antioxidants. 2023; 12(10):1847. https://doi.org/10.3390/antiox12101847
Chicago/Turabian StyleReljic, Dejan, Adriana Koller, Hans J. Herrmann, Arif B. Ekici, Markus F. Neurath, and Yurdagül Zopf. 2023. "Differential Effects of Very-Low-Volume Exercise Modalities on Telomere Length, Inflammation, and Cardiometabolic Health in Obese Metabolic Syndrome Patients: A Subanalysis from Two Randomized Controlled Trials" Antioxidants 12, no. 10: 1847. https://doi.org/10.3390/antiox12101847
APA StyleReljic, D., Koller, A., Herrmann, H. J., Ekici, A. B., Neurath, M. F., & Zopf, Y. (2023). Differential Effects of Very-Low-Volume Exercise Modalities on Telomere Length, Inflammation, and Cardiometabolic Health in Obese Metabolic Syndrome Patients: A Subanalysis from Two Randomized Controlled Trials. Antioxidants, 12(10), 1847. https://doi.org/10.3390/antiox12101847








