Vanadium(IV)-Chlorodipicolinate Protects against Hepatic Steatosis by Ameliorating Lipid Peroxidation, Endoplasmic Reticulum Stress, and Inflammation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Animal Experiments
2.3. Biochemical Parameter Tests
2.4. Histopathological Examination
2.5. RNA-Sequencing (RNA-seq)
2.6. Quantitative Real-Time PCR and Western Blot Analyses
2.7. Statistical Analysis
3. Results
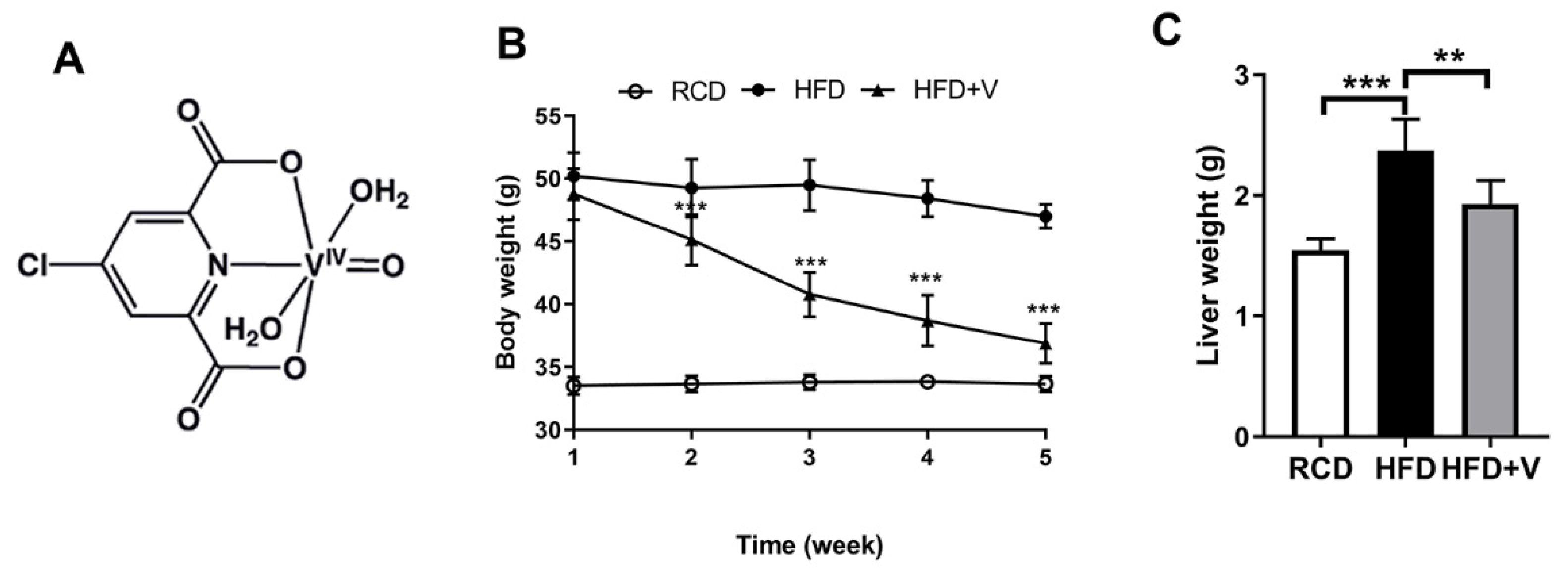
3.1. VOdipic-Cl Regulates Body Weight and Liver Weight in Obese Mice
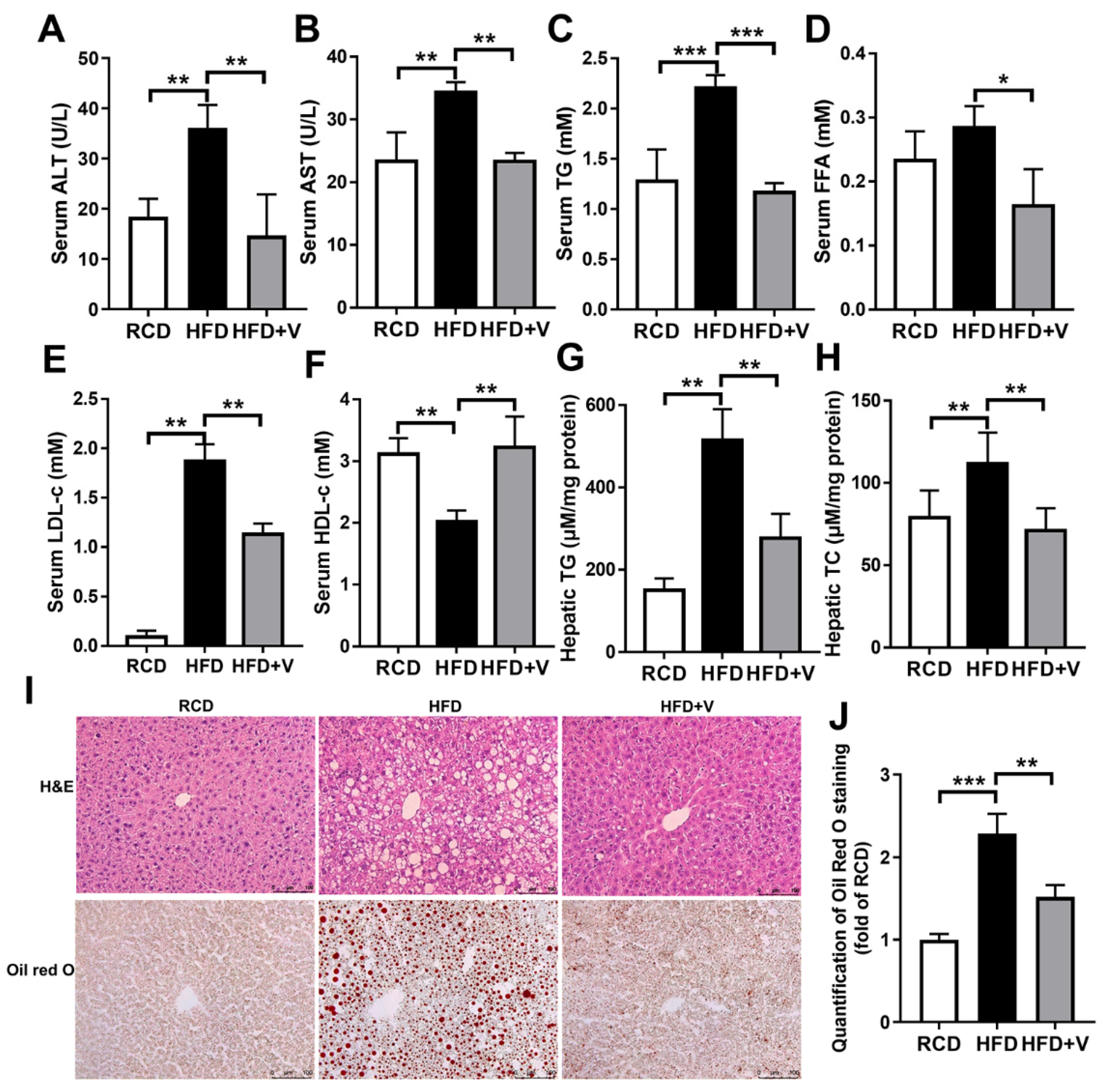
3.2. VOdipic-Cl Ameliorates HFD-Induced Liver Steatosis in Obese Mice
3.3. VOdipic-Cl Attenuates HFD-Induced Hepatic Oxidative Stress
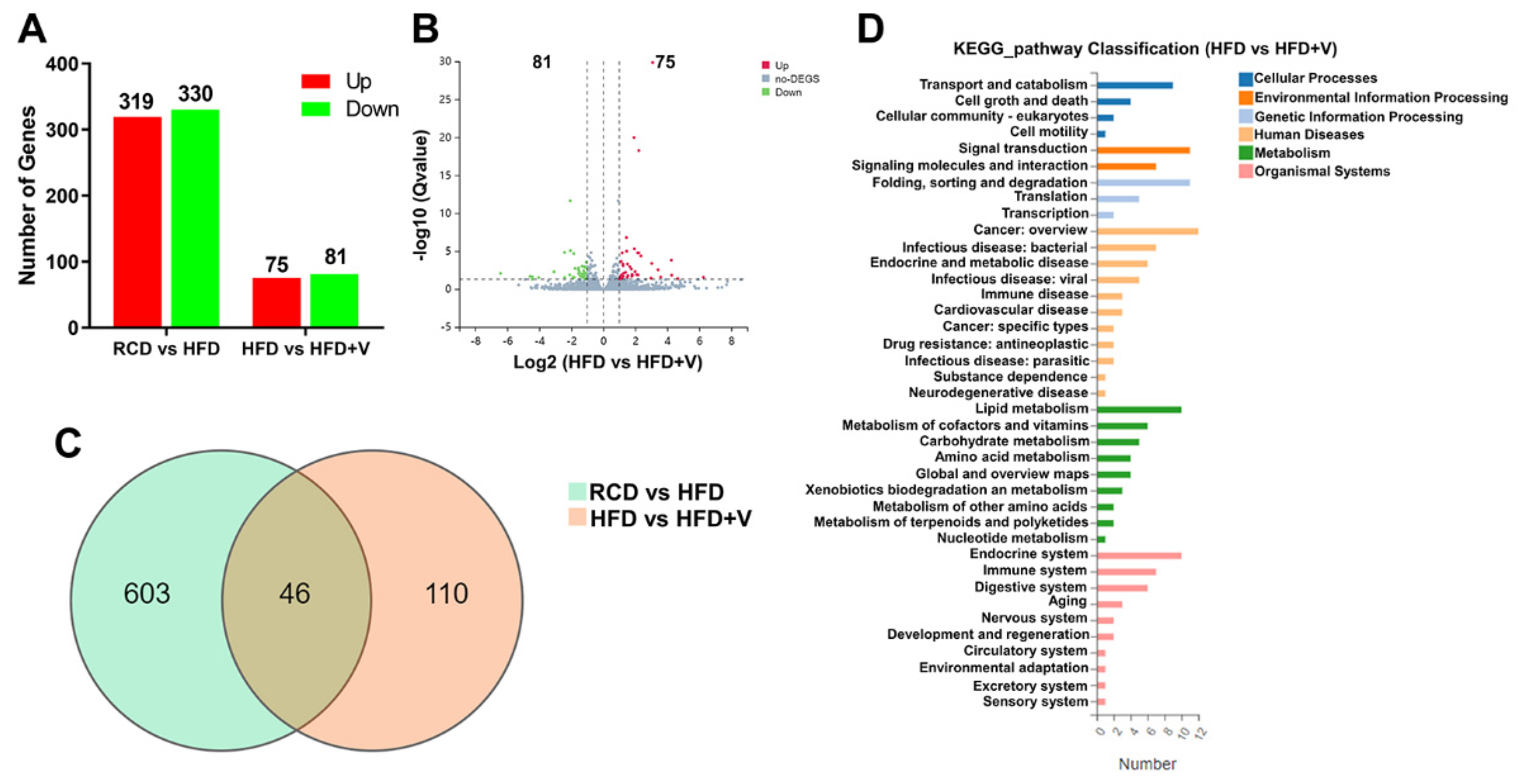
3.4. VOdipic-Cl Affects Gene Expression Profile in the Livers of Obese Mice
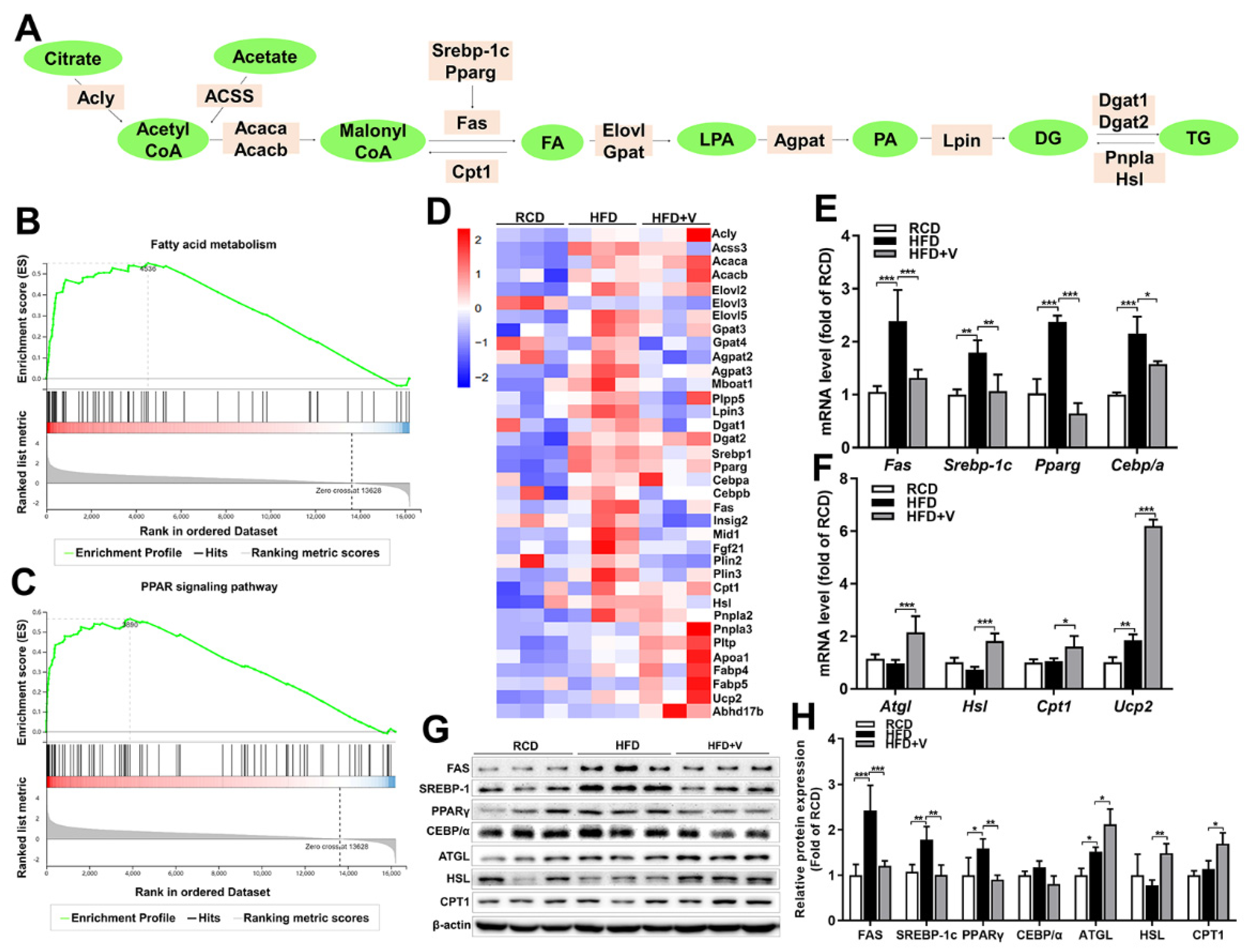
3.5. Effect of VOdipic-Cl on the Expression of Hepatic Triglyceride Synthesis and Lipolysis Genes in Obese Mice
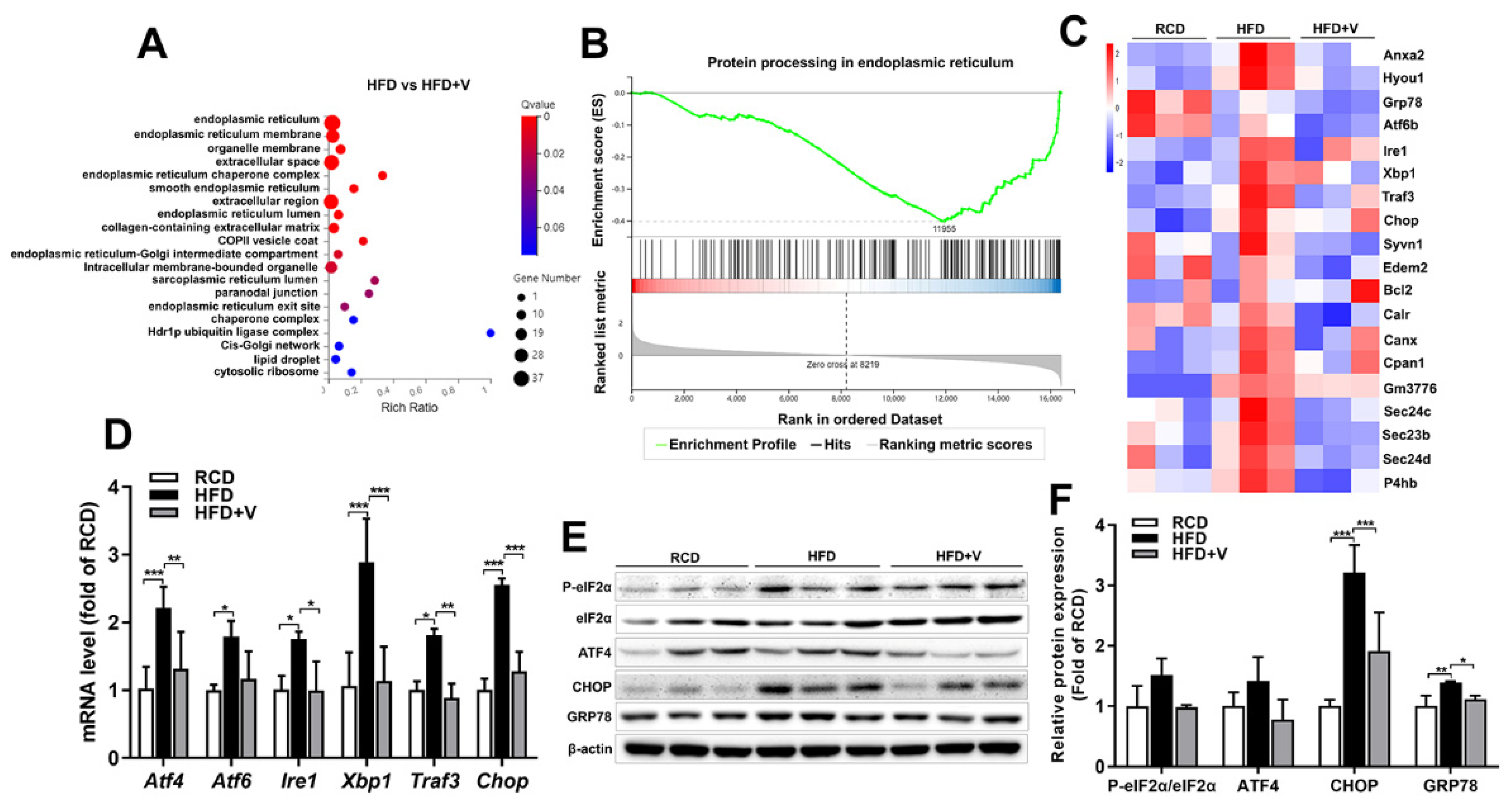
3.6. Effect of VOdipic-Cl on the Gene Expression Profile of Hepatic ER Stress in Obese Mice
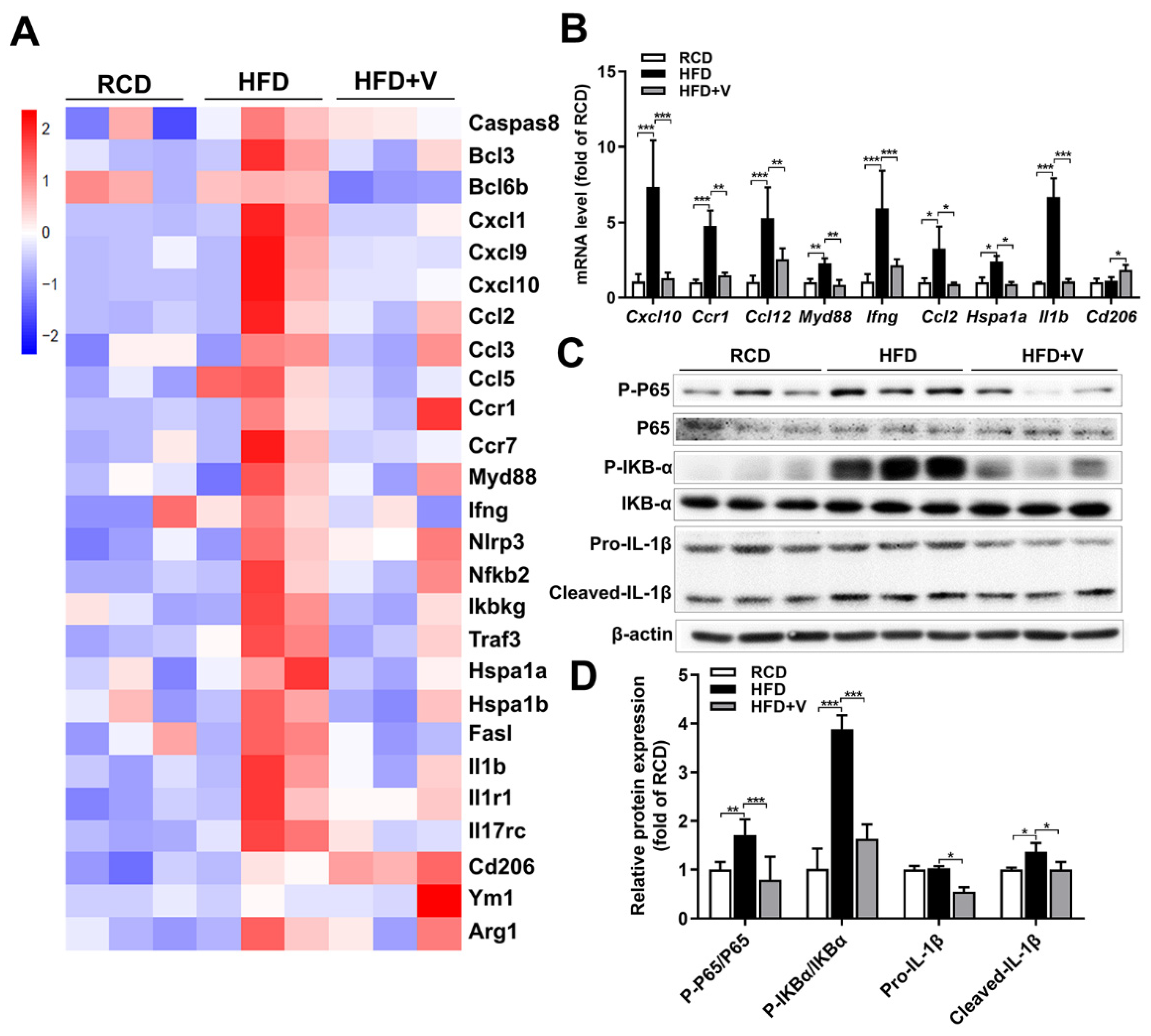
3.7. Effect of VOdipic-Cl on the Gene Expression Profile of Hepatic Inflammation in Obese Mice
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; George, J.; Bugianesi, E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Zhang, X.J.; Li, H. Progress and challenges in the prevention and control of nonalcoholic fatty liver disease. Med. Res. Rev. 2019, 39, 328–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Younes, R.; Bugianesi, E. Should we undertake surveillance for HCC in patients with NAFLD? J. Hepatol. 2018, 68, 326–334. [Google Scholar] [CrossRef]
- Negi, C.K.; Babica, P.; Bajard, L.; Bienertova-Vasku, J.; Tarantino, G. Insights into the molecular targets and emerging pharmacotherapeutic interventions for nonalcoholic fatty liver disease. Metabolism 2022, 126, 154925. [Google Scholar] [CrossRef]
- Ozcan, U.; Cao, Q.; Yilmaz, E.; Lee, A.H.; Iwakoshi, N.N.; Ozdelen, E.; Tuncman, G.; Gorgun, C.; Glimcher, L.H.; Hotamisligil, G.S. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science 2004, 306, 457–461. [Google Scholar] [CrossRef] [Green Version]
- Lomonaco, R.; Sunny, N.E.; Bril, F.; Cusi, K. Nonalcoholic fatty liver disease: Current issues and novel treatment approaches. Drugs 2013, 73, 1–14. [Google Scholar] [CrossRef]
- Shan, B.; Wang, X.; Wu, Y.; Xu, C.; Xia, Z.; Dai, J.; Shao, M.; Zhao, F.; He, S.; Yang, L.; et al. The metabolic ER stress sensor IRE1alpha suppresses alternative activation of macrophages and impairs energy expenditure in obesity. Nat. Immunol. 2017, 18, 519–529. [Google Scholar] [CrossRef]
- Lebeaupin, C.; Vallee, D.; Hazari, Y.; Hetz, C.; Chevet, E.; Bailly-Maitre, B. Endoplasmic reticulum stress signalling and the pathogenesis of non-alcoholic fatty liver disease. J. Hepatol. 2018, 69, 927–947. [Google Scholar] [CrossRef]
- Puri, P.; Mirshahi, F.; Cheung, O.; Natarajan, R.; Maher, J.W.; Kellum, J.M.; Sanyal, A.J. Activation and dysregulation of the unfolded protein response in nonalcoholic fatty liver disease. Gastroenterology 2008, 134, 568–576. [Google Scholar] [CrossRef]
- Rolo, A.P.; Teodoro, J.S.; Palmeira, C.M. Role of oxidative stress in the pathogenesis of nonalcoholic steatohepatitis. Free Radic. Biol. Med. 2012, 52, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Serviddio, G.; Bellanti, F.; Vendemiale, G. Free radical biology for medicine: Learning from nonalcoholic fatty liver disease. Free Radic. Biol. Med. 2013, 65, 952–968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diehl, A.M.; Day, C. Cause, pathogenesis, and treatment of Nonalcoholic Steatohepatitis. N. Engl. J. Med. 2017, 377, 2063–2072. [Google Scholar] [CrossRef]
- Baiceanu, A.; Mesdom, P.; Lagouge, M.; Foufelle, F. Endoplasmic reticulum proteostasis in hepatic steatosis. Nat. Rev. Endocrinol. 2016, 12, 710–722. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Chen, D.; Zhang, F.; Willsky, G.R.; Crans, D.C.; Ding, W. Effects of vanadium (III, IV, V)-chlorodipicolinate on glycolysis and antioxidant status in the liver of STZ-induced diabetic rats. J. Inorg. Biochem. 2014, 136, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Huang, Y.; Liu, F.; Zhang, F.; Ding, W. Vanadium(IV)-chlorodipicolinate inhibits 3T3-L1 preadipocyte adipogenesis by activating LKB1/AMPK signaling pathway. J. Inorg. Biochem. 2016, 162, 1–8. [Google Scholar] [CrossRef]
- Huang, Y.; Liu, F.; Zhang, F.; Liu, P.; Xu, T.; Ding, W. Vanadium(IV)-chlorodipicolinate alleviates hepatic lipid accumulation by inducing autophagy via the LKB1/AMPK signaling pathway in vitro and in vivo. J. Inorg. Biochem. 2018, 183, 66–76. [Google Scholar] [CrossRef]
- Hosoi, T.; Saito, A.; Kume, A.; Okuma, Y.; Nomura, Y.; Ozawa, K. Vanadate inhibits endoplasmic reticulum stress responses. Eur. J. Pharmacol. 2008, 594, 44–48. [Google Scholar] [CrossRef] [Green Version]
- He, Z.; Wang, M.; Zhao, Q.; Li, X.; Liu, P.; Ren, B.; Wu, C.; Du, X.; Li, N.; Liu, Q. Bis(ethylmaltolato)oxidovanadium (IV) mitigates neuronal apoptosis resulted from amyloid-beta induced endoplasmic reticulum stress through activating peroxisome proliferator-activated receptor gamma. J. Inorg. Biochem. 2020, 208, 111073. [Google Scholar] [CrossRef]
- Cong, X.Q.; Piao, M.H.; Li, Y.; Xie, L.; Liu, Y. Bis(maltolato)oxovanadium(IV) (BMOV) attenuates apoptosis in high glucose-treated cardiac cells and diabetic rat hearts by regulating the unfolded protein responses (UPRs). Biol. Trace Elem. Res. 2016, 173, 390–398. [Google Scholar] [CrossRef]
- Bin-Jaliah, I.; Sakr, H.F.; Morsy, M.D.; Dallak, M.; Haidara, M.A. Modulatory effect of concomitant administration of insulin and vanadium on inflammatory biomarkers in type 2 diabetic rats: Role of adiponectin. Chin. J. Physiol. 2018, 61, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Finelli, C.; Tarantino, G. What is the role of adiponectin in obesity related non-alcoholic fatty liver disease? World J. Gastroenterol. 2013, 19, 802–812. [Google Scholar] [CrossRef] [PubMed]
- Zhong, F.; Zhou, X.; Xu, J.; Gao, L. Rodent Models of Nonalcoholic Fatty Liver Disease. Digestion 2020, 101, 522–535. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Langmead, B.; Salzberg, S.L. HISAT: A fast spliced aligner with low memory requirements. Nat. Methods 2015, 12, 357–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langmead, B.; Salzberg, S.L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Feng, Z.; Wang, X.; Wang, X.; Zhang, X. DEGseq: An R package for identifying differentially expressed genes from RNA-seq data. Bioinformatics 2010, 26, 136–138. [Google Scholar] [CrossRef]
- Yang, W.; Wang, S.; Loor, J.J.; Lopes, M.G.; Zhao, Y.; Ma, X.; Li, M.; Zhang, B.; Xu, C. Role of diacylglycerol O-acyltransferase (DGAT) isoforms in bovine hepatic fatty acid metabolism. J. Dairy Sci. 2022, 105, 3588–3600. [Google Scholar] [CrossRef]
- Alves-Bezerra, M.; Cohen, D.E. Triglyceride Metabolism in the Liver. Compr. Physiol. 2017, 8, 1–8. [Google Scholar]
- Takeuchi, K.; Reue, K. Biochemistry, physiology, and genetics of GPAT, AGPAT, and lipin enzymes in triglyceride synthesis. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E1195–E1209. [Google Scholar] [CrossRef] [Green Version]
- Domingo, J.L.; Gomez, M. Vanadium compounds for the treatment of human diabetes mellitus: A scientific curiosity? A review of thirty years of research. Food Chem. Toxicol. 2016, 95, 137–141. [Google Scholar] [CrossRef]
- Scior, T.; Guevara-Garcia, J.A.; Do, Q.T.; Bernard, P.; Laufer, S. Why antidiabetic vanadium complexes are not in the pipeline of "big pharma" drug research? A Critical Review. Curr. Med. Chem. 2016, 23, 2874–2891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smee, J.J.; Epps, J.A.; Ooms, K.; Bolte, S.E.; Polenova, T.; Baruah, B.; Yang, L.; Ding, W.; Li, M.; Willsky, G.R.; et al. Chloro-substituted dipicolinate vanadium complexes: Synthesis, solution, solid-state, and insulin-enhancing properties. J. Inorg. Biochem. 2009, 103, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Zierath, J.R.; Livingston, J.N.; Thorne, A.; Bolinder, J.; Reynisdottir, S.; Lonnqvist, F.; Arner, P. Regional difference in insulin inhibition of non-esterified fatty acid release from human adipocytes: Relation to insulin receptor phosphorylation and intracellular signalling through the insulin receptor substrate-1 pathway. Diabetologia 1998, 41, 1343–1354. [Google Scholar] [CrossRef] [PubMed]
- Marchesini, G.; Brizi, M.; Bianchi, G.; Tomassetti, S.; Bugianesi, E.; Lenzi, M.; McCullough, A.J.; Natale, S.; Forlani, G.; Melchionda, N. Nonalcoholic fatty liver disease—A feature of the metabolic syndrome. Diabetes 2001, 50, 1844–1850. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Yu, Y.; Cai, J.; Li, H. Emerging Molecular Targets for Treatment of Nonalcoholic Fatty Liver Disease. Trends Endocrinol. Metab. 2019, 30, 903–914. [Google Scholar] [CrossRef] [PubMed]
- Yuen, V.G.; Orvig, C.; McNeill, J.H. Effects of bis(maltolato)oxovanadium(IV) are distinct from food restriction in STZ-diabetic rats. Am. J. Physiol. 1997, 272, E30–E35. [Google Scholar] [CrossRef]
- Li, M.; Ding, W.; Smee, J.J.; Baruah, B.; Willsky, G.R.; Crans, D.C. Anti-diabetic effects of vanadium(III, IV, V)-chlorodipicolinate complexes in streptozotocin-induced diabetic rats. Biometals 2009, 22, 895–905. [Google Scholar] [CrossRef]
- Chen, Z.; Tian, R.; She, Z.; Cai, J.; Li, H. Role of oxidative stress in the pathogenesis of nonalcoholic fatty liver disease. Free Radic. Biol. Med. 2020, 152, 116–141. [Google Scholar] [CrossRef]
- Mortazavi, A.; Williams, B.A.; McCue, K.; Schaeffer, L.; Wold, B. Mapping and quantifying mammalian transcriptomes by RNA-Seq. Nat. Methods 2008, 5, 621–628. [Google Scholar] [CrossRef]
- Willsky, G.R.; Chi, L.H.; Liang, Y.; Gaile, D.P.; Hu, Z.; Crans, D.C. Diabetes-altered gene expression in rat skeletal muscle corrected by oral administration of vanadyl sulfate. Physiol. Genom. 2006, 26, 192–201. [Google Scholar] [CrossRef]
- Donnelly, K.L.; Smith, C.I.; Schwarzenberg, S.J.; Jessurun, J.; Boldt, M.D.; Parks, E.J. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J. Clin. Investig. 2005, 115, 1343–1351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, Y.A. The SCAP/SREBP pathway: A mediator of hepatic steatosis. Endocrinol. Metab. 2017, 32, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Moran-Salvador, E.; Lopez-Parra, M.; Garcia-Alonso, V.; Titos, E.; Martinez-Clemente, M.; Gonzalez-Periz, A.; Lopez-Vicario, C.; Barak, Y.; Arroyo, V.; Claria, J. Role for PPARgamma in obesity-induced hepatic steatosis as determined by hepatocyte- and macrophage-specific conditional knockouts. FASEB J. 2011, 25, 2538–2550. [Google Scholar] [CrossRef] [PubMed]
- Madsen, M.S.; Siersbaek, R.; Boergesen, M.; Nielsen, R.; Mandrup, S. Peroxisome proliferator-activated receptor gamma and C/EBPalpha synergistically activate key metabolic adipocyte genes by assisted loading. Mol. Cell Biol. 2014, 34, 939–954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gruzewska, K.; Michno, A.; Pawelczyk, T.; Bielarczyk, H. Essentiality and toxicity of vanadium supplements in health and pathology. J. Physiol. Pharmacol. 2014, 65, 603–611. [Google Scholar] [PubMed]
- Sarmiento-Ortega, V.E.; Moroni-Gonzalez, D.; Diaz, A.; Moran, C.; Brambila, E.; Trevino, S. Sodium metavanadate treatment improves glycogen levels in multiple tissues in a model of metabolic syndrome caused by chronic cadmium exposure in Wistar rats. Biometals. 2021, 34, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Arab, J.P.; Arrese, M.; Trauner, M. Recent insights into the pathogenesis of nonalcoholic fatty liver disease. Annu. Rev. Pathol. 2018, 13, 321–350. [Google Scholar] [CrossRef] [PubMed]
- Samuel, V.T.; Shulman, G.I. Nonalcoholic fatty liver disease as a nexus of metabolic and hepatic diseases. Cell Metab. 2018, 27, 22–41. [Google Scholar] [CrossRef] [Green Version]
- Friedman, S.L.; Neuschwander-Tetri, B.A.; Rinella, M.; Sanyal, A.J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 2018, 24, 908–922. [Google Scholar] [CrossRef]
- Subramanian, V.; Rothenberg, A.; Gomez, C.; Cohen, A.W.; Garcia, A.; Bhattacharyya, S.; Shapiro, L.; Dolios, G.; Wang, R.; Lisanti, M.P.; et al. Perilipin A mediates the reversible binding of CGI-58 to lipid droplets in 3T3-L1 adipocytes. J. Biol. Chem. 2004, 279, 42062–42071. [Google Scholar] [CrossRef] [Green Version]
- Yamaguchi, T.; Omatsu, N.; Matsushita, S.; Osumi, T. CGI-58 interacts with perilipin and is localized to lipid droplets - Possible involvement of CGI-58 mislocalization in Chanarin-Dorfman syndrome. J. Biol. Chem. 2004, 279, 30490–30497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Listenberger, L.L.; Ostermeyer-Fay, A.G.; Goldberg, E.B.; Brown, W.J.; Brown, D.A. Adipocyte differentiation-related protein reduces the lipid droplet association of adipose triglyceride lipase and slows triacylglycerol turnover. J. Lipid Res. 2007, 48, 2751–2761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, K.T.; Mashek, M.T.; Bu, S.Y.; Greenberg, A.S.; Mashek, D.G. Adipose triglyceride lipase is a major hepatic lipase that regulates triacylglycerol turnover and fatty acid signaling and partitioning. Hepatology 2011, 53, 116–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harada, K.; Shen, W.J.; Patel, S.; Natu, V.; Wang, J.; Osuga, J.; Ishibashi, S.; Kraemer, F.B. Resistance to high-fat diet-induced obesity and altered expression of adipose-specific genes in HSL-deficient mice. Am. J. Physiol. Endocrinol. Metab. 2003, 285, E1182–E1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephens, F.B.; Constantin-Teodosiu, D.; Greenhaff, P.L. New insights concerning the role of carnitine in the regulation of fuel metabolism in skeletal muscle. J. Physiol. 2007, 581, 431–444. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Hickner, R.C.; Cortright, R.L.; Dohm, G.L.; Houmard, J.A. Lipid oxidation is reduced in obese human skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 2000, 279, E1039–E1044. [Google Scholar] [CrossRef] [Green Version]
- Kuo, T.F.; Tatsukawa, H.; Matsuura, T.; Nagatsuma, K.; Hirose, S.; Kojima, S. Free fatty acids induce transglutaminase 2-dependent apoptosis in hepatocytes via ER stress-stimulated PERK pathways. J. Cell. Physiol. 2012, 227, 1130–1137. [Google Scholar] [CrossRef]
- Malhi, H.; Kaufman, R.J. Endoplasmic reticulum stress in liver disease. J. Hepatol. 2011, 54, 795–809. [Google Scholar] [CrossRef] [Green Version]
- Song, M.J.; Malhi, H. The unfolded protein response and hepatic lipid metabolism in non alcoholic fatty liver disease. Pharmacol. Ther. 2019, 203, 107401. [Google Scholar] [CrossRef]
- Zhang, Q.; Li, Y.; Liang, T.; Lu, X.; Zhang, C.; Liu, X.; Jiang, X.; Martin, R.C.; Cheng, M.; Cai, L. ER stress and autophagy dysfunction contribute to fatty liver in diabetic mice. Int. J. Biol. Sci. 2015, 11, 559–568. [Google Scholar] [CrossRef] [Green Version]
- He, Z.; Song, J.; Li, X.; Li, X.; Zhu, H.; Wu, C.; Xiao, W.; Du, X.; Ni, J.; Li, N.; et al. Bis(ethylmaltolato)oxidovanadium (IV) alleviates neuronal apoptosis through regulating peroxisome proliferator-activated receptor gamma in a triple transgenic animal model of Alzheimer’s disease. J. Biol. Inorg. Chem. 2021, 26, 551–568. [Google Scholar] [CrossRef] [PubMed]
- Hirsova, P.; Ibrabim, S.H.; Gores, G.J.; Malhi, H. Lipotoxic lethal and sublethal stress signaling in hepatocytes: Relevance to NASH pathogenesis. J. Lipid Res. 2016, 57, 1758–1770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volmer, R.; van der Ploeg, K.; Ron, D. Membrane lipid saturation activates endoplasmic reticulum unfolded protein response transducers through their transmembrane domains. Proc. Natl. Acad. Sci. USA 2013, 110, 4628–4633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kakazu, E.; Mauer, A.S.; Yin, M.; Malhi, H. Hepatocytes release ceramide-enriched pro-inflammatory extracellular vesicles in an IRE1alpha-dependent manner. J. Lipid Res. 2016, 57, 233–245. [Google Scholar] [CrossRef] [Green Version]
- Amen, O.M.; Sarker, S.D.; Ghildyal, R.; Arya, A. Endoplasmic reticulum stress activates unfolded protein response signaling and mediates inflammation, obesity, and cardiac dysfunction: Therapeutic and molecular approach. Front. Pharmacol. 2019, 10, 977. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Liu, Q.; Pang, Y.; Xu, X.; Cui, K.; Zhang, Y.; Mai, K.; Ai, Q. Molecular cloning and the involvement of IRE1alpha-XBP1s signaling pathway in palmitic acid induced - Inflammation in primary hepatocytes from large yellow croaker (Larimichthys crocea). Fish Shellfish Immunol. 2020, 98, 112–121. [Google Scholar] [CrossRef]
- Luo, Y.; Dong, X.; Yu, Y.; Sun, G.; Sun, X. Total aralosides of aralia elata (Miq) seem (TASAES) ameliorate nonalcoholic steatohepatitis by modulating IRE1alpha-mediated JNK and NF-kappaB pathways in ApoE-/- mice. J. Ethnopharmacol. 2015, 163, 241–250. [Google Scholar] [CrossRef]
- Chipurupalli, S.; Samavedam, U.; Robinson, N. Crosstalk between ER stress, autophagy and inflammation. Front. Med. 2021, 8, 758311. [Google Scholar] [CrossRef]

| Gene ID | Gene Name | log2(HFD/RCD) | Q-value |
|---|---|---|---|
| Top 10 up-regulated genes | |||
| 12683 | Cidea | 9.023595 | 8.99 × 10−12 |
| 228677 | Sptlc3 | 7.503749 | 3.56 × 10−5 |
| 13094 | Cyp2b9 | 6.854523 | 3.98 × 10−8 |
| 13086 | Cyp2a4 | 6.713696 | 6.43 × 10−6 |
| 268958 | Capn11 | 5.638241 | 0.013663 |
| 93695 | Gpnmb | 5.318517 | 3.74 × 10−4 |
| 20753 | Sprr1a | 5.211094 | 0.019481 |
| 239463 | Fam83a | 5.151803 | 1.80 × 10−9 |
| 11537 | Cfd | 5.049939 | 0.002032 |
| 68393 | Mogat1 | 5.009104 | 3.35 × 10−20 |
| Top 10 down-regulated genes | |||
| 59012 | Moxd1 | −9.08269 | 3.80 × 10−13 |
| 13099 | Cyp2c40 | −6.86642 | 1.10 × 10−32 |
| 100043108 | Cyp2c69 | −6.54387 | 3.12 × 10−14 |
| 14282 | Fosb | −4.1573 | 6.04 × 10−5 |
| 20500 | Slc13a2 | −4.13595 | 8.11 × 10−8 |
| 20704 | Serpina1e | −3.59604 | 2.78 × 10−80 |
| 100559 | Ugt2b38 | −3.54827 | 5.53 × 10−47 |
| 77596 | Adgrf1 | −3.46736 | 1.10 × 10−32 |
| 13082 | Cyp26a1 | −3.3903 | 3.96 × 10−12 |
| 233799 | Acsm2 | −3.22653 | 0.005442 |
| Gene ID | Gene Name | log2(HFD+V/HFD) | Q-value |
|---|---|---|---|
| Top 10 up-regulated genes | |||
| 13035 | Ctsg | 6.260156209 | 0.027929352 |
| 27028 | Ermap | 4.653195976 | 0.042060535 |
| 50701 | Elane | 4.272854575 | 0.014677 |
| 59012 | Moxd1 | 4.251877958 | 1.53 × 10−4 |
| 55985 | Cxcl13 | 3.583918049 | 0.025926151 |
| 18022 | Nfe2 | 3.420277595 | 0.002922876 |
| 12700 | Cish | 3.085936054 | 1.43 × 10−30 |
| 13099 | Cyp2c40 | 3.029913721 | 4.20 × 10−4 |
| 57349 | Ppbp | 2.980473843 | 0.036379545 |
| 105246824 | Gm42048 | 2.352530182 | 4.30 × 10−5 |
| Top 10 down-regulated genes | |||
| 20753 | Sprr1a | −6.41864 | 0.008521 |
| 14857 | Gsta1 | −4.58046 | 0.021441 |
| 12164 | Bmp8b | −4.4467 | 0.04983 |
| 13844 | Ephb2 | −4.43179 | 0.023676 |
| 100042295 | Gm3776 | −4.03746 | 0.030474 |
| 13086 | Cyp2a4 | −3.07994 | 0.005285 |
| 53321 | Cntnap1 | −2.42271 | 1.48 × 10−5 |
| 239463 | Fam83a | −2.41749 | 0.028261 |
| 76293 | Mfap4 | −2.09718 | 0.013435 |
| 12053 | Bcl6 | −2.07082 | 2.32 × 10−12 |
| Pathway ID | Pathway Name | Gene Number | Rich Ratio * | Q value |
|---|---|---|---|---|
| ko3010 | Ribosome | 42 | 0.304347826 | 1.62 × 10−22 |
| ko4610 | Complement and coagulation cascades | 24 | 0.258064516 | 8.68 × 10−11 |
| ko830 | Retinol metabolism | 23 | 0.252747253 | 2.87 × 10−10 |
| ko140 | Steroid hormone biosynthesis | 20 | 0.227272727 | 3.70 × 10−8 |
| ko3320 | PPAR signaling pathway | 20 | 0.229885057 | 3.70 × 10−8 |
| ko5204 | Chemical carcinogenesis | 20 | 0.210526316 | 1.30 × 10−7 |
| ko1212 | Fatty acid metabolism | 15 | 0.245901639 | 1.24 × 10−6 |
| ko71 | Fatty acid degradation | 10 | 0.2 | 0.001626099 |
| ko983 | Drug metabolism—other enzymes | 13 | 0.147727273 | 0.003072717 |
| ko980 | Metabolism of xenobiotics by cytochrome P450 | 11 | 0.164179104 | 0.003637073 |
| ko20 | Citrate cycle (TCA cycle) | 6 | 0.1875 | 0.03105017 |
| ko4141 | Protein processing in endoplasmic reticulum | 15 | 0.091463415 | 0.06166278 |
| Pathway ID | Pathway Name | Gene Number | Rich Ratio * | Q value |
|---|---|---|---|---|
| ko100 | Steroid biosynthesis | 5 | 0.25 | 1.06 × 10−4 |
| ko4141 | Protein processing in endoplasmic reticulum | 10 | 0.06097561 | 1.40 × 10−4 |
| ko830 | Retinol metabolism | 5 | 0.054945055 | 0.050931566 |
| ko4950 | Maturity onset diabetes of the young | 3 | 0.111111111 | 0.050931566 |
| ko5204 | Chemical carcinogenesis | 5 | 0.052631579 | 0.050931566 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Chen, R.; Li, J.; Zeng, G.; Yuan, J.; Su, J.; Wu, C.; Lu, Z.; Zhang, F.; Ding, W. Vanadium(IV)-Chlorodipicolinate Protects against Hepatic Steatosis by Ameliorating Lipid Peroxidation, Endoplasmic Reticulum Stress, and Inflammation. Antioxidants 2022, 11, 1093. https://doi.org/10.3390/antiox11061093
Wang Y, Chen R, Li J, Zeng G, Yuan J, Su J, Wu C, Lu Z, Zhang F, Ding W. Vanadium(IV)-Chlorodipicolinate Protects against Hepatic Steatosis by Ameliorating Lipid Peroxidation, Endoplasmic Reticulum Stress, and Inflammation. Antioxidants. 2022; 11(6):1093. https://doi.org/10.3390/antiox11061093
Chicago/Turabian StyleWang, Yuanli, Rulong Chen, Jingyi Li, Guodong Zeng, Juntao Yuan, Jingran Su, Chunyan Wu, Zhongbing Lu, Fang Zhang, and Wenjun Ding. 2022. "Vanadium(IV)-Chlorodipicolinate Protects against Hepatic Steatosis by Ameliorating Lipid Peroxidation, Endoplasmic Reticulum Stress, and Inflammation" Antioxidants 11, no. 6: 1093. https://doi.org/10.3390/antiox11061093
APA StyleWang, Y., Chen, R., Li, J., Zeng, G., Yuan, J., Su, J., Wu, C., Lu, Z., Zhang, F., & Ding, W. (2022). Vanadium(IV)-Chlorodipicolinate Protects against Hepatic Steatosis by Ameliorating Lipid Peroxidation, Endoplasmic Reticulum Stress, and Inflammation. Antioxidants, 11(6), 1093. https://doi.org/10.3390/antiox11061093







