Jaboticaba (Myrciaria jaboticaba) Attenuates Ventricular Remodeling after Myocardial Infarction in Rats
Abstract
1. Introduction
2. Material and Methods
2.1. Experimental Groups
2.2. Feed
2.3. Physical-Chemical Characterization of Jaboticaba Samples
2.4. Echocardiographic Analysis
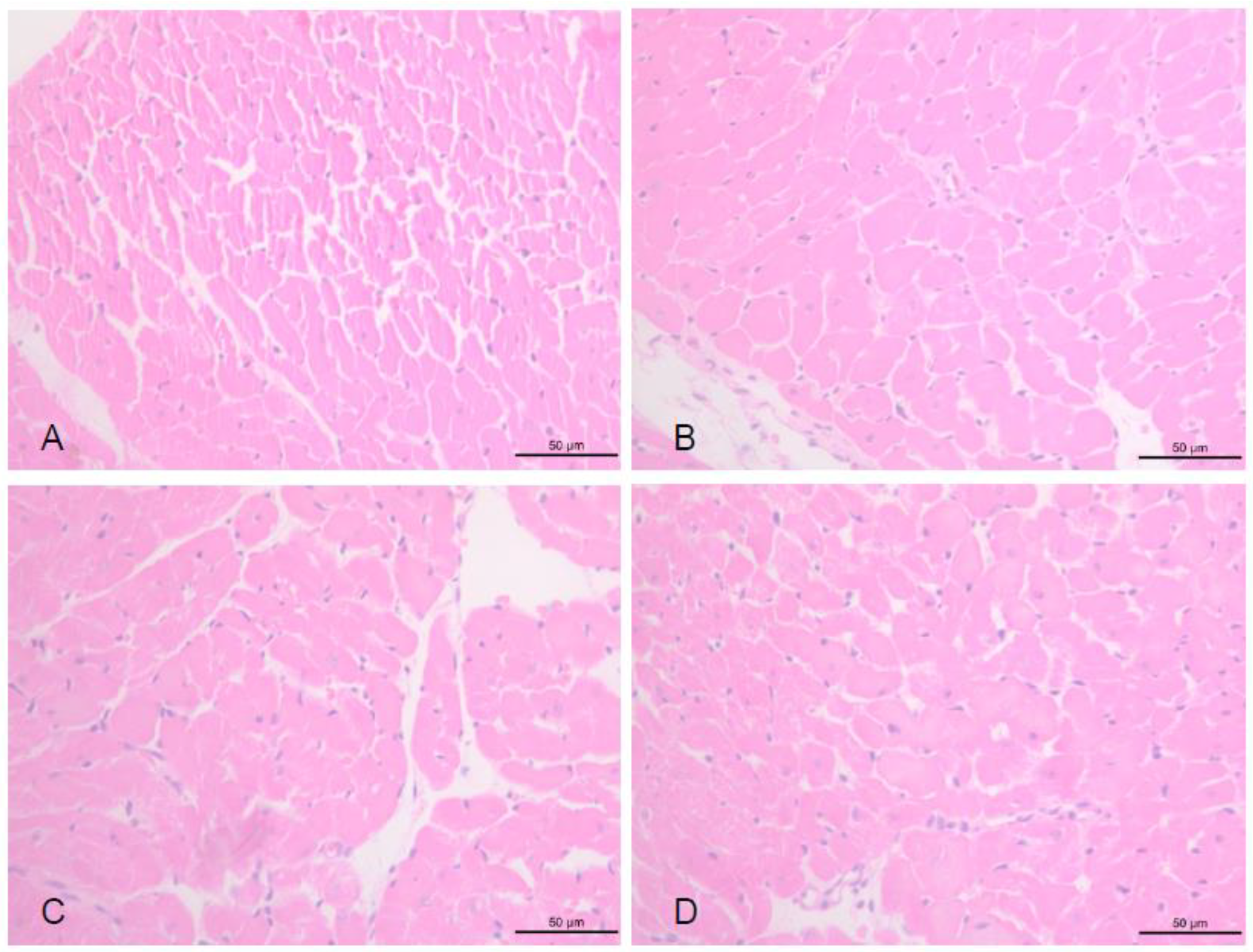
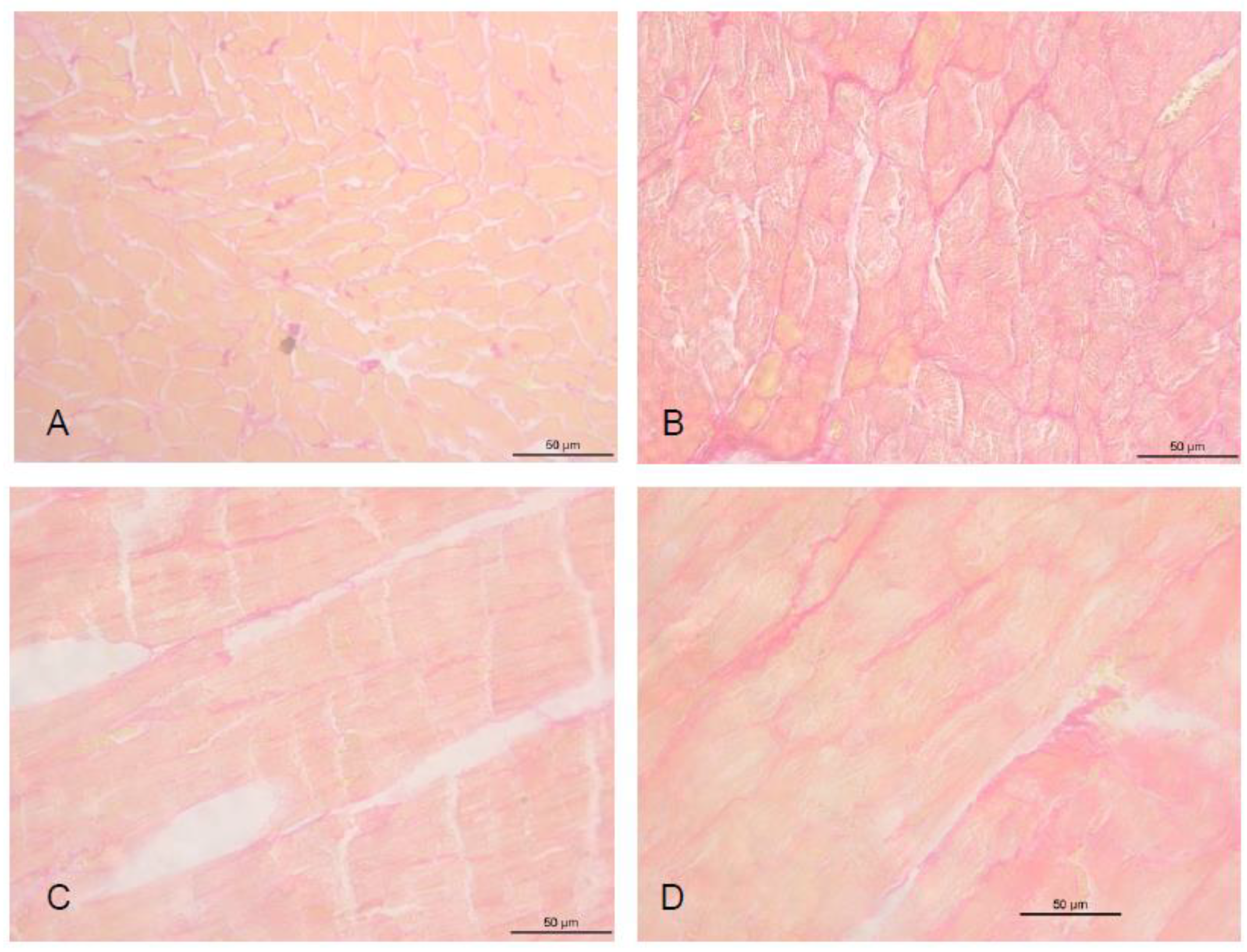
2.5. Morphometric Analysis
2.6. Cardiac Energy Metabolism and Oxidative Stress Analysis
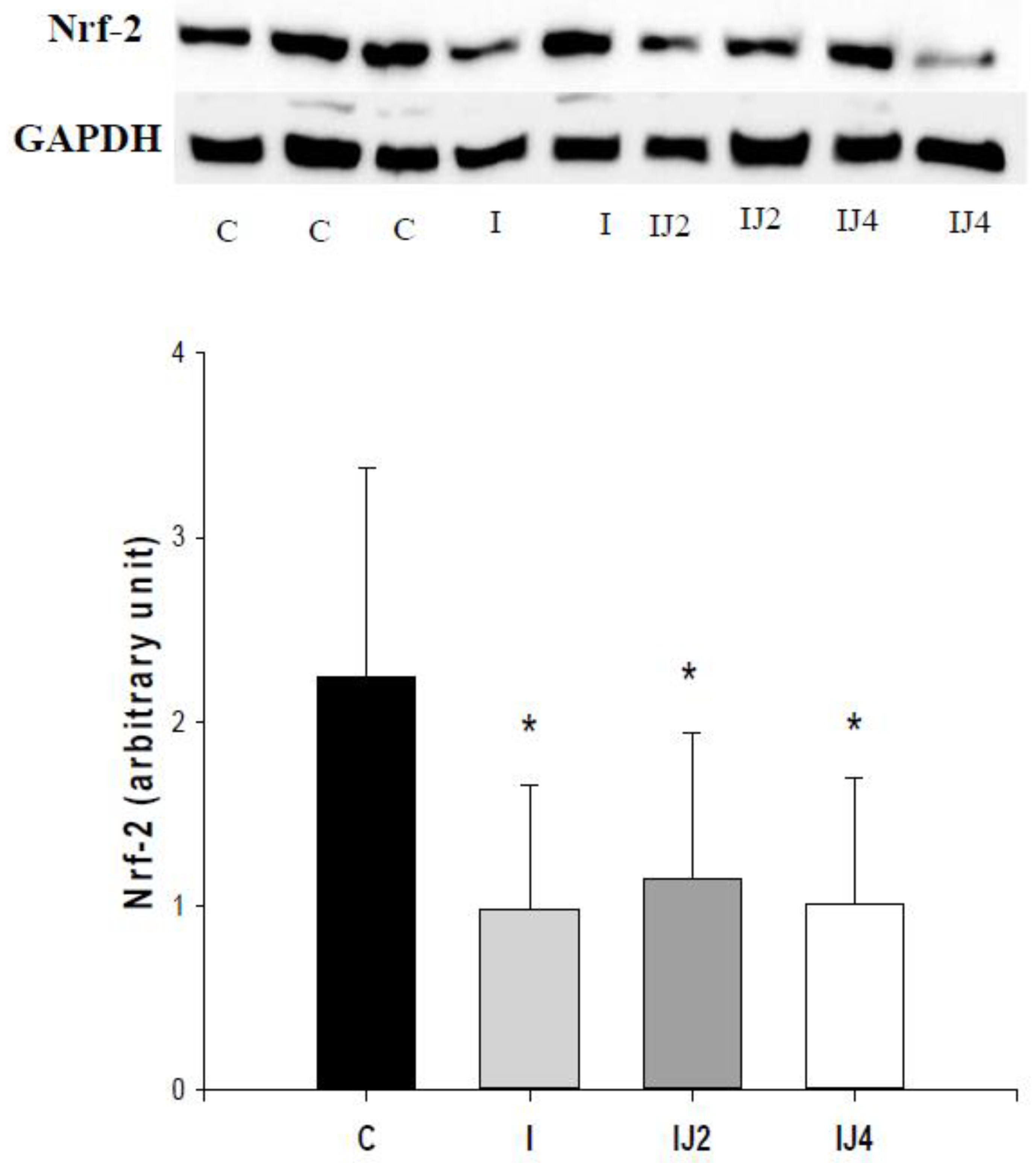
2.7. Western Blot Analysis
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pfeffer, M.A.; Braunwald, E. Ventricular remodeling after myocardial infarction: Experimental observations and clinical implications. Circulation 1990, 81, 1161–1172. [Google Scholar] [CrossRef] [PubMed]
- Cohn, J.N.; Ferrari, R.; Sharpe, N. Cardiac remodeling-concepts and clinical implications: A consensus paper from an international forum on cardiac remodeling. J. Am. Coll. Cardiol. 2000, 35, 569–582. [Google Scholar] [CrossRef]
- Azevedo, P.S.; Polegato, B.F.; Minicucci, M.F.; Paiva, S.A.; Zornoff, L.A. Cardiac remodeling: Concepts, clinical impact, pathophysiological mechanisms and pharmacologic treatment. Arq. Bras. Cardiol. 2016, 106, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Farah, E.; Cogni, A.L.; Minicucci, M.F.; Azevedo, P.S.; Okoshi, K.; Matsubara, B.B.; Zanati, S.G.; Haggeman, R.; Paiva, S.A.; Zornoff, L.A. Prevalence and predictors of ventricular remodeling after anterior myocardial infarction in the era of modern medical therapy. Med. Sci. Monit. 2012, 18, CR276–CR281. [Google Scholar] [CrossRef] [PubMed]
- Martinez, P.F.; Bonomo, C.; Guizoni, D.M.; Junior, S.A.O.; Damatto, R.L.; Cezar, M.D.M.; Lima, A.R.R.; Pagan, L.U.; Seiva, F.R.; Fernandes, D.C.; et al. Influence of N-acetylcysteine on oxidative stress in slow-twitch soleus muscle of heart failure rats. Cell. Physiol. Biochem. 2015, 35, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Lustosa, B.B.; Polegato, B.; Minicucci, M.F.; Rafacho, B.; Santos, P.P.; Fernandes, A.A.; Okoshi, K.; Batista, D.; Modesto, P.; Gonçalves, A.F.; et al. Green tea (Cammellia sinensis) attenuates ventricular remodeling after experimental myocardial infarction. Int. J. Cardiol. 2016, 225, 147–153. [Google Scholar] [CrossRef]
- Rafacho, B.; Santos, P.P.; Gonçalves, A.F.; Fernandes, A.A.; Okoshi, K.; Chiuso-Minicucci, F.; Azevedo, P.S.; Zornoff, L.; Minicucci, M.F.; Wang, X.-D.; et al. Rosemary supplementation (Rosmarinus oficinallis L.) attenuates cardiac remodeling after myocardial infarction in rats. PLoS ONE 2017, 12, e0177521. [Google Scholar]
- Pereira, B.L.B.; Reis, P.P.; Severino, F.E.; Felix, T.F.; Braz, M.G.; Nogueira, F.R.; Silva, R.A.C.; Cardoso, A.C.; Lourenço, M.A.M.; Figueiredo, A.M.; et al. Tomato (Lycopersicon esculentum) or lycopene supplementation attenuates ventricular remodeling after myocardial infarction through different mechanistic pathways. J. Nutr. Biochem. 2017, 46, 117–124. [Google Scholar] [CrossRef]
- Zhou, S.X.; Zhou, Y.; Zhang, Y.L.; Lei, J.; Wang, J.F. Antioxidant probucol attenuates myocardial oxidative stress and collagen expressions in post-myocardial infarction rats. J. Cardiovasc. Pharmacol. 2009, 54, 154–162. [Google Scholar] [CrossRef]
- Batista, A.G.; Soares, E.S.; Mendonça, M.C.P.; Silva, J.K.; Dionísio, A.P.; Sartori, C.R.; Cruz-Höfling, M.A.; Júnior, M.R.M. Jaboticaba berry peel intake prevents insulin-resistance-induced tau phosphorylation in mice. Mol. Nutr. Food Res. 2017, 61, 1600952. [Google Scholar] [CrossRef]
- Leite, A.V.; Malta, L.G.; Riccio, M.F.; Eberlin, M.N.; Pastore, G.M.; Junior, M.R.M. Antioxidant potential of rat plasma by administration of freeze-dried jaboticaba peel (Myrciaria jaboticaba Vell Berg). J. Agric. Food Chem. 2011, 59, 2277–2283. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, J.M.; Finn, P.V.; Zornoff, L.A.; Pfeffer, M.A. Endothelin—A receptor antagonism during acute myocardial infarction in rats. Cardiovasc. Drugs Ther. 2000, 14, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Paiva, S.A.; Novo, R.; Matsubara, B.B.; Matsubara, L.S.; Azevedo, P.S.; Minicucci, M.F.; Campana, A.O.; Zornoff, L. β-carotene attenuates the paradoxical effect of tobacco smoke on the mortality of rats after experimental myocardial infarction. J. Nutr. 2005, 135, 2109–3113. [Google Scholar] [CrossRef] [PubMed]
- Minicucci, M.F.; Azevedo, P.S.; Martinez, P.F.; Lima, A.R.R.; Bonomo, C.; Guizoni, D.M.; Polegato, B.F.; Okoshi, M.P.; Okoshi, K.; Matsubara, B.B.; et al. Critical infarct size to induce ventricular remodeling, cardiac dysfunction and heart failure in rats. Int. J. Cardiol. 2011, 151, 242–243. [Google Scholar] [CrossRef][Green Version]
- Reagan-Shaw, S.; Nihal, M.; Ahmad, N. Dose translation from animal to human studies revisited. FASEB J. 2008, 22, 659–661. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, L.N.; Stringheta, P.C.; Oliveira, F.A. Comparation of methods for anthocyanin quantification. Ceres 2008, 55, 297–304. [Google Scholar]
- Singleton, V.L.; Rossi, J.A. A colorimetric of total phenolics with phosphomolybdic- phosphotungstic acid reagents. Am. J. Enol. Viticul. 1965, 6, 144–158. [Google Scholar]
- Azevedo, P.S.; Minicucci, M.F.; Chiuso-Minicucci, F.; Justulin, L.A., Jr.; Matsubara, L.S.; Matsubara, B.B.; Novelli, E.; Seiva, F.; Ebaid, G.; Campana, A.O.; et al. Ventricular remodeling induced by tissue vitamin A deficiency in rats. Cell. Physiol. Biochem. 2010, 26, 395–402. [Google Scholar] [CrossRef]
- Minicucci, M.F.; Azevedo, P.S.; Oliveira, S.A., Jr.; Martinez, P.F.; Chiuso-Minicucci, F.; Polegato, B.F.; Justulin, L.A., Jr.; Matsubara, L.S.; Matsubara, B.B.; Paiva, S.; et al. Tissue vitamin A insufficiency results in adverse ventricular remodeling after experimental myocardial infarction. Cell. Physiol. Biochem. 2010, 26, 523–530. [Google Scholar] [CrossRef]
- Zornoff, L.A.; Paiva, S.A.; Minicucci, M.F.; Spadaro, J. Experimental myocardium infarction in rats: Analysis of the model. Arq. Bras. Cardiol. 2009, 93, 434–440. [Google Scholar] [CrossRef]
- Batista, D.F.; Polegato, B.F.; Silva, R.C.; Claro, R.T.; Azevedo, P.S.; Fernandes, A.A.; Okoshi, K.; Paiva, S.A.; Minicucci, M.F.; Zornorff, L. Impact of modality and intensity of early exercise training on ventricular remodeling after myocardial infarction. Oxid. Med. Cell. Longev. 2020, 2020, 5041791. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.A.C.; Golçalves, A.F.; Santos, P.P.; Rafacho, B.; Claro, R.T.; Minicucci, M.F.; Azevedo, P.S.; Polegato, B.F.; Zanati, S.G.; Fernandes, A.A.; et al. Cardiac remodeling induced by all-trans retinoic acid is detrimental in normal rats. Cell. Physiol. Biochem. 2017, 43, 1449–1459. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.B.; Dastmalchi, K.; Long, C.; Kennelly, E.J. Metabolite profiling of jaboticaba (Myrciaria cauliflora) and other dark-colored fruit juices. J. Agric. Food Chem. 2012, 60, 7513–7525. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.B.; Long, C.; Kennelly, E.J. Phytochemistry and health benefits of jaboticaba, an emerging fruit crop from Brazil. Food Res. Int. 2013, 54, 148–159. [Google Scholar] [CrossRef]
- Nile, S.H.; Park, S.W. Edible berries: Bioactive components and their effect on human health. Nutrition 2014, 30, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Lobo de Andrade, D.M.; Reis, C.F.; Castro, F.S.; Borges, L.L.; Amaral, N.O.; Torres, I.M.S.; Rezende, S.G.; Gil, E.S.; Conceição, E.C.; Pedrino, G.R.; et al. Vasorelaxant and hypotensive effects of jaboticaba fruit (Myrciaria cauliflora) extract in rats. Evid. Based Complement. Altern. Med. 2015, 2015, 696135. [Google Scholar] [CrossRef]
- Andrade, D.M.L.; Borges, L.L.; Torres, I.M.S. Jabuticaba-induced endothelium-independent vasodilating effect on isolated arteries. Arq. Bras. Cardiol. 2016, 107, 223–229. [Google Scholar] [CrossRef]
- Stanley, W.C.; Recchia, F.A.; Lopaschuk, G.D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 2005, 85, 1093–1129. [Google Scholar] [CrossRef]
- Saks, V.; Favier, R.; Guzun, R.; Schlattner, U.; Wallimann, T. Molecular system bioenergetics: Regulation of substrate supply in response to heart energy demands. J. Physiol. 2006, 577, 769–777. [Google Scholar] [CrossRef]
- Wolfe, C.L.; Sievers, R.E.; Visseren, F.L.; Donnelly, T.J. Loss of myocardial protection after preconditioning correlates with the time course of glycogen recovery within the preconditioned segment. Circulation 1993, 87, 881–892. [Google Scholar] [CrossRef]
- Ventura-Clapier, R.; Garnier, A.; Veksler, V.; Joubert, F. Bioenergetics of the failing heart. Biochim. Biophys. Acta Mol. Cell Res. 2011, 1813, 1360–1372. [Google Scholar] [CrossRef] [PubMed]
- Madamanchi, N.R.; Runge, M.S. Redox signaling in cardiovascular health and disease. Free Rad. Biol. Med. 2013, 61, 473–501. [Google Scholar] [CrossRef] [PubMed]
- van Deel, E.D.; Lu, Z.; Xu, X.; Zhu, G.; Hu, X.; Oury, T.D.; Bache, R.J.; Duncker, D.J.; Chen, Y. Extracellular superoxide dismutase protects the heart against oxidative stress and hypertrophy after myocardial infarction. Free Rad. Biol. Med. 2008, 44, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Itoh, K.; Yamamoto, M.; Zweier, J.L.; Li, Y. Role of Nrf2 signaling in regulation of antioxidants and phase 2 enzymes in cardiac fibroblasts: Protection against reactive oxygen and nitrogen species-induced cell injury. FEBS Lett. 2005, 579, 3029–3036. [Google Scholar] [CrossRef] [PubMed]
- Bayram, B.; Ozcelik, B.; Grimm, S.; Roeder, T.; Schrader, C.; Ernst, I.M.A.; Wagner, A.E.; Grune, T.; Frank, J.; Rimbach, G. A diet rich in olive oil phenolics reduces oxidative stress in the heart of SAMP8 mice by induction of Nrf2-dependent gene expression. Rejuvenation Res. 2012, 15, 71–81. [Google Scholar] [CrossRef]
- Magesh, S.; Chen, Y.; Hu, L. Small molecule modulators of Keap1-Nrf2-ARE pathway as potential preventive and therapeutic agents. Med. Res. Rev. 2012, 32, 687–726. [Google Scholar] [CrossRef]
- Ścibior, A.; Kurus, J. Vanadium and oxidative stress markers-in vivo model: A review. Curr. Med. Chem. 2019, 26, 5456–5500. [Google Scholar] [CrossRef]
- Dalle-Donne, I.; Rossi, R.; Giustarini, D.; Milzani, A.; Colombo, R. Protein carbonyl groups as biomarkers of oxidative stress. Clin. Chim. Acta 2003, 329, 23–38. [Google Scholar] [CrossRef]
- Pereira, L.D.; Barbosa, J.M.G.; Ribeiro da Silva, A.J.; Ferri, P.H.; Santos, S.C. Polyphenol and ellagitannin constituents of jabuticaba (Myrciaria cauliflora) and chemical variability at different stages of fruit development. J. Agric. Food Chem. 2017, 65, 1209–1219. [Google Scholar] [CrossRef]
- Kalt, W.; Blumberg, J.B.; McDonald, J.E.; Vinqvist-Tymchuk, M.R.; Fillmore, S.A.; Graf, B.A.; O’Leary, J.M.; Milbury, P.E. Identification of anthocyanins in the liver, eye, and brain of blueberry-fed pigs. J. Agric. Food Chem. 2008, 56, 705–712. [Google Scholar] [CrossRef]
| Variables | C (n = 16) | I (n = 14) | IJ2 (n = 23) | IJ4 (n = 18) |
|---|---|---|---|---|
| Initial body weight (g) | 251 ± 19 | 239 ± 16 | 247 ± 23 | 245 ± 24 |
| Final body weight (g) | 379 ± 30 | 388 ± 25 | 400 ± 35 | 386 ± 32 |
| Feed intake (g/day) | 20 (19–22) | 21 (19–22) | 20 (19–21) | 19 (18–20) |
| Variables | C | I | IJ2 | IJ4 |
|---|---|---|---|---|
| LA (mm) | 5.4 ± 0.6 | 6.2 ± 0.9 * | 6.5 ± 0.8 * | 6.4 ± 0.8 * |
| LVDD (mm) | 7.1 ± 0.7 | 9.2 ± 0.5 * | 9.3 ± 0.7 * | 9.4 ± 0.7 * |
| LVSD (mm) | 2.8 ± 0.6 | 7.0 ± 0.6 * | 7.1 ± 0.8 * | 7.1 ± 0.9 * |
| EF (%) | 0.9 ± 0.1 | 0.5 ± 0.1 * | 0.5 ± 0.1 * | 0.6 ± 0.1 * |
| FAC (%) | 77 ± 6.7 | 35 ± 7.7 * | 33 ± 7.6 * | 32 ± 12 * |
| EDT | 43 ± 7.1 | 47 ± 6.8 * | 51 ± 11 * | 51 ± 10 * |
| IRT/RR0.5 | 52 ± 7.0 | 62 ± 10 * | 64 ± 9.5 * | 59 ± 10 |
| Variables | C (n = 8) | I (n = 8) | IJ2 (n = 8) | IJ4 (n = 8) |
|---|---|---|---|---|
| Phosphofructokinase (nmol/g) | 148 ± 29 | 355 ± 78 *# | 340 ± 99 *# | 134 ± 62 |
| Pyruvate dehydrogenase complex (nmol/g) | 282 ± 30 | 212 ± 56 | 244 ± 35 | 186 ± 37 * |
| Lactate dehydrogenase (nmol/g) | 61 ± 10 | 92 ± 28 * | 78 ± 14 | 91 ± 24 * |
| β-Hydroxyacyl-CoA dehydrogenase (nmol/mg) | 26 ± 5 | 10 ± 3 * | 8 ± 2 * | 9 ± 3 * |
| Citrate synthase (nmol/g) | 31 ± 6 | 16 ± 3 * | 17 ± 3* | 16 ± 3 * |
| Complex I (NADH dehydrogenase) (nmol/mg) | 10 ± 1 | 6 ± 1 * | 5 ± 1 * | 5 ± 1 * |
| Complex II (Succinate dehydrogenase) (nmol/mg) | 4.87 ± 0.88 | 2.75 ± 0.54 * | 2.88 ± 0.98 * | 2.55 ± 0.48 * |
| ATP synthase (nmol/mg) | 30 ± 5 | 18 ± 4 * | 23 ± 4 | 16 ± 4 * |
| Variables | C (n = 8) | I (n = 8) | IJ2 (n = 8) | IJ4 (n = 8) |
|---|---|---|---|---|
| LH (nmol/mg of tissue) | 244 ± 34 | 325 ± 45 * | 289 ± 42 | 234 ± 39 |
| CP (nmol/mg of protein) | 2.8 ± 0.4 | 4.7 ± 0.6 * | 4.4 ± 0.9 * | 4.9 ± 0.8 * |
| CAT (µmol/g of tissue) | 53 ± 6.8 | 37 ± 5.2 * | 34 ± 6.4 * | 34 ± 7.4 * |
| SOD (nmol/mg of tissue) | 15 ± 3.1 | 11 ± 1.3 * | 9.9 ± 1.8 * | 11 ± 1.9 * |
| GSH-Px (nmol/mg of tissue) | 41 ± 8.9 | 28 ± 6.7 * | 43 ± 9.2 | 41 ± 8.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, R.C.; Polegato, B.F.; Azevedo, P.S.; Fernandes, A.A.; Okoshi, K.; de Paiva, S.A.R.; Minicucci, M.F.; Zornoff, L.A.M. Jaboticaba (Myrciaria jaboticaba) Attenuates Ventricular Remodeling after Myocardial Infarction in Rats. Antioxidants 2022, 11, 249. https://doi.org/10.3390/antiox11020249
da Silva RC, Polegato BF, Azevedo PS, Fernandes AA, Okoshi K, de Paiva SAR, Minicucci MF, Zornoff LAM. Jaboticaba (Myrciaria jaboticaba) Attenuates Ventricular Remodeling after Myocardial Infarction in Rats. Antioxidants. 2022; 11(2):249. https://doi.org/10.3390/antiox11020249
Chicago/Turabian Styleda Silva, Renata Candido, Bertha Furlan Polegato, Paula Shmidt Azevedo, Ana Angélica Fernandes, Katashi Okoshi, Sergio Alberto Rupp de Paiva, Marcos Ferreira Minicucci, and Leonardo Antônio Mamede Zornoff. 2022. "Jaboticaba (Myrciaria jaboticaba) Attenuates Ventricular Remodeling after Myocardial Infarction in Rats" Antioxidants 11, no. 2: 249. https://doi.org/10.3390/antiox11020249
APA Styleda Silva, R. C., Polegato, B. F., Azevedo, P. S., Fernandes, A. A., Okoshi, K., de Paiva, S. A. R., Minicucci, M. F., & Zornoff, L. A. M. (2022). Jaboticaba (Myrciaria jaboticaba) Attenuates Ventricular Remodeling after Myocardial Infarction in Rats. Antioxidants, 11(2), 249. https://doi.org/10.3390/antiox11020249







