The Impact of a Plant-Based Diet on Gestational Diabetes: A Review
Abstract
1. Introduction
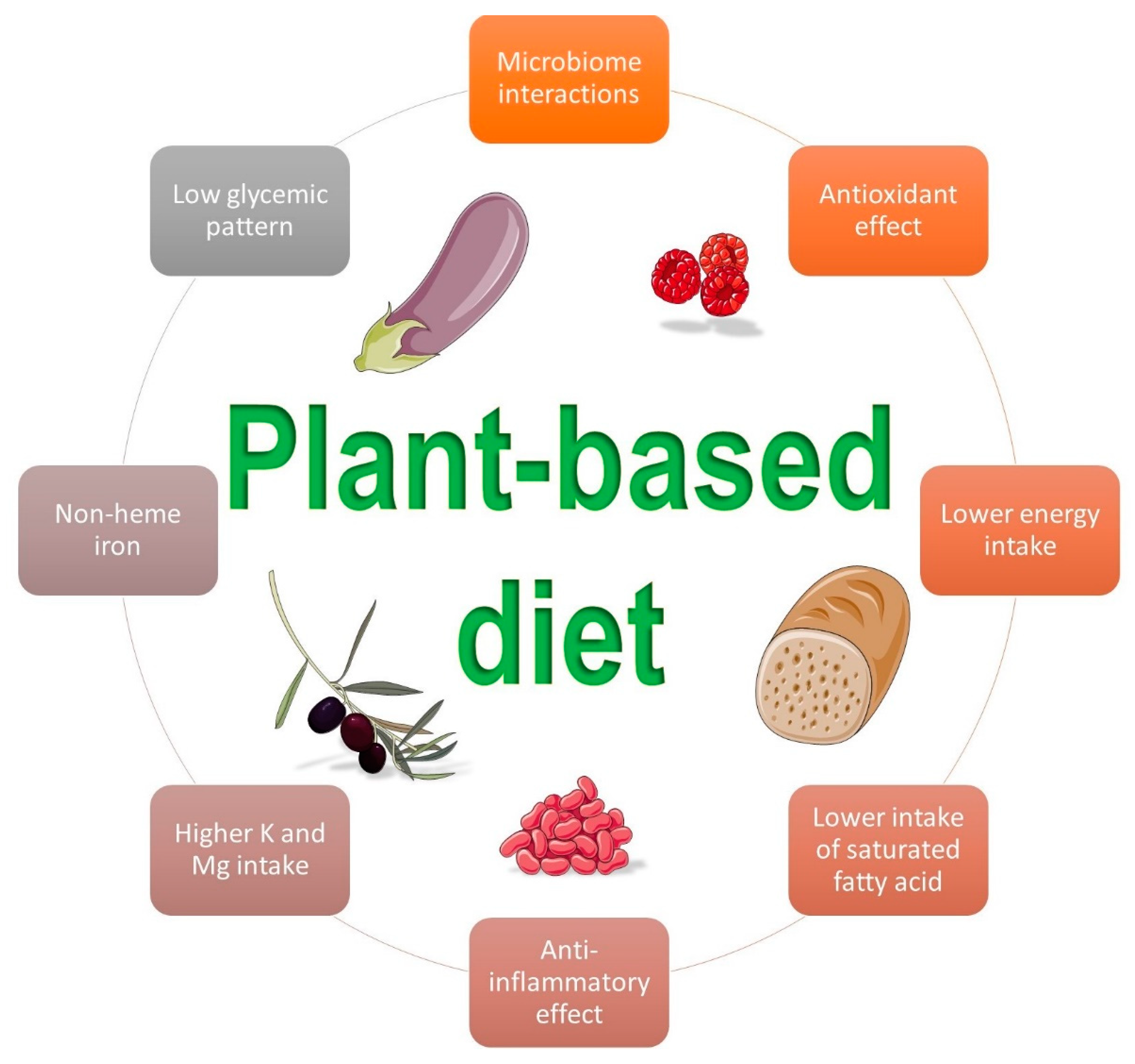
2. The Impact of a Plant-Based Diet on Gestational Diabetes
3. The Role of Insulin Sensitivity in Pregnancy
The Effects of a Plant-Based Diet on Insulin Sensitivity
4. The Link between Microbiota and Diet
The Effects of a Plant-Based Diet on Microbiota
5. Oxidative Stress and Insulin Resistance
The Effects of a Plant-Based Diet on Oxidative Stress
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AGE | Advanced Glycation End Products |
| Akt | Protein kinase B |
| ALA | Alpha-lipoic acid |
| ANG II | Angiotensin II |
| ApoA1 | Apolipoprotein A-1 |
| CRP | C-Reactive Protein |
| DASH | Dietary Approaches To Stop Hypertension |
| EVOO | Extra-Virgin Olive Oil |
| FFA | Free fatty acid |
| FT3 | Free Triiodothyronine |
| FT4 | Thyroxine |
| GDM | Gestational Diabetes Mellitus |
| GLUT | Glucose Transporter |
| GTX | Glutathione Peroxidase |
| HDL | High density lipoprotein |
| HPL | Human Placental Lactogen |
| I-κB | Kappa b inhibitor |
| IL | Interleukin |
| IRS-1 | Insulin Receptor Substrate 1 |
| MDA | Malondialdehyde |
| MedDiet | Mediterranean Diet |
| MTNR1B | Melatonin Receptor 1B |
| NAPDH | Nicotinamide Adenine Dinucleotide Phosphate |
| NF-κ | Nuclear Factor Kappa |
| NO | Nitric Oxide |
| P38 MAPK | Serine Kinase P38 Mitogen-activated Protein Kinase |
| PI 3-kinase | Phosphatidylinositol 3-kinase |
| PYR | Pyridoxamine |
| RAS | Renin–angiotensin system |
| RCT | Randomized Controlled Trial |
| ROS | Reactive Oxygen Species |
| SCFA | Short-chain Fatty Acid |
| SOD | Superoxide Dismutase |
| T2D | Type 2 Diabetes |
| TCF7L2 | Transcription Factor 7-like 2 |
| TNF-α | Tumor Necrosis Factor-α |
| TSH | Thyroid-stimulating hormone |
References
- Correa, A.; Bardenheier, B.; Elixhauser, A.; Geiss, L.S.; Gregg, E. Trends in Prevalence of Diabetes Among Delivery Hospitalizations, United States, 1993–2009. Matern. Child Health J. 2015, 19, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Mack, L.R.; Tomich, P.G. Gestational Diabetes. Obstet. Gynecol. Clin. N. Am. 2017, 44, 207–217. [Google Scholar] [CrossRef]
- Eades, C.E.; Cameron, D.M.; Evans, J.M. Prevalence of gestational diabetes mellitus in Europe: A meta-analysis. Diabetes Res. Clin. Pr. 2017, 129, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Todi, S.; Sagili, H.; Kamalanathan, S.K. Comparison of criteria of International Association of Diabetes and Pregnancy Study Groups (IADPSG) with National Institute for Health and Care Excellence (NICE) for diagnosis of gestational diabetes mellitus. Arch. Gynecol. Obstet. 2020, 302, 47–52. [Google Scholar] [CrossRef]
- Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 190: Gestational Diabetes Mellitus. Obstet. Gynecol. 2018, 131, e49–e64. [Google Scholar] [CrossRef] [PubMed]
- Caughey, A.B.; Cheng, Y.W.; Stotland, N.E.; Washington, A.E.; Escobar, G.J. Maternal and paternal race/ethnicity are both associated with gestational diabetes. Am. J. Obstet. Gynecol. 2010, 202, 616.e1–616.e5. [Google Scholar] [CrossRef] [PubMed]
- Robitaille, J.; Grant, A.M. The genetics of gestational diabetes mellitus: Evidence for relationship with type 2 diabetes mellitus. Genet. Med. 2008, 10, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.A.; Qiu, C.; Dempsey, J.C.; Luthy, D.A. Familial aggregation of type 2 diabetes and chronic hypertension in women with gestational diabetes mellitus. J. Reprod. Med. 2003, 48, 955–962. [Google Scholar]
- Wu, L.; Cui, L.; Tam, W.H.; Ma, R.C.W.; Wang, C.C. Genetic variants associated with gestational diabetes mellitus: A meta-analysis and subgroup analysis. Sci. Rep. 2016, 6, 1–9. [Google Scholar] [CrossRef]
- Xie, K.; Zhang, Y.; Wen, J.; Chen, T.; Kong, J.; Zhang, J.; Wu, X.; Hu, C.; Xu, B.; Ji, C.; et al. Genetic predisposition to gestational glucose metabolism and gestational diabetes mellitus risk in a Chinese population. J. Diabetes 2019, 11, 869–877. [Google Scholar] [CrossRef]
- Skórzyńska-Dziduszko, K.E.; Kimber-Trojnar, Ż.; Patro-Małysza, J.; Olszewska, A.; Zaborowski, T.; Małecka-Massalska, T. An Interplay between Obesity and Inflammation in Gestational Diabetes Mellitus. Curr. Pharm. Biotechnol. 2016, 17, 603–613. [Google Scholar] [CrossRef]
- Alamolhoda, S.H.; Yazdkhasti, M.; Namdari, M.; Zakariayi, S.J.; Mirabi, P. Association between C-reactive protein and gestational diabetes: A prospective study. J. Obstet. Gynaecol. 2019, 40, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Qiu, C.; Zhang, C.; Gelaye, B.; Enquobahrie, D.A.; Frederick, I.O.; Williams, M.A. Gestational Diabetes Mellitus in Relation to Maternal Dietary Heme Iron and Nonheme Iron Intake. Diabetes Care 2011, 34, 1564–1569. [Google Scholar] [CrossRef]
- Fu, S.; Li, F.; Zhou, J.; Liu, Z. The Relationship Between Body Iron Status, Iron Intake and Gestational Diabetes. Medicine 2016, 95, e2383. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, G.; Garzon, S.; Fichera, M.; Panella, M.M.; Catena, U.; Schiattarella, A.; De Franciscis, P.; Vilos, G.; Tesarik, J.; Török, P.; et al. Vitamin D and Gestational Diabetes Mellitus: Is There a Link? Antioxidants 2019, 8, 511. [Google Scholar] [CrossRef] [PubMed]
- Donazar-Ezcurra, M.; Burgo, C.L.-D.; Bes-Rastrollo, M. Primary prevention of gestational diabetes mellitus through nutritional factors: A systematic review. BMC Pregnancy Childbirth 2017, 17, 1–5. [Google Scholar] [CrossRef]
- Rogozińska, E.; Chamillard, M.; Hitman, G.A.; Khan, K.S.; Thangaratinam, S. Nutritional Manipulation for the Primary Prevention of Gestational Diabetes Mellitus: A Meta-Analysis of Randomised Studies. PLoS ONE 2015, 10, e0115526. [Google Scholar] [CrossRef]
- Song, C.; Li, J.; Leng, J.; Ma, R.C.; Yang, X. Lifestyle intervention can reduce the risk of gestational diabetes: A meta-analysis of randomized controlled trials. Obes. Rev. 2016, 17, 960–969. [Google Scholar] [CrossRef]
- Kesary, Y.; Avital, K.; Hiersch, L. Maternal plant-based diet during gestation and pregnancy outcomes. Arch. Gynecol. Obstet. 2020, 302, 887–898. [Google Scholar] [CrossRef]
- Barger, M.K. Maternal Nutrition and Perinatal Outcomes. J. Midwifery Women’s Health 2010, 55, 502–511. [Google Scholar] [CrossRef]
- Pistollato, F.; Cano, S.S.; Elio, I.; Vergara, M.M.; Giampieri, F.; Battino, M. Plant-Based and Plant-Rich Diet Patterns during Gestation: Beneficial Effects and Possible Shortcomings. Adv. Nutr. 2015, 6, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Assaf-Balut, C.; De La Torre, N.G.; Durán, A.; Fuentes, M.; Bordiú, E.; Del Valle, L.; Familiar, C.; Ortolá, A.; Jiménez, I.; Herraiz, M.A.; et al. A Mediterranean diet with additional extra virgin olive oil and pistachios reduces the incidence of gestational diabetes mellitus (GDM): A randomized controlled trial: The St. Carlos GDM prevention study. PLoS ONE 2017, 12, e0185873. [Google Scholar] [CrossRef] [PubMed]
- Zamani, B.; Milajerdi, A.; Tehrani, H.; Bellissimo, N.; Brett, N.R.; Azadbakht, L. Association of a plant-based dietary pattern in relation to gestational diabetes mellitus. Nutr. Diet. 2019, 76, 589–596. [Google Scholar] [CrossRef]
- Genc, S.; Kusku-Kiraz, Z.; Dervisoglu, E.; Oztop, N.; Dinccag, N.; Gurdol, F. The Relation of Oxidative Stress Biomarkers with Proinflammatory Cytokines in Gestational Diabetes. Clin. Investig. 2017, 7, 44–48. [Google Scholar] [CrossRef]
- Kregel, K.C.; Zhang, H.J. An integrated view of oxidative stress in aging: Basic mechanisms, functional effects, and pathological considerations. Am. J. Physiol. Integr. Comp. Physiol. 2007, 292, R18–R36. [Google Scholar] [CrossRef] [PubMed]
- Jensen, L.A.; Chik, C.L.; Ryan, E.A. Review of gestational diabetes mellitus effects on vascular structure and function. Diabetes Vasc. Dis. Res. 2016, 13, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Khambule, L.; George, J.A. The Role of Inflammation in the Development of GDM and the Use of Markers of Inflammation in GDM Screening. Adv. Exp. Med. Biol. 2019, 1134, 217–242. [Google Scholar] [CrossRef]
- Shikany, J.M.; Safford, M.M.; Newby, P.K.; Durant, R.W.; Brown, T.M.; Judd, S.E. Southern Dietary Pattern Is Associated with Hazard of Acute Coronary Heart Disease in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circulation 2015, 132, 804–814. [Google Scholar] [CrossRef] [PubMed]
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef]
- Craig, W.J.; Mangels, A.R. American Dietetic Association Position of the American Dietetic Association: Vegetarian Diets. J. Am. Diet. Assoc. 2009, 109, 1266–1282. [Google Scholar] [CrossRef]
- Sebastiani, G.; Barbero, A.H.; Borràs-Novell, C.; Alsina, M.; Aldecoa-Bilbao, V.; Andreu-Fernández, V.; Tutusaus, M.P.; Martínez, S.F.; Gómez-Roig, M.D.; García-Algar, Ó. The Effects of Vegetarian and Vegan Diet during Pregnancy on the Health of Mothers and Offspring. Nutrients 2019, 11, 557. [Google Scholar] [CrossRef]
- Baroni, L.; Rizzo, G.; Goggi, S.; Giampieri, F.; Battino, M. Vegetarian diets during pregnancy: Effects on the mother’s health. A systematic review. Food Funct. 2021, 12, 466–493. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Matoulek, M.; Malinska, H.; Oliyarnik, O.; Kazdova, L.; Neskudla, T.; Skoch, A.; Hajek, M.; Hill, M.; Kahle, M.; et al. Vegetarian diet improves insulin resistance and oxidative stress markers more than conventional diet in subjects with Type 2 diabetes. Diabet. Med. 2011, 28, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Zulyniak, M.A.; De Souza, R.J.; Shaikh, M.; Desai, D.; Lefebvre, D.L.; Gupta, M.; Wilson, J.; Wahi, G.; Subbarao, P.; Becker, A.B.; et al. Does the impact of a plant-based diet during pregnancy on birth weight differ by ethnicity? A dietary pattern analysis from a prospective Canadian birth cohort alliance. BMJ Open 2017, 7, e017753. [Google Scholar] [CrossRef]
- De La Torre, N.G.; Assaf-Balut, C.; Varas, I.J.; Del Valle, L.; Durán, A.; Fuentes, M.; Del Prado, N.; Bordiú, E.; Valerio, J.J.; Herraiz, M.A.; et al. Effectiveness of Following Mediterranean Diet Recommendations in the Real World in the Incidence of Gestational Diabetes Mellitus (GDM) and Adverse Maternal-Foetal Outcomes: A Prospective, Universal, Interventional Study with a Single Group. The St Carlos Study. Nutrition 2019, 11, 1210. [Google Scholar] [CrossRef]
- Karamanos, B.; The MGSD-GDM Study Group; Thanopoulou, A.; Anastasiou, E.; Assaad-Khalil, S.; Albache, N.; Bachaoui, M.; Slama, C.B.; El Ghomari, H.; Jotic, A.; et al. Relation of the Mediterranean diet with the incidence of gestational diabetes. Eur. J. Clin. Nutr. 2014, 68, 8–13. [Google Scholar] [CrossRef]
- Olmedo-Requena, R.; Gómez-Fernández, J.; Amezcua-Prieto, C.; Mozas-Moreno, J.; Khan, K.S.; Jiménez-Moleón, J.J. Pre-Pregnancy Adherence to the Mediterranean Diet and Gestational Diabetes Mellitus: A Case-Control Study. Nutrition. 2019, 11, 1003. [Google Scholar] [CrossRef]
- Mak, J.K.L.; Pham, N.M.; Lee, A.H.; Tang, L.; Pan, X.-F.; Binns, C.W.; Sun, X. Dietary patterns during pregnancy and risk of gestational diabetes: A prospective cohort study in Western China. Nutr. J. 2018, 17, 1–11. [Google Scholar] [CrossRef]
- Izadi, V.; Tehrani, H.; Haghighatdoost, F.; Dehghan, A.; Surkan, P.J.; Azadbakht, L. Adherence to the DASH and Mediterranean diets is associated with decreased risk for gestational diabetes mellitus. Nutrition 2016, 32, 1092–1096. [Google Scholar] [CrossRef]
- Jali, M.V.; Desai, B.R.; Gowda, S.; Kambar, S.; Jali, S.M. A hospital based study of prevalence of gestational diabetes mellitus in an urban population of India. Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 1306–1310. [Google Scholar] [PubMed]
- Arora, G.P.; Thaman, R.G.; Prasad, R.B.; Almgren, P.; Brøns, C.; Groop, L.C.; Vaag, A.A. Prevalence and risk factors of gestational diabetes in Punjab, North India: Results from a population screening program. Eur. J. Endocrinol. 2015, 173, 257–267. [Google Scholar] [CrossRef] [PubMed]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016, 65, 1812–1821. [Google Scholar] [CrossRef]
- Wada, T.; Hori, S.; Sugiyama, M.; Fujisawa, E.; Nakano, T.; Tsuneki, H.; Nagira, K.; Saito, S.; Sasaoka, T. Progesterone inhibits glucose uptake by affecting diverse steps of insulin signaling in 3T3-L1 adipocytes. Am. J. Physiol. Metab. 2010, 298, E881–E888. [Google Scholar] [CrossRef]
- Barrett, H.L.; Gomez-Arango, L.F.; Wilkinson, S.A.; McIntyre, H.D.; Callaway, L.K.; Morrison, M.; Nitert, M.D. A Vegetarian Diet Is a Major Determinant of Gut Microbiota Composition in Early Pregnancy. Nutrition 2018, 10, 890. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, S.; Solomon, C.G.; Hu, F.B. Dietary Fiber Intake, Dietary Glycemic Load, and the Risk for Gestational Diabetes Mellitus. Diabetes Care 2006, 29, 2223–2230. [Google Scholar] [CrossRef]
- Barbour, L.A.; McCurdy, C.E.; Hernandez, T.L.; Kirwan, J.P.; Catalano, P.M.; Friedman, J.E. Cellular Mechanisms for Insulin Resistance in Normal Pregnancy and Gestational Diabetes. Diabetes Care 2007, 30, S112–S119. [Google Scholar] [CrossRef]
- Friedman, J.E.; Ishizuka, T.; Shao, J.; Huston, L.; Highman, T.; Catalano, P. Impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Diabetes 1999, 48, 1807–1814. [Google Scholar] [CrossRef]
- Stanley, K.; Fraser, R.; Bruce, C. Physiological changes in insulin resistance in human pregnancy: Longitudinal study with the hyperinsulinaemic euglycaemic clamp technique. Br. J. Obstet. Gynaecol. 1998, 105, 756–759. [Google Scholar] [CrossRef] [PubMed]
- Mauri, M.; Calmarza, P.; Ibarretxe, D. Dislipemias y embarazo, una puesta al día. Clín. Investig. Arterioscler. 2021, 33, 41–52. [Google Scholar] [CrossRef]
- Sonagra, A.D. Normal Pregnancy—A State of Insulin Resistance. J. Clin. Diagn. Res. 2014, 8, CC01. [Google Scholar] [CrossRef] [PubMed]
- Catalano, P.M.; Nizielski, S.E.; Shao, J.; Preston, L.; Qiao, L.; Friedman, J.E. Downregulated IRS-1 and PPARγ in obese women with gestational diabetes: Relationship to FFA during pregnancy. Am. J. Physiol. Metab. 2002, 282, E522–E533. [Google Scholar] [CrossRef]
- Catalano, P.M.; Huston, L.; Amini, S.B.; Kalhan, S.C. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am. J. Obstet. Gynecol. 1999, 180, 903–916. [Google Scholar] [CrossRef]
- White, M.F.; Kahn, C.R. The insulin signaling system. J. Biol. Chem. 1994, 269, 1–4. [Google Scholar] [CrossRef]
- Herbst, J.J.; Andrews, G.C.; Contillo, L.G.; Singleton, D.H.; Genereux, P.E.; Gibbs, E.M.; Lienhard, G.E. Effect of the Activation of Phosphatidylinositol 3-Kinase by a Thiophosphotyrosine Peptide on Glucose Transport in 3T3-L1 Adipocytes. J. Biol. Chem. 1995, 270, 26000–26005. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, G.K.; Yu, J.G.; Ofrecio, J.; Olefsky, J.M. Increased p85/55/50 Expression and Decreased Phosphotidylinositol 3-Kinase Activity in Insulin-Resistant Human Skeletal Muscle. Diabetes 2005, 54, 2351–2359. [Google Scholar] [CrossRef]
- Retnakaran, R.; Ye, C.; Connelly, P.W.; Hanley, A.J.; Sermer, M.; Zinman, B. Serum apoA1 (Apolipoprotein A-1), Insulin Resistance, and the Risk of Gestational Diabetes Mellitus in Human Pregnancy—Brief Report. Arter. Thromb. Vasc. Biol. 2019, 39, 2192–2197. [Google Scholar] [CrossRef] [PubMed]
- Rye, K.-A.; Barter, P.J.; Cochran, B.J. Apolipoprotein A-I interactions with insulin secretion and production. Curr. Opin. Lipidol. 2016, 27, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Lea, R.G.; Howe, D.; Hannah, L.T.; Bonneau, O.; Hunter, L.; Hoggard, N. Placental leptin in normal, diabetic and fetal growth-retarded pregnancies. Mol. Hum. Reprod. 2000, 6, 763–769. [Google Scholar] [CrossRef]
- Zavalza-Gómez, A.B.; Anaya-Prado, R.; Rincón-Sánchez, A.R.; Mora-Martínez, J.M. Adipokines and insulin resistance during pregnancy. Diabetes Res. Clin. Pract. 2008, 80, 8–15. [Google Scholar] [CrossRef]
- Catalano, P.M.; Hoegh, M.; Minium, J.; Huston-Presley, L.; Bernard, S.; Kalhan, S.; Mouzon, S.H.-D. Adiponectin in human pregnancy: Implications for regulation of glucose and lipid metabolism. Diabetologia 2006, 49, 1677–1685. [Google Scholar] [CrossRef]
- Akerman, F.; Lei, Z.M.; Rao, C. V Human umbilical cord and fetal membranes co-express leptin and its receptor genes. Gynecol. Endocrinol. 2002, 16, 299–306. [Google Scholar] [CrossRef]
- Biondi, B.; Kahaly, G.J.; Robertson, R.P. Thyroid Dysfunction and Diabetes Mellitus: Two Closely Associated Disorders. Endocr. Rev. 2019, 40, 789–824. [Google Scholar] [CrossRef]
- Yanachkova, V.E.; Kamenov, Z. The relationship between Thyroid dysfunction during pregnancy and Gestational diabetes mellitus. Endokrynol. Polska 2021. [Google Scholar] [CrossRef]
- Zheng, R.; Zhang, J.; Ying, Z.; Zheng, N. Low Serum Amylase is Associated with Gestational Diabetes Mellitus in Chinese Pregnant Women. Clin. Lab. 2015, 59, 64. [Google Scholar] [CrossRef]
- Yu, F.; Zhou, W.; Tan, X.; Jiang, Y. Gestational Diabetes Mellitus is Associated with Plasma Amylase in a Chinese Pregnant Women Population. Clin. Lab. 2019, 65, 65. [Google Scholar] [CrossRef]
- Palmisano, B.T.; Zhu, L.; Stafford, J.M. Role of Estrogens in the Regulation of Liver Lipid Metabolism. Adv. Exper. Med. Biol. 2017, 1043, 227–256. [Google Scholar] [CrossRef]
- McKenzie, J.; Fisher, B.M.; Jaap, A.J.; Stanley, A.; Paterson, K.; Sattar, N. Effects of HRT on liver enzyme levels in women with type 2 diabetes: A randomized placebo-controlled trial. Clin. Endocrinol. 2006, 65, 40–44. [Google Scholar] [CrossRef]
- Khoo, C.L.; Perera, M. Diabetes and the menopause. Br. Menopause Soc. J. 2005, 11, 6–11. [Google Scholar] [CrossRef]
- Sibiak, R.; Jankowski, M.; Gutaj, P.; Mozdziak, P.; Kempisty, B.; Wender-Ożegowska, E. Placental Lactogen as a Marker of Maternal Obesity, Diabetes, and Fetal Growth Abnormalities: Current Knowledge and Clinical Perspectives. J. Clin. Med. 2020, 9, 1142. [Google Scholar] [CrossRef]
- Kahleova, H.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N.D. A Plant-Based Dietary Intervention Improves Beta-Cell Function and Insulin Resistance in Overweight Adults: A 16-Week Randomized Clinical Trial. Nutrition 2018, 10, 189. [Google Scholar] [CrossRef]
- Barnard, N.D.; Scialli, A.R.; Turner-McGrievy, G.; Lanou, A.J.; Glass, J. The effects of a low-fat, plant-based dietary intervention on body weight, metabolism, and insulin sensitivity. Am. J. Med. 2005, 118, 991–997. [Google Scholar] [CrossRef]
- Kahleova, H.; Levin, S.; Barnard, N. Cardio-Metabolic Benefits of Plant-Based Diets. Nutrition 2017, 9, 848. [Google Scholar] [CrossRef]
- Livesey, G.; Tagami, H. Interventions to lower the glycemic response to carbohydrate foods with a low-viscosity fiber (resistant maltodextrin): Meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2008, 89, 114–125. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Whincup, P.H.; Thomas, M.C.; Sattar, N. Associations Between Dietary Fiber and Inflammation, Hepatic Function, and Risk of Type 2 Diabetes in Older Men: Potential mechanisms for the benefits of fiber on diabetes risk. Diabetes Care 2009, 32, 1823–1825. [Google Scholar] [CrossRef]
- Mirabelli, M.; Chiefari, E.; Arcidiacono, B.; Corigliano, D.M.; Brunetti, F.S.; Maggisano, V.; Russo, D.; Foti, D.P.; Brunetti, A. Mediterranean Diet Nutrients to Turn the Tide against Insulin Resistance and Related Diseases. Nutrients 2020, 12, 1066. [Google Scholar] [CrossRef]
- Kahleova, H.; Tura, A.; Klementova, M.; Thieme, L.; Haluzik, M.; Pavlovicova, R.; Hill, M.; Pelikanova, T. A Plant-Based Meal Stimulates Incretin and Insulin Secretion More Than an Energy- and Macronutrient-Matched Standard Meal in Type 2 Diabetes: A Randomized Crossover Study. Nutrients 2019, 11, 486. [Google Scholar] [CrossRef]
- Bligh, H.F.J.; Godsland, I.F.; Frost, G.; Hunter, K.J.; Murray, P.; Macaulay, K.; Hyliands, D.; Talbot, D.C.S.; Casey, J.; Mulder, T.P.J.; et al. Plant-rich mixed meals based on Palaeolithic diet principles have a dramatic impact on incretin, peptide YY and satiety response, but show little effect on glucose and insulin homeostasis: An acute-effects randomised study. Br. J. Nutr. 2015, 113, 574–584. [Google Scholar] [CrossRef]
- Taddei, C.R.; Cortez, R.V.; Mattar, R.; Torloni, M.R.; Daher, S. Microbiome in normal and pathological pregnancies: A literature overview. Am. J. Reprod. Immunol. 2018, 80, e12993. [Google Scholar] [CrossRef]
- Schiattarella, A.; Riemma, G.; La Verde, M.; Franci, G.; Chianese, A.; Fasulo, D.; Fichera, M.; Gallo, P.; De Franciscis, P. Polycystic Ovary Syndrome and Probiotics: A Natural Approach to an Inflammatory Disease. Curr. Women’s Health Rev. 2021, 17, 14–20. [Google Scholar] [CrossRef]
- Blaser, M.J. Who are we? EMBO Rep. 2006, 7, 956–960. [Google Scholar] [CrossRef]
- McKenzie, C.; Tan, J.; Macia, L.; Mackay, C.R. The nutrition-gut microbiome-physiology axis and allergic diseases. Immunol. Rev. 2017, 278, 277–295. [Google Scholar] [CrossRef]
- Koren, O.; Goodrich, J.K.; Cullender, T.C.; Spor, A.; Laitinen, K.; Bäckhed, H.K.; Gonzalez, A.; Werner, J.J.; Angenent, L.T.; Knight, R.; et al. Host Remodeling of the Gut Microbiome and Metabolic Changes during Pregnancy. Cell 2012, 150, 470–480. [Google Scholar] [CrossRef]
- Blaser, M.J.; Dominguez-Bello, M.G. The Human Microbiome before Birth. Cell Host Microbe 2016, 20, 558–560. [Google Scholar] [CrossRef]
- Ardissone, A.N.; De La Cruz, D.M.; Davis-Richardson, A.G.; Rechcigl, K.T.; Li, N.; Drew, J.C.; Murgas-Torrazza, R.; Sharma, R.; Hudak, M.L.; Triplett, E.W.; et al. Meconium Microbiome Analysis Identifies Bacteria Correlated with Premature Birth. PLoS ONE 2014, 9, e90784. [Google Scholar] [CrossRef]
- Collado, M.C.; Isolauri, E.; Laitinen, K.; Salminen, S. Distinct composition of gut microbiota during pregnancy in overweight and normal-weight women. Am. J. Clin. Nutr. 2008, 88, 894–899. [Google Scholar] [CrossRef]
- Aagaard, K.; Ma, J.; Antony, K.M.; Ganu, R.; Petrosino, J.; Versalovic, J. The Placenta Harbors a Unique Microbiome. Sci. Transl. Med. 2014, 6, 237ra65. [Google Scholar] [CrossRef]
- Han, Y.W.; Shen, T.; Chung, P.; Buhimschi, I.A.; Buhimschi, C.S. Uncultivated Bacteria as Etiologic Agents of Intra-Amniotic Inflammation Leading to Preterm Birth. J. Clin. Microbiol. 2008, 47, 38–47. [Google Scholar] [CrossRef]
- Lauder, A.P.; Roche, A.M.; Sherrill-Mix, S.; Bailey, A.; Laughlin, A.L.; Bittinger, K.; Leite, R.; Elovitz, M.A.; Parry, S.; Bushman, F.D. Comparison of placenta samples with contamination controls does not provide evidence for a distinct placenta microbiota. Microbiome 2016, 4, 1–11. [Google Scholar] [CrossRef]
- Kuang, Y.-S.; Lu, J.-H.; Li, S.-H.; Li, J.-H.; Yuan, M.-Y.; He, J.-R.; Chen, N.-N.; Xiao, W.-Q.; Shen, S.-Y.; Qiu, L.; et al. Connections between the human gut microbiome and gestational diabetes mellitus. GigaScience 2017, 6, 1–12. [Google Scholar] [CrossRef]
- Pedersen, H.K.; Gudmundsdottir, V.; Nielsen, H.B.; Hyotylainen, T.; Nielsen, T.; Jensen, B.A.H.; Forslund, K.; Hildebrand, F.; Prifti, E.; Falony, G.; et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nat. Cell Biol. 2016, 535, 376–381. [Google Scholar] [CrossRef]
- Fugmann, M.; Breier, M.; Rottenkolber, M.; Banning, F.; Ferrari, U.; Sacco, V.; Grallert, H.; Parhofer, K.G.; Seissler, J.; Clavel, T.; et al. The stool microbiota of insulin resistant women with recent gestational diabetes, a high risk group for type 2 diabetes. Sci. Rep. 2015, 5, 1–8. [Google Scholar] [CrossRef]
- Acuna, J.; Cohavy, O.; Solt, I.; Reeder, J.; Kim, M.; Lebovics, I.; Paster, B.; Knight, R.; Rotmensch, S. 257: Preliminary observations on the microbial phylogeny of the oral, vaginal, and rectal microbiome in gestational diabetes and healthy pregnancies. Am. J. Obstet. Gynecol. 2011, 204, S109–S110. [Google Scholar] [CrossRef]
- Bassols, J.; Serino, M.; Carreras-Badosa, G.; Burcelin, R.; Blasco-Baque, V.; Lopez-Bermejo, A.; Fernandez-Real, J.-M. Gestational diabetes is associated with changes in placental microbiota and microbiome. Pediatr. Res. 2016, 80, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Thorburn, A.N.; Macia, L.; Mackay, C.R. Diet, Metabolites, and “Western-Lifestyle” Inflammatory Diseases. Immunity 2014, 40, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Sultana, Z.; Maiti, K.; Aitken, J.; Morris, J.; Dedman, L.; Smith, R. Oxidative stress, placental ageing-related pathologies and adverse pregnancy outcomes. Am. J. Reprod. Immunol. 2017, 77, e12653. [Google Scholar] [CrossRef]
- Henriksen, E.J.; Diamond-Stanic, M.K.; Marchionne, E.M. Oxidative stress and the etiology of insulin resistance and type 2 diabetes. Free Radic. Biol. Med. 2011, 51, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Ozler, S.; Oztas, E.; Uygur, D.; Ersoy, A.O.; Ergin, M.; Koca, C.; Danisman, N.; Erkaya, S. The Value of Total antioxidant Status and Serum Tumor Necrosis Factor-α Levels at 24–28 Weeks of Gestation in the Prediction of Optimal Treatment Protocol in Gestational Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2015, 127, 485–491. [Google Scholar] [CrossRef]
- Shang, M.; Zhao, J.; Yang, L.; Lin, L. Oxidative stress and antioxidant status in women with gestational diabetes mellitus diagnosed by IADPSG criteria. Diabetes Res. Clin. Pr. 2015, 109, 404–410. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Żebrowska, E.; Chabowski, A. Insulin Resistance and Oxidative Stress in the Brain: What’s New? Int. J. Mol. Sci. 2019, 20, 874. [Google Scholar] [CrossRef]
- Arnold, S.E.; Lucki, I.; Brookshire, B.R.; Carlson, G.C.; Browne, C.A.; Kazi, H.; Bang, S.; Choi, B.-R.; Chen, Y.; McMullen, M.F.; et al. High fat diet produces brain insulin resistance, synaptodendritic abnormalities and altered behavior in mice. Neurobiol. Dis. 2014, 67, 79–87. [Google Scholar] [CrossRef]
- Banks, W.A.; Owen, J.B.; Erickson, M.A. Insulin in the brain: There and back again. Pharmacol. Ther. 2012, 136, 82–93. [Google Scholar] [CrossRef]
- Scherer, T.; O’Hare, J.; Diggs-Andrews, K.; Schweiger, M.; Cheng, B.; Lindtner, C.; Zielinski, E.; Vempati, P.; Su, K.; Dighe, S.; et al. Brain Insulin Controls Adipose Tissue Lipolysis and Lipogenesis. Cell Metab. 2011, 13, 183–194. [Google Scholar] [CrossRef]
- Murthy, K.A.S.; Bhandiwada, A.; Chandan, S.L.; Gowda, S.L.; Sindhusree, G. Evaluation of oxidative stress and proinflammatory cytokines in gestational diabetes mellitus and their correlation with pregnancy outcome. Indian J. Endocrinol. Metab. 2018, 22, 79–84. [Google Scholar] [CrossRef]
- Jamilian, M.; Dizaji, S.H.; Bahmani, F.; Taghizadeh, M.; Memarzadeh, M.R.; Karamali, M.; Akbari, M.; Asemi, Z. A Randomized Controlled Clinical Trial Investigating the Effects of Omega-3 Fatty Acids and Vitamin E Co-Supplementation on Biomarkers of Oxidative Stress, Inflammation and Pregnancy Outcomes in Gestational Diabetes. Can. J. Diabetes 2017, 41, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Sowers, J.R.; Nistala, R.; Gong, H.; Uptergrove, G.M.-E.; Clark, S.E.; Morris, E.M.; Szary, N.; Manrique, C.; Stump, C.S. Angiotensin II-induced NADPH Oxidase Activation Impairs Insulin Signaling in Skeletal Muscle Cells. J. Biol. Chem. 2006, 281, 35137–35146. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Sowers, J.R.; Clark, S.E.; Li, W.; Ferrario, C.M.; Stump, C.S. Angiotensin II-induced skeletal muscle insulin resistance mediated by NF-κB activation via NADPH oxidase. Am. J. Physiol. Metab. 2008, 294, E345–E351. [Google Scholar] [CrossRef]
- Akaishi, T.; Abe, M.; Okuda, H.; Ishizawa, K.; Abe, T.; Ishii, T.; Ito, S. High glucose level and angiotensin II type 1 receptor stimulation synergistically amplify oxidative stress in renal mesangial cells. Sci. Rep. 2019, 9, 1–7. [Google Scholar] [CrossRef]
- Ghelani, H.; Razmovski-Naumovski, V.; Pragada, R.R.; Nammi, S. (R)-α-Lipoic acid inhibits fructose-induced myoglobin fructation and the formation of advanced glycation end products (AGEs) in vitro. BMC Complement. Altern. Med. 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Lewis, E.J.; Greene, T.; Spitalewiz, S.; Blumenthal, S.; Berl, T.; Hunsicker, L.G.; Pohl, M.A.; Rohde, R.D.; Raz, I.; Yerushalmy, Y.; et al. Pyridorin in Type 2 Diabetic Nephropathy. J. Am. Soc. Nephrol. 2011, 23, 131–136. [Google Scholar] [CrossRef]
- Williams, M.E.; Bolton, W.K.; Khalifah, R.G.; Degenhardt, T.P.; Schotzinger, R.J.; McGill, J.B. Effects of Pyridoxamine in Combined Phase 2 Studies of Patients with Type 1 and Type 2 Diabetes and Overt Nephropathy. Am. J. Nephrol. 2007, 27, 605–614. [Google Scholar] [CrossRef]
- Karam, B.S.; Chavez-Moreno, A.; Koh, W.; Akar, J.G.; Akar, F.G. Oxidative stress and inflammation as central mediators of atrial fibrillation in obesity and diabetes. Cardiovasc. Diabetol. 2017, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Capra, L.; Tezza, G.; Mazzei, F.; Boner, A.L. The origins of health and disease: The influence of maternal diseases and lifestyle during gestation. Ital. J. Pediatr. 2013, 39, 1–12. [Google Scholar] [CrossRef]
- Piccoli, G.B.; Clari, R.; Vigotti, F.N.; Leone, F.; Attini, R.; Cabiddu, G.; Mauro, G.; Castelluccia, N.; Colombi, N.; Capizzi, I.; et al. Vegan-vegetarian diets in pregnancy: Danger or panacea? A systematic narrative review. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Longo-Mbenza, B.; Kadima-Tshimanga, B.; Buassa-Bu-Tsumbu, B.; M’Buyamba, K. Diets rich in vegetables and physical activity are associated with a decreased risk of pregnancy induced hypertension among rural women from Kimpese, DR Congo. Niger. J. Med. 2008, 17, 45–49. [Google Scholar]
- Chuang, S.-Y.; Chiu, T.H.; Lee, C.-Y.; Liu, T.-T.; Tsao, C.K.; Hsiung, C.A.; Chiu, Y.-F. Vegetarian diet reduces the risk of hypertension independent of abdominal obesity and inflammation. J. Hypertens. 2016, 34, 2164–2171. [Google Scholar] [CrossRef]
- Orlich, M.J.; Singh, P.N.; Sabaté, J.; Fan, J.; Sveen, L.; Bennett, H.; Knutsen, S.F.; Beeson, W.L.; Jaceldo-Siegl, K.; Butler, T.L.; et al. Vegetarian Dietary Patterns and the Risk of Colorectal Cancers. JAMA Intern. Med. 2015, 175, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Tantamango-Bartley, Y.; Knutsen, S.F.; Knutsen, R.; Jacobsen, B.K.; Fan, J.; Beeson, W.L.; Sabate, J.; Hadley, D.; Jaceldo-Siegl, K.; Penniecook, J.; et al. Are strict vegetarians protected against prostate cancer? Am. J. Clin. Nutr. 2016, 103, 153–160. [Google Scholar] [CrossRef]
- Kerley, C.P. A Review of Plant-based Diets to Prevent and Treat Heart Failure. Card. Fail. Rev. 2018, 4, 54–61. [Google Scholar] [CrossRef]
- Tobore, T.O. Towards a comprehensive theory of obesity and a healthy diet: The causal role of oxidative stress in food addiction and obesity. Behav. Brain Res. 2020, 384, 112560. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.R.; Bryan, J.; Hodgson, J.M.; Murphy, K.J. Definition of the Mediterranean Diet; A Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- De Franciscis, P.; Conte, A.; Schiattarella, A.; Riemma, G.; Cobellis, L.; Colacurci, N. Non-hormonal Treatments for Menopausal Symptoms and Sleep Disturbances: A Comparison Between Purified Pollen Extracts and Soy Isoflavones. Curr. Pharm. Des. 2020, 26, 4509–4514. [Google Scholar] [CrossRef] [PubMed]
| Reference | Type of Study | Main Outcome | Number of Participants | Event | Definition of Plant-Based Diet |
|---|---|---|---|---|---|
| Arora et al., India [41] | Observational, cross-sectional | An increased risk of developing GDM was associated with a non-vegetarian diet | 5100 women | The prevalence of GDM was 35% using WHO 2013 criteria | Vegetarian diet |
| Barrett et al., Australia [44] | RCT | A vegetarian diet in early pregnancy increased the presence of short-chain fatty acid bacteria producers without any influence on GDM risk | 9 following a vegetarian diet and 18 an omnivorous one | Microbiome alpha diversity was similar, while beta diversity was reduced, in vegetarians | Vegetarian diet |
| De Filippis et al., Italy [42] | Observational | An increased consumption of plant foodstuffs based on a MedDiet was associated with beneficial microbiota improvements | 51 vegetarians, 51 vegans, and 51 omnivores | Positive correlation between consumption of vegetables and short-chain fatty acids, Prevotella, and Firmicutes in the gut microbiome | MedDiet |
| García de la Torre et al., Spain [35] | Observational, prospective | Following a MedDiet with EVOO and pistachio supplementation before 12 gestational weeks showed a lower GDM incidence and better maternal–fetal outcomes | 932 women | The incidence of GDM was lower in the intervention group than in the controls (RR 0.81) | MedDiet |
| Izadi et al., Iran [39] | Observational, case-control | Adherence to the DASH and MedDiet was associated with a reduced risk for GDM | 200 women with GDM and 260 without GDM | A higher adherence to DASH was related to 71% reduced risk for GDM | DASH and MedDiet |
| Jali et al., India [40] | Observational, cross-sectional | Non-vegetarian pregnant women showed an increased risk for glucose intolerance | 325 women: 202 vegetarian and 123 non-vegetarian | 52 women (16%) presented GDM. An increased prevalence of GDM in patients following a non-vegetarian diet compared to a vegetarian diet (65.5% vs. 38.5%) | Vegetarian diet |
| Kahleova et al., Czech Republic [33] | RCT | A low calorie vegetarian diet improved insulin sensitivity | 37 following a vegetarian diet and 37 following a conventional diabetic diet | A vegetarian diet improved adipokine levels and oxidative stress markers compared to a conventional diabetic diet over 24 weeks | Vegetarian diet |
| Karamanos et al., Mediterranean countries [36] | Observational, prospective | Adhering to a MedDiet pattern decreased the incidence of GDM | 1076 women | The incidence of GDM was lower in subjects with better adherence to the MedDiet (8.0% vs. 12.3%) | MedDiet |
| Kesary et al., Israel [19] | Observational, retrospective | A vegan diet is a protective factor from maternal weight gain but increased the risk for a lower birth weight | 234 vegans, 133 vegetarian, and 1052 omnivores | A vegan diet in pregnancy was associated with a lower birth weight centile compared to omnivores (42.6 ± 25.9 vs. 52.5 ± 27.0; p < 0.001) | Vegan and vegetarian diet |
| Mak et al., China [38] | Observational, prospective | Following an early pregnancy dietary pattern did not significantly increase the risk of GDM in patients. However, a high protein–low starch diet was associated with a decrease in risk for GDM among obese women | 1337 women | 199 women (14.9%) developed GDM | Plant-based and a high protein–low starch pattern diet |
| Olmedo-Requena et al., Spain [37] | Observational, case-control | A high adherence to a MedDiet before pregnancy was strongly associated with a decreased risk in GDM | 291 with GDM and 1175 without GDM | A high MedDiet adherence was associated with lower GDM risk (aOR 0.61; p = 0.028), while a very high MedDiet adherence was more strongly associated (aOR 0.33; p = 0.005) | MedDiet |
| Zhang et al., USA [45] | Observational, prospective | A low fiber and high sugar intake diet increased the risk for GDM | 13,100 women | 758 with GDM. Each 10-g/day increment in total fiber intake was associated with a 26% reduction in GDM risk | Diet rich in fiber |
| Zulyniak et al., Canada [34] | Observational, prospective | A plant-based diet was associated with lowering the birth weight for women of Caucasian ethnicity and increasing it in Asiatic women living in Canada | 3997 women | The plant-based diet was inversely associated with birth weight (β = −67.6 g per 1-unit increase; p < 0.001) | Plant-based diet |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schiattarella, A.; Lombardo, M.; Morlando, M.; Rizzo, G. The Impact of a Plant-Based Diet on Gestational Diabetes: A Review. Antioxidants 2021, 10, 557. https://doi.org/10.3390/antiox10040557
Schiattarella A, Lombardo M, Morlando M, Rizzo G. The Impact of a Plant-Based Diet on Gestational Diabetes: A Review. Antioxidants. 2021; 10(4):557. https://doi.org/10.3390/antiox10040557
Chicago/Turabian StyleSchiattarella, Antonio, Mauro Lombardo, Maddalena Morlando, and Gianluca Rizzo. 2021. "The Impact of a Plant-Based Diet on Gestational Diabetes: A Review" Antioxidants 10, no. 4: 557. https://doi.org/10.3390/antiox10040557
APA StyleSchiattarella, A., Lombardo, M., Morlando, M., & Rizzo, G. (2021). The Impact of a Plant-Based Diet on Gestational Diabetes: A Review. Antioxidants, 10(4), 557. https://doi.org/10.3390/antiox10040557









