Abstract
Neurodegenerative diseases are a heterogeneous group of disorders that are characterized by the gradual loss of neurons. The development of effective neuroprotective agents to prevent and control neurodegenerative diseases is specifically important. Recently, there has been an increasing interest in selecting flavonoid compounds as potential neuroprotective agents, owing to their high effectiveness with low side effects. Baicalin is one of the important flavonoid compounds, which is mainly isolated from the root of Scutellaria baicalensis Georgi (an important Chinese medicinal herb). In recent years, a number of studies have shown that baicalin has a potent neuroprotective effect in various in vitro and in vivo models of neuronal injury. In particular, baicalin effectively prevents neurodegenerative diseases through various pharmacological mechanisms, including antioxidative stress, anti-excitotoxicity, anti-apoptotic, anti-inflammatory, stimulating neurogenesis, promoting the expression of neuronal protective factors, etc. This review mainly focuses on the neuroprotective and cognitive enhancement effects of baicalin. The aim of the present review is to compile all information in relation to the neuroprotective and cognitive enhancement effects of baicalin and its molecular mechanisms of action in various in vitro and in vivo experimental models.
1. Introduction
Scutellaria baicalensis Georgi (Lamiaceae or Labiatae) is an important Chinese traditional medicinal plant, and commonly known as Huang-Qin or Chinese skullcap (Radix scutellariae). Traditionally, the root part of this plant has been used for the treatment of various ailments, including diarrhea, hepatitis, atherosclerosis, dysentery, diabetes, hypertension, complication of menstruation, eye diseases, vomiting, hemorrhaging, insomnia, common cold, inflammation, and respiratory infections [1]. Further, several scientific studies have reported that extracts and isolated compounds from S. baicalensis have various pharmacological properties, such as antitumor, hepatoprotective, antimicrobial, anti-inflammatory, neuroprotective, anti-hyperlipidemic, antidiabetic, antimutagenesis, anticonvulsant, and antioxidant. So far, more than 50 flavonoid components have been isolated and identified from S. baicalensis. Among them, baicalin and its aglycone baicalein are the major bioactive compounds [2,3].
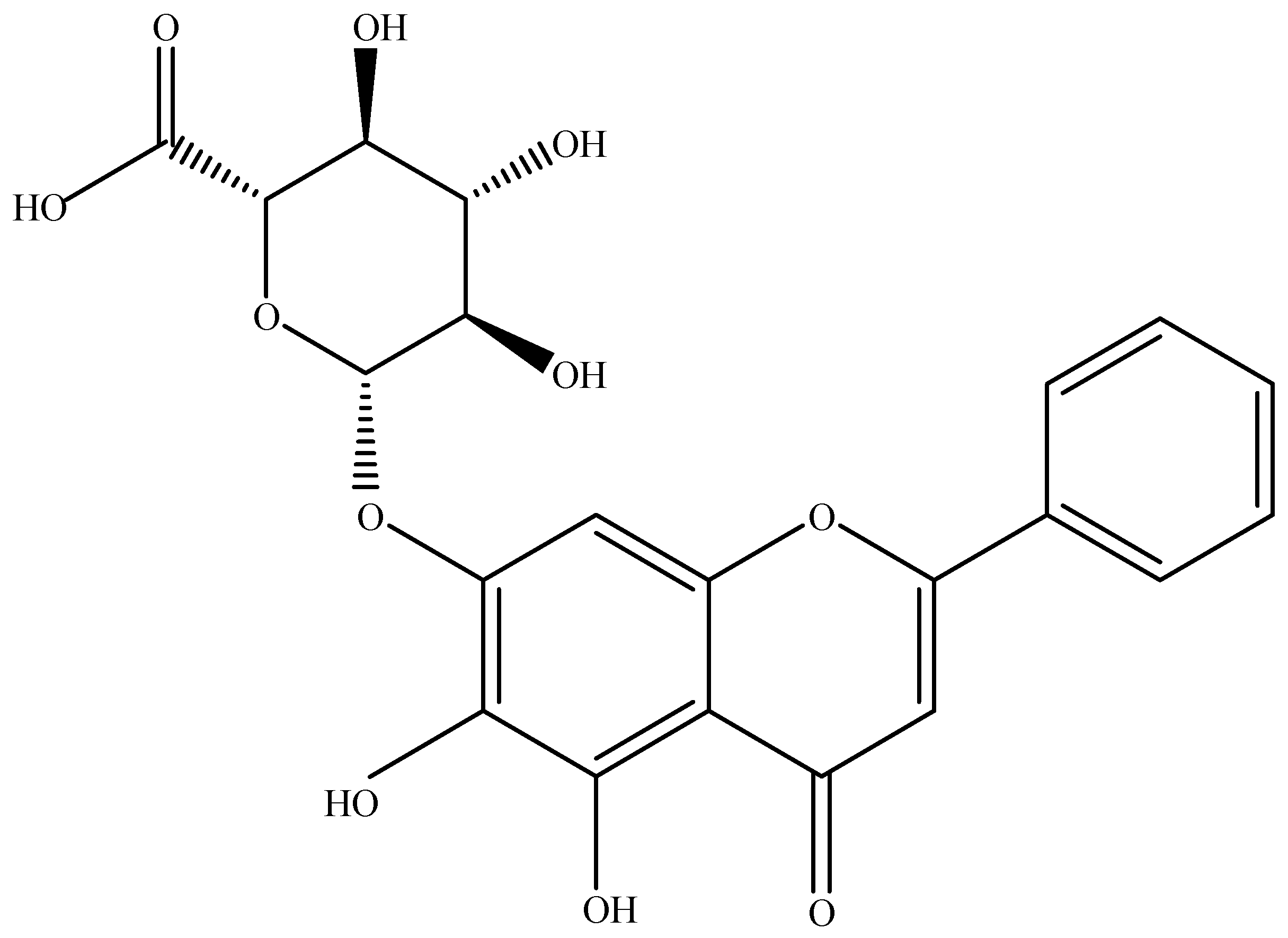
Baicalin (C21H18O11; 5,6,7-trihydroxyflavone 7-O-beta-d-glucuronide or baicalein 7-O-β-d-glucuronic acid or 7-d-glucuronic acid-5,6-dihydroxyflavone) (Figure 1) is one of the most important flavonoid components in the roots of Scutellaria baicalensis Georgi. The concentration of baicalin in the roots of S. baicalensis ranged from 8.1% to 15.6% [4,5,6,7]. The root of this plant has been traditionally used for the treatment of numerous diseases in East Asia. Synonyms of S. baicalensis are S. grandiflora Adams, S. lanceolaria Miq., and S. macrantha. Baicalin is also the major constituent in other Scutellaria species, namely S. lateriflora, S. galericulata, and S. rivularia, as well as in Oroxylum indicum (Bignoniaceae). Different species of Scutellaria are mainly distributed in Asian countries, such as China, Russia, Mongolia, Japan, and Korea [8].
Figure 1.
The chemical structure of baicalin.
Baicalin has been extensively used in pharmaceutical and food industries due to its outstanding bioactivities. A number of in vitro and in vivo studies have demonstrated that baicalin possesses various pharmacological properties, including anti-inflammatory, anticancer, antidiabetic, antithrombotic, cardioprotective, hepatoprotective, and neuroprotective properties [8,9]. In particular, baicalin exhibits a variety of beneficial effects in the central nervous system (CNS) by promoting neural differentiation and inhibiting neuronal apoptosis [10]. Further, baicalin also shows antidepressant- and anxiolytic-like properties and improving cognitive performances [6]. Previous studies have demonstrated that baicalin showed protective effect against amyloid-β (Aβ), hydrogen peroxide (H2O2), oxygen/glucose deprivation (OGD), middle cerebral artery occlusion (MCAO), ketamine, and thrombin-induced neurotoxicity in cell lines and animal models [11,12,13,14,15,16].
The brain and nervous system-related diseases affect over two billion people worldwide and many of the most harmful brain diseases are neurodegenerative. Chronic neurodegenerative diseases, including Alzheimer’s (AD), Parkinson’s (PD), and Huntington’s diseases represent a large unmet medical need in the world. These diseases refer to those conditions in which neuronal cells undergo progressive degeneration and eventual death associated with aging [17]. Accumulating evidence suggests that excitotoxicity, oxidative stress, mitochondrial dysfunction, inflammatory response, protein misfolding, and neuronal apoptosis have been associated with neurodegeneration [9,18]. The most common symptoms of neurodegenerative diseases are anxiety, apathy, depression, motor dysfunction, and memory impairment [19]. Numerous studies have shown that baicalin efficiently prevents various neurodegenerative diseases, such as AD, PD, and cerebral ischemia, by suppressing oxidative stress, inhibiting excitotoxicity, and promoting neurogenesis, reducing apoptosis, and inhibiting the production of inflammatory cytokines [9,20,21].
Previously, some authors clearly reviewed therapeutic potentials of baicalin against cancer, cerebral ischemia, tumor, cardiovascular, ocular, and inflammatory disorders [5,8,9,22,23,24,25]. However, the low aqueous solubility and poor oral bioavailability of baicalin are the major limitations in the clinical application. Baicalin showed limited permeability, probably owing to its comparatively high hydrophilicity and larger molecular weight. In addition, baicalin was found to be moderately absorbed in the stomach and poorly in the small intestine and colon [26]. Moreover, previous studies clearly demonstrated that baicalin can be detected in the blood of animals immediately after oral or intravenous administration of baicalein [27,28]. In regard to drug–drug interaction, baicalin may influence the metabolism of several CYP2E1 isozyme dependent drugs [29]. Previous study reported that following treatment with aminoglycoside, the absolute bioavailability of baicalin was decreased by nearly 40–45% when compared with untreated rats. Some studies exhibited that baicalin could interact with transporter-related drugs (rosuvastatin, and 7-ethyl-10-hydroxycamptothecin) and other drugs such as cyclosporine A, quinidine, and SKF-525A [9].
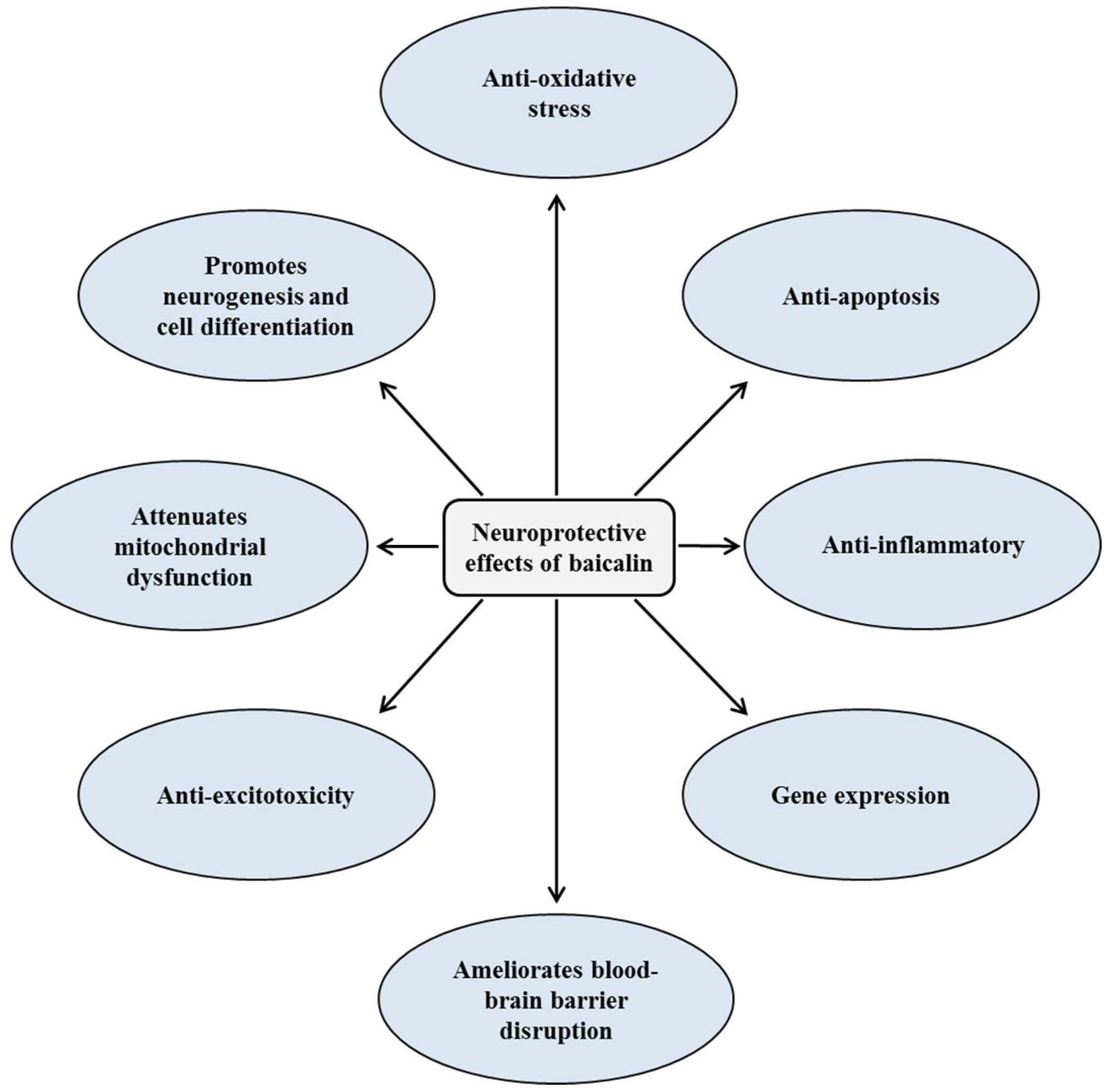
There has been no specific review of published articles in relation to neuroprotective and cognitive enhancement effects of baicalin. Herein, we reviewed the protective effects of baicalin on various neurodegenerative disorders. Current knowledge about neuroprotective and cognitive enhancement properties of baicalin and its molecular mechanisms are presented in Table 1 and Table 2. Figure 2 illustrates the role of different signaling pathways in protecting neuronal damage.

Table 1.
Neuroprotective effects of baicalin under in vitro and ex vivo models.

Table 2.
Neuroprotective effects of baicalin under in vivo models.
Figure 2.
Mechanisms of neuroprotective and cognitive enhancement effects of baicalin.
2. Neuroprotective Effects of Baicalin
2.1. Alzheimer’s Disease Model
2.1.1. In Vitro
The aggregation of Aβ peptides is an important factor in the etiopathogenesis of AD. Increasing evidence demonstrated that metal ions play a major role in the aggregation of Aβ. Hence, inhibition of Aβ aggregation appears as a potential strategy to treat AD. A study reported that baicalin can interact with copper directly and suppress Aβ1-42 aggregation. Further, baicalin showed a protective effect against Aβ1-42-induced oxidative injuries in SH-SY5Y cells by inhibiting the production of H2O2 [35]. Xiong et al. [19] determined whether baicalin regulates microglial activation or inhibits inflammatory cytokine production in Aβ42-induced BV2 cells. The results revealed that baicalin inhibited Aβ42-induced BV2 microglial cell proliferation, reduced cluster of differentiation molecule 11b (CD11b) expression, decreased the chemotactic ability of BV2 cells. In addition, baicalin effectively inhibited the production of interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and nitric oxide (NO). Furthermore, baicalin pretreatment could significantly downregulate Aβ-induced phosphorylation of Janus kinase 2 (JAK2), and signal transducer and activator of transcription 3 (STAT3).
2.1.2. In Vivo
A study was conducted to investigate therapeutic effects of a mixture of Chinese herb active components (baicalin, jasminoidin, and cholic acid) against ibotenic acid-induced rats. Pretreatment with the chemical mixture markedly attenuated abnormalities in cognition, brain functional images, and histological morphology in ibotenic acid-induced rats. The chemical mixture significantly influenced on the expression levels of 19 genes in the forebrain. In these, about 60% of genes were associated with neuroprotection and neurogenesis, and the remaining genes were linked with antioxidation, degradation of proteins, cholesterol metabolism, stress response, and apoptosis. In addition, the treatment increased the expression of these genes with the exception of the apoptosis-related gene [74]. Chen et al. [78] examined the neuroprotective effects of baicalin on pathological changes and behavioral impairments in Aβ1-42-induced AD mouse model. Baicalin could ameliorate memory impairment in the Morris water maze and probe tests. Further, baicalin treatment attenuated glial cell activation and decreased the expression of TNF-α and IL-6 in Aβ1-42-induced AD mice.
In Aβ-induced AD transgenic mice, baicalin significantly regulated the JAK2/STAT3 signaling pathway [14]. In an Aβ toxicity rat model of AD, baicalin treatment improved learning and memory deficits in Morris water maze test, and attenuated the hippocampus injury. Baicalin treatment significantly increased the level of antioxidant enzymes and their gene expressions, such as superoxide dismutase (SOD), catalase, and glutathione peroxidase (GSH-Px). In addition, baicalin increased mitochondrial membrane potential and reduced Bax/B cell lymphoma 2 family (Bcl-2) ratio, cytochrome c release, and caspase-9/-3 activation in Aβ-induced rats. Further, the antioxidative effect of baicalin may associate with the activation of nuclear factor erythroid 2-related factor 2 (Nrf2) signaling pathway [79]. Bitto et al. [85] investigated the neuroprotective effect of flavocoxid (a mixture of purified baicalin and catechin) in triple-transgenic (3xTg-AD) mice. Flavocoxid is a dual inhibitor of cyclooxygenases-1/2 (COX-1/2) and 5-lipoxygenase (5-LOX). Flavocoxid treatment improved learning and memory function, and decreased the production of eicosanoid. In addition, flavocoxid downregulated the activation of nucleotide-binding domain and leucine-rich repeat protein-3 (NLRP3) inflammasome and IL-1β production. Furthermore, flavocoxid reduced the phosphorylation level of the amyloid precursor protein (APP-p-Thr668), p-tau (p-Thr181) and extracellular signal-regulated kinases 1 and 2 (p-ERK1/2). A recent study demonstrated that baicalin increased the percentages of astrocytes and neuronal in Aβ1-40-induced rats. Moreover, baicalin treatment enhanced expressions of Nestin and nucleotide sugar epimerase [91].
2.2. Parkinson’s Disease Model
In Vivo
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) is a potent and selective nigrostriatal dopaminergic neurotoxin that produces many of the neuropathological characteristics of idiopathic PD. In MPTP-induced mice, baicalin treatment effectively prevented the loss of tyrosine hydroxylase (TH)-positive neurons in substantia nigra, and increased the dopamine content of striatum. In addition, baicalin significantly increased glutathione content (GSH) in the brain [57]. Previous studies reported that iron accumulates in the substantia nigra of patients with PD. Xiong et al. [69] found that baicalin treatment markedly inhibited iron accumulation in different brain regions, and showed a protective effect on dopaminergic neurons in rotenone-induced rats.
2.3. Ischemia
2.3.1. In Vitro
Ischemic stroke is the third most common cause of death worldwide in adults. According to the World Health Organization, 5–6 million individuals die from stroke each year [9]. OGD is a widely used in vitro model to study ischemic stroke. Liu et al. [30] investigated the effect of baicalin on ischemic-like or excitotoxic injury, and protein kinase C alpha (PKC(α)) activation in rat hippocampal slices. In OGD- and N-methyl-d-aspartate (NMDA)-induced rat hippocampal slices, baicalin ameliorated viability reduction and inhibited the increased membrane portion of PKC(α). It was reported that the activation of 5-LOX is involved in ischemic neuronal damage. Baicalin showed the protective effect against OGD-induced ischemic-like injury in rat cortical neurons by partly inhibiting NMDA receptor-mediated 5-LOX activation [31]. Jung et al. [32] found that baicalin attenuated the negative insult of light, hydrogen peroxide, and serum withdrawal to RGC-5 cells.
Nucleotide-binding oligomerization domain protein 2 (NOD2) receptor plays a key role in innate immunity, and is genetically associated with various inflammatory reactions. In this context, the effect of baicalin on NOD2/TNFα in OGD-induced BV2 cells, PC12 cells, and primary neuron cells was investigated. The results indicated that baicalin treatment could effectively suppress the expression of NOD2 and TNFα in mRNA as well as protein levels [34]. In OGD-induced microglial cells, baicalin markedly inhibited the release of TNF-α, IL-1β, IL-6, and IL-8, and reduced Toll-like receptor 4 (TLR4) mRNA expression and tumor necrosis factor receptor-associated factor 6 (TRAF6) levels. Additionally, baicalin downregulated nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor-alpha (IκB-α), c-jun, ERK1/2, c-Jun N-terminal kinase (JNK), and p38 phosphorylation, and inhibited the transfer of myeloid differentiation primary response 88 (MyD88) from cytoplasm to membrane in OGD-induced microglial cells [36].
In another study, baicalin effectively protected neurons against H2O2-induced injury and improved the SOD activity [38]. Baicalin also showed the neuroprotective effect against extraneous and endogenous peroxynitrite-induced toxicity in SH-SY5Y cells [40]. Zhang et al. [41] examined the protective effect of baicalin on OGD-induced brain microvascular endothelial cells through anti-inflammation. The results showed that baicalin increased cell viability, and decreased lactate dehydrogenase (LDH) leakage rate, TNF-α, IL-1β, and IL-6 levels in the culture media. In addition, baicalin markedly downregulated the phosphorylation of proteins in mitogen-activated protein kinase (MAPK) signaling pathways, such as p-MRK1/2, p-ERK, and p-p38. Further, baicalin significantly downregulated the phosphorylation of proteins in nuclear factor kappa B (NF-кB) signaling pathway, such as phosphorylated-IκB kinase α and β (p-IKKα and p-IKKβ), and p-IκBα. Moreover, baicalin remarkably inhibited nuclear transcriptional activity triggered by NF-κB p65 and p-IκBα in brain microvascular endothelial cells. On the basis of these findings, authors suggested that baicalin exhibited its neuroprotective effect by downregulating the MAPK and NF-κB signaling pathway.
In H2O2-induced rat primary cortical neurons, baicalin effectively inhibited neuronal apoptosis by enhancing transcription and expression of myeloid cell leukemia-1 (MCL-1) and BCL-2. Additionally, baicalin remarkably increased myocardin-related transcription factor-A (MRTF-A) level. However, the anti-apoptosis effect of baicalin was significantly abrogated by the transfection of small interfering RNA of MRTF-A (MRTF-A siRNA) in primary cortical neuron cultures. Baicalin also increased the transactivity of MCL-1 and BCL-2 promoter by activating the key CarG box (CC [A/T] 6GG) element. Moreover, baicalin-induced MRTF-A expression and transactivity and expression of MCL-1 and BCL-2 were reduced by phosphatidylinositol-3 kinase (PI3K) inhibitor, LY294002, and ERK1/2 inhibitor, PD98059 [21]. Another study indicated that baicalin showed neuroprotective effects against hypoxia and OGD/reoxygenation (RO)-induced injury in SH-SY5Y cells. Baicalin significantly attenuated OGD/RO-induced apoptotic cell death in SH-SY5Y cells, and decreased caspase-3 expression. In addition, baicalin markedly downregulated NF-κB and N-methyl-d-aspartic acid receptor-1 (NMDAR1) in OGD/RO-induced cells [45].
A recent study reported that baicalin treatment suppressed dynamin-related protein 1 (Drp-1) expression, reduced mitochondrial fission, elevated mitofusin-2 (MFN2) generation, upregulated Drp-1 Ser637 phosphorylation, and increased mitochondrial membrane potential in OGD/reperfusion-induced PC12 cells via the inhibition of reactive oxygen species (ROS) production. In addition, baicalin attenuated cell apoptosis and increased mitophagy [13]. Luo et al. [48] evaluated the protective effect of baicalin against OGD-induced ischemic injury in endothelial cells. The authors found that baicalin effectively inhibited cell death, decreased cell membrane damage, and maintained the integrity of the nucleus. Baicalin treatment also decreased necroptosis ratio and regulated the expression of RIP-1 and RIP-3 in bEnd.3 cells. Furthermore, baicalin inhibited the production of ROS and malondialdehyde (MDA), and increased SOD activity in OGD-induced bEnd.3 cells.
2.3.2. In Vivo
A number of researchers have used middle cerebral artery occlusion (permanent or transient) to study focal cerebral ischemia in mice or rats. A study indicated that that baicalin treatment reduced MCAO-induced neuronal damage, brain edema, and blood–brain barrier (BBB) permeability by inhibiting the expression of matrix metallopeptidase 9 (MMP-9) and MMP-9-mediated occludin degradation [63]. Baicalin also showed a protective effect against MCAO-induced cerebral ischemia in rat by reducing the expression of TLR2/4, NF-κB, inducible nitric oxide synthase (iNOS), and COX-2. In addition, baicalin administration decreased the serum content of TNF-α and IL-1β [64]. In another study, baicalin markedly reduced the enzymatic activity of myeloperoxidase (MPO) and downregulated the expression of iNOS and COX-2 mRNAs, and cleaved caspase-3 protein in MCAO-induced rats [59]. In addition, baicalin downregulated the expression of NOD2 and TNFα proteins in bilateral common carotid artery ligation (BCCL)-induced mice [34]. Xue et al. [61] found that baicalin treatment decreased the level of NF-κB p65 in MCAO-induced focal cerebral ischemia in rats. In gerbils with transient global cerebral ischemic/reperfusion injury, the administration of baicalin significantly attenuated ischemia-induced neuronal cell damage in gerbils. In addition, baicalin reduced the level of MDA, and increased SOD, GSH, and GSH-Px activities. Moreover, baicalin markedly upregulated the expression of BDNF and suppressed the expression of caspase-3 at mRNA and protein levels [62].
Zhang et al. [55] compared the individual and combined effects of baicalin with jasminoidin on cerebral ischemia/reperfusion injury in rats. When compared with individual treatment, the combined treatment significantly ameliorated the results of 2,3,5-triphenyltetrazolium chloride (TTC) and histological examination. In addition, this combination ameliorated diffusion weighted imaging (DWI) of magnetic resonance imaging (MRI) and promoted brain-derived neurotrophic factor (BDNF) expression and inhibited caspase-3 expression. The capillary electrophoresis-laser-induced fluorescence detection technique was used to investigate the effect of baicalin on changes of amino acid neurotransmitters level during cerebral ischemia in rats. In the results, concentrations of Glu, Asp, gamma-aminobutyric acid (GABA), and Gly in the brain cortex were elevated due to cerebral ischemia. However, baicalin treatment could attenuate the elevations of Glu and Asp in the cerebral cortex [51]. A study also attempted to investigate and determine the effect of baicalin on different protein expression modes in MCAO-induced mice brains. However, there was no significant difference in the expression of twenty-four proteins between baicalin-treated MCAO group and the sham-operation group [60].
In ischemia/reperfusion to the rat retina, baicalin treatment regulated the localization of Thy-1 and choline acetyltransferase (ChAT) level, and the level of various proteins and mRNAs in the retina. However, baicalin treatment did not affect the level of caspase-8 and caspase-3 mRNAs caused by ischemia/reperfusion [32]. Chang et al. [56] examined the prophylactic effect of baicalin in an animal model of heatstroke. Baicalin administration effectively attenuated the hyperthermia, intracranial hypertension, and increased NO2−, glutamate, glycerol, lactate/pyruvate ratio, and dihydroxybenzoic acid levels in the hypothalamus of heatstroke-induced rats. Further, baicalin markedly decreased the levels of IL-1β and TNF-α in the serum, as well as the hypothalamus.
In intracerebral hemorrhage (ICH)-induced rats, baicalin significantly attenuated brain edema, inhibited cell apoptosis, and suppressed the expression of brain protease-activated receptor-1 (PAR-1) at both the mRNA and protein levels [70]. Baicalin could also improve neurological function and decrease brain infarction in MCAO-induced rats. Further, baicalin reduced cell apoptosis and the production of ROS and MDA. Moreover, baicalin interfered with SOD and nicotinamide adenine dinucleotide 2′-phosphate oxidase (NOX) activities [38]. Dai et al. [71] investigated the effect of baicalin on global ischemia-induced gerbils, and found that baicalin treatment effectively facilitated neurological function and attenuated the ischemia-induced neuronal damage. Additionally, baicalin administration increased the expression of GABAA receptor (GABA(A)R) α1, GABA(A)R γ2, and K–Cl co-transporter 2 (KCC2), and decreased the expression of Na–K–Cl cotransporter 1 (NKCC1) in the hippocampus of gerbils following an ischemic insult. Moreover, baicalin treatment markedly increased the protein expressions of HSP70 and phosphorylated ERK (p-ERK), and decreased the expression of phosphorylated JNK (p-JNK) and phosphorylated p38 (p-p38) in ischemic gerbils. Baicalin also inhibited 3-nitrotyrosine formation, decreased infarct size, and attenuated apoptotic cell death in ischemia/reperfusion-induced injury in rat brain [40].
A study reported that baicalin treatment increased the number of newly generated cells in the hippocampus of rats exposed to transient cerebral ischemia. Additionally, baicalin improved cognitive impairment as measured in the Morris water maze test [42]. In a rat model of collagenase VII-induced ICH, baicalin administration reduced brain edema, inhibited NF-κB activation, and suppressed MMP-9 expression. In addition, baicalin reduced the production of IL-1β and IL-6, as well as BBB permeability [77]. Baicalin effectively inhibited neuronal apoptosis by enhancing the transcription and expression of MCL-1 and BCL-2 in MCAO-induced rats. In addition, baicalin administration increased MRTF-A level in ischemic hemisphere [21]. Baicalin also improved learning and memory dysfunction in global cerebral ischemia/reperfusion-induced gerbils by downregulating the phosphorylation level of Ca2+/calmodulin-dependent protein kinase II (CaMKII) and preventing hippocampal neuronal apoptosis [46]. In a recent study, baicalin administration significantly decreased the mortality rates, and ameliorated BBB disruption and hemorrhagic transformation. In addition, baicalin markedly scavenged peroxynitrite and inhibited MMP-9 expression and activity in MCAO-induced ischemic brains with delayed tissue plasminogen activator treatment [86]. The effect of baicalin on hyperglycemia-exacerbated cerebral ischemia/reperfusion injury in rats was investigated by Li et al. [13]. In their study, baicalin treatment decreased blood glucose, alleviated neurological deficit and reduced infarct volume.
Inflammatory responses and blood–brain barrier disruption play a critical role in the formation of edema during subarachnoid hemorrhagic brain injury. The protective effect of baicalin against filament perforation-induced subarachnoid hemorrhagic brain injury in mice was investigated by Shi et al. [88]. Baicalin administration effectively increased neurological score and brain water content. Baicalin also restored levels of tight junction proteins, such as survivin, claudin-5, zonula occludens-1 (ZO-1), and collagen IV. In addition, baicalin treatment inhibited the production of IL-1β, IL-6, and chemokine (C–X–C motif) ligand 3 (CXCL-3) in subarachnoid hemorrhage mice. Furthermore, baicalin downregulated the mRNA and protein levels of NOS-2 and NOX-2 in subarachnoid hemorrhage mice. Recently, the neuroprotective effect of baicalin in a rat model of hypoxic-ischemic encephalopathy was investigated. In the results, baicalin markedly reduced apoptosis and increased the expression of phosphorylated protein kinase B (p-Akt) and glutamate transporter 1. Further, the PI3K/Akt inhibitor, LY294002 blocked the effect of baicalin on p-Akt and glutamate transporter 1 [89].
2.4. Neuroprotective and Cognitive Enhancement Effects
2.4.1. In Vitro
Ketamine is extensively used as an anesthetic in pediatric clinical practice. However, a number of studies have demonstrated that exposure to ketamine during the developmental period induces neuronal toxicity. In vitro experiments showed that baicalin attenuated ketamine-induced cell viability decrease, morphological change, and caspase-3 expression activation in the primary neuron–glia mixed cultures. Further, the results demonstrated that baicalin showed the neuroprotective effect against ketamine-induced toxicity by activating PI3K/Akt and its downstream cAMP response element-binding protein (CREB)/BDNF/Bcl-2 signaling pathways [16]. Baicalin also suppressed co-listin sulfate-induced neuronal apoptosis in PC12 cells by inhibiting free radical injury, and downregulating caspase-3 and lactate dehydrogenase activities [39]. Additionally, baicalin showed a potent neuroprotective effect against H2O2-induced toxicity in PC12 cells. Baicalin pretreatment of PC12 cells reduced the viability loss and apoptotic rate in H2O2-induced PC12 cells. In addition, baicalin increased SOD, GSH-Px activities and decreased the level of MDA. Moreover, baicalin upregulated the expression of survivin, Bcl-2, and p-STAT3, and downregulated the expression of caspase-3 expression [15]. In thrombin-induced injury in SH-SY5Y cells, baicalin reduced cell death by inhibiting NF-κB activation and suppressing the expression of PAR-1 and caspase-3 [12].
Prolyl oligopeptidase (POP) is a cytosolic serine peptidase that has been related to schizophrenia, bipolar affective disorder, and associated neuropsychiatric disorders. An in vitro study demonstrated that baicalin inhibited the generation of prolyl oligopeptidase in a dose-dependent manner [33]. STAT3 and basic helix–loop–helix (bHLH) gene family are main cellular signaling molecules to regulate cell fate decision and neuronal differentiation of neural stem/progenitor cells (NSPCs). In this context, Li et al. [37] examined the effects of baicalin on stat3 phosphorylation, the expression of bHLH family proteins, and neuronal differentiation of NSPCs. In their study, baicalin treatment promoted the number of microtubule-associated protein (MAP-2) positive-staining cells, and reduced glial fibrillary acidic protein (GFAP)-staining cells. Additionally, baicalin suppressed the expression of p-stat3 and Hes1, and upregulated the expression of NeuroD1 and Mash1.
In another study, Morita et al. [44] determined whether baicalin promotes neuronal differentiation in human iPS cells, and the expression of bHLH gene during neuronal differentiation. The results demonstrated that baicalin can influence the neuronal fate decision in human iPS cells by promoting neuronal differentiation and inhibiting glial differentiation. In addition, baicalin treatment decreased the level of Hes1 protein and upregulated the expression of Ascl1 gene. The proliferation and migration of Schwann cells (SCs) are important events in the process of peripheral nerve repair. A recent study indicated that baicalin could promote the viability of RSC96 SCs and exhibit the greatest gene expression of neurotrophic factors, such as glial cell-derived neurotrophic factor (GDNF), BDNF, and ciliary neurotrophic factor (CNTF). These neurotrophic factors are considered essential factors in the process of never cell regeneration [49].
2.4.2. In Vivo
In rats with spinal cord injury (SCI), BC treatment remarkably decreased the water content of spinal cord tissue, the permeability of blood–spinal cord barrier, and oxidant stress. Further, baicalin decreased the expression of TNF-α, NF-κB, Bax, Bcl-2, and caspase-3 [20]. Baicalin exhibited a strong neuroprotective activity against ketamine-induced apoptotic neurotoxicity in rat pups. Baicalin treatment increased the expression of p-Akt, phosphorylated-glycogen synthase kinase-3 beta (p-GSK-3β), p-CREB, and BDNF in ketamine-induced rats. In addition, baicalin increased the expression of bcl-2/Bax and decreased the expression of caspase-3 in ketamine-induced rats [16]. The administration of baicalin also enhanced memory impairment as measured in the passive avoidance Morris water maze tests in corticosterone-induced rats. Additionally, the administration of baicalin effectively alleviated memory-related decreases in the expression levels of BDNF and CREB in the hippocampus [75]. Ma et al. [81] found that baicalin exhibited a strong protective activity against streptozotocin-induced diabetes-associated cognitive deficits in rats. The results revealed that baicalin treatment improved memory performances and increased the neuronal survival in streptozotocin-induced rats. Baicalin treatment also increased ChAT, p-ERK, BDNF, and Bcl-2. Furthermore, baicalin decreased the levels of hippocampal acetylcholinesterase (AchE), p-JNK, p-p38, caspase-3, Bax, and plasma glucose.
2.5. Epilepsy: In Vivo
Oxidative stress can markedly alter neuronal function, and has been associated with status epilepticus. Liu et al. [67] investigated whether baicalin could exhibit anticonvulsant and neuroprotective effects in pilocarpine-induced epileptic rats. Baicalin treatment remarkably postponed the onset of the first limbic seizures and status epilepticus, reduced the mortality rate, and decreased the changes in the levels of lipid peroxidation, and nitrite and reduced glutathione contents in the hippocampus. Moreover, baicalin attenuated the neuronal cell damage, apoptosis, and degeneration in pilocarpine-induced seizures in the hippocampus of rats. In kainic acid-induced epileptic mice, baicalin administration effectively attenuated neuronal injury and apoptosis in the hippocampus. Further, baicalin decreased the expression of miR-497 and cleaved caspase-3 protein, and upregulated the expression of Bcl-2 protein [83].
2.6. Antidepressant Effect: In Vivo
In depressive disorders, the regulation of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor expression plays a key role in the viability of neurons and the level of BDNF in the brain. In chronic unpredictable mild stress (CMS)-induced rats, baicalin administration significantly increased AMPA receptor expression and decreased neuron apoptosis [76]. A study was also carried out to investigate the effect of baicalin on CMS-treated rats. The results demonstrated that baicalin effectively reversed the changes in depressive-like behaviors, such as decreased sucrose intake and locomotor activity, and increased immobility time. In addition, baicalin treatment significantly decreased the activation of NLRP3 inflammasome and the levels of IL-1β and IL-6 in rat prefrontal cortex [10]. Baicalin treatment also increased the sucrose preference, decreased serum corticosterone levels, downregulated the activity and expression of COX-2 mRNA, and decreased the level of prostaglandin E2 (PGE2) in CMS-induced rats [73].
In corticosterone-induced mice, baicalin treatment relieved depressive-like behaviors, including the increased sucrose preference and decreased the duration of immobility. In addition, baicalin restored the level of serum corticosterone, upregulated the expression of glucocorticoid receptor and BDNF, as well as downregulated serum- and glucocorticoid-regulated kinase 1 (SGK1) in the hippocampus. Furthermore, baicalin markedly increased the expression of 11β-hydroxysteroid dehydrogenase-2 (11β-HSD2) protein in the hippocampus [80]. A recent study also demonstrated that baicalin inhibited adaptor protein, phosphotyrosine, interacting with PH domain and leucine zipper 2 (APPL2)-mediated glucocorticoid receptor (GR) hyperactivity, promoted adult neurogenesis, released depressive and anxiety symptoms, and enhanced olfactory functions in chronic corticosterone-induced mice [90]. In a rat model of olfactory bulbectomy-induced depression, Yu et al. [84] found that baicalin effectively increased the performance in depression-like behavioral tests, and decreased oxidative stress, synaptophysin expression, and hippocampal apoptosis. Further, baicalin regulated the levels or activity of MDA, SOD, and GSH-Px. Moreover, baicalin treatment prevented apoptotic PAR-1 expression and suppressed caspase-mediated apoptosis signaling cascades in olfactory bulbectomy-induced rats. In another study, baicalin improved antidepressant-like behaviors in mice and rats. Additionally, oral administration of baicalin effectively inhibited monoamine oxidase A and B activity in rats. Furthermore, baicalin showed a significant recovery in sucrose intake in CMS-induced rats [92]. Zhang et al. [93] found that baicalin treatment improved anxiety/depression-like behaviors and promotes hippocampal neurogenesis in chronic corticosterone-induced mice. Further, baicalin may normalize GR function through serum- and glucocorticoid-inducible kinase 1- and FK506-binding protein 51-mediated GR phosphorylation.
2.7. Anxiolytic-Like Effect: In Vivo
Liao et al. [51] found that the anxiolytic-like effect of baicalin may be mediated through the activation of benzodiazepine binding site of GABA(A) receptors. The anxiolytic effects of baicalin alone, and in combination with other anxiolytics in mice, were investigated by Xu et al. [54]. Baicalin treatment showed significant anxiolytic-like effects as measured in the elevated plus-maze test. Co-administration of baicalin with DL-tetrahydropalmatine also exhibited a considerable anxiolytic-like effect. In mice with picrotoxin-induced seizure, Wang et al. [58] suggested that baicalin administration showed anxiolytic-like effects through the alpha2- and alpha3-containing GABA(A) subtypes.
2.8. Blood–Brain Barrier Penetrating Ability
The BBB is a highly selective semipermeable membrane barrier, plays an important role in maintaining homeostasis of the CNS. It protects the brain by blocking the passage of medications into the brain. Hence, BBB-penetrating ability is a prerequisite for medications used for the treatment of various brain disorders [45]. Zhang et al. [94] investigated the effect of baicalin on the transport of nimodipine (a dihydropyridine calcium channel blocker) across the BBB. In their study, baicalin (at 2–5 μg/mL) increased the uptake of nimodipine, whereas baicalin (at 10–20 μg /mL) decreased the uptake of nimodipine in rat brain microvascular endothelial cell culture. Liu et al. [95,96] developed a novel brain-targeting drug delivery system based on baicalin-loaded PEGylated cationic solid lipid nanoparticles modified by OX26 antibody (OX26-PEG-CSLN) and demonstrated that OX26-PEG-CSLN improved the uptake of baicalin across the BBB, and enhanced the bioavailability of baicalin in cerebral spinal fluid of rats with cerebral ischemia/reperfusion injury.
Another study demonstrated that intranasal administration of baicalin, about 52.36–100% baicalin content at 8 h, was transported to the brain through the olfactory pathway [97]. Zhang et al. [98] also investigated the pharmacokinetic process of baicalin in normal rat blood, as well as cerebral nuclei, such as cortex, hippocampus, striatum, thalamus, and brain stem. Yang et al. [99] examined the role of Panax notoginsenosides in the pharmacokinetic behavior of baicalin in rat brain. The data indicated that Panax notoginsenosides decreased the elimination rate of baicalin from rat plasma and promoted the penetration of baicalin into rat brain. Additionally, Panax notoginsenosides increased the concentration and reduced the elimination of baicalin from rat brain. A recent study also demonstrated that six Radix scutellariae flavones such as baicalein, wogonin, oroxylin A, baicalin, wogonoside, and oroxyloside could cross the blood–brain barrier, with brain concentrations ranging from 7.9 to 224.0 pmol/g [100].
3. Conclusions and Future Perspectives
S. baicalensis has been traditionally used for the treatment of a variety of disorders since ancient times. Baicalin is the main bioactive component from the root of S. baicalensis. The present review summarizes the protective effects of baicalin for the treatment of neurotoxicity-related diseases such as ischemic stroke, AD, and PD. In addition, baicalin exhibits considerable anxiolytic-like and antidepressant effects. In the mechanistic aspects, baicalin shows a strong protective activity against neurotoxicity-mediated disorders by regulating different cell signaling pathways. The published reports reveal that baicalin has antioxidant, anti-inflammatory, anti-apoptotic, and anti-excitotoxicity properties. Interestingly, baicalin promotes neurogenesis and cell differentiation. Baicalin may be a potential candidate for the prevention and treatment of various neurodegenerative diseases and enhancement of cognitive functions due to its multitargeted actions and BBB-penetrating ability. Although baicalin showed potent neuroprotective effects under in vitro and in vivo models, clinical studies in association with baicalin against these diseases are meager. Further studies in relation to safety profiles of baicalin, improvement of its bioavailability and clinical trials are needed.
Author Contributions
K.S. wrote the manuscript; P.D. and M.K. conducted the literature review; S.J.P. and S.K. corrected and revised the manuscript.
Acknowledgments
This work was supported by Korea Institute of Planning and Evaluation for Technology in Food, Agriculture, Forestry and Fisheries (IPET) through High Value-added Food Technology Development Program, funded by Ministry of Agriculture, Food and Rural Affairs (MAFRA) (317044-03) and the research grant from Kangwon National University, Chuncheon, Republic of Korea.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| 11β-HSD2 | 11β-hydroxysteroid dehydrogenase-2 |
| 5-LOX | 5-lipoxygenase (5-LOX) |
| AchE | acetylcholinesterase |
| AD | Alzheimer’s disease |
| Akt | protein kinase B |
| AMPA | α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid |
| APP | amyloid precursor protein |
| APPL2 | adaptor protein, phosphotyrosine interacting with PH domain and leucine zipper 2 |
| Aβ | amyloid-β |
| BBB | blood–brain barrier |
| BCCA | bilateral common carotid artery |
| BCCL | bilateral common carotid artery ligation |
| Bcl-2 | B cell lymphoma 2 family |
| BDNF | brain-derived neurotrophic factor |
| bHLH | basic helix–loop–helix |
| CaMKII | Ca2+/calmodulin-dependent protein kinase II |
| CD11b | cluster of differentiation molecule 11b |
| ChAT | choline acetyltransferase |
| CMS | chronic mild stress |
| CNS | central nervous system |
| CNTF | ciliary neurotrophic factor |
| COX-1/2 | cyclooxygenases-1/2 |
| CREB | cAMP response element-binding protein |
| CXCL3 | chemokine (C–X–C motif) ligand 3 (CXCL-3) |
| Drp-1 | dynamin-related protein 1 |
| DWI | diffusion weighted imaging |
| ERK1/2 | extracellular signal-regulated kinases 1 and 2 |
| GABA(A)R | GABAA receptor |
| GABA | gamma-aminobutyric acid |
| GDNF | glial cell-derived neurotrophic factor |
| GFAP | glial fibrillary acidic protein |
| GR | glucocorticoid receptor |
| GSH-Px | glutathione peroxidase |
| GSH | glutathione |
| GSK-3β | glycogen synthase kinase 3 beta |
| H2O2 | hydrogen peroxide |
| HSP-70 | heat shock protein-70 |
| IL-6 | interleukin 6 |
| IL-β | interleukin beta |
| iNOS | inducible nitric oxide synthase |
| IκB-α | nuclear factor of kappa light polypeptide gene enhancer in B cells inhibitor-alpha |
| JAK2 | Janus kinase 2 |
| JNK | c-Jun N-terminal kinase |
| KCC2 | K–Cl co-transporter 2 |
| LDH | lactate dehydrogenase |
| MAP-2 | microtubule-associated protein |
| MAPK | mitogen-actives protein kinases |
| MCAO | middle cerebral artery occlusion |
| MCL-1 | myeloid cell leukemia-1 |
| MDA | malondialdehyde |
| MFN2 | mitochondrial fission, elevated mitofusin-2 |
| MMP-9 | matrix metallopeptidase 9 |
| MPO | myeloperoxidase |
| MPTP | 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine |
| MRI | magnetic resonance imaging |
| MRTF-A | myocardin-related transcription factor-A |
| MyD88 | myeloid differentiation primary response 88 |
| NF-κB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NKCC1 | Na–K–Cl cotransporter-1 |
| NLRP3 | nucleotide-binding domain and leucine-rich repeat protein-3 |
| NMDA | N-methyl-d-aspartic acid |
| NMDAR1 | N-methyl-d-aspartic acid receptor-1 |
| NO | nitric oxide |
| NOD2 | nucleotide-binding oligomerization domain protein 2 |
| NOX | nicotinamide adenine dinucleotide 2′-phosphate oxidase |
| Nrf2 | nuclear factor erythroid 2-related factor 2 |
| NSPCs | neural stem/progenitor cells |
| OGD | oxygen/glucose deprivation |
| OGD/RO | oxygen/glucose deprivation/reoxygenation |
| PAR-1 | protease-activated receptor-1 |
| PD | Parkinson’s disease |
| PGE2 | prostaglandin E2 |
| PI3K | phosphatidylinositide 3-kinase |
| POP | prolyl oligopeptidase |
| ROS | reactive oxygen species |
| SCI | spinal cord injury |
| SCs | Schwann cells |
| SGK1 | serum- and glucocorticoid-regulated kinase 1 |
| siRNA | small interfering RNA |
| SOD | superoxide dismutase |
| STAT3 | signal transducer and activator of transcription 3 |
| TH | tyrosine hydroxylase |
| TLR4 | Toll like receptor-4 |
| TNF-α | tumor necrosis factor alpha |
| TRAF6 | tumor necrosis factor receptor-associated factor 6 |
| TRkB | tropomyosin receptor kinase B |
| TTC | 2,3,5-triphenyltetrazolium chloride |
| ZO-1 | zonula occludens-1. |
References
- Zhao, Q.; Chen, X.Y.; Martin, C. Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Sci. Bull. (Beijing) 2016, 6, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; He, X.; He, X.; Li, M.; Zhang, R.; Fan, P.; Zhang, Q.; Jia, Z. The genus Scutellaria an ethnopharmacological and phytochemical review. J. Ethnopharmacol. 2010, 128, 279–313. [Google Scholar] [CrossRef] [PubMed]
- Gaire, B.P.; Moon, S.K.; Kim, H. Scutellaria baicalensis in stroke management: Nature’s blessing in traditional Eastern medicine. Chin. J. Integr. Med. 2014, 20, 712–720. [Google Scholar] [CrossRef] [PubMed]
- Ishimaru, K.; Nishikawa, K.; Omoto, T.; Asai, I.; Yoshihira, K.; Shimomura, K. Two flavone 21-glucosides from Scutellaria baicalensis. Phytochemistry 1995, 40, 279–281. [Google Scholar] [CrossRef]
- Noh, K.; Kang, Y.; Nepal, M.R.; Jeong, K.S.; Oh, D.G.; Kang, M.J.; Lee, S.; Kang, W.; Jeong, H.G.; Jeong, T.C. Role of intestinal microbiota in baicalin-induced drug interaction and its pharmacokinetics. Molecules 2016, 21, 337. [Google Scholar] [CrossRef] [PubMed]
- Zheljazkov, V.D.; Cantrell, C.L.; Ebelhar, M.W.; Coker, C.; Evans, W.B. Quality assessment and yield of baikal skullcap (Scutellaria baicalensis) grown at multiple locations. HortScience 2007, 42, 1183–1187. [Google Scholar]
- Bochoráková, H.; Paulová, H.; Slanina, J.; Musil, P.; Táborská, E. Main flavonoids in the root of Scutellaria baicalensis cultivated in Europe and their comparative antiradical properties. Phytother. Res. 2003, 17, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Dinda, B.; Dinda, S.; DasSharma, S.; Banik, R.; Chakraborty, A.; Dinda, M. Therapeutic potentials of baicalin and its aglycone, baicalein against inflammatory disorders. Eur. J. Med. Chem. 2017, 131, 68–80. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Huang, X.; Chen, W. The effects of baicalin and baicalein on cerebral ischemia: A review. Aging Dis. 2017, 8, 850–867. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, C. Baicalin ameliorates chronic unpredictable mild stress-induced depressive behavior: Involving the inhibition of NLRP3 inflammasome activation in rat prefrontal cortex. Int. Immunopharmacol. 2017, 48, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Gasiorowski, K.; Lamer-Zarawska, E.; Leszek, J.; Parvathaneni, K.; Yendluri, B.B.; Błach-Olszewska, Z.; Aliev, G. Flavones from root of Scutellaria baicalensis Georgi: Drugs of the future in neurodegeneration? CNS Neurol. Disord. Drug Targets 2011, 10, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Ju, X.N.; Mu, W.N.; Liu, Y.T.; Wang, M.H.; Kong, F.; Sun, C.; Zhou, Q.B. Baicalin protects against thrombin induced cell injury in SH-SY5Y cells. Int. J. Clin. Exp. Pathol. 2015, 8, 14021–14027. [Google Scholar] [PubMed]
- Li, S.; Sun, X.; Xu, L.; Sun, R.; Ma, Z.; Deng, X.; Liu, B.; Fu, Q.; Qu, R.; Ma, S. Baicalin attenuates in vivo and in vitro hyperglycemia-exacerbated ischemia/reperfusion injury by regulating mitochondrial function in a manner dependent on AMPK. Eur. J. Pharmacol. 2017, 815, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Wang, C.; Chen, H.; Hu, Y.; Tian, L.; Pan, J.; Geng, M. Aβ-induced microglial cell activation is inhibited by baicalin through the JAK2/STAT3 signaling pathway. Int. J. Neurosci. 2014, 124, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.X.; Wang, F.; Cao, X.L.; Pan, H.Y.; Liu, X.Y.; Hu, X.M.; Sun, Y.Y. Baicalin protects PC-12 cells from oxidative stress induced by hydrogen peroxide via anti-apoptotic effects. Brain Inj. 2014, 28, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Zuo, D.; Lin, Y.; Liu, L.; Wang, C.; Xu, J.; Sun, F.; Li, L.; Li, Z.; Wu, Y. Baicalin attenuates ketamine-induced neurotoxicity in the developing rats: Involvement of PI3K/Akt and CREB/BDNF/Bcl-2 pathways. Neurotox. Res. 2016, 30, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Tejada, S.; Setzer, W.; Daglia, M.; Nabavi, S.F.; Sureda, A.; Braidy, N.; Gortzi, O.; Nabavi, S.M. Neuroprotective effects of ellagitannins: A brief review. Curr. Drug Targets 2016, 7, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.L.; Yang, C.M. Role of redox signaling in neuroinflammation and neurodegenerative disease. BioMed Res. Int. 2013, 2013, 484613. [Google Scholar] [CrossRef] [PubMed]
- Sowndhararajan, K.; Deepa, P.; Kim, M.; Park, S.J.; Kim, S. Baicalein as a potent neuroprotective agent: A review. Biomed. Pharmacother. 2017, 95, 1021–1032. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Li, G.; Wang, Y.F.; Fan, Z.K.; Yu, D.S.; Wang, Z.D.; Bi, Y.L. Neuroprotective effect of baicalin on compression spinal cord injury in rats. Brain Res. 2010, 1357, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.X.; Cao, X.L.; Wang, F.; Wang, J.; Ying, T.Z.; Xiao, W.; Zhang, Y.; Xing, H.; Dong, W.; Xu, S.Q.; et al. Baicalin inhibiting cerebral ischemia/hypoxia-induced neuronal apoptosis via MRTF-A-mediated transactivity. Eur. J. Pharmacol. 2015, 767, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Bao-An, C.; Senthilkumar, R.; Rong, F.; Guo, Q.L. Cardioprotective potential of baicalein: A short review of in vitro and in vivo studies. Pharm. Anal. Acta 2014, 5, 280–284. [Google Scholar]
- de Oliveira, M.R.; Nabavi, S.F.; Habtemariam, S.; Erdogan Orhan, I.; Daglia, M.; Nabavi, S.M. The effects of baicalein and baicalin on mitochondrial function and dynamics: A review. Pharmacol. Res. 2015, 100, 296–308. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Snyder, S.A.; Smith, J.N.; Chen, Y.C. Anticancer properties of baicalein: A review. Med. Chem. Res. 2016, 25, 1515–1523. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.R.; Do, C.W.; To, C.H. Potential therapeutic effects of baicalein, baicalin and wogonin in ocular disorders. J. Ocul. Pharmacol. Ther. 2014, 30, 605–614. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.Y.; Hsiu, S.L.; Tsai, S.Y.; Hou, Y.C.; Chao, P.D.L. Comparison of metabolic pharmacokinetics of baicalin and baicalein in rats. J. Pharm. Pharmacol. 2003, 55, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Du, L.; Wang, S.; He, G.; Yang, T.; Li, X. Pharmacokinetic study of baicalein and its major metabolites after IV administration in dogs. Chin. Herb. Med. 2011, 3, 196–201. [Google Scholar]
- Dou, J.; Chen, L.; Xu, G.; Zhang, L.; Zhou, H.; Wang, H.; Su, Z.; Ke, M.; Guo, Q.; Zhou, C. Effects of baicalein on sendai virus in vivo are linked to serum baicalin and its inhibition of hemagglutinin-neuraminidase. Arch. Virol. 2011, 156, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.I.; Kim, H.J.; Hwang, K.M.; Jekal, S.J.; Pae, H.O.; Choi, B.M.; Yun, Y.G.; Kwon, T.O.; Chung, H.T.; Kim, Y.C. Hepatoprotective effect of baicalin, a major flavone from Scutellaria radix, on acetaminophen-induced liver injury in mice. Immunopharmacol. Immunotoxicol. 2003, 25, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.Y.; Wei, E.Q.; Zhao, Y.M.; Chen, F.X.; Wang, M.L.; Zhang, W.P.; Chen, Z. Protective effects of baicalin on oxygen/glucose deprivation- and NMDA-induced injuries in rat hippocampal slices. J. Pharm. Pharmacol. 2005, 57, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Ge, Q.F.; Hu, X.; Ma, Z.Q.; Liu, J.R.; Zhang, W.P.; Chen, Z.; Wei, E.Q. Baicalin attenuates oxygen-glucose deprivation-induced injury via inhibiting NMDA receptor-mediated 5-lipoxygenase activation in rat cortical neurons. Pharmacol. Res. 2007, 55, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.H.; Kang, K.D.; Ji, D.; Fawcett, R.J.; Safa, R.; Kamalden, T.A.; Osborne, N.N. The flavonoid baicalin counteracts ischemic and oxidative insults to retinal cells and lipid peroxidation to brain membranes. Neurochem. Int. 2008, 53, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Tarragó, T.; Kichik, N.; Claasen, B.; Prades, R.; Teixidó, M.; Giralt, E. Baicalin, a prodrug able to reach the CNS, is a prolyl oligopeptidase inhibitor. Bioorg. Med. Chem. 2008, 16, 7516–7524. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Hu, J.; Ma, L.; Yuan, Z.; Wang, Y.; Wang, X.; Xing, D.; Lei, F.; Du, L. Comprehensive study of baicalin down-regulating NOD2 receptor expression of neurons with oxygen-glucose deprivation in vitro and cerebral ischemia-reperfusion in vivo. Eur. J. Pharmacol. 2010, 649, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Yin, F.; Liu, J.; Ji, X.; Wang, Y.; Zidichouski, J.; Zhang, J. Baicalin prevents the production of hydrogen peroxide and oxidative stress induced by Aβ aggregation in SH-SY5Y cells. Neurosci. Lett. 2011, 492, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Wang, J.; Zhang, P.; Li, D.; Zhang, C.; Zhao, H.; Fu, J.; Wang, B.; Liu, J. Baicalin attenuates proinflammatory cytokine production in oxygen-glucose deprived challenged rat microglial cells by inhibiting TLR4 signaling pathway. Int. Immunopharmacol. 2012, 14, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhuang, P.; Shen, B.; Zhang, Y.; Shen, J. Baicalin promotes neuronal differentiation of neural stem/progenitor cells through modulating p-stat3 and bHLH family protein expression. Brain Res. 2012, 1429, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Lu, Y.; Zhong, X.; Song, W.; Wang, X.; Sun, X.; Qin, J.; Guo, S.; Wang, Q. Baicalin’s therapeutic time window of neuroprotection during transient focal cerebral ischemia and its antioxidative effects in vitro and in vivo. Evid. Based Complement. Alternat. Med. 2013, 2013, 120261. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Lv, P.; Li, J.; Wang, H.; Zhou, T.; Liu, Y.; Lin, W. Baicalin inhibits colistin sulfate-induced apoptosis of PC12 cells. Neural Regen. Res. 2013, 8, 2597–2604. [Google Scholar] [PubMed]
- Xu, M.; Chen, X.; Gu, Y.; Peng, T.; Yang, D.; Chang, R.C.; So, K.F.; Liu, K.; Shen, J. Baicalin can scavenge peroxynitrite and ameliorate endogenous peroxynitrite-mediated neurotoxicity in cerebral ischemia-reperfusion injury. J. Ethnopharmacol. 2013, 150, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Hou, J.; Fu, J.; Li, D.; Zhang, C.; Liu, J. Baicalin protects rat brain microvascular endothelial cells injured by oxygen-glucose deprivation via anti-inflammation. Brain Res. Bull. 2013, 97, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, P.W.; Cui, G.Z.; Zhang, Y.J.; Zhang, M.X.; Guo, H.; Zhang, J.B.; Lu, Z.Q.; Isaiah, A.O.; Lin, Y.X. Baicalin regulates neuronal fate decision in neural stem/progenitor cells and stimulates hippocampal neurogenesis in adult rats. CNS Neurosci. Ther. 2013, 19, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Chen, X.; Xiong, P. Baicalin suppresses iron accumulation after substantia nigra injury: Relationship between iron concentration and transferrin expression. Neural Regen. Res. 2014, 9, 630–636. [Google Scholar] [PubMed]
- Morita, A.; Soga, K.; Nakayama, H.; Ishida, T.; Kawanishi, S.; Sato, E.F. Neuronal differentiation of human iPS cells induced by baicalin via regulation of bHLH gene expression. Biochem. Biophys. Res. Commun. 2015, 465, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Han, X.; Wang, J.; Sun, J. Baicalin may have a therapeutic effect in attention deficit hyperactivity disorder. Med. Hypotheses 2015, 85, 761–764. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Cao, Y.; Yu, J.; Liu, R.; Bai, B.; Qi, H.; Zhang, Q.; Guo, W.; Zhu, H.; Qu, L. Baicalin alleviates ischemia-induced memory impairment by inhibiting the phosphorylation of CaMKII in hippocampus. Brain Res. 2016, 1642, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zhao, R.; Yan, W.; Wang, H.; Jia, M.; Zhu, N.; Zhu, Y.; Zhang, Y.; Wang, P.; Lei, H. Compositions, formation mechanism, and neuroprotective effect of compound precipitation from the traditional Chinese prescription Huang-Lian-Jie-Du-Tang. Molecules 2016, 21, 1094. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Li, S.; Zhu, L.; Fang, S.H.; Chen, J.L.; Xu, Q.Q.; Li, H.Y.; Luo, N.C.; Yang, C.; Luo, D.; et al. Effect of baicalin on oxygen-glucose deprivation-induced endothelial cell damage. Neuroreport 2017, 28, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Zuo, W.; Wu, H.; Zhang, K.; Lv, P.; Xu, F.; Jiang, W.; Zheng, L.; Zhao, J. Baicalin promotes the viability of Schwann cells in vitro by regulating neurotrophic factors. Exp. Ther. Med. 2017, 14, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Zhuge, W.; Hu, J.; Yang, J.; Wang, X.; Wen, F.; Wang, C.; Zhuge, Q. Baicalin reverses the impairment of synaptogenesis induced by dopamine burden via the stimulation of GABAAR-TrkB interaction in minimal hepatic encephalopathy. Psychopharmacology 2018, 235, 1163–1178. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wang, H.; Chen, J.H.; Wang, L.H.; Zhang, H.S.; Fan, Y. Determination of amino acid neurotransmitters in cerebral cortex of rats administered with baicalin prior to cerebral ischemia by capillary electrophoresis-laser-induced fluorescence detection. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2003, 788, 93–101. [Google Scholar] [CrossRef]
- Liao, J.F.; Hung, W.Y.; Chen, C.F. Anxiolytic-like effects of baicalein and baicalin in the Vogel conflict test in mice. Eur. J. Pharmacol. 2003, 464, 141–146. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, Z.; Zhang, X.; Ying, K.; Liu, J.; Wang, Y. Gene expression profile induced by oral administration of baicalin and gardenin after focal brain ischemia in rats. Acta Pharmacol. Sin. 2005, 26, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Wang, F.; Tsang, S.Y.; Ho, K.H.; Zheng, H.; Yuen, C.T.; Chow, C.Y.; Xue, H. Anxiolytic-Like Effect of baicalin and its additivity with other anxiolytics. Planta Med. 2006, 72, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xing, D.; Wang, W.; Wang, R.; Du, L. Kinetic difference of baicalin in rat blood and cerebral nuclei after intravenous administration of Scutellariae Radix extract. J. Ethnopharmacol. 2006, 103, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.P.; Huang, W.T.; Cheng, B.C.; Hsu, C.C.; Lin, M.T. The flavonoid baicalin protects against cerebrovascular dysfunction and brain inflammation in experimental heatstroke. Neuropharmacology 2007, 52, 1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, N.; Zou, H.Y. Protective effect of baicalin on mouse with Parkinson’s disease induced by MPTP. Zhongguo Zhong Xi Yi Jie He Za Zhi 2007, 27, 1010–1012. [Google Scholar] [PubMed]
- Wang, F.; Xu, Z.; Ren, L.; Tsang, S.Y.; Xue, H. GABA a receptor subtype selectivity underlying selective anxiolytic effect of baicalin. Neuropharmacology 2008, 55, 1231–1237. [Google Scholar] [CrossRef] [PubMed]
- Tu, X.K.; Yang, W.Z.; Shi, S.S.; Wang, C.H.; Chen, C.M. Neuroprotective effect of baicalin in a rat model of permanent focal cerebral ischemia. Neurochem. Res. 2009, 34, 1626–1634. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wu, R.; Li, P.; Liu, F.; Zhang, W.; Zhang, P.; Li, P.; Wang, Y. Baicalin administration is effective in positive regulation of twenty-four ischemia/reperfusion-related proteins identified by a proteomic study. Neurochem. Int. 2009, 54, 488–496. [Google Scholar] [CrossRef] [PubMed]
- Xue, X.; Qu, X.J.; Yang, Y.; Sheng, X.H.; Cheng, F.; Jiang, E.N.; Wang, J.H.; Bu, W.; Liu, Z.P. Baicalin attenuates focal cerebral ischemic reperfusion injury through inhibition of nuclear factor κB p65 activation. Biochem. Biophys. Res. Commun. 2010, 403, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Mao, X.; Sun, C.; Zheng, P.; Gao, J.; Wang, X.; Min, D.; Sun, H.; Xie, N.; Cai, J. Baicalin attenuates global cerebral ischemia/reperfusion injury in gerbils via anti-oxidative and anti-apoptotic pathways. Brain Res. Bull. 2011, 85, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Tu, X.K.; Yang, W.Z.; Liang, R.S.; Shi, S.S.; Chen, J.P.; Chen, C.M.; Wang, C.H.; Xie, H.S.; Chen, Y.; Ouyang, L.Q. Effect of baicalin on matrix metalloproteinase-9 expression and blood-brain barrier permeability following focal cerebral ischemia in rats. Neurochem. Res. 2011, 36, 2022–2028. [Google Scholar] [CrossRef] [PubMed]
- Tu, X.K.; Yang, W.Z.; Shi, S.S.; Chen, Y.; Wang, C.H.; Chen, C.M.; Chen, Z. Baicalin inhibits TLR2/4 signaling pathway in rat brain following permanent cerebral ischemia. Inflammation 2011, 34, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Cheng, O.; Li, Z.; Han, Y.; Jiang, Q.; Yan, Y.; Cheng, K. Baicalin improved the spatial learning ability of global ischemia/reperfusion rats by reducing hippocampal apoptosis. Brain Res. 2012, 1470, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Gaire, B.P.; Song, J.; Lee, S.H.; Kim, H. Neuroprotective effect of four flavonoids in the root of Scutellaria baicalensis Georgi. Planta Med. 2012, 78, PF71. [Google Scholar] [CrossRef]
- Liu, Y.F.; Gao, F.; Li, X.W.; Jia, R.H.; Meng, X.D.; Zhao, R.; Jing, Y.Y.; Wang, Y.; Jiang, W. The anticonvulsant and neuroprotective effects of baicalin on pilocarpine-induced epileptic model in rats. Neurochem. Res. 2012, 37, 1670–1680. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Zhao, M.; Liu, H.; Wang, L.; Zhang, X. Pharmacokinetic effects of baicalin on cerebral ischemia-reperfusion after iv administration in rats. Chin. Herb. Med. 2012, 4, 53–57. [Google Scholar]
- Xiong, P.; Chen, X.; Guo, C.; Zhang, N.; Ma, B. Baicalin and deferoxamine alleviate iron accumulation in different brain regions of Parkinson’s disease rats. Neural Regen. Res. 2012, 7, 2092–2098. [Google Scholar] [PubMed]
- Zhou, Q.B.; Jia, Q.; Zhang, Y.; Li, L.Y.; Chi, Z.F.; Liu, P. Effects of baicalin on protease-activated receptor-1 expression and brain injury in a rat model of intracerebral hemorrhage. Chin. J. Physiol. 2012, 55, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Chen, L.; Qiu, Y.M.; Li, S.Q.; Xiong, W.H.; Yin, Y.H.; Jia, F.; Jiang, J.Y. Activations of GABAergic signaling, HSP70 and MAPK cascades are involved in baicalin’s neuroprotection against gerbil global ischemia/reperfusion injury. Brain Res. Bull. 2013, 90, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhang, Y.; Yu, Y.; Li, B.; Chen, Y.; Wu, H.; Wang, J.; Li, J.; Xiong, X.; He, Q.; et al. Systemic revealing pharmacological signalling pathway networks in the hippocampus of ischaemia-reperfusion mice treated with baicalin. Evid. Based Complement. Alternat. Med. 2013, 2013, 630723. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Shen, J.D.; Li, J.; Wang, R.; Jiao, S.; Yi, L.T. Chronic treatment with baicalin prevents the chronic mild stress-induced depressive-like behavior: Involving the inhibition of cyclooxygenase-2 in rat brain. Prog. Neuropsychopharmacol. Biol. Psychiatry 2013, 40, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, P.; Wang, Y.; Liu, J.; Zhang, Z.; Cheng, W.; Wang, Y. Ameliorative effects of a combination of baicalin, jasminoidin and cholic acid on ibotenic acid-induced dementia model in rats. PLoS ONE 2013, 8, e56658. [Google Scholar]
- Lee, B.; Sur, B.; Shim, I.; Lee, H.; Hahm, D.H. Baicalin improves chronic corticosterone-induced learning and memory deficits via the enhancement of impaired hippocampal brain-derived neurotrophic factor and cAMP response element-binding protein expression in the rat. J. Nat. Med. 2014, 68, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Yin, Z.; Yang, S.; Ma, S. Baicalin reverse AMPA receptor expression and neuron apoptosis in chronic unpredictable mild stress rats. Biochem. Biophys. Res. Commun. 2014, 451, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.B.; Jin, Y.L.; Jia, Q.; Zhang, Y.; Li, L.Y.; Liu, P.; Liu, Y.T. Baicalin attenuates brain edema in a rat model of intracerebral hemorrhage. Inflammation 2014, 37, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Li, X.; Gao, P.; Tu, Y.; Zhao, M.; Li, J.; Zhang, S.; Liang, H. Baicalin attenuates alzheimer-like pathological changes and memory deficits induced by amyloid β1-42 protein. Metab. Brain Dis. 2015, 30, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Wang, H.; Zhao, Y.; Sun, D.; Zhai, X. Protective effects of baicalin on Aβ1–42-induced learning and memory deficit, oxidative stress, and apoptosis in rat. Cell Mol. Neurobiol. 2015, 35, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Wang, L.L.; Pei, Y.Y.; Shen, J.D.; Li, H.B.; Wang, B.Y.; Bai, M. Baicalin decreases SGK1 expression in the hippocampus and reverses depressive-like behaviors induced by corticosterone. Neuroscience 2015, 311, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Ma, P.; Mao, X.Y.; Li, X.L.; Ma, Y.; Qiao, Y.D.; Liu, Z.Q.; Zhou, H.H.; Cao, Y.G. Baicalin alleviates diabetes-associated cognitive deficits via modulation of mitogen-activated protein kinase signaling, brain-derived neurotrophic factor and apoptosis. Mol. Med. Rep. 2015, 12, 6377–6383. [Google Scholar] [CrossRef] [PubMed]
- Dang, H.; Li, K.; Yu, Y.; Zhang, Y.; Liu, J.; Wang, P.; Li, B.; Wang, H.; Li, H.; Wang, Z.; et al. Variation of pathways and network profiles reveals the differential pharmacological mechanisms of each effective component to treat middle cerebral artery ischemia-reperfusion mice. Exp. Biol. Med. 2016, 241, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.J.; Liang, R.S.; Shi, S.S.; Wang, C.H.; Yang, W.Z. Effect of baicalin on hippocampal damage in kainic acid-induced epileptic mice. Exp. Ther. Med. 2016, 12, 1405–1411. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.Y.; Yin, Z.J.; Yang, S.J.; Ma, S.P.; Qu, R. Baicalin reverses depressive-like behaviours and regulates apoptotic signalling induced by olfactory bulbectomy. Phytother. Res. 2016, 30, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Bitto, A.; Giuliani, D.; Pallio, G.; Irrera, N.; Vandini, E.; Canalini, F.; Zaffe, D.; Ottani, A.; Minutoli, L.; Rinaldi, M.; et al. Effects of COX1-2/5-LOX blockade in Alzheimer transgenic 3xTg-AD mice. Inflamm. Res. 2017, 66, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Guan, B.; Chen, X.; Chen, X.; Li, C.; Qiu, J.; Yang, D.; Liu, K.J.; Qi, S.; Shen, J. Baicalin attenuates blood-brain barrier disruption and hemorrhagic transformation and improves neurological outcome in ischemic stroke rats with delayed t-PA treatment: Involvement of ONOO--MMP-9 pathway. Transl. Stroke Res. 2017. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Liu, J.; Wang, P.; Zhang, Y.; Li, B.; Yu, Y.; Dang, H.; Li, H.; Zhang, X.; Wang, Z. Poly-dimensional network comparative analysis reveals the pure pharmacological mechanism of baicalin in the targeted network of mouse cerebral ischemia. Brain Res. 2017, 1666, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Fu, Y.; Zhang, S.; Ding, H.; Chen, J. Baicalin attenuates subarachnoid hemorrhagic brain injury by modulating blood-brain barrier disruption, inflammation, and oxidative damage in mice. Oxid. Med. Cell Longev. 2017, 2017, 1401790. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.Q.; Li, Y.L.; Ao, Z.B.; Wen, Z.L.; Chen, Q.W.; Huang, Z.G.; Xiao, B.; Yan, X.H. Baicalin protects neonatal rat brains against hypoxic-ischemic injury by upregulating glutamate transporter 1 via the phosphoinositide 3-kinase/protein kinase B signaling pathway. Neural Regen. Res. 2017, 12, 1625–1631. [Google Scholar] [PubMed]
- Gao, C.; Du, Q.; Li, W.; Deng, R.; Wang, Q.; Xu, A.; Shen, J. Baicalin modulates APPL2/glucocorticoid receptor signaling cascade, promotes neurogenesis, and attenuates emotional and olfactory dysfunctions in chronic corticosterone-induced depression. Mol. Neurobiol. 2018. [CrossRef] [PubMed]
- Zhao, J.; Lu, S.; Yu, H.; Duan, S.; Zhao, J. Baicalin and ginsenoside Rb1 promote the proliferation and differentiation of neural stem cells in Alzheimer’s disease model rats. Brain Res. 2018, 1678, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Ma, S.; Qu, R.; Kang, D.; Liu, Y. Antidepressant effect of baicalin extracted from the root of Scutellaria baicalensis in mice and rats. Pharm. Biol. 2006, 44, 503–510. [Google Scholar] [CrossRef]
- Zhang, K.; Pan, X.; Wang, F.; Ma, J.; Su, G.; Dong, Y.; Yang, J.; Wu, C. Baicalin promotes hippocampal neurogenesis via SGK1- and FKBP5-mediated glucocorticoid receptor phosphorylation in a neuroendocrine mouse model of anxiety/depression. Sci. Rep. 2016, 6, 30951. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.M.; Liu, H.Y.; Xie, L.; Liu, X.D. Effect of baicalin and berberine on transport of nimodipine on primary-cultured, rat brain microvascular endothelial cells. Acta Pharmacol. Sin. 2007, 28, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, L.; He, Q.; Liu, X.; Okeke, C.I.; Tong, L.; Guo, L.; Yang, H.; Zhang, Q.; Zhao, H.; et al. Effect of Baicalin-loaded PEGylated cationic solid lipid nanoparticles modified by OX26 antibody on regulating the levels of baicalin and amino acids during cerebral ischemia-reperfusion in rats. Int. J. Pharm. 2015, 489, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhao, H.; Shu, L.; Zhang, Y.; Okeke, C.; Zhang, L.; Li, J.; Li, N. Preparation and evaluation of Baicalin-loaded cationic solid lipid nanoparticles conjugated with OX26 for improved delivery across the BBB. Drug Dev. Ind. Pharm. 2015, 41, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Je, Y.J.; Yang, M.; Jiang, X.H.; Ma, J.H. Pharmacokinetics of baicalin-phospholipid complex in rat plasma and brain tissues after intranasal and intravenous administration. Pharmazie 2011, 66, 374–377. [Google Scholar] [PubMed]
- Zhang, Z.J.; Li, P.; Wang, Z.; Li, P.T.; Zhang, W.S.; Sun, Z.H.; Zhang, X.J.; Wang, Y.Y. A comparative study on the individual and combined effects of baicalin and jasminoidin on focal cerebral ischemia-reperfusion injury. Brain Res. 2006, 1123, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.F.; Li, Z.; Xin, W.F.; Wang, Y.Y.; Zhang, W.S. Pharmacokinetics and brain distribution differences of baicalin in rat underlying the effect of Panax notoginsenosides after intravenous administration. Chin. J. Nat. Med. 2014, 12, 632–640. [Google Scholar] [CrossRef]
- Fong, S.Y.K.; Li, C.; Ho, Y.C.; Li, R.; Wang, Q.; Wong, Y.C.; Xue, H.; Zuo, Z. Brain uptake of bioactive flavones in Scutellariae Radix and its relationship to anxiolytic effect in mice. Mol. Pharm. 2017, 14, 2908–2916. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).