Preventive Psychological Interventions for the Management of Perinatal Anxiety: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Strategy for the Selection of Studies and Analysis of Results
3. Results
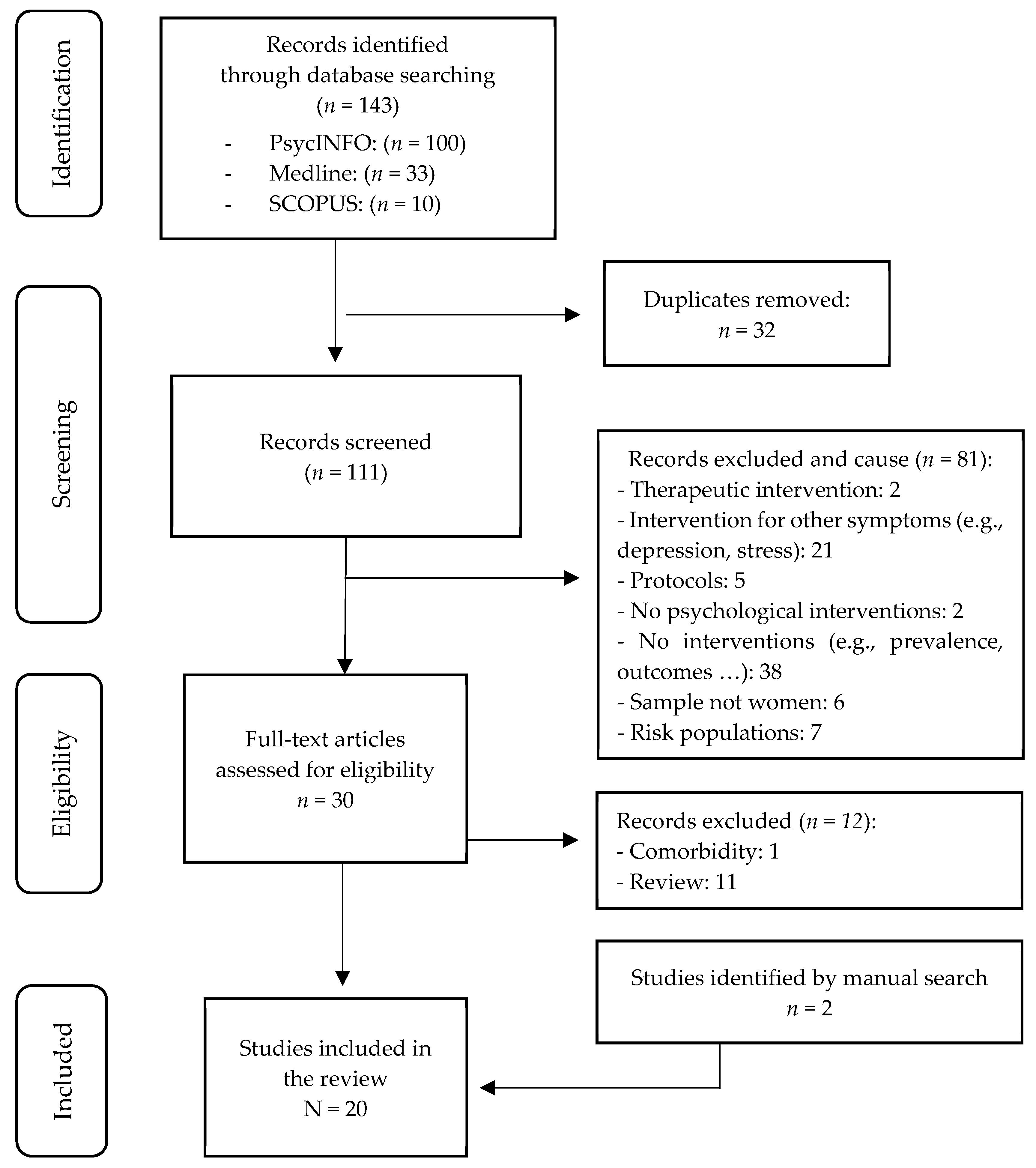
3.1. Study Selection
3.2. Characteristics of Selected Studies
3.3. Characteristics of Interventions
3.3.1. Type of Prevention Program
3.3.2. Therapeutic Approach and Application Format
3.3.3. Effectiveness of Intervention
4. Discussion
4.1. Implications of the Study
4.2. Limitations
4.3. Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hadfield, K.; Akyirem, S.; Sartori, L.; Abdul-Latif, A.M.; Akaateba, D.; Bayrampour, H.; Daly, A.; Hadfield, K.; Abiiro, G.A. Measurement of pregnancy-related anxiety worldwide: A systematic review. BMC Pregnancy Childbirth 2022, 22, 331. [Google Scholar] [CrossRef]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- Higgins, A.; Downes, C.; Carroll, M.; Gill, A.; Monohan, M. There is more to perinatal mental health care than depression: Public health nurses reported engagement and competence in perinatal mental health care. J. Clin. Nurs. 2018, 27, e476–e487. [Google Scholar] [CrossRef]
- World Health Organization. Guide for Integration of Perinatal Mental Health in Maternal and Child Health Services. 2022. Available online: https://www.who.int/publications/i/item/9789240057142?_ga=2.252791369.1707140999.1715966799-1484490870.1713198781 (accessed on 5 June 2025).
- Tang, X.; Lu, Z.; Hu, D.; Zhong, X. Influencing factors for prenatal stress, anxiety and depression in early pregnancy among women in Chongqing, China. J. Affect. Disord. 2019, 253, 292–302. [Google Scholar] [CrossRef]
- Dennis, C.-L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef]
- Falah-Hassani, K.; Shiri, R.; Dennis, C. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A metaanalysis. Psychol. Med. 2017, 47, 2041–2053. [Google Scholar] [CrossRef]
- Maguire, P.N.; Clark, G.I.; Wootton, B.M. The efficacy of cognitive behavior therapy for the treatment of perinatal anxiety symptoms: A preliminary meta-analysis. J. Anxiety Disord. 2018, 60, 26–34. [Google Scholar] [CrossRef]
- Bayrampour, H.; McDonald, S.; Tough, S. Risk factors of transient and persistent anxiety during pregnancy. Midwifery 2015, 31, 582–589. [Google Scholar] [CrossRef]
- Val, A.; Míguez, M.C. Prevalence of antenatal anxiety in European women: A literature review. Int. J. Environ. Res. Public Health 2023, 20, 1098. [Google Scholar] [CrossRef]
- Bauer, A.; Knapp, M.; Parsonage, M. Lifetime costs of perinatal anxiety and depression. J. Affect. Disord. 2016, 192, 83–90. [Google Scholar] [CrossRef]
- Míguez, M.C.; Fernández, V.; Pereira, B. Depresión postparto y factores asociados en mujeres con embarazos de riesgo [Postpartum depression and associated risk factors among women with risk pregnancies]. Behav. Psychol. 2017, 25, 47–64. [Google Scholar]
- Della Vedova, A.M.; Santoniccolo, F.; Sechi, C.; Trombetta, T. Perinatal Depression and Anxiety Symptoms, Parental Bonding and Dyadic Sensitivity in Mother-Baby Interactions at Three Months Post-Partum. Int. J. Environ. Res. Public Health 2023, 20, 4253. [Google Scholar] [CrossRef]
- Field, T. Prenatal anxiety effects: A review. Infant Behav. Dev. 2017, 49, 120–128. [Google Scholar] [CrossRef]
- Dufford, A.J.; Salzwedel, A.P.; Gilmore, J.H.; Gao, W.; Kim, P. Maternal trait anxiety symptoms, frontolimbic resting-state functional connectivity, and cognitive development in infancy. Dev. Psychobiol. 2021, 63, e22166. [Google Scholar] [CrossRef]
- Göbel, A.; Stuhrmann, L.Y.; Harder, S.; Schulte-Markwort, M.; Mudra, S. The association between maternal-fetal bonding and prenatal anxiety: An explanatory analysis and systematic review. J. Affect. Disord. 2018, 239, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Grigoriadis, S.; Graves, L.; Peer, M.; Mamisashvili, L.; Tomlinson, G.; Vigod, S.N.; Dennis, C.-L.; Steiner, M.; Brown, C.; Cheung, A.; et al. A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes. Arch. Women’s Ment. Health 2019, 22, 543–556. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Muñoz, M.F.; Soto-Balbuena, C.; Olivares-Crespo, M.E.; Marcos-Nájera, R.; Al-Halabí, S. Tratamientos psicológicos para los trastornos mentales o del comportamiento asociados con el embarazo, parto o el puerperio. In Fonseca Coord, Manual de Tratamientos Psicológicos: Adultos; Pirámide: Madrid, Spain, 2021; pp. 607–633. [Google Scholar]
- Fonseca, A.; Ganho-Ávila, A.; Berg, M.L.-V.D.; Lupattelli, A.; Rodriguez-Muñoz, M.F.; Ferreira, P.; Radoš, S.N.; Bina, R. Emerging issues and questions on peripartum depression prevention, diagnosis and treatment: A consensus report from the cost action riseup-PPD. J. Affect. Disord. 2020, 274, 167–173. [Google Scholar] [CrossRef]
- O’Mahen, H.; Fedock, G.; Henshaw, E.; Himle, J.A.; Forman, J.; Flynn, H.A. Modifying CBT for perinatal depression: What do women want?: A qualitative study. Cog. Behav. Pract. 2012, 19, 359–371. [Google Scholar] [CrossRef]
- Sockol, L.E. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J. Affect. Disord. 2015, 177, 7–21. [Google Scholar] [CrossRef]
- Loughnan, S.A.; Wallace, M.; Joubert, A.E.; Haskelberg, H.; Andrews, G.; Newby, J.M. A systematic review of psychological treatments for clinical anxiety during the perinatal period. Arch. Women’s Ment. Health 2018, 21, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Dowswell, T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst. Rev. 2013, 2013, CD001134. [Google Scholar] [CrossRef] [PubMed]
- Simhi, M.; Sarid, O.; Cwikel, J. Preferences for mental health treatment for post-partum depression among new mothers. Isr. J. Health Policy Res. 2019, 8, 84. [Google Scholar] [CrossRef] [PubMed]
- Green, S.M.; Haber, E.; Frey, B.N.; McCabe, R.E. Cognitive-behavioral group treatment for perinatal anxiety: A pilot study. Arch. Women’s Ment. Health 2015, 18, 631–638. [Google Scholar] [CrossRef]
- McAllister-Williams, R.H.; Baldwin, D.S.; Cantwell, R.; Easter, A.; Gilvarry, E.; Glover, V.; Green, L.; Gregoire, A.; Howard, L.M.; Jones, I.; et al. British Association for Psychopharmacology consensus guidance on the use of psychotropic medication preconception, in pregnancy and postpartum. J. Psychopharmacol. 2017, 31, 519–552. [Google Scholar] [CrossRef] [PubMed]
- Misri, S.; Abizadeh, J.; Sanders, S.; Swift, E. Perinatal Generalized Anxiety Disorder: Assessment and Treatment. J. Women’s Health 2015, 24, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Sockol, L.E. A systematic review and meta-analysis of interpersonal psychotherapy for perinatal women. J. Affect. Disord. 2018, 232, 316–328. [Google Scholar] [CrossRef]
- Özer, D.; Dişsiz, M. Effects of mindfulness-based practices in the perinatal and postpartum periods on women’s health: A systematic review. Psikiyatr. Güncel Yaklaşımlar 2025, 17, 147–165. [Google Scholar] [CrossRef]
- Mihalopoulos, C.; Chatterton, M.L. Economic evaluations of interventions designed to prevent mental disorders: A systematic review. Early Interv. Psychiatry 2015, 9, 85–92. [Google Scholar] [CrossRef]
- Jorm, A.F.; Patten, S.B.; Brugha, T.S.; Mojtabai, R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 2017, 16, 90–99. [Google Scholar] [CrossRef]
- Muñoz, R.F.; Mrazek, P.J.; Haggerty, R.J. Institute of Medicine report on prevention of mental disorders: Summary and commentary. Am. Psychol. 1996, 51, 1116–1122. [Google Scholar] [CrossRef]
- Muñoz, R.F. Prevent depression in pregnancy to boost all mental health. Nature 2019, 574, 631–633. [Google Scholar] [CrossRef]
- O’Connor, E.; Senger, C.A.; Henninger, M.; Gaynes, B.N.; Coppola, E.; Soulsby Weyrich, M. Interventions to Prevent Perinatal Depression: A Systematic Evidence Review for the U.S. Preventive Services Task Force; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2019. [Google Scholar]
- Rae, C.; McRae, R.; Holliday, E.; Chojenta, C. Interventions to Prevent Relapse or Recurrence of Preconception Anxiety and/or Depression in Perinatal Women: A Systematic Review. Matern. Child Health J. 2025, 29, 294–303. [Google Scholar] [CrossRef]
- Clinkscales, N.; Golds, L.; Berlouis, K.; MacBeth, A. The effectiveness of psychological interventions for anxiety in the perinatal period: A systematic review and meta-analysis. Psychol. Psychother. 2023, 96, 296–327. [Google Scholar] [CrossRef]
- Zimmermann, M.; Julce, C.; Sarkar, P.; McNicholas, E.; Xu, L.; Carr, C.; Boudreaux, E.D.; Lemon, S.C.; Byatt, N. Can psychological interventions prevent or reduce risk for perinatal anxiety disorders? A systematic review and meta-analysis. Gen. Hosp. Psychiatry 2023, 84, 203–214. [Google Scholar] [CrossRef]
- Callanan, F.; Tuohy, T.; Bright, A.M.; Grealish, A. The effectiveness of psychological interventions for pregnant women with anxiety in the antenatal period: A systematic review. Midwifery 2022, 104, 103169. [Google Scholar] [CrossRef] [PubMed]
- Bayrampour, H.; Trieu, J.; Tharmaratnam, T. Effectiveness of eHealth interventions to reduce perinatal anxiety: A systematic review and meta-Analysis. J. Clin. Psychiatry. 2019, 80, 18r12386. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Blackmore, E.R.; Gustafsson, H.; Gilchrist, M.; Wyman, C.; O’Connor, T.G. Pregnancy-related anxiety: Evidence of distinct clinical significance from a prospective longitudinal study. J. Affect. Disord. 2016, 197, 251–258. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT), Version 2018; McGill University: Montreal, QC, Canada, 2018; Available online: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria%20manual_2018%20-08-01_ENG.pdf (accessed on 18 May 2025).
- Dennis-Tiwary, T.A.; Denefrio, S.; Gelber, S. Salutary effects of an attention bias modification mobile application on biobehavioral measures of stress and anxiety during pregnancy. Biol. Psychol. 2017, 127, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, A.; Shiner, C.T.; Grierson, A.B.; Sharrock, M.J.; Loughnan, S.A.; Harrison, V.; Millard, M. Online cognitive behaviour therapy for maternal antenatal and postnatal anxiety and depression in routine care. J. Affect. Disord. 2023, 338, 121–128. [Google Scholar] [CrossRef]
- Anton, R.; David, D. A randomized clinical trial of a new preventive rational emotive and behavioral therapeutical program of prepartum and postpartum emotional distress. J. Evid.-Based Psychother. 2015, 15, 3. [Google Scholar]
- Fontein-Kuipers, Y.J.; Ausems, M.; de Vries, R.; Nieuwenhuijze, M.J. The effect of Wazzup Mama?! An antenatal intervention to prevent or reduce maternal distress in pregnancy. Arch. Women’s Ment. Health 2016, 19, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Salehi, F.; Pourasghar, M.; Khalilian, A.; y Shahhosseini, Z. Comparison of group cognitive behavioral therapy and interactive lectures in reducing anxiety during pregnancy: A quasi experimental trial. Medicine 2016, 95, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Kaur, B. Effect of progressive muscle relaxation on anxiety among antenatal mothers attending antenatal OPD of GGSMC & Hospital, Faridkot, Punjab. Int. J. Nurs. Educ. 2020, 12, 79–84. [Google Scholar]
- Warriner, S.; Crane, C.; Dymond, M.; Krusche, A. An evaluation of mindfulness-based childbirth and parenting courses for pregnant women and prospective fathers/partners within the UK NHS (MBCP-4-NHS). Midwifery 2018, 64, 1–10. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Cui, Y.X.; Zhou, Y.Q.; Li, Y.L. Effects of mindfulness-based stress reduction on prenatal stress, anxiety and depression. Psychol. Health Med. 2019, 24, 51–58. [Google Scholar] [CrossRef]
- Burger, H.; Verbeek, T.; Aris-Meijer, J.L.; Beijers, C.; Mol, B.W.; Hollon, S.D.; Ormel, J.; Van Pampus, M.G.; Bockting, C.L.H. Effects of psychological treatment of mental health problems in pregnant women to protect their offspring: Randomised controlled trial. Br. J. Psychiatry 2020, 216, 182–188. [Google Scholar] [CrossRef]
- Heller, H.M.; Hoogendoorn, A.W.; Honig, A.; Broekam, B.F.P.; van Straten, A. The Effectiveness of a Guided Internet-Based Tool for the Treatment of Depression and Anxiety in Pregnancy (MamaKits Online): Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e15172. [Google Scholar] [CrossRef]
- Loughnan, S.A.; Sie, A.; Hobbs, M.J.; Joubert, A.E.; Smith, J.; Haskelberg, H.; Mahoney, A.E.J.; Kladnitski, N.; Holt, C.J.; Milgrom, J.; et al. A randomized controlled trial of ‘MUMentum pregnancy’: Internet-delivered cognitive behavioral therapy program for antenatal anxiety and depression. J. Affect. Disord. 2019, 243, 381–390. [Google Scholar] [CrossRef]
- MacKinnon, A.L.; Madsen, J.W.; Giesbrecht, G.F.; Campbell, T.; Carlson, L.E.; Dimidjian, S.; Letourneau, N.; Though, S.; Tomfohr-Madsen, L. Effects of mindfulness-based cognitive therapy in pregnancy on psychological distress and gestational age: Outcomes of a randomized controlled trial. Mindfulness 2021, 12, 1173–1184. [Google Scholar] [CrossRef]
- Townshend, K.; Caltabiano, N.J.; Powrie, R.; O’Grady, H. A preliminary study investigating the effectiveness of the caring for body and mind in pregnancy (CBMP) in reducing perinatal depression, anxiety and stress. J. Child Fam. Stud. 2018, 27, 1556–1566. [Google Scholar] [CrossRef]
- Yang, M.; Jia, G.; Sun, S.; Ye, C.; Zhang, R.; Yu, X. Effects of an Online Mindfulness Intervention Focusing on Attention Monitoring and Acceptance in Pregnant Women: A Randomized Controlled Trial. J. Midwifery Womens Health 2019, 64, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Zhou, X.; Ye, C.; Li, J.; Sun, S.; Yu, X. Emphasizing mindfulness training in acceptance relieves anxiety and depression during pregnancy. Psychiatry Res. 2022, 312, 114540. [Google Scholar] [CrossRef] [PubMed]
- Yazdanimehr, R.; Omidi, A.; Sadat, Z.; Akbari, H. The effect of mindfulness integrated cognitive behaviour therapy on depression and anxiety among pregnant women: A randomized clinical trial. J. Caring Sci. 2016, 5, 195–204. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Y.; Wang, J.; Mao, F.; Wu, L.; Huang, Y.; Sun, J.; Cao, F. Effectiveness of digital guided self-help mindfulness training during pregnancy on maternal psychological distress and infant neuropsychological development: Randomized controlled trial. J. Med. Internet Res. 2023, 25, e41298. [Google Scholar] [CrossRef]
- Zhang, X.; Lin, P.; Sun, J.; Sun, Y.; Shao, D.; Cao, D.; Cao, F. Prenatal stress self-help mindfulness intervention via social media: A randomized controlled trial. J. Med. Internet Res. 2023, 32, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Appleton, J.; Fowler, C.; Latouche, L.; Smit, J.; Booker, M.; Fairbrother, G. Evaluation of group therapy intervention for anxiety and depression in the postnatal period. Matern. Child Health J. 2025, 29, 537–548. [Google Scholar] [CrossRef]
- Loughnan, S.A.; Butler, C.; Sie, A.A.; Grierson, A.B.; Chen, A.Z.; Hobbs, M.J.; Joubert, A.E.; Haskelberg, H.; Mahoney, A.; Holt, C.; et al. A randomised controlled trial of ‘MUMentum postnatal’: Internet-delivered cognitive behavioural therapy for anxiety and depression in postpartum women. Behav. Res. Ther. 2019, 116, 94–103. [Google Scholar] [CrossRef]
- Soto-Balbuena, C.; Kovacheva, K.; Rodríguez-Munoz, M.F. Ansiedad durante el embarazo y postparto. In Rodríguez-Muñoz y Caparrós González Coords, Psicología Perinatal en Entornos de Salud; Pirámide: Madrid, Spain, 2022; pp. 39–51. [Google Scholar]
- National Institute for Health and Clinical Excellence. Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance CG192; NICE: London, UK, 2014. [Google Scholar]
- National Collaborating Centre for Mental Health. The Perinatal Mental Health Care Pathways. In Full Implementation Guidance; National Collaborating Centre for Mental Health: London, UK, 2018. [Google Scholar]
- Ruiz-Segovia, N.; Rodriguez-Munoz, M.F.; Olivares, M.E.; Izquierdo, N.; Coronado, P.; Le, H.N. Healthy moms and babies preventive psychological intervention application: A study protocol. Int. J. Environ. Res. Public Health 2021, 18, 12485. [Google Scholar] [CrossRef]
- Barrera, A.Z.; Rosales, M.; Ruiz-Segovia, N.; Rodríguez-Munoz, M.F. Sistemas e-Health en el periodo perinatal. In Rodríguez-Muñoz Coord., Psicología Perinatal: Teoría y Práctica; Pirámide: Madrid, Spain, 2019; pp. 371–381. [Google Scholar]
- Yasuma, N.; Narita, Z.; Sasaki, N.; Obikane, E.; Sekiya, J.; Inagawa, T.; Nakajima, A.; Yamada, Y.; Yamazaki, R.; Matsunaga, A.; et al. Antenatal psychological intervention for universal prevention of antenatal and postnatal depression: A systematic review and meta-analysis. J. Affect. Disord. 2020, 273, 231–239. [Google Scholar] [CrossRef]
- Dahò, M. Conscious decisions in perinatal hospice: Innovative support for parenthood, family psychophysical well-being, and grief processing. Ital. J. Psychol. 2024, 51, 433–450. [Google Scholar] [CrossRef]
- Juarez Padilla, J.; Lara-Cinisomo, S.; Navarrete, L.; Lara, M.A. Perinatal anxiety symptoms: Rates and risk factors in Mexican women. Int. J. Environ. Res. Public Health 2020, 18, 82. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.M.J.; Nogueira, D.A.; Clapis, M.J.; Leite, E.P.R.C. Anxiety in pregnancy: Prevalence and associated factors. Rev. Esc. Enferm. USP 2017, 51, e03253. [Google Scholar] [CrossRef] [PubMed]
- Val, A.; Posse, C.M.; Míguez, M.C. Risk Factors for Prenatal Anxiety in European Women: A Review. J. Clin. Med. 2025, 14, 3248. [Google Scholar] [CrossRef]
| Study | Sample | Duration | Intervention | Results | Conclusions | ||||
|---|---|---|---|---|---|---|---|---|---|
| * Anton and David (2015) Romania [45] | 48 pregnant women with no previous mental illness and no previous psychotherapy. IG: 23 CG: 25 | 9 weekly sessions of 90 min each. First individual session. Subsequent group sessions. | GI: 8-session REBT program GC: usual care | Pretest | Half Treatment | Post-Test | IG significantly reduces anxiety, depression and negative emotionality at mid-treatment and at the end of treatment. Differences in IG remain significant in anxiety and negative emotionality at 3 months postpartum. | ||
| STAI-S (M) | (5th week) | (end) | 3PPM | ||||||
| IG | 42.22 | 39.11 | 35.58 | 32.46 | |||||
| CG | 44.60 | 44.60 | 41.38 | 39.40 | |||||
| * Fontein-Kuipers et al. (2016) Netherlands [46] | 433 pregnant women (4–14 weeks gestation). IG: 218 CG: 215 | Onset in the 1st trimester of pregnancy. | IG: online support program “WazzUp Mama?!” CG: usual care | Pretest (1st trimester) | Post-Test (3rd trimester) | There were significant reductions in anxiety levels between the first and third trimester. The results support the efficacy of the intervention. | |||
| STAI-T ≥ 41 | |||||||||
| IG | 28.7 | 26.9 | |||||||
| CG | 28.9 | 31.6 | |||||||
| * Salehi et al. (2016) Iran [47] | 91 nulliparous pregnant women (13–26 weeks gestation) with a low to moderate level of anxiety (STAI < 75). IG1: 31 IG2: 30 CG: 30 | Beginning in the 2nd trimester of pregnancy. 4 sessions (2 sessions/week) of 120–150 min. | IG1: group cognitive behavioral therapy (GCBT). IG2: interactive classes. CG: usual care | Pretest | Post-Test (4 weeks after treatment) | CBT and interactive lectures were effective in reducing both state and trait anxiety at 4 weeks after the intervention compared to the control group. CBT was more effective than lectures. | |||
| STAI-T (M) | |||||||||
| IG1 | 38.5 | 32.3 | |||||||
| IG2 | 40.8 | 36.2 | |||||||
| CG | 37.7 | 38.0 | |||||||
| STAI-S (M) | |||||||||
| IG1 | 38.0 | 38.0 | |||||||
| IG2 | 41.1 | 41.1 | |||||||
| CG | 38.3 | 38.3 | |||||||
| Dennis-Tiwary et al. (2017) USA [43] | 29 women (19–29 weeks of gestation). IG: 15 CG: 14 | Complete 160 rounds (40/week) of 40 min. | IG: attention bias modification training (ABMT). CG: placebo training (PT). | Pretest | Post-Test (end treatment) | It was observed that there was an increase in anxiety levels between the pre- and post-test means in the intervention group, as assessed using the DASS and HAM-A. | |||
| DASS (M) | |||||||||
| IG | 2.87 | 3.20 | |||||||
| CG | 2.15 | 2.07 | |||||||
| HAM-A (M) | |||||||||
| IG | 7.73 | 9.20 | |||||||
| CG | 7.92 | 6.93 | |||||||
| * Warriner et al. (2018) UK [49] | 64 pregnant women. | 4 weekly sessions of 2.5 h (10 h) | IG: Mindfulness-based childbirth and parenting (MBCP). It combines traditional prenatal teaching with mindfulness-based skills. | Pretest | Post-Test (2 weeks) | Significant differences were observed between pre- and post-test measures for anxiety, depression, stress and worry. This prenatal intervention shows promise for implementation in the national health care system. | |||
| GAD-7 (M) | |||||||||
| 8.53 | 5.08 | ||||||||
| Zhang et al. (2019) China [50] | 63 women between 14 and 28 weeks of gestation. IG: 32 CG: 31 | 8 weekly sessions of 90 min. | IG: Mindfulness-based stress reduction (MBSR) Group therapy (3 to 6 women). CG: usual care. | Pretest | Post-Test | This study provides preliminary evidence that MBSR is suitable for decreasing prenatal stress and anxiety in pregnant Chinese women. | |||
| STAI (M) | |||||||||
| IG | 71.53 | 66.91 | |||||||
| CG | 71.29 | 72.13 | |||||||
| * Sharma et al. (2020) India [48] | 70 pregnant women ≥ 20 weeks gestation. IG: 35 CG: 35 | 4 sessions. | IG: progressive muscle relaxation technique (PMRT). CG: conventional care. | Pretest | Post-Test (4 weeks) | The progressive muscle relaxation technique is effective in reducing anxiety in pregnant women after 4 weeks of intervention. | |||
| PASS (M) | |||||||||
| IG | 33.82 | 28.88 | |||||||
| CG | 34.28 | 38.45 | |||||||
| * Mahoney et al. (2023) Australia [44] | 529 pregnant women. | 3 online skills training lessons. Recommended to be completed in 4–6 weeks. Available for 12 months. | IG: Internet-applied cognitive behavioral therapy (iCBT). | Pretest | Post-Test | Significant pre- and post-treatment reductions in symptoms of anxiety, depression and psychological distress were observed. The results support the use of iCBT in the perinatal stage. | |||
| GAD-7 (EMM) | |||||||||
| 9.62 | 6.76 | ||||||||
| Study | Sample | Duration | Intervention | Results | Conclusions | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pregnancy | |||||||||||
| * Yazdanimehr et al. (2016) Iran [58] | 63 women between the first and sixth month of gestation and with EPDS > 13 BAI > 16 IG: 30 CG: 33 | 8 sessions of 90 min | IG: cognitive behavioral therapy based on mindfulness. CG: usual care. At the end of the intervention, they received a manual on the sessions given in the IG. | Pretest | Post-Test | Mindfulness-based cognitive behavioral therapy can significantly reduce anxiety in pregnant women. | |||||
| (end) | (1 month) | ||||||||||
| BAI (M) | |||||||||||
| IG | M = 19.76 | M = 10.86 | IG | ||||||||
| CG | M = 20.24 | M = 20.54 | CG | ||||||||
| * Townshend et al. (2018) Australia [55] | 109 women < 30 weeks gestation, having had a previous episode of depression and/or elevated depression scores, having risk factors for anxiety or perinatal depression. | 8 sessions (1 session per week) 30-min home practice. | IG: Caring for Body and Mind in Pregnancy (CBMP) | Pretest | Post-Test | CBMP significantly reduced perinatal anxiety and general stress scores. | |||||
| DASS-21 (M) | |||||||||||
| 9.99 | 8.49 | ||||||||||
| PASS (M) | |||||||||||
| 33.95 | 27.13 | ||||||||||
| * Loughnan, Sie, et al. (2019) Australia [53] | 77 women (13–30 weeks gestation) who met criteria for probable GAD and/or major depression and internet access. IG: 43 CG: 44 | IG: Access to a virtual platform in which they had to complete three skills training lessons in 4 weeks. They did not have to go to their health center except if there was suicidal ideation. CG: they could make use of health services. At the end of the study they had access to the MUMentum program. | IG: internet-applied brief cognitive behavioral therapy (iCBT): MUMentum Pregnancy. CG: usual care. | Pretest | Post-Test | Significant differences were observed between IG and CG in the reduction in anxiety at 1 week after the intervention, but not at 1 month. IG significantly reduced anxiety. | |||||
| (1 week) | (4 weeks) | ||||||||||
| GAD-7 (M) | |||||||||||
| GI | 12.66 | 7.49 | GI | ||||||||
| GC | 11.84 | 9.43 | GC | ||||||||
| Yang et al. (2019) China [56] | 123 women between 20–34 weeks gestation with GAD-7 or PHQ-9 > 4 and with internet access. IG: 62 CG: 61 | The intervention was carried out through a virtual platform. It consisted of 4 sessions of 40 min each, developed over 8 weeks. There was also a telematic group for participants to share experiences. | IG: online therapy based on mindfulness. CG: usual care combined with emotion management skills. | Pretest | Post-Test (end) | Significant reductions in intergroup and IG anxiety and depression were found at the end of the intervention. Mindfulness interventions during pregnancy could be part of the psychological care provided to women during pregnancy. | |||||
| GAD-7 (M) | |||||||||||
| IG | 5.52 | 2.97 | |||||||||
| CG | 5.19 | 5.26 | |||||||||
| Burger et al. (2020) Netherlands [51] | 282 pregnant women with moderate or severe anxiety and/or depression scores. IG: 140 CG: 142 | Beginning in the 20th week of gestation and ending 3 months after delivery. 10–14 individual sessions. | IG: cognitive behavioral therapy CG: usual care | STAI (M) | No improvement was found in the levels of anxiety and depression at any time after the intervention. CBT applied in the perinatal stage does not improve emotional symptomatology. | ||||||
| IG | CG | ||||||||||
| Pretest | 48.6 | 48.6 | |||||||||
| 24 SG | 47.7 | 47.7 | |||||||||
| 36 SG | 43.2 | 43.2 | |||||||||
| 6 SPP | 40.9 | 40.9 | |||||||||
| 3 MPP | 43.8 | 43.8 | |||||||||
| 6 MPP | 42.1 | 42.1 | |||||||||
| 12 MPP | 41.0 | 41.0 | |||||||||
| 18 MPP | 40.9 | 40.1 | |||||||||
| Heller et al. (2020) Netherlands [52] | 159 women < 30 weeks gestation with CES-D> 16 and/or HADS-A≥ 8. IG: 79 CG: 80 | Start before 30 weeks of gestation. IG: five modules presented on a weekly basis. Each module consists of information, examples of other mothers and homework. | IG: internet-based intervention “MamaKits online” based on problem-solving. CG: usual care | Pretest | Post-test | No significant differences were found between the groups. | |||||
| HADS-A (>8) | End | 36 GW | 6 PPW | ||||||||
| IG | 11.4 | 8.4 | 7.9 | 7.1 | |||||||
| CG | 11.9 | 8.6 | 7.9 | 7.9 | |||||||
| MacKinnon et al. (2021) Canada [54] | 60 pregnant women between 12–28 weeks of gestation with elevated levels of distress. IG: 28 CG: 32 | IG: 8 group sessions (3–6 participants) per week of 2 h duration. CG: usual care. | Mindfulness-based cognitive therapy for perinatal depression (MBCT-PD). | * Point out the quadratic effect. | The intervention group significantly reduced levels of distress, but there was no reduction in symptoms of depression and anxiety. | ||||||
| Pretest | |||||||||||
| GAD-7 (M) | |||||||||||
| IG | 6.32 | ||||||||||
| CG | 8.52 | ||||||||||
| Yang et al. (2022) China [57] | 149 women with gestational age < 32, with GAD-7 or PHQ-9 > 4 and with internet access. IG: 100 MT = 50 MAT = 50 CG: 49 | The intervention was carried out through a virtual platform. The participants received 4 weekly mindfulness sessions lasting an hour and a half. There was also a telematic group to share experiences among the participants. During weeks 2 and 4 the psychologist contacted them to solve problems and encourage adherence. MT: present-centered training MAT: acceptance-centered training. | IG: online therapy based on mindfulness-based mindfulness focused on the present (MT). IG: online therapy based on mindfulness focused on acceptance (MAT). CG: course of emotion management without mindfulness practice. | GAD-7 (M) | Significant differences in anxiety and depression were observed in the MAT group. Differences were not significant in the MAT group nor in the control group, nor between both groups. Mindfulness could be a promising technique to improve anxious and depressive symptoms. | ||||||
| Pretest | MT | 6.96 | |||||||||
| MAT | 7.20 | ||||||||||
| CG | 6.90 | ||||||||||
| Post-test (2 weeks) | MT | 5.48 | |||||||||
| MAT | 2.60 | ||||||||||
| CG | 6.50 | ||||||||||
| * Zhang, Li et al. (2023) China [59] | 160 women between 12–24 weeks gestation with symptoms of anxiety (GAD-7 ≥ 5) or depression EPDS ≥ 9). IG: 80 CG: 80 | The intervention was carried out through a Wechat program. It consisted of 6 modules, each lasting 1 week. Each module consisted of a thematic lesson and homework. | IG: guided self-help mindfulness therapy (Wechat). CG: usual care. | Pre (12–20 GW) | End (20–28 GW) | Before delivery (36–37 GW) | 6PPW | 3PPM | 6PPM | Digitally delivered programs are effective in reducing distress among pregnant women. | |
| GAD-7 (M) | |||||||||||
| IG | 5.56 | 3.14 | 3.32 | 4.49 | 4.34 | 3.75 | |||||
| CG | 5.80 | 5.61 | 6.18 | 7.31 | 5.90 | 5.90 | |||||
| Zhang, Lin et al. (2023) China [60] | 108 women between 12 and 24 weeks of pregnancy with symptoms of anxiety (GAD-7 ≥ 5) or depression (EPDS ≥ 9). IG: 54 CG: 54 | IG: Intervention carried out through the WeChat program. It consisted of four weekly sessions, each lasting 30 min, and between 30 and 45 min of daily mindfulness practice. CG: Education on prenatal care through the WeChat program. | IG: Mindfulness course through the WeChat program. CG: prenatal education. | Pretest | Post-Test | The self-help and mindfulness intervention reduced prenatal stress and negative affect and improved positive affect and mindfulness. | |||||
| (end treatm.) | (15 weeks) | ||||||||||
| GAD-7 (M) | |||||||||||
| IG | 5.73 | 4.56 | IG | ||||||||
| CG | 5.63 | 5.98 | CG | ||||||||
| Postpartum | |||||||||||
| * Loughnan, Butler, et al. (2019) Australia [62] | 131 women within 12 months postpartum with GAD-7 and/or PHQ-9 ≥ 10 and with internet access. IG: 69 CG: 62 | IG: Access to a virtual platform where they had to complete three skill training lessons in six weeks. They were only contacted if they presented suicidal ideation. CG: They could make use of health services. | GI: Brief Cognitive Behavioral Therapy applied via the internet (iCBT): MUMentum Postnatal CG: usual CARE | Pretest | Post-Test | Significant reductions in intergroup and intragroup anxiety and depression levels were observed both one week and one month after the intervention. There is preliminary evidence of the program’s effectiveness in treating anxiety and/or depression in women during the postpartum period. | |||||
| (1 week) | (4 weeks) | ||||||||||
| GAD-7 (M) | |||||||||||
| IG | 12.08 | 6.66 | GI | ||||||||
| CG | 12.26 | 10.44 | GC | ||||||||
| * Appleton et al. (2025) Australia [61] | 141 women up to 24 weeks postpartum who score high in stress, depression or anxiety. | IG: Eight weekly two-hour (16 h) group sessions per week with a maximum of 12 women per group and two facilitators + a follow-up session (group meeting) four weeks after the last sessions, and an individual psychoeducation session for the woman’s partner around the fifth or sixth week after the last sessions, with a maximum of 12 women per group and two facilitators + a follow-up session (group meeting) four weeks after the last sessions, and an individual psychoeducation session for the woman’s partner around the fifth or sixth week after the last sessions. | IG: Group psychotherapy program | Pretest | Post-Test | These findings support the efficacy of group psychotherapy interventions in reducing symptoms of depression and anxiety in the postpartum period. | |||||
| EDS-3A (M) | |||||||||||
| 5.68 | 4.37 | ||||||||||
| Study | Intervention Type | Perinatal Period (Pregnancy/Postpartum) | Therapeutic Approach | Application Format | Effective Interventions |
|---|---|---|---|---|---|
| Anton & David (2015) [45] | Universal | Pregnancy | CBT | Face-to-face Individual + Group | V |
| Fontein-Kuipers et al. (2016) [46] | Universal | Pregnancy | Peer support program | Online Individual | V |
| Salehi et al. (2016) [47] | Universal | Pregnancy | CBT | Face-to-face Group | V |
| Yazdanimehr et al. (2016) [58] | Selective/ Indicated | Pregnancy | Cognitive behavioral therapy based on mindfulness | Face-to-face Group | V |
| Dennis-Tiwary et al. (2017) [43] | Universal | Pregnancy | ABMT | Online Individual | |
| Townshend et al. (2018) [55] | Selective/ Indicated | Pregnancy | Mindfulness | Face-to-face Group | V |
| Warriner et al. (2018) [49] | Universal | Pregnancy | Mindfulness | Face-to-face Group | V |
| Loughnan, Sie, et al. (2019) [53] | Selective/ Indicated | Pregnancy | CBT | Online Individual | |
| Yang et al. (2019) [56] | Selective/ Indicated | Pregnancy | Mindfulness | Online Individual | |
| Zhang et al. (2019) [50] | Universal | Pregnancy | Mindfulness | Face-to-face Group | |
| Burger et al. (2020) [51] | Selective/ Indicated | Pregnancy | CBT | Face-to-face Group | |
| Heller et al. (2020) [52] | Selective/ Indicated | Pregnancy | CBT | Online Individual | |
| Sharma et al. (2020) [48] | Universal | Pregnancy | CBT | Face-to-face Not specified | V |
| MacKinon et al. (2021) [54] | Selective/ Indicated | Pregnancy | Cognitive behavioral therapy based on mindfulness | Face-to-face Group | |
| Yang et al. (2022) [57] | Selective/ Indicated | Pregnancy | Mindfulness | Online Individual | |
| Mahoney et al. (2023) [44] | Universal | Pregnancy | CBT | Online Individual | |
| Zhang, Li, et al. (2023) [59] | Selective/ Indicated | Pregnancy | Mindfulness | Online Individual | V |
| Zhang, Lin, et al. (2023) [60] | Selective/ Indicated | Pregnancy | Mindfulness | Online Individual | |
| Loughnan, Butler, et al. (2019) [62] | Selective/ Indicated | Postpartum | CBT | Online Individual | V |
| Appleton et al. (2025) [61] | Selective/ Indicated | Postpartum | Combines different therapeutic approaches | Face-to-face Group | V |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Val, A.; Posse, C.M.; Míguez, M.C. Preventive Psychological Interventions for the Management of Perinatal Anxiety: A Systematic Review. Brain Sci. 2025, 15, 861. https://doi.org/10.3390/brainsci15080861
Val A, Posse CM, Míguez MC. Preventive Psychological Interventions for the Management of Perinatal Anxiety: A Systematic Review. Brain Sciences. 2025; 15(8):861. https://doi.org/10.3390/brainsci15080861
Chicago/Turabian StyleVal, Alba, Cristina M. Posse, and M. Carmen Míguez. 2025. "Preventive Psychological Interventions for the Management of Perinatal Anxiety: A Systematic Review" Brain Sciences 15, no. 8: 861. https://doi.org/10.3390/brainsci15080861
APA StyleVal, A., Posse, C. M., & Míguez, M. C. (2025). Preventive Psychological Interventions for the Management of Perinatal Anxiety: A Systematic Review. Brain Sciences, 15(8), 861. https://doi.org/10.3390/brainsci15080861





